Abstract
Objective
To assess and compare the effects produced in the maxillary dental arch by means of Connecticut intrusion arch (CIA) with or without a cinch back on the distal end of the tube of the first molars.
Materials and Methods
This study included 44 patients with a mean age of 13.1 ± 1.8 years treated for deep bite with a CIA randomly divided into two groups: group 1 (G1), 22 patients with initial mean age of 12.72 ± 1.74 years treated with the CIA in the upper arch without a cinch back on the distal surface of the tube of the first molars, and group 2 (G2), 22 patients with an initial mean age of 13.67 ± 2.03 years treated with the CIA with a cinch back. Lateral cephalograms were available before treatment (T1) and after intrusion of maxillary incisors (T2). The mean treatment period was 5.5 ± 1.45 months. Intragroup and intergroup changes in the maxillary incisor and molar positions were analyzed by paired and independent t-tests associated with the Holm-Bonferroni correction method for multiple comparisons (P < .05).
Results
There were significant differences between groups in terms of maxillary incisor displacement. The maxillary incisors flared labially (2.17°) and proclined (1.68 mm) in group 1, whereas a palatal inclination (−1.99°) and retroclination (−1.13 mm) was observed in group 2. No significant differences were found for the molar positions between the groups.
Conclusions
The presence or absence of a distal bend in CIA affects incisor tipping and proclination during intrusion mechanics.
Keywords: Overbite, Intrusion arch, Biomechanics
INTRODUCTION
Deep bite is a common malocclusion for which treatment depends mainly on its etiology including mandibular and maxillary growth, altered lip and tongue function, and dentoalveolar development.1,2 Depending on diagnosis and treatment goals, overbite can be corrected by intrusion of maxillary and/or mandibular incisors, extrusion of the posterior segment, or a combination of both.3–7 In cases with increased vertical dimension,8 increased interlabial gap, and excess distance from the incisors to stomion point, incisor intrusion is indicated,9 which seems to be more stable mechanics in the long term.10,11
The intrusion of incisors can be performed with a variety of intrusion arches.3,9,12 The location of the point of force application in relation to the center of resistance (Cr) of the anterior segment involved in segmented intrusion mechanics with intrusion arches can change incisor axial tipping, which is not always desirable.6,8,12,13 A more anterior location of the point of force application causes flaring,2,6,8 whereas a more posterior location can produce uprighting of the anterior teeth.6 The Cr for all four normally positioned incisors is located in a region between the distal side of the canine14 and the distal side of the lateral incisor.15
To date, only one clinical trial6 investigated whether the application of an intrusive force passing near the Cr caused a change in the axial inclination of the anterior segment. That study found that intrusion of the incisors was accompanied by significant labial axial inclination (8.74°).
However, it is possible that not only the location at which the intrusion arch is attached to the incisors in relation to the Cr is important but also whether a distal bend was constructed at the distal aspect of the maxillary first molar tube in the intrusion arch, which can influence the magnitude of flaring of the maxillary incisors. No studies previously compared the possible influence of two different intrusion arch configurations on the biomechanical outcomes of incisor intrusion. Thus, the purpose of this study was to analyze and compare the effects of a distal bend made in the Connecticut intrusion arch (CIA) on both anterior and posterior maxillary tooth movements.
MATERIALS AND METHODS
This prospective study was approved by the institution review board of the University of North Paraná (UNOPAR), Londrina, Paraná, Brazil. Patients and guardians were fully informed about the study and its implications and written consent was obtained.
The Strengthening the Reporting of Observational Studies in Epidemiology statement guidelines for observational studies were followed. The clinical trial was conducted from March 2014 to September 2018. Sample size estimation was based on a statistical significance level of 5% (α) and a β value of 0.2 to achieve a minimum of 80% probability of detecting a mean difference of 1.4 mm between groups for the amount of flaring of the maxillary incisor as the major outcome variable with a standard deviation (SD) set at 1.5 mm.6 A minimum of 22 patients was required in each group.
As shown by the study flowchart (Figure 1), 60 patients with deep bites were initially enrolled. From 60 patients, 10 were excluded because of not meeting the following inclusion criteria: age between 10 and 15 years, presence of at least first molars and fully erupted permanent maxillary central and lateral incisors, no history of previous orthodontic treatment, normal facial growth pattern, class I or mild class II molar relationship, with normal incisor axial inclination (within 2 SD) and overbite greater than 5 mm. In addition, patients with significant crowding in the upper arch (>3 mm), crossbite in the posterior and/or anterior regions, tooth agenesis (except for third molars), or severe class II malocclusion or with extremely flared or retroclined maxillary incisors were excluded. The remaining 50 patients were randomly divided into two equal groups of 25 each: group 1 (G1) patients were treated with the CIA in the upper arch without a cinch back on the distal surface of the tube of the first molars (Figure 2), and group 2 (G2) patients were treated with the CIA with a cinch back bilaterally (Figure 3). However, 6 patients were lost during the study to follow-up (3 patients had excessive breakage of appliance and 3 moved to another city). A total of 44 patients remained until the end of the study. Therefore, G1 comprised 22 patients: 10 females and 12 males with an initial mean age of 12.72 ± 1.74 years. G2 comprised 22 patients: 12 females and 10 males with an initial mean age of 13.67 ± 2.03 years. Both groups were treated by one researcher until the overbite was fully corrected, for a mean treatment period of 5.5 ± 1.45 months.
Figure 1.
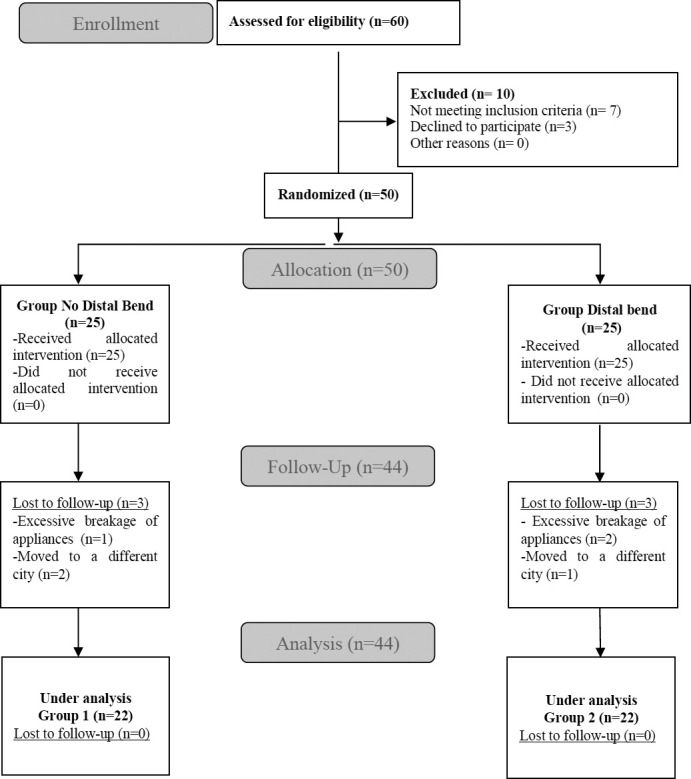
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
Figure 2.
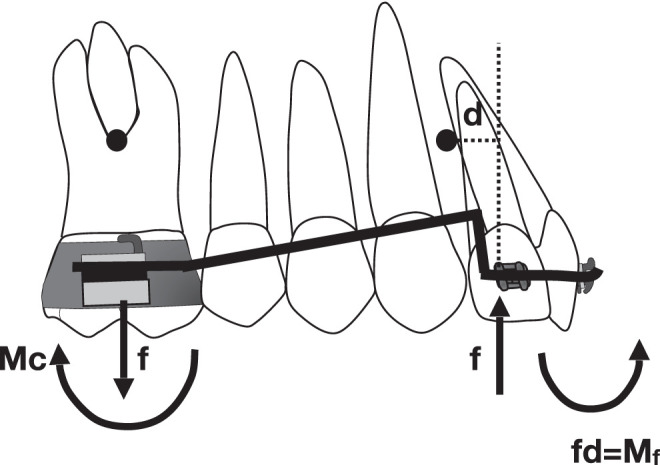
Intrusion arch without a cinch back at the molar tube and the force system.
Figure 3.
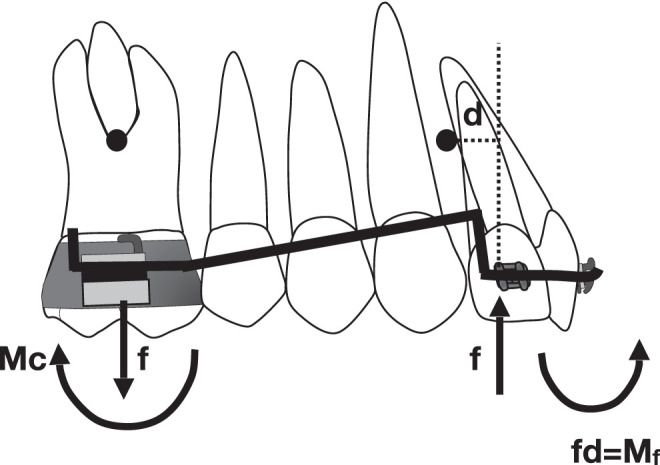
Intrusion arch with a cinch back at the molar tube and the force system.
Intrusion Mechanics and Guidelines
All patients received a 2 × 4 appliance bonded to the maxillary incisors with 0.022 × 0.028-inch slot conventional brackets, Roth prescription (3M Unitek, Monrovia, Calif). Bands were cemented to the maxillary first molars with triple tubes. A passive, transpalatal bar for anchorage was adapted to the first molars.
All patients were treated during the leveling and alignment protocol with the same sequence of archwire beginning with 0.016 × 0.016-inch heat-activated nickel-titanium, followed by a 0.019 × 0.025-inch stainless-steel archwire. Subsequently, a 0.017 × 0.025-inch CIA (Ultimate Wireforms Inc, Bristol, Conn) was placed in the maxillary first molar auxiliary tubes and tied anteriorly over the distal wings of the maxillary lateral incisor brackets secured by a metal ligature. The CIA was tied over a 0.016 × 0.022 nickel-titanium (NiTi) anterior segment. After the complete leveling and alignment of the incisors, the CIA was tied over a 0.019 × 0.025 stainless steel (SS). The position of the V bend was 3–5 mm mesial to the maxillary molars. The CIA was made of nickel titanium with a V bend calibrated to deliver an intrusive force of approximately 40–60 g.12,16,17
Lateral Cephalometric Analysis
Digitized radiographs were traced with the aid of Dolphin Imaging software (version 11.7, Dolphin Imaging and Management Solutions, Chatsworth, Calif). Lateral cephalometric radiographs were obtained from all patients at two time points: before beginning treatment (T1) and when intrusion was completed (T2).
The following measurement protocol was adopted: two reference axes were constructed (x = horizontal reference line passing from anterior nasal spine [ANS] to the posterior nasal spine [PNS]; y = vertical reference line perpendicular to the x axis passing through Sella), and nine variables were identified. The linear and angular measurements for evaluating the molar and incisor changes are summarized in Figure 4.
Figure 4.
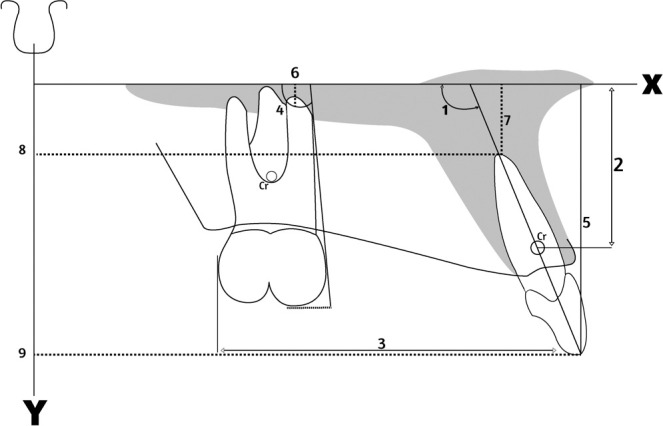
Cephalometric diagram used for cephalogram measurements. The centroid (Cr) point was a constructed point 15 mm from the incisal edge along the long axis of the maxillary incisor. 1 = U1 angle to X: angulation of maxillary central incisor to X-axis; 2 = U1cr to X (linear distance of maxillary incisor centroid to x axis); 3 = U1 tip to U6D (linear distance of maxillary incisor tip to maxillary first molar distal aspect, perpendicular to x axis); 4 = U6 to X: angle of a line perpendicular to maxillary first molar mesial surface to x axis); 5 = U1 tip to X (linear distance between maxillary incisor tip to x axis perpendicularly); 6 = U6 apex to X (distance of maxillary first molar mesialbuccal root apex to x axis); 7 = U1 apex to X (distance of maxillary incisor apex to x axis); 8 = U1 apex to Y (distance of maxillary incisor apex to y axis); 9 = U1 tip to Y (distance of maxillary incisor edge to y axis). X indicates horizontal reference line passing from the ANS to the PNS; Y, vertical reference line perpendicular to the x axis passing through sella turcica. U1, maxillary central incisor; U1cr, centroid point of maxillary central incisor; U6, maxillary first molar; U6D, distal aspect of maxillary first molar.
Statistical Analysis
Data were described by means and SDs. The Kolmogorov-Smirnov test revealed a normal distribution of data; parametric tests were employed for analyses. To compare patients' sex distribution between groups, Fisher's exact test was used (Table 1). An unpaired t-test was used to compare age distribution between groups (Table 2). For comparison of differences between both groups at T1 (Table 3) and intergroup changes (Table 4), t-tests were used. P-values were obtained by Holm-Bonferroni correction for multiple comparisons. Significance level was set at 5%. All statistical procedures were performed with the aid of Statistica 5.0 software (StatSoft Inc., Tulsa, Okla).
Table 1. .
Description and Comparison of Gender Composition Between Groupsa
| Group |
Female |
Male |
Total |
||
| n |
% |
n |
% |
||
| 1 (N = 22) | 10 | 45.5 | 12 | 54.5 | 22 |
| 2 (N = 22) | 12 | 54.5 | 10 | 45.5 | 22 |
Fisher test: P = .763 not significant.
Table 2. .
Description and Comparison of Age Between Groups at T1a
| Group 1 (N = 22) |
Group 2 (N = 22) |
Difference |
P |
|||
| Mean |
SD |
Mean |
SD |
|||
| Age | 12.72 | 1.74 | 13.67 | 2.03 | 0.95 | .100 NSb |
NS indicates not significant; SD, standard deviation; T1, before treatment.
Unpaired t-test.
Table 3. .
Mean Cephalometric Differences Between Groups at T1a
| Variable |
Group 1 (N = 22), No Cinched Back |
Group 2 (N = 22), Cinched Back |
Difference |
P Value |
P Critical |
||
| Mean |
SD |
Mean |
SD |
||||
| U1 to X (°) | 111.65 | 7.98 | 109.65 | 7.17 | −2.01 | .730 | .025 |
| U1cr to X (mm) | 11.56 | 2.57 | 10.91 | 2.35 | −0.65 | .302 | .010 |
| U1 tip to U6D (mm) | 40.11 | 3.46 | 39.88 | 3.29 | −0.23 | .837 | .050 |
| U6 to X (°) | −87.13 | 6.59 | −86.31 | 5.21 | 0.83 | .719 | .017 |
| U1 tip to X (mm) | 26.31 | 2.96 | 25.76 | 2.62 | −0.55 | .275 | .008 |
| U6 apex to X (mm) | 1.49 | 1.59 | 2.06 | 2.93 | 0.57 | .465 | .013 |
| U1 apex to X (mm) | 3.25 | 2.45 | 2.77 | 2.13 | −0.48 | .183 | .007 |
| U1 apex to Y (mm) | 53.63 | 5.16 | 53.40 | 3.15 | −0.23 | .850 | .043 |
| U1 tip to Y (mm) | 61.90 | 6.05 | 62.72 | 4.20 | −0.82 | .057 | .013 |
SD indicates standard deviation; T1, before treatment; U1, maxillary central incisor; U1cr, centroid point of maxillary central incisor; U6, maxillary first molar; U6D, distal aspect of maxillary first molar.
Table 4. .
Mean Cephalometric Changes From T1 to T2 Between Groupsa
| Variable |
Group 1 (N = 22), No Cinched Back |
Group 2 (N = 22), Cinched Back |
Difference |
P Value |
P Critical |
||
| Mean |
SD |
Mean |
SD |
||||
| U1 to X (°) | 2.17 | 2.82 | −1.99 | 2.39 | −4.17 | <.001* | .006 |
| U1cr to X (mm) | −2.09 | 1.44 | −2.23 | 0.94 | −0.14 | .896 | .050 |
| U1 tip to U6D (mm) | −0.58 | 1.89 | −1.42 | 1.51 | −0.84 | .257 | .010 |
| U6 to X (°) | 7.21 | 6.28 | 6.75 | 7.19 | −0.46 | .858 | .025 |
| U1 tip to X (mm) | −1.29 | 1.21 | −0.48 | 1.37 | 0.81 | .642 | .017 |
| U6 apex to X (mm) | 1.10 | 1.26 | 0.46 | 1.31 | −0.64 | .033 | .008 |
| U1 apex to X (mm) | −2.16 | 1.29 | −2.88 | 1.43 | −0.72 | .493 | .013 |
| U1 apex to Y (mm) | −3.50 | 1.90 | 1.09 | 1.65 | 4.59 | .060 | .009 |
| U1 tip to Y (mm) | 1.68 | 1.72 | −1.13 | 2.12 | −2.81 | .000* | .007 |
SD indicates standard deviation; T1, before treatment; T2, after intrusion of maxillary incisors; U1, maxillary central incisor; U1cr, centroid point of maxillary central incisor; U6, maxillary first molar; U6D, distal aspect of maxillary first molar.
P < .05.
Error of the Method
Thirty days after the first evaluation, 50% of the lateral cephalometric radiographs were randomly selected, and the respective measurements were repeated to determine intraexaminer errors by means of a paired t-test and the Dahlberg test. Intraexaminer agreement was excellent. Random error averaged less than 1.8° and 0.8 mm for the angular and linear measurements, respectively. Interexaminer reliability was assessed with the intraclass correlation coefficient. The intraclass correlation coefficient ranged from 0.61 to 0.99, showing good to excellent reliability between raters.
RESULTS
The groups were comparable at T1 regarding sex distribution, initial age, and cephalometric variables (Tables 1 to 3).
Table 4 shows that no significant differences were found between the groups for most variables. Of nine measurements, two showed a statistically significant difference between groups. An increase of the mean axial inclination of the maxillary incisors occurred for the G1 patients (2.17° ± 2.82°). Conversely, lingual inclination of the maxillary incisors (−1.99° ± 2.39°) was observed in the G2 patients. Also, a proclination of 1.68 ± 1.72 mm occurred in the G1 patients. However, a retroclination of −1.13 ± 2.12 mm was seen in the G2 patients.
No significant difference was found between groups in the amount of intrusion achieved measured at the centroid of the maxillary incisors. The G1 patients experienced mean intrusion of 2.09 ± 1.44 mm, whereas the G2 patients showed a mean intrusion of 2.23 ± 1.44 mm. The distance between the maxillary incisor tip and maxillary first molar distal surface did not show statistical difference between the groups. Distal crown tipping of the maxillary first molar was attained in both groups (G1, 7.21° ± 6.28°; G2, 6.75° ± 7.19°). Vertically, the incisal edge of the maxillary incisors intruded by −1.29 ± 1.21 mm in the G1 patients and −0.48 ± 1.37 mm in the G2 patients. Molar extrusion was observed in both groups (G1, 1.10 ± 1.26 mm; G2, 0.46 ± 1.31 mm). The maxillary incisor apex intruded by −2.16 ± 1.29 mm in the G1 patients and −2.88 ± 1.43 mm in the G2 patients. The incisor root apex moved lingually by −3.50 ± 1.90 mm in the G1 patients and moved labially 1.09 ± 1.65 mm in the G2 patients.
DISCUSSION
The main objective of this randomized prospective study was to quantify the amount of anteroposterior and vertical maxillary incisor and molar movements in deep bite patients treated with the CIA in two different configurations. Different methods aimed at incisor intrusion have appeared in the literature.8,11,17–24 Previous intrusion arch studies have used segmented mechanics for intrusion of anterior teeth.4,8,17 However, there is variation in the literature regarding dental arch segmentation, particularly in terms of the number of teeth in the posterior region involved, with possibilities including molars and premolars,6,11 molars, premolars and canines,2,11,16,17 or first molars only.3,13 Regarding the side effects in the posterior anchorage unit, it has been acknowledged that there was a significant clockwise moment generated on maxillary molars during intrusion of incisors, which results in both a tendency toward extrusion8,19,24 and distal crown tipping.6,7,13,19,21 It has been shown that a transpalatal bar12 can be used to help minimize the anchorage unit side effects.
It is well known that intrusion arches can change the maxillary incisor axial inclination by altering the point of force application in relation to the Cr of the anterior segment. An interesting study6 investigated whether the application of an intrusive force by an intrusion arch tied to the distal wings of the lateral incisor brackets caused a change in the axial inclination of the anterior segment. Surprisingly, they found that the mean incisor axial inclination increased a statistically significant 8.74°. This could increase the amount of overjet and worsen a class II malocclusion, although the authors tied their one-piece intrusion arch near the Cr of the maxillary incisors.6
The rationale of cinching the end of the CIA tightly was that it seemed to prevent flaring of the incisors in a clinical situation where maxillary incisor labial movement was not desired.12 In the current study, it was found that the G1 incisors showed a mean labial tipping of 2.17°. Conversely, palatal tipping of the maxillary incisors of −1.99° occurred in the G2 patients, when a distal bend cinch back was added to the CIA. Similarly, labial movement of the incisor tip by 1.68 mm was observed in the G1 patients, whereas palatal movement of −1.13 mm occurred for the G2 patients. The increased angular change of the incisors obtained in this study in the G1 patients was also observed in another study using a CIA,19 where the authors observed that maxillary incisors flared labially 0.4 mm with 3.31° of labial tipping.
Thus, the current study suggested that performing a cinch back to the CIA not only successfully prevented labial movement of the incisors but also caused lingual tipping of these teeth as a result of the clockwise moment of the force expressed. The most likely explanation for this finding was that, as the first molars rotated distally in the G2 patients (distal tipping 6.75°), the maxillary incisors accompanied the distal movement of the molars. On the basis of these findings, in a clinical situation where maxillary incisor intrusion is desired and the incisor axial inclination can be increased such as in a class II division 2 patient, a one-piece intrusion arch without a cinch back bend is preferred. Then, the wire will slide forward through the molar tube as the incisors flare. On the other hand, in a class II division 1 patient, when incisors are already flared and an intrusion is needed, then the CIA should have its end cinched back to prevent more incisor flaring.
Regarding the genuine amount of intrusion achieved, G1 incisors intruded a mean of 2.09 mm, whereas G2 mean intrusion was 2.23 mm. Despite no statistically significant differences between the groups in the amount of intrusion, the incisors tipped labially in the G1 patients, creating “uncontrolled tipping.”25 Similar amounts of intrusion were found in other studies: 2.23 mm17 and 2.20 mm.26
The amount of flaring of the maxillary incisor in combination with distal tipping of the molar was not significantly different between the groups (Figure 4, measure 3): G1 patients showed a mean decrease of 0.58 mm, whereas G2 patients showed a mean decrease of 1.42 mm, which can be explained by increased lingual tipping of the incisors observed in the G2 patients.
Angular movement of the first molars resulting from the clockwise moment produced by the CIA was similar between the groups. In the G1 patients, there was 7.21° distal crown tipping, whereas 6.75° was seen in the G2 patients. The amount of angular displacement of the maxillary first molar was similar to that reported in another study (6.65°).19 Based on these findings, cinching a CIA distal to the molar tubes does not seem to prevent distal tipping of the maxillary first molar. Molar extrusion in the G1 patients was a mean of 1.10 mm, whereas the G2 patients presented mean extrusion of 0.46 mm, with no significant difference. This was similar to another study.19 One limitation of the current study was that measurements of molar position were not performed using a jig inserted in the molar tube, which could have accurately differentiated between the left and right molars.
This study provided evidence regarding the incisor and molar movements attained during incisor intrusion mechanics. The evidence supported that the use of a CIA cinched distal to the molar tube during intrusion mechanics was indicated in cases where the desired effect was to inhibit labial incisor tipping and proclination. It can be concluded that the distal bend made at the end of an intrusion arch is clinically relevant but should be used according to the maxillary incisor initial inclination and treatment goals.
CONCLUSIONS
Maxillary incisor intrusion aimed at overbite correction was achieved with the CIA successfully in both groups.
An intrusion arch inserted in the auxiliary molar tube with no cinch back produced significant labial tipping and proclination of the maxillary incisors.
The use of CIA with a cinch back at its distal end minimized labial movement of the maxillary incisors and also provided retroclination of those teeth.
REFERENCES
- 1.Burstone CJ, van Steenbergen E, Hanley KJ. Modern Edgewise Mechanics and the Segmented Arch Technique. Farmington, CT: University of Connecticut; 1995. [Google Scholar]
- 2.Nielsen IL. Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment. Angle Orthod. 1991;61:247–260. doi: 10.1043/0003-3219(1991)061<0247:VMEDDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Ricketts R. Bioprogressive therapy as an answer to orthodontic needs. Part II. Am J Orthod. 1976;70:359–397. doi: 10.1016/0002-9416(76)90111-1. [DOI] [PubMed] [Google Scholar]
- 4.Nanda R. Correction of deep overbite in adults. Dent Clin North Am. 1997;41:67–87. [PubMed] [Google Scholar]
- 5.Melsen B, Agerbaek N, Markenstam G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop. 1989;96:232–241. doi: 10.1016/0889-5406(89)90460-5. [DOI] [PubMed] [Google Scholar]
- 6.van Steenbergen E, Burstone CJ, Prahl-Andersen B, Aartman IHA. The relation between the point of force application and flaring of the anterior segment. Angle Orthod. 2005;75:730–735. doi: 10.1043/0003-3219(2005)75[730:TRBTPO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Almeida MR, Vieira GM, Guimarães CH, Amad Neto M, Nanda R. Biomechanics in Orthodontics: smart archwires. Dental Press J Orthod. 2006;11:122–156. [Google Scholar]
- 8.Greig DGM. Bioprogressive therapy: overbite reduction with the lower utility arch. Br J Orthod. 1983;10:214–216. doi: 10.1179/bjo.10.4.214. [DOI] [PubMed] [Google Scholar]
- 9.Burstone CJ, Goldberg AJ. Beta titanium: a new orthodontic alloy. Am J Orthod. 1980;77:121–132. doi: 10.1016/0002-9416(80)90001-9. [DOI] [PubMed] [Google Scholar]
- 10.Burstone CJ. The mechanical of the segmented arch technique. Angle Orthod. 1966;36:99–120. doi: 10.1043/0003-3219(1966)036<0099:TMOTSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Nanda R. The differential diagnosis and treatment of excessive overbite. Dental Clin North Am. 1981;25:69–84. [PubMed] [Google Scholar]
- 12.Nanda R. Biomechanics and Esthetic Strategies in Clinical Orthodontics 1st ed. St. Louis, MO: Elsevier/Saunders; 2005. [Google Scholar]
- 13.Schwertner A, Almeida RR, Gonini A, Almeida MR. Photoelastic analysis of stress generated by Connecticut intrusion arch (CIA) Dental Press J Orthod. 2017;22:57–64. doi: 10.1590/2177-6709.22.1.057-064.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vanden Bulcke M, Sachdeva R, Burstone CJ. The center of resistance of anterior teeth during intrusion using the laser reflection technique and holographic interferometry. Am J Orthod. 1986;90:211–219. doi: 10.1016/0889-5406(86)90068-5. [DOI] [PubMed] [Google Scholar]
- 15.Dermaut LR, Vanden Bulcke MM. Evaluation of intrusive mechanics of the type ‘‘segmented arch'' on a macerated human skull using the laser reflection technique and holographic interferometry. Am J Orthod Dentofacial Orthop. 1986;89:251–263. doi: 10.1016/0002-9416(86)90041-2. [DOI] [PubMed] [Google Scholar]
- 16.Burstone CJ. Deep overbite correction by intrusion. Am J Orthod. 1977;72:1–22. doi: 10.1016/0002-9416(77)90121-x. [DOI] [PubMed] [Google Scholar]
- 17.Almeida MR, Marçal ASB, Fernandes TMF, Vasconcelos BJ, Almeida RR, Nanda R. A comparative study of the effect of the intrusion arch and straight wire mechanics on incisor root resorption: a randomized, controlled trial. Angle Orthod. 2018;88:20–26. doi: 10.2319/06417-424R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oyama K, Motoyoshi M, Hirabayashi M, Hosoi K, Shimizu N. Effects of root morphology on stress distribution at the root apex. Eur J Orthod. 2007;29:113–117. doi: 10.1093/ejo/cjl043. [DOI] [PubMed] [Google Scholar]
- 19.Janakiraman N, Gill P, Upadhyay M, Nanda R, Uribe F. Response of the maxillary dentition to a statically determinate one-couple system with tip-back mechanics: a prospective clinical trial. Angle Orthod. 2016;86:32–38. doi: 10.2319/012815-68.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng J, Major PW, Heo G, Flores-Mir C. True incisor intrusion attained during orthodontic treatment: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2005;128:212–219. doi: 10.1016/j.ajodo.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 21.Sifakakis I, Pandis N, Makou M, Eliades T, Bourauel C. Forces and moments generated with various incisor intrusion systems on maxillary and mandibulary anterior teeth. Angle Orthod. 2009;79:928–933. doi: 10.2319/120908-622.1. [DOI] [PubMed] [Google Scholar]
- 22.Vanden Bulcke MM, Burstone CJ, Sachedeva R, Dermaut LR. Location of the centers of resistence for anterior teeth during retraction using the laser reflection technique. Am J Orthod Dentofacial Orthop. 1987;9:375–384. doi: 10.1016/0889-5406(87)90390-8. [DOI] [PubMed] [Google Scholar]
- 23.Uribe F, Nanda R. Treatment of class II division 2 malocclusion in adults: biomechanical considerations. J Clin Orthod. 2003;37:599–606. [PubMed] [Google Scholar]
- 24.van Steenbergen E, Burstone CJ, Prahl-Andersen B, Aartman IH. The role of a high pull headgear in counteracting side effects from intrusion of the maxillary anterior segment. Angle Orthod. 2004;74:480–486. doi: 10.1043/0003-3219(2004)074<0480:TROAHP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Isaacson RJ, Lindauer SJ, Rubenstein LK. Moments with the edgewise appliance: incisor torque control. Am J Orthod Dentofacial Orthop. 1993;103:428–438. doi: 10.1016/S0889-5406(05)81793-7. [DOI] [PubMed] [Google Scholar]
- 26.Senısık NE, Türkkahraman H. Treatment effects of intrusion arches and mini-implant systems in deepbite patients. Am J Orthod Dentofacial Orthop. 2012;141:723–733. doi: 10.1016/j.ajodo.2011.12.024. [DOI] [PubMed] [Google Scholar]


