Abstract
Objective
To investigate the differences in mandibular retromolar space among skeletal Class I subjects with different vertical divergence using cone-beam computed tomography (CBCT).
Materials and Methods
A total of 123 skeletal Class I patients (aged 20–40 years) were categorized into hypodivergent, normodivergent, and hyperdivergent groups based on S-N/Go-Me and facial height index (FHI). Mandibular retromolar space was measured at four planes parallel to the occlusal plane along the sagittal line and molar cuspal line, respectively. The mandibular retromolar space was compared among the three vertical groups.
Results
The hyperdivergent group had a significantly smaller mandibular retromolar space compared with the other two groups, while the hypodivergent group had the largest retromolar space. In addition, the hyperdivergent group had a larger number of subjects whose roots contacted the lingual cortex of the mandibular body.
Conclusions
The hyperdivergent group tends to exhibit the smallest mandibular retromolar space and highest risk of cortex contact. Clinicians should keep in mind that successful molar distalization requires sufficient retromolar space, especially for hyperdivergent subjects, which should be verified with CBCT.
Keywords: Vertical facial types, Retromolar space, Molar distalization, CBCT
INTRODUCTION
Space management is the main task in orthodontic treatment. Expansion, extraction, and interproximal reduction are some of the methods used by orthodontists to resolve crowding and achieve an ideal molar relationship.1 Recently, molar distalization has gained more attention. Compared with other treatment modalities, molar distalization has fewer irreversible effects.2,3
Successful molar distalization depends on the identification of the anatomic limit of the mandible. This is important to minimize the risk of potential damage to molar roots and alveolar bone. Existing studies regarding the retromolar space were conducted on panoramic radiographs or lateral cephalograms in which the anterior border of the ramus was presumed to be the posterior anatomic limitation for mandibular molar distalization.4,5 However, those studies used two-dimensional radiographs with inherent limitations due to the superimposition and distortion of anatomical structures.
Cone-beam computed tomography (CBCT) has been widely used in dental research as a reliable and accurate method for linear measurements.6 The close proximity of lower molar roots to buccal and lingual cortices has been observed in several studies. The lingual cortex rather than the ramus was found to be a more suitable anatomic limit. In addition, one-third of the mandibular second molar roots were found to be in contact with the inner lingual cortex.7 Recently, a study compared the retromolar space between subjects with Class I and Class III malocclusions.8 However, there has yet to be a study exploring how the vertical facial types influence the retromolar space at the root level.
The purpose of this study was to investigate the association between different vertical facial types and retromolar space in skeletal Class I subjects using CBCT images.
MATERIALS AND METHODS
CBCT scans of 123 subjects, aged between 20 and 40 years, were included in this study. These subjects were selected from a large pool of patients who were admitted for orthodontic treatment from 2014 to 2018 at the Department of Orthodontics, Affiliated Stomatology Hospital of Guangzhou Medical University. The inclusion criteria were (1) skeletal (0° < ANB < 4°) and dental (canine/molar) Class I relationship, (2) crowding of less than 4 mm in the mandibular arch, (3) normal overjet and overbite, (4) healthy periodontal state with no noticeable alveolar bone loss, (5) no prostheses or missing teeth (except third molars), (6) no obvious facial asymmetry and deformation, (7) no cleft lip and/or palate, (8) no diagnosed systemic disease, and (9) no history of orthodontic treatment. The study was approved by the Research and Ethics Committee of the Affiliated Stomatology Hospital of Guangzhou Medical University (No. KY2019023). The CBCT scans were obtained using Newtom (VG, Verona, Italy). The imaging parameters were as follows: 110 kV, 3.07 mA, scan time of 18 seconds, with a voxel size of 0.15 mm and focal spot of 0.3 mm. Images were saved as digital imaging and communications in medicine (DICOM) format. The DICOM files were reconstructed into three-dimensional (3D) images using QR-NNT software (version 7.2, ImageWork, Elmsford, NY).
Cephalometric analyses were performed on CBCT-derived cephalograms obtained with Dolphin 9.0 Imaging software (Dolphin Imaging & Management Solutions, Chatsworth, Calif). The mandibular plane angle and facial height index (FHI) were used to determine the vertical facial types. The mandibular plane angle (S-N/Go-Me) was formed by the Sella-Nasion line and the Gonion-Menton line. The FHI was the ratio of the posterior facial height (distance from Sella to Gonion) to the anterior facial height (distance from Nasion to Menton). According to these two measurements, all subjects were classified into one of the three groups: hypodivergent group (S-N/Go-Me <27°, FHI >69%), normodivergent group (27° < S-N/Go-Me < 37°, 61% < FHI < 69%), and hyperdivergent group (S-N/Go-Me >37°, FHI <61%).9
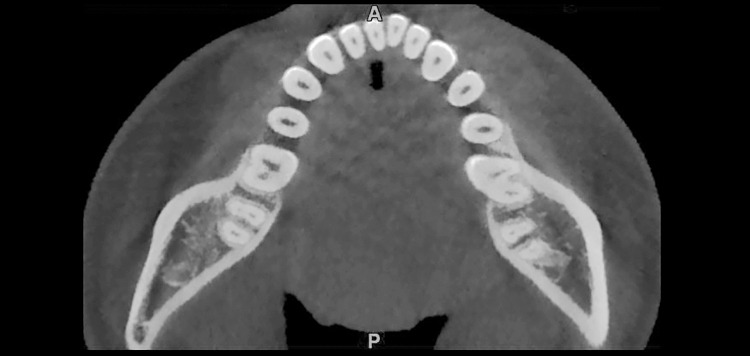
To obtain standardized orientation of the 3D images, the mandibular occlusal plane connecting the mesiobuccal cusp tips of the mandibular first molars and the right mandibular central incisor tip was used as the horizontal reference plane. The midsagittal plane was constructed using the crista galli, ANS, and opisthion (Figure 1). The retromolar space of the mandible was measured on four different planes parallel to the mandibular occlusal plane. The plane passing through the furcation of the mandibular second molar root was named the 0-plane, whereas the other three planes, which were located at the depths of 2, 4, and 6 mm apical to the 0-plane, were named the 2-plane, 4-plane, and 6-plane, respectively. The cuspal line, which connects the mesial buccal cusps of the mandibular first and second molar, was constructed at the occlusal reference plane (Figure 2A, line b). The sagittal line was then constructed from the point of interception of the cuspal line with the occlusal outline of the first mandibular molars and parallel to the midsagittal plane (Figure 2A, line a). These two reference lines were then projected to the 0-, 2-, 4-, and 6-planes as the reference lines in each plane for linear measurements.8 The angle formed by these two reference lines was measured (Figure 2A). The number of subjects whose roots contacted the inner lingual cortex of the mandibular body was calculated at each plane. Lastly, the shortest distances between the most lingual point of the distal root of the mandibular second molar and inner and outer lingual cortex of the mandibular body were measured parallel to both the sagittal line and the cuspal line at the 0-, 2-, 4-, and 6-planes (Figure 2B, C). All measurements in this study were conducted using the QR-NNT software.
Figure 1.
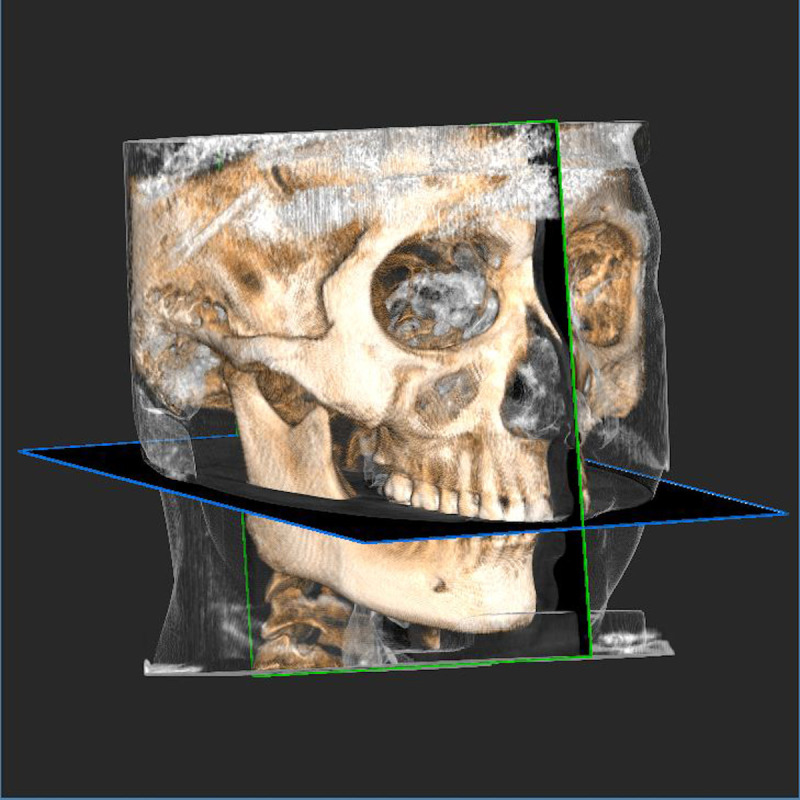
Reference planes used in this study. The mandibular occlusal plane: connection of the mesiobuccal cusps of the mandibular first molars and the right mandibular central incisor tip. The midsagittal plane: passing through ANS, crista galli, opisthion, and midpoint of the mandibular incisor tip.
Figure 2.

(A) Reference lines at the occlusal level. (a) The sagittal line that parallels the midsagittal plane. (b) The cuspal line that connects the mesial buccal cusps of the mandibular first and second molars. (α) The angle between the sagittal and cuspal lines. (B) Retromolar space at root level. (C) Close-up view of the mandibular retromolar space. (S–I) Distance between the most lingual point of the distal root of the mandibular second molar and the inner lingual cortex of the mandibular body measured parallel to the sagittal line. (S–O) Distance between the most lingual point of the distal root of the mandibular second molar and the outer lingual cortex of the mandibular body measured parallel to the sagittal line. (C–I) Distance between the most lingual point of the distal root of the mandibular second molar and the inner lingual cortex of the mandibular body measured parallel to the cuspal line. (C–O) Distance between the most lingual point of the distal root of the mandibular second molar and the outer lingual cortex of the mandibular body measured parallel to the cuspal line.
Statistical Analysis
PASS software (PASS 11. NCSS, LLC, Kaysville, Utah) was used to estimate the minimum sample size, and 123 subjects, with 41 patients in each group, were included in this study. The statistical analyses were performed using SPSS software (version 24.0, IBM Corporation, NY).
To assess the reliability of the measurements, 35 randomly selected 3D images were reoriented and remeasured by the same investigator 2 weeks after the initial analysis. The methodological errors (MEs) were calculated using Dahlberg's formula: ME:  , where d represents the difference between two registrations and n is the number of duplicate registrations. The data were then checked for normal distribution by Shapiro-Wilk test and homogeneity of the variances.
, where d represents the difference between two registrations and n is the number of duplicate registrations. The data were then checked for normal distribution by Shapiro-Wilk test and homogeneity of the variances.
Since an independent t-test showed no statistically significant difference between the measurements on the left and right sides, the averaged values were used. To investigate the impact of the third molar on the retromolar space, the two sides of 123 patients were divided into two groups: the third-molar group and the no third-molar group (ie, the third molar was extracted or congenitally missing). Since the independent t-test showed no significant differences between the two groups for any measurement at each plane, subsequent statistical analyses were performed on the whole sample.
One-way analysis of variance and chi-square tests were applied to detect significant differences in baseline information and variables relevant to the retromolar space among the three groups. The SNK-q test was used to compare each pair of two groups. The numbers of patients whose root contacted with the inner surface of the lingual cortex in at least one plane in the three groups were compared through the chi-square test (Figure 3). The significance level was set at P < .05 for all statistical analyses.
Figure 3.
Patient with root contacting the lingual cortex.
RESULTS
The ME for retromolar space measurements ranged from 0.11 mm for the distance along the sagittal line at the 2-plane to 0.35 mm along the cuspal line at the 2-plane. There was no significant difference between the measurements performed 2 weeks apart. No significant difference was found in age or gender distribution among the three experimental groups, except for S-N/Go-Me and FHI. The baseline information for subjects in the three groups is shown in Table 1. The distances of the retromolar space did not show statistical differences between the left and right sides (Table 2). Likewise, the presence of the mandibular third molar had no significant influence on the distance of the retromolar space (Table 3). The angle formed between the sagittal and cuspal lines also showed no significant differences among the three groups (Table 4).
Table 1.
Patient Characteristics in the Three Groupsa
| SN-MP (Mean ± SD) |
FHI (Mean ± SD) |
Age (Mean ± SD) |
Sex |
Number (n) |
||
| Male (%) |
Female (%) |
|||||
| Hypodivergent | 23.11 ± 3.10 | 71.65 ± 2.35 | 24.00 ± 3.87 | 24.39% (n = 10) | 75.61% (n = 31) | 41 |
| Normodivergent | 32.26 ± 2.70 | 65.35 ± 1.71 | 23.39 ± 2.79 | 21.95% (n = 9) | 78.05% (n = 32) | 41 |
| Hyperdivergent | 41.36 ± 3.38 | 58.44 ± 2.69 | 23.46 ± 3.98 | 17.07% (n = 7) | 82.93% (n = 34) | 41 |
| F/χ2 | 360.683 | 342.244 | 0.353 | 0.683 | — | |
| P | .000* | .000* | .703 | .711 | — | |
Values are presented as mean ± standard deviation.
Statistically significant at P < .05.
Table 2.
Comparison of Retromolar Space Between the Left Side and Right Side Among Groupsa
| Hypodivergent (41) |
Normodivergent (41) |
Hyperdivergent (41) |
||||||||||
| Right Side |
Left Side |
t |
P |
Right Side |
Left Side |
t |
P |
Right Side |
Left Side |
t |
P |
|
| Sagittal line to inner | ||||||||||||
| 0-plane | 3.19 ± 1.54 | 3.72 ± 1.77 | −1.444 | .268 | 2.26 ± 1.27 | 2.66 ± 1.59 | −1.256 | .110 | 1.56 ± 1.34 | 1.67 ± 1.65 | −0.331 | .221 |
| 2-plane | 3.01 ± 1.53 | 3.10 ± 1.70 | −0.276 | .583 | 2.12 ± 1.38 | 2.38 ± 1.65 | −0.764 | .492 | 1.48 ± 1.49 | 1.53 ± 1.66 | −0.147 | .996 |
| 4-plane | 2.90 ± 1.43 | 2.60 ± 1.55 | 0.917 | .727 | 1.96 ± 1.41 | 2.06 ± 1.36 | −0.342 | .650 | 1.27 ± 1.42 | 1.30 ± 1.64 | −0.082 | .921 |
| 6-plane | 2.88 ± 1.62 | 2.81 ± 1.56 | 0.215 | .871 | 2.10 ± 1.23 | 2.10 ± 1.56 | 0.016 | .121 | 1.36 ± 1.48 | 1.34 ± 1.63 | 0.057 | .752 |
| Cuspal line to inner | ||||||||||||
| 0-plane | 6.27 ± 3.37 | 6.47 ± 3.33 | −0.267 | .893 | 4.57 ± 2.88 | 4.84 ± 2.94 | −0.418 | .950 | 3.48 ± 3.41 | 3.18 ± 3.05 | 0.409 | .432 |
| 2-plane | 5.56 ± 2.95 | 5.33 ± 3.24 | 0.335 | .575 | 3.95 ± 2.78 | 4.06 ± 2.76 | −0.191 | .560 | 2.77 ± 2.96 | 2.74 ± 2, 91 | 0.056 | .954 |
| 4-plane | 5.13 ± 2.63 | 4.69 ± 3.08 | 0.698 | .399 | 3.63 ± 2.48 | 3.70 ± 2.67 | −0.137 | .927 | 2.32 ± 2.56 | 2.17 ± 2.60 | 0.269 | .960 |
| 6-plane | 5.58 ± 3.43 | 4.93 ± 2.91 | 0.921 | .668 | 3.80 ± 2.38 | 3.51 ± 2.58 | 0.530 | .383 | 2.49 ± 2.68 | 2.28 ± 2.66 | 0.3565 | .620 |
| Sagittal line to outer | ||||||||||||
| 0-plane | 6.75 ± 1.89 | 6.86 ± 1.90 | −0.233 | .676 | 5.50 ± 1.79 | 6.18 ± 2.19 | −1.522 | .369 | 4.85 ± 1.79 | 5.12 ± 2.67 | −0.529 | .347 |
| 2-plane | 6.53 ± 1.92 | 6.40 ± 1.87 | 0.315 | .791 | 5.44 ± 1.92 | 5.78 ± 2.02 | −0.778 | .940 | 4.71 ± 2.06 | 4.76 ± 2.17 | −0.089 | .754 |
| 4-plane | 6.35 ± 1.64 | 5.99 ± 1.90 | 0.915 | .364 | 5.26 ± 2.05 | 5.43 ± 2.05 | −0.372 | .612 | 4.27 ± 2.10 | 4.38 ± 2.03 | −0.241 | .508 |
| 6-plane | 6.28 ± 1.98 | 5.92 ± 1.86 | 0.833 | .755 | 5.29 ± 1.78 | 5.21 ± 2.12 | 0.175 | .208 | 4.32 ± 2.01 | 4.50 ± 2.06 | −0.396 | .887 |
| Cuspal line to outer | ||||||||||||
| 0-plane | 10.60 ± 3.45 | 10.65 ± 3.64 | −0.065 | .578 | 8.94 ± 3.11 | 9.26 ± 3.08 | −0.460 | .804 | 8.06 ± 3.62 | 7.46 ± 3.07 | 0.812 | .185 |
| 2-plane | 10.03 ± 3.46 | 9.80 ± 3.51 | 0.310 | .824 | 8.43 ± 3.17 | 8.58 ± 3.08 | −0.223 | .574 | 7.19 ± 3.47 | 7.18 ± 3.26 | 0.023 | .488 |
| 4-plane | 9.91 ± 3.41 | 9.24 ± 3.57 | 0.869 | .491 | 8.06 ± 3.16 | 8.29 ± 3.44 | −0.314 | .063 | 6.77 ± 3.45 | 6.96 ± 3.55 | −0.249 | .884 |
| 6-plane | 10.11 ± 4.01 | 9.76 ± 3.81 | 0.407 | .865 | 8.62 ± 3.17 | 8.23 ± 3.63 | 0.511 | .368 | 7.37 ± 4.16 | 7.50 ± 3.64 | −0.141 | .315 |
Values are presented as mean ± standard deviation.
Table 3.
Comparison of Retromolar Space Between Mandibular Third Molar Group and Nonmandibular Third Molar Groupa
| Inner Cortex |
t |
P |
Outer Cortex |
t |
P |
||||
| Without |
With |
Without |
With |
||||||
| Total sample | n = 75 | n = 171 | n = 75 | n = 171 | |||||
| Through sagittal line | 0-plane | 2.32 ± 1.64 | 2.59 ± 1.74 | −1.143 | .168 | 4.23 ± 3.38 | 5.05 ± 3.36 | −1.754 | .109 |
| 2-plane | 2.01 ± 1.57 | 2.38 ± 1.72 | −1.595 | .220 | 5.26 ± 2.01 | 5.75 ± 2.13 | −1.684 | .326 | |
| 4-plane | 1.68 ± 1.47 | 2.16 ± 1.60 | −0.200 | .339 | 4.85 ± 2.01 | 5.47 ± 2.11 | −2.142 | .593 | |
| 6-plane | 1.90 ± 1.54 | 2.31 ± 2.06 | −1.559 | .325 | 4.98 ± 1.97 | 5.37 ± 2.11 | −1.366 | .538 | |
| Through cuspal line | 0-plane | 5.44 ± 1.96 | 6.07 ± 2.25 | −2.097 | .140 | 8.57 ± 3.81 | 9.42 ± 3.35 | −1.749 | .885 |
| 2-plane | 3.61 ± 3.22 | 4.27 ± 3.05 | −1.542 | .523 | 7.84 ± 3.74 | 8.84 ± 3.33 | −2.083 | .863 | |
| 4-plane | 2.96 ± 2.74 | 3.89 ± 2.89 | −2.357 | .339 | 7.25 ± 3.42 | 8.62 ± 3.58 | −2.809 | .547 | |
| 6-plane | 3.24 ± 2.87 | 4.00 ± 3.05 | −1.837 | .583 | 7.91 ± 3.58 | 8.90 ± 3.95 | −1.862 | .310 | |
| Hyperdivergent | n=20 | n=62 | n=20 | n=62 | |||||
| Through sagittal line | 0-plane | 1.23 ± 1.23 | 1.74 ± 1.56 | 1.236 | .189 | 1.60 ± 0.36 | 2.44 ± 0.31 | 0.928 | .356 |
| 2-plane | 1.25 ± 1.18 | 1.59 ± 1.68 | 0.845 | .401 | 4.40 ± 1.89 | 4.85 ± 2.17 | 0.830 | .409 | |
| 4-plane | 0.96 ± 1.29 | 1.39 ± 1.56 | 1.096 | .276 | 4.02 ± 1.74 | 4.43 ± 2.15 | 0.769 | .444 | |
| 6-plane | 1.10 ± 1.45 | 1.43 ± 1.58 | 0.823 | .408 | 4.10 ± 1.64 | 4.50 ± 2.14 | 0.776 | .440 | |
| Through cuspal line | 0-plane | 2.47 ± 2.43 | 3.61 ± 3.41 | 1.388 | .169 | 6.72 ± 2.76 | 8.10 ± 3.47 | 1.624 | .108 |
| 2-plane | 2.03 ± 2.01 | 2.99 ± 3.14 | 1.282 | .204 | 7.61 ± 3.52 | 5.85 ± 2.39 | 1.997 | .052 | |
| 4-plane | 1.45 ± 1.80 | 2.50 ± 2.73 | 1.613 | .111 | 5.62 ± 2.26 | 7.27 ± 3.72 | 1.868 | .065 | |
| 6-plane | 1.67 ± 2.22 | 2.62 ± 2.76 | 1.398 | .166 | 6.54 ± 2.89 | 7.72 ± 4.14 | 1.193 | .237 | |
| Normodivergent | n=26 | n=56 | n=26 | n=56 | |||||
| Through sagittal line | 0-plane | 2.16 ± 0.87 | 2.60 ± 1.63 | 1.292 | .200 | 5.33 ± 1.91 | 6.07 ± 2.04 | 1.579 | .118 |
| 2-plane | 1.75 ± 0.98 | 2.48 ± 1.66 | 1.870 | .066 | 5.06 ± 1.47 | 5.86 ± 2.12 | 1.740 | .086 | |
| 4-plane | 1.68 ± 1.19 | 2.16 ± 1.45 | 1.469 | .146 | 4.82 ± 1.96 | 5.59 ± 2.05 | 1.595 | .115 | |
| 6-plane | 1.79 ± 1.18 | 2.24 ± 1.47 | 1.358 | .178 | 4.72 ± 1.76 | 5.49 ± 1.99 | 1.697 | .094 | |
| Through cuspal line | 0-plane | 3.88 ± 1.67 | 5.09 ± 3.25 | 1.783 | .078 | 8.19 ± 2.49 | 9.51 ± 3.25 | 1.834 | .070 |
| 2-plane | 3.26 ± 1.79 | 4.35 ± 3.06 | 1.675 | .098 | 7.83 ± 2.71 | 8.83 ± 3.25 | 1.356 | .179 | |
| 4-plane | 3.03 ± 2.11 | 3.96 ± 2.71 | 1.555 | .124 | 7.28 ± 2.95 | 8.59 ± 3.38 | 1.695 | .094 | |
| 6-plane | 3.09 ± 2.26 | 3.92 ± 2.26 | 1.400 | .164 | 7.62 ± 3.16 | 8.80 ± 3.47 | 1.471 | .145 | |
| Hypodivergent | n=29 | n=53 | n=29 | n=53 | |||||
| Through sagittal line | 0-plane | 3.27 ± 1.63 | 3.55 ± 1.69 | 0.702 | .485 | 6.53 ± 1.88 | 6.95 ± 1.88 | 0.978 | .331 |
| 2-plane | 2.95 ± 1.61 | 3.11 ± 1.62 | 0.400 | .690 | 6.27 ± 1.97 | 6.56 ± 1.84 | 0.656 | .514 | |
| 4-plane | 2.59 ± 1.52 | 2.82 ± 1.48 | 0.659 | .512 | 5.95 ± 1.82 | 6.29 ± 1.76 | 0.805 | .423 | |
| 6-plane | 2.87 ± 1.57 | 2.83 ± 1.59 | −0.086 | .932 | 6.07 ± 1.95 | 6.11 ± 1.92 | 0.080 | .937 | |
| Through cuspal line | 0-plane | 5.91 ± 3.94 | 6.60 ± 2.95 | 0.908 | .367 | 10.21 ± 4.34 | 10.85 ± 3.00 | 0.785 | .435 |
| 2-plane | 5.46 ± 3.74 | 5.43 ± 2.69 | −0.052 | .959 | 9.78 ± 4.30 | 9.98 ± 2.95 | 0.253 | .801 | |
| 4-plane | 4.60 ± 3.00 | 5.07 ± 2.79 | 0.708 | .481 | 9.05 ± 3.79 | 9.85 ± 3.32 | 0.985 | .328 | |
| 6-plane | 5.06 ± 3.11 | 5.09 ± 2.91 | 0.039 | .969 | 9.66 ± 3.73 | 10.09 ± 4.00 | 0.486 | .628 | |
Values are presented as mean ± standard deviation. n, number of subject.
Table 4.
Comparison of Angle Between the Sagittal Line and Cuspal Line Among Groupsa
| Angle (Mean ± SD) |
|
| Hypodivergent (41) | 18.72 ± 4.63 |
| Normodivergent (41) | 18.26 ± 4.21 |
| Hyperdivergent (41) | 18.93 ± 4.94 |
| F | 0.462 |
| P | .631 |
Values are presented as mean ± standard deviation.
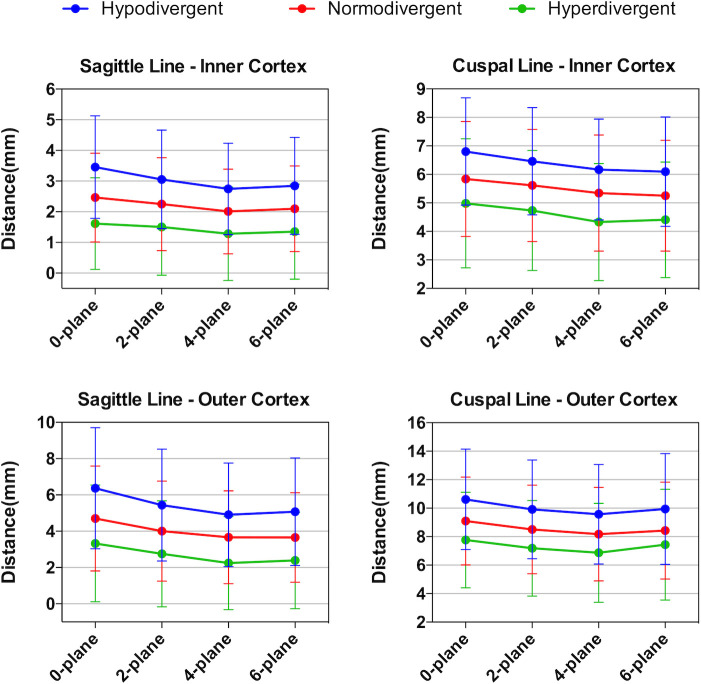
Significant intergroup differences were noticed in distances between the most lingual point of the distal root of the mandibular second molar and the inner/outer lingual cortex of the mandibular body measured along the two reference lines on four measurement planes among the three groups (P < .001), and the SNK-q test showed there were statistically significant differences among the three groups (Tables 5 and 6; Figure 4). When considering the number of mandibular molar distal roots in contact with the inner lingual cortex of the mandible in at least one plane among the three groups, a significantly higher number was found in the hyperdivergent group (27, 65.85%) as compared with the normodivergent group (11, 26.83%) and hypodivergent group (5, 12.20%; Table 7).
Table 5.
Comparison of Distance Between the Distal Root of the Mandibular Second Molar and the Inner Surface of the Lingual Cortex of the Mandibular Body Among the Three Groupsa
| Distance Measured by Sagittal Line |
F |
P |
Distance Measured by Cuspal Line |
F |
P |
|||||
| Hypodivergent (n = 41) |
Normodivergent (n = 41) |
Hyperdivergent (n = 41) |
Hypodivergent (n = 41) |
Normodivergent (n = 41) |
Hyperdivergent (n = 41) |
|||||
| 0-plane | 3.45 ± 1.67 | 2.46 ± 1.45b | 1.61 ± 1.49bc | 29.355 | .000* | 6.37 ± 3.33 | 4.70 ± 2.89b | 3.33 ± 3.22bc | 19.101 | .000* |
| 2-plane | 3.05 ± 1.60 | 2.25 ± 1.51b | 1.50 ± 1.57bc | 20.166 | .000* | 5.44 ± 3.08 | 4.00 ± 2.75b | 2.75 ± 2.92bc | 17.358 | .000* |
| 4-plane | 2.74 ± 1.49 | 2.01 ± 1.38b | 1.28 ± 1.52bc | 20.308 | .000* | 4.91 ± 2.85 | 3.67 ± 2.56b | 2.24 ± 2.57bc | 20.528 | .000* |
| 6-plane | 2.85 ± 1.58 | 2.10 ± 1.39b | 1.35 ± 1.54bc | 20.059 | .000* | 5.08 ± 2.96 | 3.65 ± 2.47b | 2.39 ± 2.66bc | 20.337 | .000* |
| F | 3.129 | 1.566 | 0.769 | 2.417 | 1.461 | 1.693 | ||||
| P | .053 | .198 | .512 | .066 | .225 | .168 | ||||
Values are presented as mean ± standard deviation.
Significant difference with hypodivergent group.
Significant difference with normodivergent group.
Statistically significant at P < .05.
Table 6.
Comparison of Distance Between the Distal Root of the Mandibular Second Molar and the Outer Surface of the Lingual Cortex of the Mandibular Body Among the Three Groupsa
| Distance Measured by Sagittal Line |
F |
P |
Distance Measured by Cuspal Line |
F |
P |
|||||
| Hypodivergent (n = 41) |
Normodivergent (n = 41) |
Hyperdivergent (n = 41) |
Hypodivergent (n = 41) |
Normodivergent (n = 41) |
Hyperdivergent (n = 41) |
|||||
| 0-plane | 6.80 ± 1.88 | 5.84 ± 2.02b | 4.98 ± 2.27bc | 15.970 | .000* | 10.62 ± 3.52 | 9.10 ± 3.08b | 7.76 ± 3.35bc | 15.190 | .000* |
| 2-plane | 6.46 ± 1.88 | 5.61 ± 1.97b | 4.74 ± 2.10bc | 15.466 | .000* | 9.91 ± 3.47 | 8.51 ± 3.11b | 7.18 ± 3.35bc | 13.939 | .000* |
| 4-plane | 6.17 ± 1.77 | 5.35 ± 2.04b | 4.33 ± 2.05bc | 18.224 | .000* | 9.57 ± 3.49 | 8.17 ± 3.29b | 6.86 ± 3.48bc | 12.854 | .000* |
| 6-plane | 6.10 ± 1.92 | 5.25 ± 1.95b | 4.41 ± 2.02bc | 15.230 | .000* | 9.94 ± 3.89 | 8.43 ± 3.40b | 7.43 ± 3.89bc | 9.366 | .000* |
| F | 3.725 | 2.768 | 2.364 | 1.223 | 1.213 | 0.955 | ||||
| P | .051 | .062 | .071 | .301 | .305 | .414 | ||||
Values are presented as mean ± standard deviation.
Significant difference with hypodivergent group.
Significant difference with normodivergent group.
Statistically significant at P < .05.
Figure 4.
Graph of the retromolar space at four different levels of measurement by two different reference lines.
Table 7.
Numbers and Percentages of Patients Whose Root Contacted With the Inner Surface of the Lingual Cortex of the Mandibular Body in Different Vertical Facial Types
| Number |
Percentage (%) |
|
| Hypodivergent (41) | 5 | 12.20 |
| Normodivergent (41) | 11 | 26.83 |
| Hyperdivergent (41) | 27 | 65.85 |
| χ2 | 27.747 | |
| P | .000* | |
Statistically significant at P < .05.
DISCUSSION
Distalization of the mandibular molars/dentition was once considered a challenging treatment objective compared with the distalization of the upper molars/dentition. However, the benefits of distalization of the mandibular molars/dentition are the elimination of mild to moderate crowding, correction of the molar relationship, correction of anterior crossbite, and improvement of a concave facial profile, making it an attractive approach for clinical practice. A previous study found that Class III patients had a larger retromolar space only at the level of the second molar furcation when compared with Class I patients.8 However, the anatomical limitation for molar distalization should be located at the apex level, since the retromolar space decreased as the measurements were taken closer to the root apex.7,8 Therefore, skeletal anteroposterior relations should not have a remarkable effect on retromolar space, and Class I patients were used to explore the association between the vertical facial type and the retromolar space.
Recently, the application of temporary anchorage devices (TADs) has increased the envelope of orthodontic treatment, providing a reliable approach for the distalization of the lower molars/dentition.10 The application of TADs in interradicular spaces between molars could distalize the lower molars no more than 2 to 3 mm. This distance increased to 4 to 5 mm when the retromolar area or the external oblique ridge areas were used.11 In addition, a 3D finite element study has shown that the ramal plate had greater amounts of distal displacement of the posterior teeth than miniscrews, since the force vector with the ramal plate is located superior to the center of resistance (CR) of the lower dentition.12 However, tooth movement may slow down once the root contacts the inner surface of the cortex. Undesirable effects of such root to cortical bone contact may result in root or cortical bone resorption, dehiscence, fenestration, or gingival recession.13 A previous study reported that the minimal mean of the retromolar space was 2.87 mm in Class I subjects, apparently shorter than the 4 to 5 mm of distalization achievable by a ramal plate and miniscrews.7 This discrepancy can be explained by the fact that the distal movement of the lower molars was a tipping movement rather than bodily movement.14 Therefore, successful distalization of the lower dentition can be accomplished only by avoiding cortical bone contact.
Facial divergence has been associated with cortical bone thickness and the morphology of the mandible.15 Hyperdivergent subjects are frequently associated with certain morphological characteristics of the mandible, including a thinner cortex and narrower cross-sectional area.16 In addition, previous studies showed that hyperdivergent subjects have a high incidence of mandibular third molar impaction.17 Therefore, it is reasonable to speculate that facial divergence may also have an effect on retromolar space.
The finding that the presence of the third molar had no significant influence on the retromolar space in the three groups was well in line with the results of a previous study.7 Hence, the presence of the third molar did not lead to remarkable variation of retromolar space, at least in skeletal Class I subjects. In addition, the results were in agreement with a previous study that reported a high correlation between the measurements along the cuspal and sagittal lines at each measurement depth.8 In addition, the angle formed by these two lines was almost constant among the three groups, which verified that the cuspal line can be used as a reliable reference line in future studies.
In the current study, statistical differences were noticed in the retromolar space at each plane among the three groups, which were smallest in the hyperdivergent group and largest in the hypodivergent group. The minimum distance between the root and inner cortex in the hyperdivergent group along the cuspal line was 2.24 and 2.39 mm at the 4-plane and 6-plane, respectively. These distances were fairly close to 2 mm, the amount of distalization of lower molars at the root level reported previously.14 In addition, root contact with the inner lingual cortex was found in 27 of 41 subjects. Because the smallest retromolar space and highest percentage of root contact were observed in the hyperdivergent group, distalization of the mandibular dentition should be carried out cautiously, and CBCT scanning is of vital importance to prevent any undesirable damage.18 Other options, such as premolar extraction, could be considered as an alternative. On the other hand, the retromolar space was 4.91 and 5.08 mm at the 4-plane and 6-plane in the hypodivergent group, more than twice as large as the distance in the hyperdivergent group. Thus, distalization of the mandibular dentition is a more feasible option for hypodivergent subjects. Clinically, the biomechanical strategy must be chosen carefully based on different vertical facial types, since the force direction in relation to the CR of the entire dentition determines rotation of the occlusal plane.19 A force vector parallel to or above the occlusal plane is desirable for hyperdivergent subjects because this force direction can lead to counter-clockwise rotation of the lower occlusal plane, which could contribute to the prevention of open-bite tendency in these subjects. On the other hand, a force vector nearly passing through the CR of the mandibular dentition could maintain the vertical dimension better and facilitate the treatment of hypodivergent subjects.20
A previous study reported that the retromolar space decreased gradually and was smallest at the root apex level.7 However, the current findings showed that the smallest distance was at the 4-plane rather than at the 6-plane, with the exception of the measurements in normodivergent subjects at the cuspal line. This result was in agreement with another study that found that the shortest retromolar space was located at the 4-plane rather than at the 6-plane in Class I subjects.8
One of the limitations of the current study was that differences among gender, which may have an effect on the retromolar space,21 were not evaluated. This was due to the small sample size of male subjects in the study. Furthermore, molar inclinations and eruption and impaction status of the third molars may also influence the retromolar space. Therefore, the impact of these possible additional factors on the retromolar space should be evaluated in future studies.
CONCLUSIONS
The skeletal Class I hyperdivergent group tends to have the smallest retromolar space. The hypodivergent group presents the largest retromolar space, which is more than twice as large as in hyperdivergent subjects.
The hyperdivergent group also has the largest number of subjects whose root contacts with the lingual cortex compared with the normodivergent and hypodivergent groups.
CBCT scanning is recommended in patients who require a large degree of molar distalization, especially hyperdivergent subjects.
REFERENCES
- 1.Vaden JL, Kiser HE. Straight talk about extraction and nonextraction: a differential diagnostic decision. Am J Orthod Dentofacial Orthop. 1996;109:445–452. doi: 10.1016/s0889-5406(96)70127-0. [DOI] [PubMed] [Google Scholar]
- 2.Garib DG, Henriques JF, Janson G, de Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749–758. doi: 10.1016/j.ajodo.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 3.Koretsi V, Chatzigianni A, Sidiropoulou S. Enamel roughness and incidence of caries after interproximal enamel reduction: a systematic review. Orthod Craniofac Res. 2014;17:1–13. doi: 10.1111/ocr.12030. [DOI] [PubMed] [Google Scholar]
- 4.Abu Alhaija ES, AlBhairan HM, AlKhateeb SN. Mandibular third molar space in different antero-posterior skeletal patterns. Eur J Orthod. 2011;33:570–576. doi: 10.1093/ejo/cjq125. [DOI] [PubMed] [Google Scholar]
- 5.Ghougassian SS, Ghafari JG. Association between mandibular third molar formation and retromolar space. Angle Orthod. 2014;84:946–950. doi: 10.2319/120113-883.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozdemir F, Tozlu M, Germec-Cakan D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J Orthod Dentofacial Orthop. 2013;143:190–196. doi: 10.1016/j.ajodo.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Kim SJ, Choi TH, Baik HS, Park YC, Lee KJ. Mandibular posterior anatomic limit for molar distalization. Am J Orthod Dentofacial Orthop. 2014;146:190–197. doi: 10.1016/j.ajodo.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Choi YT, Kim YJ, Yang KS, Lee DY. Bone availability for mandibular molar distalization in adults with mandibular prognathism. Angle Orthod. 2018;88:52–57. doi: 10.2319/040617-237.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horn AJ. Facial height index. Am J Orthod Dentofacial Orthop. 1992;102:180–186. doi: 10.1016/0889-5406(92)70031-5. [DOI] [PubMed] [Google Scholar]
- 10.Ganzer N, Feldmann I, Bondemark L. Pain and discomfort following insertion of miniscrews and premolar extractions: a randomized controlled trial. Angle Orthod. 2016;86:891–899. doi: 10.2319/123115-899.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jing Y, Han X, Guo Y, Li J, Bai D. Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am J Orthod Dentofacial Orthop. 2013;143:877–887. doi: 10.1016/j.ajodo.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 12.Kim YB, Bayome M, Park JH, et al. Displacement of mandibular dentition during total arch distalization according to locations and types of TSADs: 3D finite element analysis. Orthod Craniofac Res. 2019;22:46–52. doi: 10.1111/ocr.12256. [DOI] [PubMed] [Google Scholar]
- 13.Nakada T, Motoyoshi M, Horinuki E, Shimizu N. Cone-beam computed tomography evaluation of the association of cortical plate proximity and apical root resorption after orthodontic treatment. J Oral Sci. 2016;58:231–236. doi: 10.2334/josnusd.15-0566. [DOI] [PubMed] [Google Scholar]
- 14.Yu J, Park JH, Bayome M, Kim S, Kook YA, Kim Y, Kim CH. Treatment effects of mandibular total arch distalization using a ramal plate. Korean J Orthod. 2016;46:212–219. doi: 10.4041/kjod.2016.46.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sato H, Kawamura A, Yamaguchi M, Kasai K. Relationship between masticatory function and internal structure of the mandible based on computed tomography findings. Am J Orthod Dentofacial Orthop. 2005;128:766–773. doi: 10.1016/j.ajodo.2005.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Swasty D, Lee J, Huang JC, Maki K, Gansky SA, Hatcher D, Miller AJ. Cross-sectional human mandibular morphology as assessed in vivo by cone-beam computed tomography in patients with different vertical facial dimensions. Am J Orthod Dentofacial Orthop. 2011;139:e377–e389. doi: 10.1016/j.ajodo.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 17.Breik O, Grubor D. The incidence of mandibular third molar impactions in different skeletal face types. Aust Dental J. 2008;53:320–324. doi: 10.1111/j.1834-7819.2008.00073.x. [DOI] [PubMed] [Google Scholar]
- 18.Oh YH, Park HS, Kwon TG. Treatment effects of microimplant-aided sliding mechanics on distal retraction of posterior teeth. Am J Orthod Dentofacial Orthop. 2011;139:470–481. doi: 10.1016/j.ajodo.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 19.Chae JM, Park JH, Kojima Y, Tai K, Kook YA, Kyung HM. Biomechanical analysis for total distalization of the mandibular dentition: a finite element study. Am J Orthod Dentofacial Orthop. 2019;155:388–397. doi: 10.1016/j.ajodo.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Jo AR, Mo SS, Lee KJ, Sung SJ, Chun YS. Finite-element analysis of the center of resistance of the mandibular dentition. Korean J Orthod. 2017;47:21–30. doi: 10.4041/kjod.2017.47.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chong MX, Khoo CD, Goh KH, Rahman F, Shoji Y. Effect of age on bite force. J Oral Sci. 2016;58:361–363. doi: 10.2334/josnusd.15-0675. [DOI] [PubMed] [Google Scholar]