Abstract
Objective
To evaluate the effects of nonextraction and all first premolar extraction modalities of orthodontic treatment on oral health–related quality of life (OHRQoL) among adolescents.
Materials and Methods
Sixty-eight adolescents of aged 12–18 years were chosen. Subjects who required nonextraction orthodontic treatment were included in group I, and those who required all first premolar extractions for orthodontic treatment were included in group II. Baseline OHRQoL data (T0) were recorded before the start of treatment. To evaluate the impact of orthodontic treatment on OHRQoL, the Oral Health Impact Profile-14 (OHIP-14) questionnaire was presented to all subjects for retrospective evaluation at 1 month (T1), 3 months (T2), 6 months (T3) and 1 year (T4) after the start of orthodontic treatment and 1 week after completion of orthodontic treatment (T5).
Results
At T1 and T2, the physical pain and physical disability domains of OHIP-14 were impacted significantly by comprehensive orthodontic treatment in both groups (P < .001). The negative impact of orthodontic treatment on OHRQoL was maximum at T1 and then slowly recovered to the pretreatment level at T3 in both groups. Recovery of OHIP-14 scores was relatively faster in group I subjects compared to group II subjects. At T1 and T2, social disability and handicap domains were deteriorated significantly in group II subjects compared to group I subjects (P < .01).
Conclusions
The severity of OHRQoL deterioration was similar in both modalities of orthodontic treatment, but recovery from negative impacts was relatively slower in the first premolar extraction subjects.
Keywords: Orthodontic treatment, Nonextraction treatment, Extraction treatment, Quality of life, Adolescents
INTRODUCTION
Improvement of facial appearance and functional occlusion are the main objectives of orthodontic treatment. Awareness of how facial appearance affects quality of life (QoL) has rapidly increased the demand for orthodontic treatment.1 The motivating factors for undergoing orthodontic treatment are enhanced dental and facial esthetics and, consequently, minimized psychosocial problems, which contribute to QoL.2,3 Many studies4–7 have explored the physical, social, or psychological effects of orthodontic treatment and how discomfort and pain affect these aspects of QoL.4–7 It was found that depending on the phase of the treatment, orthodontic treatment may either compromise or improve oral health–related quality of life (OHRQoL).4–6
The impact of orthodontic treatment on OHRQoL usually decreases toward the end of orthodontic treatment.4–6 As the treatment of malocclusion has a large psychosocial component, it is necessary to use OHRQoL measures.6 The OHRQoL index provides insight into how individual oral health status affects overall QoL and how oral health care brings about improvements to patients' overall QoL.8,9 Thus, OHRQoL can be used as an important tool not only for the assessment, planning, and implementation of orthodontic treatment but also for the evaluation of orthodontic treatment outcomes.7
In orthodontics, tooth extraction has traditionally been highly debated, and the percentage of cases in which extraction occurs has displayed considerable variation throughout the years depending on treatment trends and other various factors. However, in contemporary orthodontics, nearly 30% of cases require premolar extractions for the management of malocclusion.10–12 It was found that tooth extraction significantly deteriorated the QoL in normal individuals.13 Thus, it is apparent that extraction of teeth for the correction of malocclusion will further deteriorate the QoL of an orthodontic patient. No previous studies evaluated the impact of tooth extraction on the OHRQoL among orthodontic patients. Thus, the present study was designed to evaluate the effect of orthodontic treatment with all first premolar extractions on the OHRQoL among adolescents undergoing comprehensive orthodontic treatment.
MATERIALS AND METHODS
The study was approved by the institutional review board (T/IM-F/Dental/15/10) (Institutional Ethics Committee, All India Institute of Medical Sciences, Bhubaneswar). A total of 68 healthy adolescents (male = 34, female = 34) in the age range of 12–18 years were chosen for this prospective cohort study. A sample size of 28 in each group was calculated based on following formula:
 |
where Zα = 1.96, Zβ = 0.84 (considering power at 80%), SD (standard deviation) = 4, number of groups = 2, and d = 3 (ie, clinically significant difference between two groups). However, considering the expected loss to follow-up as 20%, the final sample size was increased to 34 in each group.
Patients who had a perceived need for orthodontic treatment and had finished other dental therapy, such as restoration, impacted third molars, or endodontic or periodontal treatments, before the start of orthodontic treatment; those who could understand English properly; and those who had an Angle Class I malocclusion with a full complement of erupted teeth except for the third molars were included in the study. However, patients with known medical disorders or any cognitive disorders, those who had previously received any type of orthodontic treatment, those with any craniofacial anomalies or any untreated dental caries, those with poor periodontal health status or any impacted tooth, and those requiring extraoral anchorage for the management of their malocclusion were excluded from the study. After recruiting the patients in the study, a written informed consent form was completed. Patients who declined to participate in the study were excluded from the sample.
After selecting a subject for the study, all the orthodontic records were recorded and analyzed. The severity of the malocclusion and the need for orthodontic treatment were evaluated by the Dental Aesthetic Index (DAI).14 Based on the analysis of various orthodontic records, an extraction or nonextraction treatment plan for each subject was carried out. Subjects who required nonextraction orthodontic treatment were included in group I (control group; n = 34; males = 17, females = 17); and those who required all first premolar extractions for the treatment of their malocclusion were included in group II (study group; n = 34; males = 17, females = 17). Group I included subjects with Class I spacing or mild to moderate crowding, whereas all subjects with Class I bimaxillary protrusion with mild to moderate crowding or spacing were included in group II.
The OHRQoL for all subjects was assessed by the short-form Oral Health Impact Profile (OHIP-14).15 The baseline OHRQoL data (T0) were obtained before the start of comprehensive orthodontic treatment in all subjects. The OHRQoL questionnaire was given to the subjects and the questionnaire was filled out by the subjects within a 10-minute time frame. After recording the baseline data (T0), orthodontic appliances were placed in the group I subjects. In group II subjects, extraction of all first premolars was carried out first and then the orthodontic appliances were placed. In all subjects, standard edgewise orthodontic appliances (0.018-inch slot, Leone, Firenze, Italy) were used for the correction of their malocclusion. Anchorage in the first premolar extraction cases was managed with a Nance button and translingual arch (TLA) in the maxillary and mandibular arches, respectively. The maxillary and mandibular arches were aligned and leveled in both groups. In group II subjects, individual canine retraction was accomplished first by sliding mechanics, and then incisor retraction was done by loop mechanics on a continuous archwire. The anchorage devices were removed at the beginning of incisor retraction from both arches. The occlusion was finished with 0.017 × 0.025-inch stainless-steel wire in both groups. For the evaluation of the impact of orthodontic treatment on OHRQoL, the OHIP-14 questionnaire was presented to all of the subjects for retrospective evaluation of OHRQoL at 1 month (T1), 3 months (T2), 6 months (T3) and 1 year (T4) after the start of orthodontic treatment and 1 week after the completion of orthodontic treatment (T5). The response to each item was scored as follows: 0 = never, 1 = hardly ever, 2 = occasionally, 3 = fairly often, and 4 = very often. The OHIP-14 score was calculated by summing the response codes for the 14 items. Consequently, the total score ranged from 0 to 56, with higher scores indicating poorer OHRQoL.
Statistical Method
A master file was created, and the data were statistically analyzed on a computer with SPSS software version 17 (SPSS Inc, Chicago, IL, USA). The data were subjected to normality tests. Descriptive statistics were used. Friedman's analysis of variance and Wilcoxon signed rank tests were used for within-group comparisons. The Mann-Whitney U-test was used for between-group comparisons. A P-value of .05 was considered statistically significant.
RESULTS
The mean age of the subjects in groups I and II was 16.27 ± 1.40 years and 16.55 ± 1.76 years, respectively. The mean DAI score in group I and II subjects was 26.79 ± 2.05 and 27.40 ± 3.63, respectively. The mean duration between various time intervals of follow-up is described in Table 1. The mean total duration of treatment in group I and II subjects was 16.19 ± 3.49 months and 23.79 ± 3.02 months, respectively.
Table 1. .
Mean Age of the Subjects and Duration of Follow-Up Between Various Time Points of Evaluationa
| Groups |
Age, y Mean ± SD |
Duration Between Various Time Intervals of Follow-Up, mo |
||||
| T0-T1, Mean ± SD |
T0-T2, Mean ± SD |
T0-T3, Mean ± SD |
T0-T4, Mean ± SD |
T0-T5, Mean ± SD |
||
| I (nonextraction) | 16.27 ± 1.40 | 1.12 ± 0.12 | 2.99 ± 0.20 | 6.01 ± 0.37 | 12.40 ± 0.60 | 16.19 ± 3.49 |
| II (first premolar extraction) | 16.55 ± 1.76 | 1.10 ± 0.12 | 3.02 ± 0.28 | 6.01 ± 0.43 | 12.46 ± 0.44 | 23.79 ± 3.02 |
SD indicates standard deviation.
The details of the OHIP-14 scores in group I are described in Tables 2 and 3. The total OHIP-14 score was 5.91 ± 3.92 at T0 and increased significantly to 12.12 ± 6.16 and 8.03 ± 6.26 at T1 (P < .001) and T2 (P < .05), respectively. At T3, the total OHIP-14 score was 5.53 ± 4.38, which was not significantly different to that at T0, and then the score decreased significantly to 2.71 ± 2.50 and 0.76 ± 0.89 at T4 and T5, respectively (P < .001). There was 87.14% reduction in the total OHIP-14 score at the end of comprehensive orthodontic treatment (T5) compared to the pretreatment score (T0).
Table 2. .
Oral Health Impact Profile (OHIP) Scores in Group I (Nonextraction) Subjects at Various Time Intervals of Observationa
| Items |
OHIP Dimensions |
OHIP Scores at Various Time Intervals of Evaluation |
Significance (P-Value) |
|||||
| T0, Mean ± SD |
T1, Mean ± SD |
T2, Mean ± SD |
T3, Mean ± SD |
T4, Mean ± SD |
T5, Mean ± SD |
|||
| Domain 1: Functional limitations | ||||||||
| 1 | Had trouble in pronouncing words | 0.29 ± 0.63 | 0.82 ± 0.83 | 0.82 ± 0.83 | 0.26 ± 0.45 | 0.26 ± 0.45 | 0.00 ± 0.00 | .000*** |
| 2 | Felt that sense of taste had worsened | 0.00 ± 0.00 | 0.09 ± 0.29 | 0.00 ± 0.00 | 0.09 ± 0.29 | 0.09 ± 0.29 | 0.00 ± 0.00 | .065NS |
| Total (1 + 2) | 0.29 ± 0.63 | 0.91 ± 0.10 | 0.82 ± 0.83 | 0.35 ± 0.48 | 0.35 ± 0.65 | 0.00 ± 0.00 | .000*** | |
| Domain 2: Physical pain | ||||||||
| 3 | Had painful aching in your mouth | 0.09 ± 0.29 | 2.06 ± 0.92 | 1.71 ± 0.97 | 1.35 ± 0.48 | 0.35 ± 0.65 | 0.18 ± 0.39 | .000*** |
| 4 | Had uncomfortable when eating food | 0.09 ± 0.29 | 2.09 ± 0.79 | 1.41 ± 1.10 | 1.35 ± 0.80 | 0.71 ± 0.63 | 0.35 ± 0.65 | .000*** |
| Total (3 + 4) | 0.18 ± 0.58 | 3.88 ± 1.79 | 3.12 ± 1.83 | 2.71 ± 1.14 | 1.06 ± 1.03 | 0.53 ± 0.90 | .000*** | |
| Domain 3: Psychological discomfort | ||||||||
| 5 | Has been feeling self-conscious | 2.47 ± 1.31 | 2.65 ± 0.89 | 1.38 ± 1.56 | 0.85 ± 1.05 | 0.59 ± 0.82 | 0.21 ± 0.41 | .000*** |
| 6 | Had felt tense | 1.09 ± 1.24 | 0.74 ± 0.96 | 0.53 ± 0.90 | 0.26 ± 0.62 | 0.09 ± 0.29 | 0.00 ± 0.00 | .000*** |
| Total (5 + 6) | 3.56 ± 2.10 | 3.38 ± 1.67 | 1.82 ± 1.85 | 1.12 ± 1.45 | 0.68 ± 1.00 | 0.21 ± 0.41 | .000*** | |
| Domain 4: Physical disability | ||||||||
| 7 | Diet has been unsatisfactory | 0.18 ± 0.39 | 1.35 ± 0.65 | 0.71 ± 0.87 | 0.44 ± 0.50 | 0.44 ± 0.50 | 0.00 ± 0.00 | .000*** |
| 8 | Has had to interrupt meals | 0.00 ± 0.00 | 1.09 ± 0.51 | 0.74 ± 0.62 | 0.26 ± 0.45 | 0.18 ± 0.39 | 0.00 ± 0.00 | .000*** |
| Total (7 + 8) | 0.18 ± 0.39 | 2.44 ± 0.99 | 1.44 ± 1.38 | 0.71 ± 0.87 | 0.62 ± 0.78 | 0.00 ± 0.00 | .000*** | |
| Domain 5: Psychological disability | ||||||||
| 9 | Finds it difficult to relax | 0.09 ± 0.29 | 0.44 ± 0.66 | 0.34 ± 0.48 | 0.18 ± 0.39 | 0.00 ± 0.00 | 0.00 ± 0.00 | .000*** |
| 10 | Has been a bit embarrassed | 1.62 ± 1.23 | 1.41 ± 1.26 | 0.82 ± 0.94 | 0.56 ± 0.89 | 0.21 ± 0.41 | 0.09 ± 0.30 | .000*** |
| Total (9 + 10) | 1.71 ± 1.36 | 1.85 ± 1.28 | 1.18 ± 0.71 | 0.74 ± 1.14 | 0.21 ± 0.41 | 0.09 ± 0.30 | .000*** | |
| Domain 6: Social disability | ||||||||
| 11 | Has been irritable with other people | 0.09 ± 0.29 | 0.09 ± 0.29 | 0.18 ± 0.39 | 0.09 ± 0.30 | 0.00 ± 0.00 | 0.00 ± 0.00 | .050NS |
| 12 | Has had difficulty during usual jobs | 0.09 ± 0.29 | 0.00 ± 0.00 | 0.18 ± 0.39 | 0.09 ± 0.30 | 0.00 ± 0.00 | 0.00 ± 0.00 | .005** |
| Total (11 + 12) | 0.18 ± 0.58 | 0.09 ± 0.29 | 0.26 ± 0.62 | 0.26 ± 0.62 | 0.00 ± 0.00 | 0.00 ± 0.00 | .006** | |
| Domain 7: Handicap | ||||||||
| 13 | Has been life less satisfying | 0.09 ± 0.29 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | .010* |
| 14 | Has been totally unable to function | 0.09 ± 0.29 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | .010* |
| Total (13 + 14) | 0.18 ± 0.58 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | .010* | |
| Total OHIP-14 score | 5.91 ± 3.92 | 12.12 ± 6.16 | 8.03 ± 6.26 | 5.53 ± 4.38 | 2.71 ± 2.50 | 0.76 ± 0.89 | .000*** | |
SD indicates standard deviation; T0, baseline data; T1, 1 month after start of orthodontic treatment; T2, 3 months after start of orthodontic treatment; T3, 6 months after start of orthodontic treatment; T4, 1 year after start of orthodontic treatment; T5, 1 week after completion of orthodontic treatment; and NS, nonsignificant.
P < .05; ** P < .01; *** P < .001.
Table 3. .
Comparison of Oral Health Impact Profile Scores at Various Time Intervals of Observation in Group I (Nonextraction) Subjectsa
| Items |
T0-T1 |
T0-T2 |
T0-T3 |
T0-T4 |
T0-T5 |
T1-T2 |
T1-T3 |
T1-T4 |
T1-T5 |
T2-T3 |
T2-T4 |
T2-T5 |
T3-T4 |
T3-T5 |
T4-T5 |
| Domain 1: Functional limitations | |||||||||||||||
| 1 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| 2 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Total (1 + 2) | ** | * | NS | NS | * | NS | * | ** | *** | * | *** | *** | NS | ** | ** |
| Domain 2: Physical pain | |||||||||||||||
| 3 | *** | *** | *** | * | NS | ** | *** | *** | *** | * | *** | *** | *** | *** | * |
| 4 | *** | *** | *** | *** | * | ** | *** | *** | *** | NS | *** | *** | *** | *** | ** |
| Total (3 + 4) | *** | *** | *** | ** | NS | ** | ** | *** | *** | * | *** | *** | *** | *** | *** |
| Domain 3: Psychological discomfort | |||||||||||||||
| 5 | NS | ** | *** | *** | *** | *** | *** | *** | *** | ** | *** | *** | ** | ** | ** |
| 6 | * | * | ** | *** | *** | NS | ** | *** | *** | * | ** | ** | * | * | NS |
| Total (5 + 6) | NS | *** | *** | *** | *** | *** | *** | *** | *** | ** | *** | *** | ** | ** | ** |
| Domain 4: Physical disability | |||||||||||||||
| 7 | *** | ** | * | * | * | *** | *** | *** | *** | * | NS | *** | NS | *** | *** |
| 8 | *** | *** | ** | * | NS | ** | *** | *** | *** | ** | ** | *** | NS | ** | * |
| Total (7 + 8) | *** | *** | ** | * | NS | ** | *** | *** | *** | ** | ** | *** | NS | ** | * |
| Domain 5: Psychological disability | |||||||||||||||
| 9 | ** | * | NS | NS | NS | NS | ** | ** | ** | NS | ** | ** | * | * | NS |
| 10 | NS | ** | *** | *** | *** | ** | ** | *** | *** | * | *** | *** | ** | ** | * |
| Total (9 + 10) | NS | ** | ** | *** | *** | ** | *** | *** | *** | ** | *** | *** | ** | *** | * |
| Domain 6: Social disability | |||||||||||||||
| 11 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | * | * | NS | NS | NS |
| 12 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | * | * | NS | NS | NS |
| Total (11 + 12) | NS | NS | NS | NS | NS | NS | * | NS | NS | NS | * | * | * | * | NS |
| Doamin 7: Handicap | |||||||||||||||
| 13 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| 14 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Total (13 + 14) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Total OHIP-14 score | *** | * | NS | *** | *** | *** | *** | *** | *** | *** | *** | *** | *** | *** | *** |
T0 indicates baseline data; T1, 1 month after start of orthodontic treatment; T2, 3 months after start of orthodontic treatment; T3, 6 months after start of orthodontic treatment; T4, 1 year after start of orthodontic treatment; T5, 1 week after completion of orthodontic treatment; and NS, nonsignificant.
P < .05; ** P < .01; *** P < .001.
The details of the OHIP-14 scores in group II are described in Tables 4 and 5. The total OHIP-14 score was increased significantly from its pretreatment (T0) value of 7.71 ± 4.21 to 15.59 ± 5.78 at T1 and to 12.47 ± 6.28 at T2 (P < .001). At T3, although the total OHIP-14 score (8.12 ± 5.28) was greater compared to the T0 score (7.71 ± 4.21), the scores were not significantly different. The total OHIP-14 scores at T4 (P < .01) and T5 (P < .001) were 5.15 ± 4.17 and 1.50 ± 2.62, respectively, which were significantly less compared to the T0 value of 7.71 ± 4.21.
Table 4. .
Oral Health Impact Profile (OHIP) Scores in Group II (First Premolar Extraction) Subjects at Various Time Intervals of Observationa
| Items |
OHIP Dimensions |
OHIP Scores at Various Time Intervals of Evaluation |
Significance (P-Value) |
|||||
| T0, Mean ± SD |
T1, Mean ± SD |
T2, Mean ± SD |
T3, Mean ± SD |
T4, Mean ± SD |
T5, Mean ± SD |
|||
| Domain 1: Functional limitations | ||||||||
| 1 | Had trouble in pronouncing words | 0.21 ± 0.48 | 0.94 ± 0.98 | 0.76 ± 0.99 | 0.56 ± 0.75 | 0.47 ± 0.56 | 0.12 ± 0.33 | .000*** |
| 2 | Felt that sense of taste had worsened | 0.15 ± 0.36 | 0.26 ± 0.57 | 0.26 ± 0.57 | 0.06 ± 0.24 | 0.06 ± 0.24 | 0.06 ± 0.24 | .057NS |
| Total (1 + 2) | 0.35 ± 0.60 | 1.18 ± 1.24 | 1.00 ± 1.15 | 0.62 ± 0.85 | 0.53 ± 0.71 | 0.18 ± 0.46 | .000*** | |
| Domain 2: Physical pain | ||||||||
| 3 | Had painful aching in your mouth | 0.44 ± 0.61 | 2.12 ± 0.88 | 1.71 ± 0.90 | 1.24 ± 0.78 | 0.82 ± 0.80 | 0.15 ± 0.36 | .000*** |
| 4 | Had uncomfortable when eating food | 0.35 ± 0.69 | 2.29 ± 0.91 | 1.82 ± 0.94 | 1.15 ± 0.78 | 0.79 ± 0.60 | 0.21 ± 0.48 | .000*** |
| Total (3 + 4) | 0.82 ± 0.99 | 4.15 ± 1.57 | 3.41 ± 1.58 | 2.32 ± 1.30 | 1.62 ± 1.18 | 0.29 ± 0.67 | .000*** | |
| Domain 3: Psychological discomfort | ||||||||
| 5 | Has been feeling self-conscious | 2.32 ± 1.29 | 2.41 ± 1.23 | 1.19 ± 1.22 | 1.35 ± 1.15 | 0.85 ± 0.89 | 0.35 ± 0.59 | .000*** |
| 6 | Had felt tense | 0.85 ± 0.82 | 0.88 ± 1.01 | 0.71 ± 0.87 | 0.56 ± 0.78 | 0.21 ± 0.54 | 0.03 ± 0.17 | .000*** |
| Total (5 + 6) | 2.91 ± 1.78 | 3.29 ± 1.77 | 2.68 ± 1.79 | 2.09 ± 1.66 | 1.06 ± 1.25 | 0.38 ± 0.65 | .000*** | |
| Domain 4: Physical disability | ||||||||
| 7 | Diet has been unsatisfactory | 0.26 ± 0.57 | 1.59 ± 1.31 | 1.12 ± 1.01 | 0.71 ± 0.80 | 0.41 ± 0.61 | 0.09 ± 0.30 | .000*** |
| 8 | Has had to interrupt meals | 0.29 ± 0.68 | 1.21 ± 0.95 | 1.09 ± 0.90 | 0.59 ± 0.66 | 0.38 ± 0.55 | 0.06 ± 0.24 | .000*** |
| Total (7+ 8 ) | 0.56 ± 1.05 | 2.74 ± 1.90 | 2.21 ± 1.67 | 1.29 ± 1.35 | 0.79 ± 1.01 | 0.15 ± 0.44 | .000*** | |
| Domain 5: Psychological disability | ||||||||
| 9 | Finds it difficult to relax | 0.41 ± 0.78 | 0.71 ± 0.87 | 0.47 ± 0.66 | 0.29 ± 0.52 | 0.24 ± 0.43 | 0.06 ± 0.24 | .001** |
| 10 | Has been a bit embarrassed | 1.53 ± 1.08 | 1.71 ± 0.97 | 1.44 ± 1.05 | 1.03 ± 0.72 | 0.62 ± 0.65 | 0.26 ± 0.45 | .000*** |
| Total (9 + 10) | 1.79 ± 1.32 | 2.38 ± 1.26 | 1.94 ± 1.45 | 1.32 ± 0.95 | 0.82 ± 0.83 | 0.41 ± 0.70 | .000*** | |
| Domain 6: Social disability | ||||||||
| 11 | Has been irritable with other people | 0.35 ± 0.65 | 0.59 ± 0.82 | 0.53 ± 0.89 | 0.29 ± 0.63 | 0.12 ± 0.33 | 0.09 ± 0.30 | .000*** |
| 12 | Has had difficulty during usual jobs | 0.24 ± 0.55 | 0.38 ± 0.70 | 0.29 ± 0.52 | 0.21 ± 0.48 | 0.12 ± 0.33 | 0.03 ± 0.17 | .023* |
| Total (11 + 12) | 0.59 ±1.10 | 0.97 ± 1.19 | 0.79 ± 1.22 | 0.50 ± 0.82 | 0.24 ± 0.55 | 0.12 ± 0.41 | .000*** | |
| Doamin 7: Handicap | ||||||||
| 13 | Has been life less satisfying | 0.29 ± 0.63 | 0.21 ± 0.48 | 0.26 ± 0.51 | 0.18 ± 0.38 | 0.09 ± 0.29 | 0.03 ± 0.17 | .019* |
| 14 | Has been totally unable to function | 0.03 ± 0.17 | 0.12 ± 0.41 | 0.03 ± 0.17 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.03 ± 0.17 | .267NS |
| Total (13 + 14) | 0.32 ± 0.73 | 0.38 ± 0.89 | 0.29 ± 0.58 | 0.15 ± 0.36 | 0.09 ± 0.29 | 0.06 ± 0.34 | .009** | |
| Total OHIP-14 score | 7.71 ± 4.21 | 15.59 ± 5.78 | 12.47 ± 6.28 | 8.12 ± 5.28 | 5.15 ± 4.17 | 1.50 ± 2.62 | .000*** | |
SD indicates standard deviation; T0, baseline data; T1, 1 month after start of orthodontic treatment; T2, 3 months after start of orthodontic treatment; T3, 6 months after start of orthodontic treatment; T4, 1 year after start of orthodontic treatment; T5, 1 week after completion of orthodontic treatment; and NS, nonsignificant.
P < .05; ** P < .01; *** P < .001.
Table 5. .
Comparison of Oral Health Impact Profile Scores at Various Time Intervals of Observation in Group II (First Premolar Extraction) Subjectsa
| Items |
T0-T1 |
T0-T2 |
T0-T3 |
T0-T4 |
T0-T5 |
T1-T2 |
T1-T3 |
T1-T4 |
T1-T5 |
T2-T3 |
T2-T4 |
T2-T5 |
T3-T4 |
T3-T5 |
T4-T5 |
| Domain 1: Functional limitations | |||||||||||||||
| 1 | * | NS | NS | NS | NS | NS | NS | NS | NS | * | NS | NS | NS | NS | NS |
| 2 | * | NS | NS | NS | NS | NS | NS | NS | NS | * | NS | NS | NS | NS | NS |
| Total (1 + 2) | ** | ** | NS | NS | NS | NS | ** | ** | *** | * | ** | ** | NS | ** | * |
| Domain 2: Physical pain | |||||||||||||||
| 3 | *** | *** | *** | ** | ** | * | *** | *** | *** | ** | *** | *** | ** | *** | *** |
| 4 | *** | *** | *** | ** | NS | ** | *** | *** | *** | *** | *** | *** | ** | *** | *** |
| Total (3 + 4) | *** | *** | *** | ** | ** | ** | *** | *** | *** | *** | *** | *** | ** | *** | *** |
| Domain 3: Psychological discomfort | |||||||||||||||
| 5 | NS | * | ** | *** | *** | ** | *** | *** | *** | ** | *** | *** | ** | *** | ** |
| 6 | NS | * | * | ** | *** | NS | NS | *** | *** | NS | *** | *** | ** | ** | NS |
| Total (5 + 6) | * | NS | * | *** | *** | * | *** | *** | *** | ** | *** | *** | *** | *** | ** |
| Domain 4: Physical disability | |||||||||||||||
| 7 | *** | ** | * | NS | NS | ** | ** | *** | *** | ** | ** | *** | * | *** | ** |
| 8 | *** | ** | NS | NS | NS | NS | ** | *** | *** | ** | *** | *** | * | *** | ** |
| Total (7 + 8) | *** | *** | * | NS | NS | * | *** | *** | *** | ** | *** | *** | * | *** | ** |
| Domain 5: Psychological disability | |||||||||||||||
| 9 | * | NS | NS | NS | * | NS | * | ** | ** | NS | * | ** | NS | * | * |
| 10 | NS | NS | ** | *** | *** | NS | ** | *** | *** | * | *** | *** | *** | *** | ** |
| Total (9 + 10) | * | NS | NS | *** | *** | NS | *** | *** | *** | * | *** | *** | ** | *** | * |
| Domain 6: Social disability | |||||||||||||||
| 11 | * | NS | NS | * | * | NS | * | *** | ** | NS | ** | * | NS | NS | NS |
| 12 | NS | NS | NS | NS | NS | NS | NS | * | * | NS | NS | ** | NS | NS | NS |
| Total (11 + 12) | * | NS | NS | NS | * | NS | * | *** | ** | NS | * | ** | * | * | NS |
| Doamin 7: Handicap | |||||||||||||||
| 13 | NS | NS | NS | * | * | NS | NS | * | NS | NS | * | * | NS | NS | NS |
| 14 | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Total (13 + 14) | NS | NS | NS | * | NS | NS | NS | * | NS | NS | ** | NS | NS | NS | NS |
| Total OHIP-14 score | *** | *** | NS | ** | *** | *** | *** | *** | *** | *** | *** | *** | *** | *** | *** |
T0 indicates baseline data; T1, 1 month after start of orthodontic treatment; T2, 3 months after start of orthodontic treatment; T3, 6 months after start of orthodontic treatment; T4, 1 year after start of orthodontic treatment; T5, 1 week after completion of orthodontic treatment; and NS, nonsignificant.
P < .05; ** P < .01; *** P < .001.
The total OHIP-14 score was reduced 80.54% at T5 compared to T0.
The comparison of total OHIP-14 scores between groups I and II is described in Table 6 and Figure 1. The total OHIP-14 score at the beginning of treatment (T0) was 5.90 ± 3.92 and 7.71 ± 4.21 in groups I and II, respectively, and these scores were not significantly different (P = .112). At T1 and T2, the total OHIP-14 score in group II was significantly greater compared to that of group I subjects (P < .01). Also, at T3 and T4, the total OHIP-14 scores were significantly greater in group II subjects (P < .05). At T5, total OHIP-14 scores were not significantly different between the two groups (P = .363).
Table 6. .
Comparison of Various Oral Health Impact Profile (OHIP) Scores Between Groups I and II at Various Time Intervals of Observationa
| Items |
OHIP Dimensions |
Comparison of OHIP Scores Between Two Groups at Various Time Intervals of Evaluation |
|||||
| T0 | T1 | T2 | T3 | T4 | T5 | ||
| Gr. I vs Gr. II, Significance |
Gr. I vs Gr. II, Significance |
Gr. I vs Gr. II, Significance |
Gr. I vs Gr. II, Significance |
Gr. I vs Gr. II, Significance |
Gr. I vs Gr. II, Significance |
||
| Domain 1: Functional limitations | |||||||
| 1 | Had trouble in pronouncing words | .687NS | .734NS | .569NS | .113NS | .116NS | .041* |
| 2 | Felt that sense of taste had worsened | .021* | .157NS | .006** | .645NS | .645NS | .154NS |
| Total (1 + 2) | .486NS | .460NS | .754NS | .318NS | .189NS | .021* | |
| Domain 2: Physical pain | |||||||
| 3 | Had painful aching in your mouth | .004** | .613NS | .691NS | .723NS | .006** | .744NS |
| 4 | Had discomfort when eating food | .081NS | .414NS | .153NS | .348NS | .516NS | .346NS |
| Total (3 + 4) | .000*** | .439NS | .365NS | .293NS | .053NS | .307NS | |
| Domain 3: Psychological discomfort | |||||||
| 5 | Has been feeling self-conscious | .618NS | .467NS | .058NS | .070NS | .173NS | .345NS |
| 6 | Had felt tense | .716NS | .478NS | .284NS | .049* | .417NS | .317NS |
| Total (5 + 6) | .205NS | .881NS | .021* | .009** | .139NS | .317NS | |
| Domain 4: Physical disability | |||||||
| 7 | Diet has been unsatisfactory | .680NS | .348NS | .058NS | .236NS | .606NS | .079NS |
| 8 | Has had to interrupt meals | .011* | .832NS | .106NS | .031* | .093NS | .154NS |
| Total (7 + 8) | .169NS | .676NS | .057NS | .066NS | .623NS | .041* | |
| Domain 5: Psychological disability | |||||||
| 9 | Finds it difficult to relax | .046* | .223NS | .611NS | .357NS | .003** | .154NS |
| 10 | Has been a bit embarrassed | .686NS | .371NS | .010* | .003** | .004** | .058NS |
| Total (9 + 10) | .955NS | .167NS | .015* | .002** | .001** | .015* | |
| Domain 6: Social disability | |||||||
| 11 | Has been irritable with other people | .049* | .002** | .141NS | .097NS | .041* | .079NS |
| 12 | Has had difficulty during usual jobs | .260NS | .001** | .357NS | .273NS | .041* | .317NS |
| Total (11 + 12) | .024* | .000*** | .044* | .169NS | .011* | .079NS | |
| Doamin 7: Handicap | |||||||
| 13 | Has been life less satisfying | .148NS | .011* | .003** | .011* | .079NS | .317NS |
| 14 | Has been totally unable to function | .306NS | .079NS | .317NS | P = 1.000NS | P = 1.000NS | .317NS |
| Total (13 + 14) | .206NS | .006** | .003** | .021* | .079NS | .317NS | |
| Total score | .112NS | .009** | .001** | .039* | .019* | .363NS | |
Gr. indicates group; T0, baseline data; T1, 1 month after start of orthodontic treatment; T2, 3 months after start of orthodontic treatment; T3, 6 months after start of orthodontic treatment; T4, 1 year after start of orthodontic treatment; T5, 1 week after completion of orthodontic treatment; and NS, nonsignificant.
P < .05; ** P < .01; *** P < .001.
Figure 1.
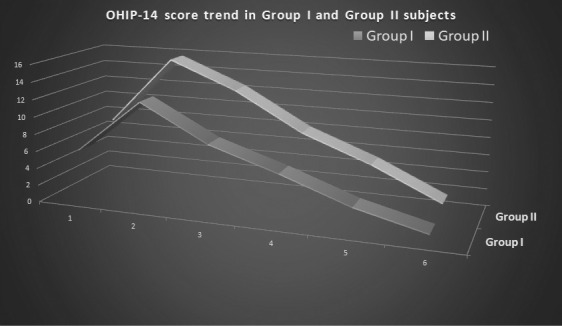
Comparison of total OHIP-14 score trends between group I (nonextraction) and group II (premolar extraction) subjects at various time intervals of observation.
DISCUSSION
Malocclusion has a significant negative impact on OHRQoL.16–18 Daily normal functions, emotional well-being, and interpersonal relationships are affected negatively by malocclusion.16,19,20 Correction of malocclusion leads to a significant improvement of OHRQoL.21–23 Better oral function, facial appearance, and dental esthetics following orthodontic treatment improve OHRQoL.16 Similar to the findings of many previous studies,18,21–23 significant improvements in OHRQoL were also observed at the end of orthodontic treatment in this study. In contrast to the present and previous studies,17,21,22 Taylor et al.23 reported no improvement in QoL by orthodontic treatment. In the current study, it was observed that all patients who underwent orthodontic treatment either by nonextraction or with first premolar extractions benefitted psychologically through improved facial and dental appearance and the associated increased self-confidence that resulted in improvement in OHRQoL.
There are many indices to evaluate the need for the orthodontic treatment. Patient-based assessment of oral health status is, however, considered a better tool to understand the patient's actual need and satisfaction with treatment.9 OHRQoL is the commonly used tool that includes subjective evaluation of physical, psychological, and social aspects of oral health. The child perception questionnaire (CPQ11–14) and short form of OHIP-14 are commonly used tools for the assessment of OHRQoL among children and adolescents. However, the OHIP-14 is a reliable and widely accepted assessment tool for the evaluation of OHRQoL in orthodontics.4
Wearing multibonded orthodontic appliances has a temporary negative impact on patients' QoL.5,24 The negative impacts are greater in females than in males.25 More than a two times deterioration of OHIP-14 score was observed in this study at the end of 1 month of treatment compared to pretreatment levels. In contrast to this observation, Feu et al.20 found 1.9 times higher OHIP-14 scores at the end of 1 year after the start of orthodontic treatment and a 60% reduction in the total score at the end of treatment. However, in the current study, 87.14% and 80.54% reductions of total OHIP-14 scores were observed in nonextraction and first premolar extraction subjects, respectively, at the end of orthodontic treatment. The functional limitations, physical pain, and physical disability domains deteriorated significantly during the first month of treatment in nonextraction subjects, whereas in the first premolar extraction subjects all domains except the handicap domain deteriorated during that period. Previous literature4,20,26 suggested that the psychological discomfort and psychological disability domains underwent maximum deterioration during comprehensive orthodontic treatment. Feu et al.20 reported that worsening of QoL during orthodontic treatment occurred as a result of functional limitations and physical pain. Paes da Silva et al.7 also observed that in adolescents, esthetics in combination with pain had a significant negative influence on OHRQoL.
In the current study, it was observed that painful aching in the mouth, discomfort with eating food, unsatisfactory diet, and the need to interrupt meals were the major reports in all patients following the start of comprehensive orthodontic treatment. It was also observed that all of these problems continued until 6 months of treatment and then started decreasing. Similarly, Zhang et al.27 also observed significant improvement in the quality of life 6 months after the start of comprehensive orthodontic treatment. However, in contrast to the current study, Chen et al.4 reported maximum deterioration of OHRQoL at 1 week after the start of comprehensive orthodontic treatment. In the current study, as treatment progressed, the total OHIP-14 score decreased in spite of deterioration of a few domains, such as physical pain and physical disability. The gradual decrease in symptoms could have been due to adaptation to treatment and correction of the malocclusion. The improvement of various OHRQoL symptoms was better in nonextraction subjects compared to first premolar extraction subjects. However, after 1 year of treatment in first premolar extraction subjects, the OHIP-14 score was reduced below the pretreatment score, and this could have been due to improvement in self-concept and reduction in negative social experience secondary to extraction space closure and correction of the malocclusion.
In nonextraction subjects, the psychological discomfort and psychological disability domains did not deteriorate following the start of treatment, but these two domains were affected significantly in first premolar extraction subjects. Reports of irritability with other people, difficulty in doing usual work, and a less satisfying life were frequent reports during the first month of orthodontic treatment in first premolar extraction subjects. This may have been due to the presence of extraction space in the first premolar extraction subjects. The deterioration of OHRQoL peaked at 1 month after the start of comprehensive orthodontic treatment in both groups and thereafter started decreasing and reached the pretreatment level at 6 months. However, in subjects with first premolar extractions, the recovery of OHRQoL was relatively slower at each observation point compared to results in the nonextraction subjects.
The results provided important knowledge for orthodontists, who could use these outcomes to inform patients prior to treatment that they may experience temporary deterioration in overall OHRQoL, specifically painful aching in the mouth, discomfort in eating food, unsatisfactory diet, and interruption in meals until 6 months following the placement of orthodontic appliances. Thereafter, patients were able to overcome the negative effects of treatment. The oral health impact reports may be relatively greater and last for a longer duration among subjects undergoing comprehensive orthodontic treatment with premolar extractions. These findings can also help orthodontists obtain better patient cooperation during treatment to achieve more acceptable treatment results.
CONCLUSIONS
Both nonextraction and first premolar extraction modalities of comprehensive orthodontic treatment had a temporary negative impact on OHRQoL.
The pattern of OHRQoL deterioration was similar in both nonextraction and first premolar extraction subjects.
The negative impacts of comprehensive orthodontic treatment on OHRQoL were greatest at 1 month after the start of comprehensive orthodontic treatment and continued until 6 months of treatment.
The functional limitations, physical pain, and physical disability domains deteriorated significantly in nonextraction subjects, whereas in first premolar extraction subjects, all domains except the handicap domain deteriorated during comprehensive orthodontic treatment.
Recovery from the negative impact was relatively slow in first premolar extraction subjects.
There were 87.14% and 80.54% reductions in total OHIP-14 scores in nonextraction and first premolar extraction subjects, respectively, at the end of comprehensive orthodontic treatment.
ACKNOWLEDGMENTS
We are thankful to Miss Puchu and Dr Anusuya for reading the manuscript for necessary English corrections.
REFERENCES
- 1.Othman SA, Mansor N, Saub R. Randomized controlled clinical trial of oral health-related quality of life in patients wearing conventional and self-ligating brackets. Korean J Orthod. 2014;44:168–176. doi: 10.4041/kjod.2014.44.4.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmidt A, Ciesielski R, Orthuber W, Koos B. Survey of oral health-related quality of life among skeletal malocclusion patients following orthodontic treatment and orthognathic surgery. J Orofac Orthop. 2013;74:287–294. doi: 10.1007/s00056-013-0151-2. [DOI] [PubMed] [Google Scholar]
- 3.Bellot-Arcís C, Montiel-Company JM, Almerich-Silla JM. Psychosocial impact of malocclusion in Spanish adolescents. Korean J Orthod. 2013;43:193–200. doi: 10.4041/kjod.2013.43.4.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen M, Da-Wei Wang, Wu Li-Ping. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M, McGrath C, Hagg U. Changes in oral health related quality of life during fixed orthodontic appliance therapy. Am J Orthod Dentofacial Orthop. 2008;133:25–29. doi: 10.1016/j.ajodo.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 6.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–27. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 7.Paes da Silva S, Pitchika V, Baumert U, et al. Oral health related quality of life in orthodontics: a cross sectional multicenter study on patients in orthodontic treatment. Eur J Orthod. 2019. Oct 12: Epub ahead of print. [DOI] [PubMed]
- 8.Williams KB, Gadbury-Amyot CC, Bray KK, Manne D, Collins P. Oral health-related quality of life: a model for dental hygiene. J Dent Hyg. 1998;72:19–26. [PubMed] [Google Scholar]
- 9.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–158. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor BM. Contemporary trends in orthodontic practice: a national survey. Am J Orthod Dentofacial Orthop. 1993;103:163–170. doi: 10.1016/S0889-5406(05)81766-4. [DOI] [PubMed] [Google Scholar]
- 11.Turpin DL. Percentage swings in extraction frequencies. Angle Orthod. 1994;64:403. doi: 10.1043/0003-3219(1994)064<0403:PSIEF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Konstantonis D, Anthopoulou C, Makou M. Extraction decision and identification of treatment predictors in Class I malocclusions. Prog Orthod. 2013;14:47–54. doi: 10.1186/2196-1042-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adeyemo WL, Taiwo OA, Oderinu O, Adeyemi MF, Ladeinde AL, Ogunlewe MO. Oral health-related quality of life following non-surgical (routine) tooth extraction: a pilot study. Contemp Clin Dent. 2012;3:427–432. doi: 10.4103/0976-237X.107433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jenny J, Cons NC. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Aust Dent J. 1996;41:43–46. doi: 10.1111/j.1834-7819.1996.tb05654.x. [DOI] [PubMed] [Google Scholar]
- 15.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 16.Demirovic K, Habibovic J, Dzemidzic V, Tiro A, Nakas E. Comparison of oral health related quality of life in treated and non-treated orthodontic patients. Med Arch. 2019;73:113–117. doi: 10.5455/medarh.2019.73.113-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grewal H, Sapawat P, Modi P, Aggarwal S. Psychological impact of orthodontic treatment on quality of life—a longitudinal study. Int Orthod. 2019;17:269–276. doi: 10.1016/j.ortho.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Olkun HK, Sayar G. Impact of orthodontic treatment complexity on oral-health related quality of life in Turkish patients. A prospective clinical study. Turk J Orthod. 2019;32:125–131. doi: 10.5152/TurkJOrthod.2019.18042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dimberg L, Arnrup K, Bondemark L. The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod. 2015;37:238–247. doi: 10.1093/ejo/cju046. [DOI] [PubMed] [Google Scholar]
- 20.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–898. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andiappan M, Gao W, Bernabe E, Kandala NB, Donaldson AN. Malocclusion, orthodontic treatment, and the Oral Health Impact Profile (OHIP-14): systematic review and meta-analysis. Angle Orthod. 2015;85:493–500. doi: 10.2319/051414-348.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Javidi H, Vettore M, Benson PE. Does orthodontic treatment before the age of 18 years improve the health-related quality of life? A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017;151:644–655. doi: 10.1016/j.ajodo.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 23.Taylor KR, Kiyak A, Huang GJ, Greenlee GM, Jolley CJ, King GJ. Effects of malocclusion and its treatment on the quality of life in adolescents. Am J Orthod Dentofacial Orthop. 2009;136:382–392. doi: 10.1016/j.ajodo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 24.Costa AA, Serra-Negra JM, Bendo CB, Pordeus IA, Paiva SM. Impact of wearing fixed orthodontic appliances on quality of life among adolescents: case-control study. Angle Orthod. 2016;86:121–126. doi: 10.2319/100514716.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corradi-Dias L, Paiva SM, Pretti H, Pordeus IA, Abreu LG. Impact of the onset of fixed appliance therapy on adolescents' quality of life using a specific condition questionnaire: a cross-sectional comparison between male and female individuals. J Orthod. 2019;46:195–204. doi: 10.1177/1465312519851220. [DOI] [PubMed] [Google Scholar]
- 26.Zheng DH, Wang XX, Su YR, et al. Assessing changes in quality of life using the Oral Health Impact Profile (OHIP) in patients with different classifications of malocclusion during comprehensive orthodontic treatment. BMC Oral Health. 2015;15:148. doi: 10.1186/s12903-015-0130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang M, McGrath C, Hagg U. Patients' expectations and experiences of fixed orthodontic appliances therapy. Impact on quality of life. Angle Orthod. 2007;77:318–322. doi: 10.2319/0003-3219(2007)077[0318:PEAEOF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]


