Abstract
Objectives
To provide a comprehensive summary of the implications of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and coronavirus disease 2019 (COVID-19) on orthodontic treatment, contingency management, and provision of emergency orthodontic treatment, using currently available data and literature.
Materials and Methods
Orthodontically relevant sources of information were searched using electronic databases including PubMed and Google Scholar and current reports from major health bodies such as Centers for Disease Control and Prevention, World Health Organization, National Institutes of Health, and major national orthodontic associations.
Results
Where available, peer-reviewed and more recent publications were given priority. Due to the rapidly evolving nature of COVID-19 and limitations in quality of evidence, a narrative synthesis was undertaken. Relevant to orthodontics, human-to human transmission of SARS-CoV-2 occurs predominantly through the respiratory tract via droplets, secretions (cough, sneeze), and or direct contact, where the virus enters the mucous membrane of the mouth, nose, and eyes. The virus can remain stable for days on plastic and stainless steel. Most infected persons experience a mild form of disease, but those with advanced age or underlying comorbidities may suffer severe respiratory and multiorgan complications.
Conclusions
During the spread of the COVID-19 pandemic, elective orthodontic treatment should be suspended and resumed only when permitted by federal, provincial, and local health regulatory authorities. Emergency orthodontic treatment can be provided by following a contingency plan founded on effective communication and triage. Treatment advice should be delivered remotely first when possible, and where necessary, in-person treatment can be performed in a well-prepared operatory following the necessary precautions and infection prevention and control (IPAC) protocol.
Keywords: COVID-19, SARS-CoV-2, Orthodontics, Dentistry, Orthodontic emergency
INTRODUCTION
Since the beginning of 2020, coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; first named as the 2019-novel coronavirus or 2019-nCoV) has rapidly spread throughout the inhabited world and led to unprecedented major health, humanitarian, and financial crises. Efforts to contain the spread of the disease have led to major disruptions, forcing regional and, in many cases, national emergencies and lockdowns, leaving only essential services to continue. In many such efforts, performing elective tasks, including orthodontic treatment, are required to be suspended on orders of the federal, provincial/state, and local civic and public health or professional regulatory bodies. Since orthodontic treatment is a long and continuous process, there are millions of patients who were already undergoing orthodontic treatment when scheduled care was abruptly suspended. Due to the unprecedented nature of this pandemic and the unknown length of time that mandatory suspension of elective treatment may be in effect in different regions, consolidated information and guidelines for the clinical orthodontic management of patients during the COVID-19 pandemic are lacking. The aim of this review was to provide a comprehensive summary of the implications of SARS-CoV-2 and COVID-19 on orthodontic treatment and to discuss the contingency management and provision of emergency orthodontic care, using currently available data and literature.
MATERIALS AND METHODS
To ensure that all relevant information regarding the rapidly evolving COVID-19 pandemic and any orthodontic implications were obtained, a wide selection of sources were searched and summarized. These sources included peer-reviewed literature publications from electronic databases such as PubMed and Google Scholar using the following search terms: “Coronavirus,” or “COVID-19,” or “SARS-CoV-2,” or “2019-nCoV,” separately combined with “structure,” “incubation,” “latency,” “transmission,” “symptoms,” “dentistry,” “infection control,” “treatment,” and “protocol.” Up-to-date reports and communications from major health bodies such as the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), National Institutes of Health, and major national orthodontic associations and health professional regulatory bodies were also referenced.
RESULTS
Due to the rapidly evolving nature of the disease and the need for scientific evidence to be available quickly, most of the studies were descriptive, small investigational studies, narrative reviews, and expert opinions (Table 1). More recent studies and peer-reviewed studies were preferred when available. As the evidence is still new and limited in quality, a narrative synthesis was undertaken to provide a broad review of key aspects relevant to orthodontists during the current pandemic.
Table 1. .
Sources of Literature and Information Included in This Review, With Levels of Evidence*
| Ref. no. |
Author |
Country |
Title/Topic |
Type of Study |
Level of Evidence |
| 1 | Guo YR, et al. (2020) | China, Singapore | The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status | Narrative review | 5 |
| 2 | Giovanetti M, et al. (2020) | Italy | The first two cases of 2019-nCoV in Italy: Where they come from? | Case series | 4 |
| 3 | Paraskevis D, et al. (2020) | Greece | Full-genome evolutionary analysis of the novel coronavirus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event | Short communication, Investigational, mechanism-based reasoning | 5 |
| 4 | Schoeman D, et al. (2020) | South Africa | Coronavirus envelope protein: current knowledge | Narrative review | 5 |
| 5 | Ji W, et al. (2020) | China | Cross-species transmission of the newly identified coronavirus 2019-nCoV | Investigational, mechanism-based reasoning | 5 |
| 6 | Lam TT-Y, et al. (2020) | China, Hong Kong | Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins | Investigational, mechanism-based reasoning | 5 |
| 7 | Zhu N, et al. (2019) | China | A novel coronavirus from patients with pneumonia in China, 2019 | Case series | 4 |
| 8 | Fehr AR, et al. (2015) | United States | Coronaviruses: an overview of their replication and pathogenesis | Narrative review | 5 |
| 9 | Kampf G, et al. (2020) | Germany | Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents | Narrative review | 5 |
| 10 | van Doremalen N, et al. (2020) | United States | Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1 | Correspondence, investigational, mechanism-based reasoning | 5 |
| 11 | Zhou P, et al. (2020) | China | A pneumonia outbreak associated with a new coronavirus of probable bat origin | Case series | 4 |
| 12 | Li Q, et al. (2020) | China | Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia | Case series | 4 |
| 13 | Zhao S, et al. (2020) | China | Anesthetic management of patients with COVID-19 infections during emergency procedures | Case series | 4 |
| 14 | Belser JA, et al. (2013) | United States | Ocular tropism of respiratory viruses | Narrative review | 5 |
| 15 | Lu CW, et al. (2020) | China | 2019-nCoV transmission through the ocular surface must not be ignored | Correspondence, expert opinion | 5 |
| 16 | Chen N, et al. (2020) | China | Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study | Case series | 4 |
| 17 | Rothe C, et al. (2020) | Germany | Transmission of 2019-nCoV infection from an asymptomatic contact in Germany | Correspondence, mechanism-based reasoning | 5 |
| 18 | Zhang W, et al. (2020) | China | Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes | Case series | 4 |
| 19 | To KK, et al. (2020) | China | Consistent Detection of 2019 Novel Coronavirus in Saliva | Case series | 5 |
| 20 | Santarpia JL, et al. (2020) | United States | Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center | Case series | 4 |
| 21 | Lauer SA, et al. (2020) | United States, Germany | The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application | Case series | 4 |
| 22 | Lan L, et al. (2020) | China | Positive RT-PCR test results in patients recovered from COVID-19 | Correspondence, case series | 4 |
| 23 | Ling Y, et al. (2020) | China | Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients | Case series | 4 |
| 24 | Dong Y, et al. (2020) | China | Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. | Case series | 4 |
| 25 | Wu Z, et al. (2020) | China | Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention | Viewpoint, review of reported data | 5 |
| 26 | Guan WJ, et al. (2020) | China | Clinical characteristics of Covid-19 in China | Case series | 4 |
| 27 | Huang C, et al. (2020) | China | Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China | Case series | 4 |
| 28 | Roser M, et al. (2020) | England | Coronavirus disease (COVID-19) – statistics and research | Review of reported data | 5 |
| 29 | Wang Y, et al. (2020) | China | Oral health management of children during the epidemic period of coronavirus disease 2019 | Narrative review | 5 |
| 30 | Sabino-Silva R, et al. (2020) | Canada, Brazil | Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis | Correspondence, mechanism-based reasoning | 5 |
| 31 | American Association of Orthodontists (2020) | United States | COVID-19 resources for orthodontists | Expert opinion | 5 |
| 32 | Centers for Disease Control and Prevention (2020) | United States | What to do if you are sick | Expert opinion | 5 |
| 33 | Ti LK, et al. (2020) | Singapore | What we do when a COVID-19 patient needs an operation: operating room preparation and guidance | Correspondence, expert opinion | 5 |
| 34 | Kim HJ, et al. (2020) | Korea | Recommendations for anesthesia in patients suspected of coronavirus 2019-nCoV infection | Expert opinion | 5 |
| 35 | Liu Y, et al. (2020) | China | Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak | Investigational, mechanism based reasoning | 5 |
| 36 | Ather B, et al. (2020) | United States | Coronavirus disease 19 (COVID-19): implications for clinical dental care | Narrative review | 5 |
| 37 | Centers for Disease Control and Prevention (2020) | United States | Dental settings | Expert opinion | 5 |
| 38 | Centers for Disease Control and Prevention (2020) | United States | Recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings | Expert opinion | 5 |
| 39 | American Dental Association (2020) | United States | Coronavirus frequently asked questions | Expert opinion | 5 |
| 40 | Centers for Disease Control and Prevention (2020) | United States | PPE sequence | Expert opinion | 5 |
| 41 | Peng X, et al. (2020) | China | Transmission routes of 2019-nCoV and controls in dental practice | Narrative review | 5 |
| 42 | Xie X, et al. (2020) | Hong Kong, China | Exhaled droplets due to talking and coughing | Investigational, mechanism-based reasoning | 5 |
| 43 | Samaranayake LP, et al. (2004) | Hong Kong | Severe acute respiratory syndrome and dentistry: a retrospective view | Review | 5 |
| 44 | Meng L, et al. (2020) | Wuhan, China | Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine | Review and expert opinion | 5 |
| 45 | World Health Organization (2020) | Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected - Interim guidance. 2020 | Expert opinion | 5 | |
| 46 | World Health Organization (2014) | Geneva | Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in health care. Annex G, use of disinfectants: alcohol and bleach | Expert opinion | 5 |
| American Association of Orthodontists (AAO) | United States | Recommendations and guidelines | Local communications | 5 | |
| Canadian Association of Orthodontists | Canada | Recommendations and guidelines | Local communications | 5 | |
| British Orthodontic Society | Britain | Recommendations and guidelines | Local communications | 5 | |
| American Dental Association | United States | Recommendations and guidelines | Local communications | 5 | |
| Royal College of Dental Surgeons of Ontario | Canada | Recommendations and guidelines | Local communications | 5 |
Level of evidence rating scheme based on Oxford Centre for Evidence-based Medicine (OCEBM) Levels of Evidence Working Group. “The Oxford Levels of Evidence 2:” Oxford Centre for Evidence-Based Medicine. Available at: https://www.cebm.net/index.aspx?o=5653. Accessed on April 5, 2020.
DISCUSSION
Etiology of the Pandemic
COVID-19 was first reported in Wuhan, Hubei province, central China in December 2019, where bats were suspected to be the primary host.1–3 Although many coronaviruses primarily infect animals, human infection occurs when the animal-human species barrier is crossed4 and, in the case of COVID-19, pangolins and snakes have been suspected to be the intermediate host.1,5,6 COVID-19 spread worldwide due to travel and, on March 11, 2020, the WHO declared COVID-19 as a pandemic. Currently, COVID-19 can be spread within cities through local transmission from an infected person or community transmission, where the source of infection is unknown. As of April 5, 2020, there have been more than 1.2 million confirmed cases of COVID-19 in 183 countries around the world and more than 69,000 people have died due to this disease (current data available at https://coronavirus.jhu.edu).
The Particle
Structure.
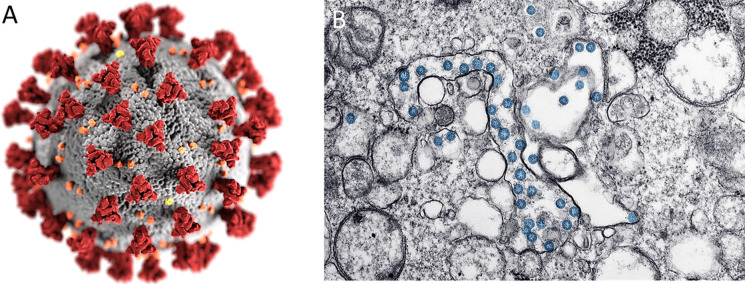
Coronaviruses (CoVs) are divided into four genera: namely alpha-, beta-, gamma-, and delta-coronavirus. Part of the beta-coronavirus genera, SARS-CoV-2 is a lipid bilayer enveloped non-segmented positive-sense RNA virus (Figure 1).7 Coronavirus virions are spherical and their surface appears crown-like (hence the name corona) due to spiked glycoprotein projections.8
Figure 1.
(A) Illustration of the ultrastructure of the coronavirus (Image open source: Centers for Disease Control and Prevention, CDC; Eckert A, Higgins D); (B) Transmission electron micrograph image of an isolate from the first U.S. case of COVID-19 showing the viral particles (blue) (Image open source: CDC, Bullock HA, Tamim A).
Lability and stability.
Human coronaviruses have been reported to remain infectious on inanimate surfaces in the range between 2 hours to up to 9 days.9 In a recent study performed under experimental conditions, SARS-CoV-2 specifically was detected on copper for up to 4 hours, cardboard for up to 24 hours, and stainless steel and plastic for up to 3 days.10 More importantly for dentistry and orthodontics, SARS-CoV-2 was detected in aerosols for up to 3 hours when created using a nebulizer.10 SARS-CoV-2 did experience an exponential decay in all experimental conditions, where the longest viability of the virus was on stainless steel and plastic (estimated median half-life of 5.6 hours on stainless steel and 6.8 hours on plastic).10
Transmission.
Although direct contact with the intermediate host is suspected to be the initial transmission route of SARS-CoV-2, progression of the virus allowed for human-to-human transmission.1,11 Human transmission is predominantly through the respiratory tract via droplets, respiratory secretions (cough, sneeze), and or direct contact,12 where the virus enters the mucous membrane of the mouth, nose, and eyes.13–15 Although contact with symptomatic patients is the typical route of transmission, asymptomatic individuals or those within the viral incubation period may also be able to transmit COVID-19.16,17 Recent studies have also found SARS-CoV-2 in blood, saliva, and fecal swabs,1,18,19 as well as potential transmission through respiration,20 indicating that more transmission routes may be possible.
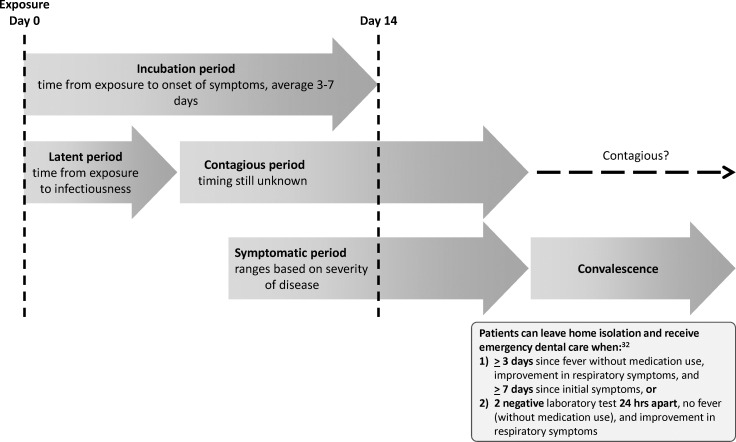
Incubation, latency, and contagious period.
The incubation period of SARS-CoV-2 reportedly ranges from 1 to 14 days, with an average of 3–7 days (Figure 2).1 The time from exposure to infectiousness (latent period) is shorter than the incubation period, as COVID-19 can transfer through asymptomatic or mildly symptomatic carriers.21 Generally, patients are considered to be in convalescence when they present with the following: (1) a normal temperature for more than 3 days, (2) resolved respiratory symptoms, and (3) two negative oropharyngeal swab reverse transcription polymerase chain reaction (RT-PCR) viral ribonucleic acid (RNA) tests that are taken at least 24 hours apart.22,23 However, SARS-CoV-2 detection can also occur after this, as seen from RT-PCR test results 5–13 days later,22 and positive fecal viral RNA tests in a small percentage of patients during convalescence.23 Currently, there is insufficient evidence to determine if patients can be contagious during convalescence.
Figure 2.
Incubation, latency, symptomatic, and contagious periods of SARS-CoV-2.
Clinical Manifestations
COVID-19 manifestations range from a complete lack of symptoms to symptomatic patients with severe complications leading to multiorgan dysfunction, septic shock, and systematic failure. COVID-19 can be classified into mild, moderate, severe, or critical diseases.24,25 In a retrospective study of 72,000 cases, 81% of symptomatic patients presented with mild symptoms, whereas severe and critical symptoms were seen in 14% and 5% of the cases, respectively.25
Most COVID-19 patients experience a dry cough, fatigue, and fever. Shortness of breath and gastrointestinal symptoms (diarrhea, vomiting), as well as atypical symptoms, including sore throat, severe headache, confusion, and muscle pain, may also occur. A small proportion of patients develop severe complications, including respiratory distress syndrome, shock, and arrhythmias, and some complications can lead to death.26,27 The proportion of severe or fatal infection varies among countries and the estimated case fatality percentage, as of April 5, 2020, varies between 0.33% and 11.03%.28
Populations at Risk
Individuals of all ages are susceptible to being infected with COVID-19. The age distribution of COVID-19 may vary among countries. Based on currently available information, individuals with certain risk factors are at higher risk of developing severe illness from COVID-19. These include advanced age (particularly individuals aged 65 years and older), presence of comorbidities in individuals of any age (eg, chronic lung disease, moderate-to-severe asthma, heart disease with complications, diabetes, hypertension, renal failure, liver disease, immunocompromised), and close contact with individuals diagnosed with COVID-19. Even though the symptoms are generally less severe in children with COVID-19, young children, particularly infants, were shown to be more susceptible and also more likely to manifest as severe or critical cases.24
Implications for Orthodontic Management During the Pandemic
All dental professionals, including orthodontists, may be at risk of acquiring COVID-19 through multiple transmission routes, including the following: (1) respiratory droplets from coughing and sneezing or created during a dental or orthodontic procedure, (2) indirect contact where viral droplets fall onto a surface that the dental professional or orthodontist later contacts, (3) aerosols created during dental or orthodontic procedures, (4) treating patients who may have experienced indirect contact transmission from removing and replacing aligners, appliances, and rubber bands, and (5) being in contact with multiple such persons, including those who accompany the patients.29 As SARS-CoV-2 has also been identified in the saliva of infected individuals,19 this poses an additional risk for dental professionals and their patients.30 Orthodontists must be especially cognizant of the available evidence to provide a safe environment for themselves, their patients (and patient family members), and the entire orthodontic team.
Strict adherence to the most up-to-date recommendations from federal, state/provincial, and local public health authorities is essential for all orthodontists. In the current stage of the COVID-19 pandemic, most authorities have suggested that all elective and routine dental treatment should be suspended and that only emergency dental treatment can be provided. A true dental emergency is one that deals with swelling, uncontrollable pain, bleeding, infection, and trauma to teeth and or bones. Orthodontic emergencies may include the embedment of an orthodontic appliance into the gingiva or oral mucosa leading to severe pain and or infection, circumstances related to dental trauma, or conditions where a lack of management would be harmful to the patient.31
In dealing with a pandemic of this nature, orthodontists should have a contingency plan in place for the management of their patients. The following key steps are recommended, based on an accumulation of the recommendations and suggestions of multiple professional regulatory bodies:
Provide patients with a broadcast communication describing the changes in access to the orthodontic clinic/office as per recommendations of the local public health and or dental regulatory authority,
Provide active patients with recommendations on treatment progression either on an as-needed individual basis or in a communication provided to all patients (eg, when to stop turning an expander, what to do when the patient has reached their final aligner, etc.). Patients should also be reminded to always wash their hands prior to and after placing and removing appliances or elastics, to clean their appliances regularly by wiping with alcohol, and to store appliances in their cases,29
Provide a means of communication (phone number or email) to patients to allow them to contact the orthodontist or an orthodontic team member with any questions or concerns, and send problem-related intraoral mobile-phone digital images,
Use phone calls or, where possible, video-calling or appropriate teledentistry facilities to assist patients in resolving any emergent orthodontic problem that can be managed at home, or to determine which patients need in-person attendance,
Provide emergent orthodontic treatment in a safe manner, where necessary, and
Exercise evidence-based precautions during the provision of any in-office emergency treatment.
In the case of orthodontic emergencies, orthodontists should first try to manage the emergency over the phone or remotely. A verbal or electronically signed consent should be obtained to provide advice in this manner and orthodontists should record all advice that was given in accordance with normal record keeping. If possible, orthodontists should guide patients on how to manage minor emergencies at home.29 Table 2 lists some orthodontic emergencies that may be encountered and advice that the orthodontist can give to patients for home management. Orthodontists can also provide their patients with links to such information with audiovisual aids, which may be available on professional orthodontic association websites (eg, https://www1.aaoinfo.org/). If appropriate, an over-the-counter analgesic may be prescribed for mild pain.
Table 2. .
Advice That Can Be Provided to Patients for the Short-Term Management of Orthodontic Emergencies at Homea–c
| Orthodontic Emergency |
How the Patient Can Attempt to Handle it at Home |
| Irritation of lip and/or cheek from the brackets | - Push/pinch a small piece of rolled relief waxd over the bracket or long wire that is causing the irritation. - Orthodontic wax that is accidentally swallowed is harmless. - Mouth sores can be relieved by applying a small amount of topical anesthetic (eg, Orabase, Colgate-Palmolive, New York, New York; or Orajel, Church & Dwight, Ewing, New Jersey) directly to the ulcerated surface using a cotton swab (reapplication might be needed). |
| Elastic ligature has come loose from a bracket during eating or tooth brushing. | - The ligature can be placed back around the bracket using a sterile tweezer. - If the patient is anxious about debonding the bracket or cannot place the ligature back in place, then a sterile tweezer can be used to remove the ligature. |
| Metallic ligature has come loose from a bracket or is irritating the lips and cheeks. | - If the ligature is loose, a sterile tweezer can be used to remove it. - If the ligature is not loose but is sticking out, a cotton swab/cotton bud or a clean pencil eraser can be used to bend the ligature back down. |
| Broken or loose elastic chain | - The extra segment can be removed with a sterile tweezer or cut with a sterile clipper. |
| Loose orthodontic attachment (bracket, tube, or band) | - If the patient cannot be seen in person by the orthodontist and the loose bracket is flipping (rotating) around on the wire and causing discomfort, a sterile tweezer can be used to correct this problem. First the bracket is moved along the wire so that it is in between two teeth. The bracket is then rotated back (unflipped) to its proper relation (as noted from the other brackets, which are not loose) and is then moved along the wire back to the center of the tooth. - If the bracket is used as an anchor for wearing elastic rubber bands, elastic wear should be stopped. - If the loose bracket is the last attachment in the arch, it can be slid off the wire if it is safe for a care provider to do so. The bracket can also be held securely and the wire with the loose bracket can be cut at the point of the last tooth that has a secure orthodontic attachment on it (see the following material). The cut end of the wire with the loose bracket attachment should be carefully removed from the mouth. |
| Protruding wire at the end of the braces | - A cotton swab/cotton bud or clean pencil eraser can be used to push the wire so that it flattens against the tooth. - A protruding wire can sometimes result from the archwire slipping away from one side and extruding past the other side, and if so, using a sterile tweezer, the wire can be gripped and moved back so that it is equally secure on both sides, and comfortable. - If the wire cannot be moved to a comfortable position, the wire can be covered with relief wax (see the entry on “Irritation of lips and/or cheeks”). - If the wire is extremely irritating, and the patient cannot be seen in person by the orthodontist, the patient or care provider may use a sterile nail clipper to cut the wire. Folded tissue or gauze should be used around the area while cutting the wire to reduce the possibility of swallowing of the snipped piece of wire. Relief wax may still be needed to provide comfort to the irritated area. |
| Piece of appliance or a bracket is swallowed | - Most small orthodontic appliances (eg, brackets) that are swallowed will pass through the digestive tract uneventfully. - If an object is swallowed, it should be confirmed that the patient did/does not have difficulty breathing or experience sudden coughing after the object was swallowed. In the case of sudden difficulty breathing or sudden coughing following ingestion of the broken appliance or bracket, the patient should go to an emergency department of a hospital. - The orthodontist may advise the patient to seek clinical examination and or radiographic assessment in the emergency department of a hospital. |
| Broken bonded retainer | - If the whole bonded retainer is loose and the patient cannot be seen in person by the orthodontist, the retainer should be left outside of the mouth. The patient should be advised to wear their removable retainer (if provided) until their next visit with the orthodontist when the clinic/practice reopens for routine treatment. - If only one or two teeth have resin pads that are loose and the patient cannot be seen in person by the orthodontist, the patient can: - attempt to push the loose retainer wire back towards its tooth as much as possible, or - cut the exposed unbonded part of the retainer using a sterile clipper (see previous example of protruding wire). - If only a small portion of the retainer is still bonded, a sterile tweezer can be used gently to pull and remove the whole retainer. If too much force is required to remove the retainer, then it should be cut with a sterile clipper. |
| Long, hanging gold chains that are severely irritating | - If the patient cannot be seen in person by the orthodontist, if possible, a piece of dental floss can be threaded through or tied around the last link at the loose end of the chain by the care provider at home, and then tied to a bracket so that it is no longer hanging and causing severe irritation. - It is not advised to cut the hanging long chain, as there is a risk of aspiration. |
| Broken or loose fixed expander or a lingual/palatal arch | - If the expander/lingual/palatal arch is partially glued and still present in the mouth, it can be placed back in position, and any remaining screw activations should be stopped until the patient can be seen in-person by the orthodontist. - If the expander has fallen out completely it should be kept in a safe place until further instructions are received from the orthodontist. |
| Broken intermaxillary spring, eg, Class II corrector appliance | - If completely broken (and the spring cannot be reattached to the rod) the patient or home care provider can use a piece of dental floss to secure the loose end of the appliance to the remaining archwire and brackets. |
| Part of orthodontic appliance embedded in the gingiva leading to severe pain and or infection | - This would represent a true emergency that could be seen by the orthodontist in office, provided that the patient has cleared the triage questions with respect to COVID-19 and the orthodontist has suitable PPE and if this is permitted by the local health regulatory bodies, or should be seen in a hospital setting. - If the patient cannot be seen in person by the orthodontist, the patient or home care provider can use a sterile clipper to cut the wire if it is attached to the broken or loose part and remove the broken part from the mouth using sterile tweezers. However, this may not be possible to do with large diameter wires. |
Adapted from online resources posted on the websites of the American Association of Orthodontists, the British Orthodontic Society, and the Canadian Association of Orthodontists.
In all emergencies, patients should first consult their orthodontic care provider and follow the recommendations provided by their orthodontic care provider. Orthodontists should consider the jurisdictional requirements and permissions of regulatory professional bodies of the area in which their practice is located. In-person emergency dental treatment, including handling of orthodontic emergencies may also be undertaken by general dental practitioners or other dental specialists in accordance with the jurisdictional requirements and permissions of regulatory professional bodies of the area in which their practice is located.
These should be attempted only if it is safe for the patient to do so, or by a care provider who is capable of undertaking these steps at home, who should wear gloves if possible. Some of the methods and steps described here may not be possible for patients or care providers to perform if they have COVID-19 or are quarantined.
Wax provided by the orthodontist or purchased from the drug store/pharmacy.
When telecommunication is made by the orthodontist, the patient's health history should be obtained to elicit symptoms or contact history relevant to COVID-19. The patient should be advised to seek appropriate medical treatment or hospitalization based on the analysis of this history. In the event that the patient has to be seen in person, the medical history will also allow the orthodontist to assess the potential transmission risks and to ensure that the clinical operatory is equipped with the proper personal protective equipment (PPE). In-person orthodontic treatment should be deferred for 2 weeks if the patient has been in contact with someone who has been infected or if the patient has travelled.
For patients with a history of COVID-19, the CDC currently recommends that patients can leave home isolation when the following criteria have been met: (1) At least 72 hours have passed since recovery (resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms, eg, cough, shortness of breath), and at least 7 days have passed since initial symptoms; or (2) The patient has had two negative laboratory tests 24 hours apart, has no fever (without the use of fever-reducing medications), and other symptoms have improved.32 For orthodontic emergencies, most patients with suspected or confirmed COVID-19 should not be seen unless the patient has cleared the CDC's guidelines. If the patient must be seen due to the nature of the emergency, proper use of PPE is critical, including fit-tested N95 masks, double gloving, over gown, and face/eye protection.33,34 The PPE should include hair covers and hoods and eyewear with side shields or full-face shields. Fluid-impermeable shoes are preferred. It has also been reported that SARS-CoV-2 may become re-suspended during the removal of contaminated PPE or from the floor with movement of health care professionals.35 Airborne infection isolation rooms (AIIR) with negative suction and air purifiers with high-efficiency particulate air filters may significantly reduce the risk of transmission and, for this reason, emergency orthodontic and/or dental treatment of known cases of COVID-19 may be more appropriately undertaken in hospital settings where such facilities exist.36
When a patient needs to be seen in practice, triage over the phone is needed to confirm a negative history for COVID-19 symptoms, no contact with an infected individual, and no recent travel.37 A screening questionnaire should be completed electronically if possible, prior to entering the practice/office. It is recommended that the patient enter the office with a maximum of one accompanying person,29 who should not be at high-risk for COVID-19 infection (eg, not medically compromised).38 Hand hygiene is the single most important practice for control of nosocomial infections. Washing hands for a minimum 20 seconds with soap, as soap breaks down the lipid layer of the virus, or alcohol-based hand rub (ABHR) with at least 60% ethanol is recommended. Both 80% ethanol and 75% 2-propanol have been established to have reliable and equal potency for SARS-CoV-2, while benzalkonium chloride was not found to be as effective.9 At the point of entry to the clinic, the patient and accompanying person should use ABHR.29 After recording the temperature of every person entering the registration area29 by a staff member with appropriate PPE, a screening questionnaire should be completed verbally for each entrant while maintaining a distance of 6 feet between people. This questionnaire should reconfirm the triage questions that were asked over the phone. To avoid contact between people, magazines or other materials that cannot be disinfected should be removed from the waiting room and, when more than one patient needs to be seen for an emergency, appointments should be staggered as much as possible.39
Where possible, only the patient should be allowed entry into the clinical/operatory area. The orthodontic practice/office must maintain a very high standard of sterilization and infection prevention and control (IPAC) protocol, including effective hand hygiene before and after contact with a patient,38 and following the proper sequence for replacement and removal of PPE.40 During the provision of emergency treatment, the practitioner must be careful to only do what is necessary to resolve the emergency and to take the patient to a position of safety. SARS-CoV-2 is vulnerable to oxidation; therefore, preprocedural mouthrinse containing 1% hydrogen peroxide or 0.2% povidone-iodine41 can be advised, although the level of evidence for its use is low. During the pandemic, practitioners should refrain from performing any procedures that lead to aerosols, avoiding air water syringes, high-speed handpieces, and ultrasonic scalers. This is because long-distance transmission is possible when viral particles become suspended in the air42 and viral particles may remain in aerosols for up to 3 hours.10 The CDC has recommended that N95 masks, eye protection, a gown, and gloves should be used for any aerosol-producing procedure that must be completed, and that they should ideally take place in an AIIR,38 as asymptomatic individuals can transmit COVID-19.16,17 Practitioners should check recommendations made by their local regulatory bodies if an aerosol-producing procedure cannot be avoided though, from an orthodontic perspective, this should be rare. If handpiece use is imperative, anti-retraction handpieces are advised to restrict debris and fluid aspiration and later, ejection.43 High-volume suction is critical for all aerosol-producing procedures.
Radiographs should be deferred during the pandemic but, if radiographs are required, extraoral radiography is preferred over intraoral radiography to reduce saliva and aerosol production due to gagging and coughing.36,44 If local anesthesia is required, a local anesthetic gel is preferable over local anesthetic sprays due to potential virus spread in the air.34
Orthodontic practices must follow rigorous disinfection following the completion of any emergency treatment to minimize spread through fomites and environmental surfaces. Any steel wires and appliance parts that were cut or removed should be treated as highly infected medical equipment and disposed of as a medical hazard. All surfaces should be thoroughly disinfected using hospital-grade disinfectants such as sodium hypochlorite.9 For coronaviruses, bleach/sodium hypochlorite should be used at a concentration of 0.1%–0.2% for 1 minute, rather than the typical 0.05% concentration.9,45,46 Ethanol in concentrations of 62%–95% is also recommended to disinfect small surfaces.9,46 Hydrogen peroxide vaporizer has also been proposed for post-procedure operatory decontamination.33 Waterlines that have been used should be adequately purged to prevent a backflow of pathogens, which can harbor in the plastic tubing. All instruments should be properly disinfected and sterilized immediately and all used, as well as unused, disposables that were within the exposed portion of the operatory, should be presumed to be infected and disposed of as infected medical waste.33
CONCLUSIONS
During the COVID-19 pandemic, it is imperative that orthodontists think globally and act locally to minimize the risks of transmitting SARS-CoV-2 in the orthodontic setting.
Elective treatment, including routine orthodontic treatment, should be suspended and resumed only when permitted by federal, state/provincial, and local health regulatory authorities.
Emergency orthodontic treatment can be provided by following a contingency plan founded on effective communication and triage. Treatment advice should be delivered remotely first whenever possible and, where necessary, in-person treatment can be performed in a well-prepared operatory following the necessary precautions and IPAC protocol.
Guidelines and practice advisories issued by federal, state/provincial, and local health and regulatory authorities should be followed.
REFERENCES
- 1.Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovanetti M, Benvenuto D, Angeletti S, Ciccozzi M. The first two cases of 2019-nCoV in Italy: Where they come from? J Med Virol. 2020;92(5):518–521. doi: 10.1002/jmv.25699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paraskevis D, Kostaki EG, Magiorkinis G, Panayiotakopoulos G, Sourvinos G, Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect Genet Evol. 2020;79:104212. doi: 10.1016/j.meegid.2020.104212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019;16(1):69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol. 2020;92(4):433–440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam TT-Y, Shum MH-H, Zhu H-C, et al. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature. 2020. [DOI] [PubMed]
- 7.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. [DOI] [PMC free article] [PubMed]
- 11.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao S, Ling K, Yan H, et al. Anesthetic management of patients with COVID 19 infections during emergency procedures. J Cardiothorac Vasc Anesth. 2020;34(5):1125–1131. doi: 10.1053/j.jvca.2020.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belser JA, Rota PA, Tumpey TM. Ocular tropism of respiratory viruses. Microbiol Mol Biol Rev. 2013;77(1):144–156. doi: 10.1128/MMBR.00058-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.To KK, Tsang OT, Chik-Yan Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed]
- 20.Santarpia JL, Rivera DN, Herrera V, et al. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv. 2020.
- 21.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 22.Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020. e1–e2. [DOI] [PMC free article] [PubMed]
- 23.Ling Y, Xu SB, Lin YX, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl) 2020. [DOI] [PMC free article] [PubMed]
- 24.Dong Y, Mo X, Hu Y, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020.
- 25.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. [DOI] [PubMed]
- 26.Guan WJ, Zhong NS. Clinical Characteristics of Covid-19 in China. Reply. N Engl J Med. 2020. 382. [DOI] [PubMed]
- 27.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roser M, Ritchie H, Ortiz-Ospina E. Coronavirus disease (COVID-19) – statistics and research. 2020 Available at: https://ourworldindata.org/coronavirus Accessed April 5, 2020.
- 29.Wang Y, Zhou CC, Shu R, Zou J. [Oral health management of children during the epidemic period of coronavirus disease 2019 (Chinese)] Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51(2):151–154. doi: 10.12182/20200360101. [DOI] [PubMed] [Google Scholar]
- 30.Sabino-Silva R, Jardim ACG, Siqueira WL. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig. 2020;24(4):1619–1621. doi: 10.1007/s00784-020-03248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Association of Orthodontists. COVID-19 Resources for Orthodontists. 2020 Available at: https://www1.aaoinfo.org/covid-19/ Accessed April 5, 2020.
- 32.Centers for Disease Control and Prevention. What to Do if You Are Sick. 2020 Available at: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html Accessed April 5, 2020.
- 33.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020. pp. 1–3. [DOI] [PMC free article] [PubMed]
- 34.Kim HJ, Ko JS, Kim TY. Recommendations for anesthesia in patients suspected of coronavirus 2019-nCoV infection. Korean J Anesthesiol. 2020. pp. 89–91. [DOI] [PMC free article] [PubMed]
- 35.Liu Y, Ning Z, Chen Y, et al. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. bioRxiv. 2020.
- 36.Ather A, Nikita B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020. 46(5) [DOI] [PMC free article] [PubMed]
- 37.Centers for Disease Control and Prevention. Dental Settings. 2020 Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html Accessed April 5, 2020.
- 38.Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. 2020 Available at: https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html#manage_access Accessed April 5, 2020.
- 39.American Dental Association. Coronavirus Frequently Asked Questions. 2020 Available at: https://success.ada.org/en/practice-management/patients/coronavirus-frequently-asked-questions Accessed April 5, 2020.
- 40.Centers for Disease Control and Prevention. PPE Sequence. 2020 Available at: https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf Accessed April 5, 2020.
- 41.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009;6(Suppl 6):S703–714. doi: 10.1098/rsif.2009.0388.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Samaranayake LP, Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. J Am Dent Assoc. 2004;135(9):1292–1302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020. 22034520914246. [DOI] [PMC free article] [PubMed]
- 45.World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected - Interim guidance. 2020 Available at: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 Accessed April 5, 2020.
- 46.World Health Organization. Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care. Annex G Use of disinfectants alcohol and bleach. 2014. Available at: https://www.ncbi.nlm.nih.gov/books/NBK214356/ Accessed April 5, 2020. [PubMed]