Abstract
Objectives
To compare the effects of Forsus appliances with and without temporary anchorage devices (TADs) for patients with skeletal Class II malocclusion.
Materials and Methods
Through a predefined search strategy, electronic searching was conducted in PubMed, Embase, Web of Science, CENTRAL, ProQuest Dissertations & Theses, and SIGLE with no language restrictions. Eligible study selection, data extraction, and evaluation of risk of bias (Cochrane Collaboration tool) were conducted by two authors independently and in duplicate. Any disagreement was solved by discussion or judged by a third reviewer. Statistical pooling, sensitivity analysis, subgroup analysis, and assessment of small-study effects were conducted by using Comprehensive Meta-Analysis and Stata 12.0. Heterogeneity was analyzed for different types of study designs, TADs, and radiographic examinations.
Results
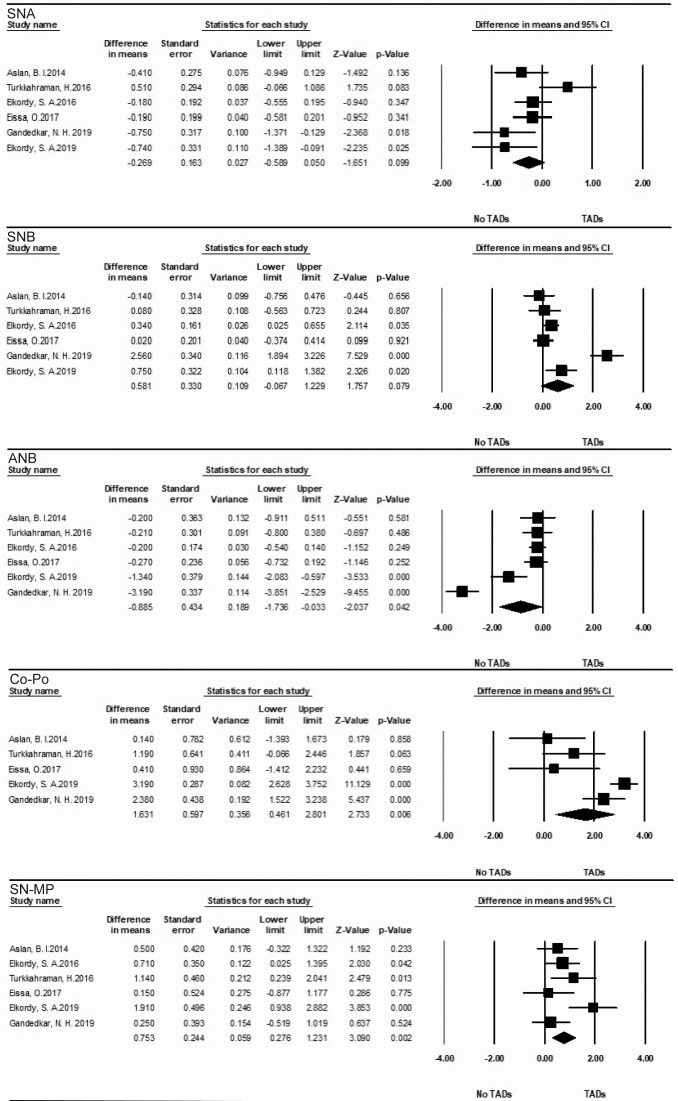
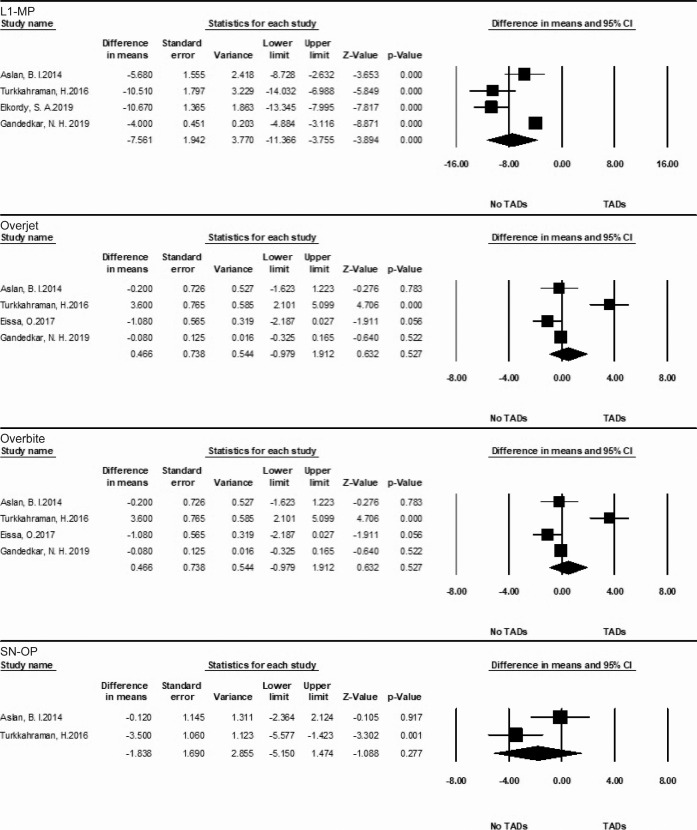
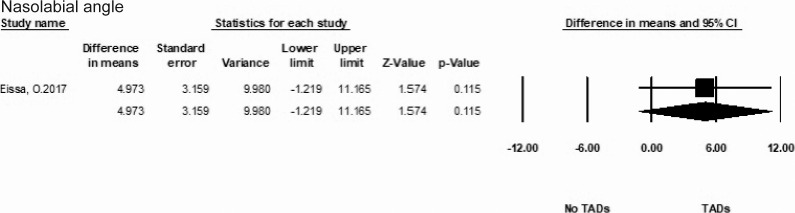
Electronic search yielded a total of 256 studies after removing duplicates. Among them, six studies were finally included. All articles were of high quality. The pooled mean differences were –0.27 (95% confidence interval [CI]: –0.59, 0.05) for SNA, 0.58 (95% CI: –0.07, 1.23) for SNB, –0.86 (95% CI: –1.74, –0.03) for ANB, 1.63 (95% CI: 0.46, 2.80) for Co-Po, 0.75 (95% CI: 0.28, 1.23) for SN-MP, –7.56 (95% CI: –11.37, –3.76) for L1-MP, 0.47 (95% CI: –0.98, 1.91) for overjet, 0.39 (95% CI: –0.57, 1.35) for overbite, –1.84 (95% CI: −5.15, 1.47) for SN-OP, and 4.97 (95% CI: –1.22, 11.17) for nasolabial angle.
Conclusions
TADs (especially miniplates) were able to eliminate dental adverse effects of Forsus appliances for correction of skeletal Class II malocclusion.
Keywords: Class II malocclusion, Forsus, Temporary anchorage devices, Systematic review, Meta-analysis
INTRODUCTION
Class II malocclusion is a constellation of several types of malocclusion. Patients with Class II malocclusion can exhibit maxillary protrusion, mandibular retrusion, or their combinations, together with abnormal dental relationship problems and facial esthetic disorders.1 In particular, mandibular retrusion, rather than maxillary protrusion, is the main etiologic factor for Class II malocclusion2 and the most common characteristic of Class II malocclusion.3 Therefore, orthodontic treatments promoting mandibular growth or advancement are indicated for growing patients with mandibular retrusion.
A variety of orthodontic appliances have been designed for mandibular retrusion, including fixed functional and removable functional appliances. They achieve Class II correction by inducing mandibular lengthening sagittally and vertically by stimulating condylar growth.4 While the treatment effects of removable functional appliances are limited by poor patient cooperation, fixed functional appliances (FFAs) are more advantageous and are able to achieve clinically significant mandibular elongation.5 Among various FFAs, Forsus Fatigue Resistant Device (FFRD; 3M Unitek, Monrovia, Calif)6 is an example of a hybrid FFA, which is used for treatment of mandibular retrusion in growing patients. However, it has been suggested that Forsus could induce mandibular lengthening at the expense of dentoalveolar compensations. Forsus exerts anteriorly directed force on the mandibular dentition, and this may result in proclination of the mandibular incisors, jeopardizing the long-term stability of treatment outcomes.7
To minimize the adverse effects of Forsus, a combination of Forsus and temporary anchorage devices (TADs) has been claimed to preserve dental anchorage and avoid adverse dental effects.8–12 However, controversy arose regarding whether Forsus with and without skeletal anchorage produced similar treatment results.9,13 These conflicting results are likely attributed to different types of skeletal anchorage and different study designs. To date, no conclusion has been made whether Forsus with TADs are superior to Forsus only. The aims of this study were to compare the effects of Forsus with and without TADs for patients with Class II mandibular retrusion.
MATERIALS AND METHODS
Protocol and Registration
The protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO; http://www.crd.york.ac.uk/prospero; registration number CRD42020140721).
Inclusion Criteria
Growing patients diagnosed with skeletal Class II base with mandibular retrusion were included. Interventions were Forsus and fixed appliances with or without TADs (eg, miniscrews and miniplates) for mandibular advancement. Both randomized controlled trials (RCTs) and prospective controlled clinical trials (CCTs) were eligible.
Exclusion Criteria
Patients with severe orofacial anomalies (eg, cleft lip), dental pathology (eg, cyst), and medical conditions (eg, osteoporosis) were excluded.
Information Sources, Search Strategy, and Study Selection
The databases searched included those of PubMed, Embase, Web of Science, Cochrane Central Register of Controlled Trials (CENTRAL), ProQuest Dissertations & Theses, and the gray literature database of SIGLE. Specifically, the electronic search parameters were articles from January 1980 to April 2020 with no language restrictions. The specific search strategy of PubMed is presented in Table 1. Titles and abstracts were assessed according to the eligibility criteria. The selected articles were evaluated after reading full texts, and a final selection was determined. Searching and assessment of studies was performed independently and in duplicate by two reviewer authors (Miss Liu and Miss Zhan), and disagreements were judged by a third reviewer (Dr Long).
Table 1.
Search Strategy for PubMed
| Step |
PubMed Search Strategy |
| 1 | “Malocclusion, Angle Class II” [mesh] OR Angle Class II OR Class II, Angle OR Class II OR Distocclusion* OR Distal occlusion* |
| 2 | Forsus OR functional appliance OR orthopedic OR mandibular advancement |
| 3 | Dental implant OR Micro-implant OR Microimplant OR Micro implant OR Mini-implant OR Mini implant OR Mini-screw OR Miniscrew OR Mini screw OR Mini-plate OR Miniplate OR Mini plate OR Skeletal anchorage OR Bone anchorage OR Bone screw |
| 4 | 1 AND 2 AND 3 |
Data Extraction
Results regarding study design, demographic data (age, sample size, grouping, and skeletal age), detailed description (interventions, treatment duration, and comparator), and outcomes (skeletal, dentoalveolar, and soft-tissue measurements from anteroposterior, and vertical direction) were all extracted.
Study Outcomes
Study outcomes were skeletal indices (SNA, SNB, ANB, Co-Po, SN-MP), dental indices (L1-MP, overjet, overbite, SN-OP), and soft-tissue indices (nasolabial angle). Primary outcomes were ANB, SN-MP, and L1-MP, and secondary outcomes were SNA, SNB, Co-Po, overjet, overbite, SN-OP, and nasolabial angle.
Risk of Bias and Quality Assessment
The evaluation of risk of bias for the included studies was performed independently and in duplicate by two review authors (Miss Liu and Miss Zhan) according to the Cochrane tool for assessing risk of bias in randomized trials (RoB 2.0 tool)14 and in nonrandomized trials (ROBINS-I tool).15 For each bias domain, a judgment score was given following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 Any disagreement was solved by discussion or judged by a third reviewer (Dr Long). Additionally, the Grading of Recommendation Assessment, Development and Evaluation (GRADE) system of rating quality of evidence was used to appraise the quality of each outcome in this review.16–21
Meta-analysis
Original outcome data were subject to statistical pooling through random effect models. The criteria of data pooling were determined a priori on the basis of the comparability of study design, patient type, treatments, outcomes, and risk of bias. Mean difference (MD) was used for statistical pooling for continuous data. Heterogeneity across studies was assessed through the I2 statistic, and an I2 statistic greater than 50% was considered as substantial heterogeneity.
If substantial heterogeneity existed, a subgroup analysis on different study designs, types of TADs, and radiographic modalities was executed to explore the potential heterogeneity. In addition, sensitivity analysis for studies with small sample sizes was conducted to evaluate the robustness of the pooled results in the meta-analysis. Cumulative meta-analysis was performed to determine the chronological changes of the pooled results. The Egger test and Begg test were used to assess publication bias or small study effect.
All the meta-analyses were performed in Comprehensive Meta-Analysis (version 2.2.064, Biostat, Englewood, NJ) and Stata 12.0 (Stata Corp, College Station, Tex).
RESULTS
Description of Studies
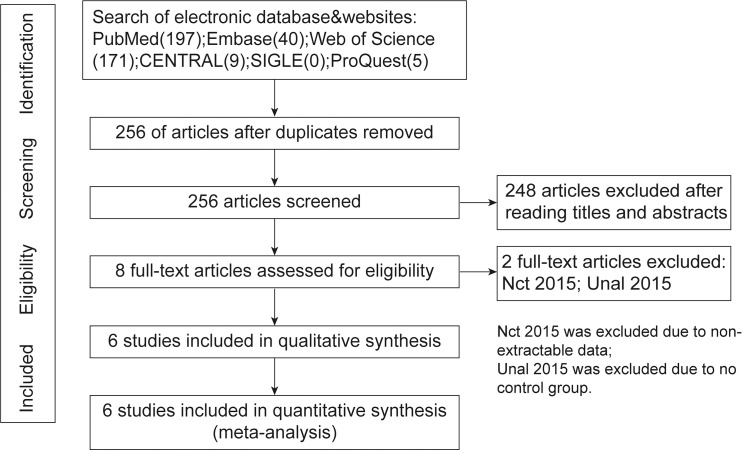
Initially, 256 articles from the database were identified and 248 were excluded as irrelevant. The remaining eight articles were further assessed for eligibility, and six studies (three RCTs and three prospective CCTs) were finally included in this systematic review.8–13 The procedures of electronic searching and selection are shown in Figure 1. Sample sizes ranged from 8 to 16 in different groups, with ages between 12 and 14 years old. The active Forsus treatment durations ranged from 4.86 months to 10.45 months. The details of each study are presented in Table 2. All six articles8–13 were high quality. Risk of bias is presented in Table 3.
Figure 1.
PRISMA flow diagram for studies retrieved through the search and selection processes.
Table 2.
General Information Provided in the Included Studies a.
| Study |
Design |
Participants |
Skeletal Class II |
Skeletal Maturation |
Treatment Duration (mo) |
Fixed Appliance |
TAD |
Radiograph Analysis |
| Aslan et al. 20148 | Prospective CCT | TAD: n = 16, age = 13.68 ± 1.09 No TAD: n = 17, age = 14.64 ± 1.56 | Class II molar relationship with mandibular retrognathia | N/A | TAD: 6.5 ± 1.97 No TAD: 5.5 ± 1.80 | 0.018-inch slot Roth brackets | Miniscrew | Lateral cephalometric |
| Eissa et al. 201713 | RCT | TAD: n = 15, age = 12.52 ± 1.12 No TAD: n = 14, age = 12.76 ± 1.0 | ANB > 4.5° SNB < 76° | Stage 2–4 (CVM) | TAD: 6.42 ± 1.04 No TAD: 6.06 ± 0.76 | 0.022-inch slot MBT brackets | Miniscrew | Lateral cephalometric |
| Elkordy et al. 201910 | RCT | TAD: n = 15, age = 12.06 ± 0.79 No TAD: n = 15, age = 12.54 ± 0.90 | SNB < 76° | Stage 3–4 (CVM) | TAD: 9.42 ± 0.98 No TAD: 6.23 ± 1.61 | 0.022-inch slot MBT brackets | Miniplate | CBCT |
| Elkordy et al. 20169 | RCT | TAD: n = 15, age = 13.07 ± 1.41 No TAD: n = 16, age = 13.25 ± 1.12 | SNB < 76° | Stage G–H (MP3) | TAD: 5.34 ± 1.29 No TAD: 4.86 ± 1.32 | 0.022-inch slot MBT brackets | Miniscrew | CBCT |
| Gandedkar et al. 201911 | Prospective CCT | TAD: n = 8, age = 12.96 ± 0.38 No TAD: n = 8, age = 13.11 ± 0.38 | SNA 84 ± 2° SNB 76 ± 2° ANB > 4 ± 1° | 15% prepubertal 70% pubertal 15% postpubertal | TAD: 10.45 ± 0.16 No TAD: 7.59 ± 0.32 | 0.022-inch slot brackets | Miniplate | CBCT |
| Turkkahraman et al. 201612 | Prospective CCT | TAD: n = 15, age = 12.77 ± 1.24 No TAD: n = 15, age = 13.26 ± 0.82 | Angle Class II molar relationship; convex profile with mandibular deficiency | N/A | TAD: 9.40 ± 2.25 No TAD: 9.46 ± 0.81 | 0.018-inch slot Roth brackets | Miniplate | Lateral cephalom-etric |
CBCT indicates cone-beam computed tomography; CCT, controlled clinical trial; N/A, not applicable; RCT, randomized controlled trial; TAD, temporary anchorage device; CVM, cervical vertebrae maturation; MP3, middle phalanges of the 3rd finger; MBT, McLaughlin, Bennett and Trerisi.
Table 3.
Risk of Bias of the Included Studies
| Study |
Item 1 |
Item 2 |
Item 3 |
Item 4 |
Item 5 |
Item 6 |
Item 7 |
Quality |
| ROB 2.0a | ||||||||
| Elkordy et al. 20169 | Low | Low | Low | Low | Low | Low | High | |
| Eissa et al. 201713 | Low | Low | Unclear | Low | Low | Unclear | High | |
| Elkordy et al. 201910 | Low | Low | Unclear | Low | Low | Unclear | High | |
| ROBINS-Ib | ||||||||
| Aslan et al. 20148 | Unclear | Low | Low | Low | Low | Unclear | Low | High |
| Turkkahraman et al. 201612 | Unclear | Low | Low | Low | Low | Unclear | Low | High |
| Gandedkar et al. 201911 | Unclear | Low | Low | Low | Low | Unclear | Low | High |
ROB 2.0: item 1, bias arising from the randomization process; item 2, bias due to deviations from intended interventions; item 3, bias due to missing outcome data; item 4, bias in measurement of the outcome; item 5, bias in selection of the reported result; and item 6, overall bias. Scoring rules: low indicates a score of 2; unclear, a score of 1; and high, a score of 0. Quality was categorized as low (score 1–4), medium (score 5–8), or high (score 9–12).
ROBINS-I: item 1, bias due to confounding; item 2, bias in selection of participants into the study; item 3, bias in classification of interventions; item 4, bias due to deviations from intended interventions; item 5, bias due to missing data; item 6, bias in measurement of outcomes; and item 7, bias in selection of the reported result. Scoring rules: low indicates a score of 2; unclear, a score of 1; and high, a score of 0. Quality was categorized as low (score 1–5), medium (score 6–10), or high (score 11–14).
Description of Interventions
Forsus appliances and fixed appliances were used in all the included studies. Two types of TADs were used among the included studies: miniscrew and miniplate. Among the included studies, three studies8,9,13 used miniscrews and the other three studies10–12 used miniplates. A total of 169 participants were included in this systematic review: 84 received Forsus+TADs and 85 received Forsus only. Among the 84 participants receiving Forsus+TADs, miniscrews were used in 46 participants, and the remaining 38 received miniplates.
Description of Outcomes
Among the proposed study outcomes, 10 outcomes were investigated in the included studies: skeletal outcomes (SNA, SNB, ANB, Co-Po, and SN-MP), dental outcomes (L1-MP, overjet, overbite, and SN-OP), and soft-tissue outcome (nasolabial angle). Outcomes at the active treatment effect period (changes from before Forsus treatment to after Forsus treatment) were studied in this meta-analysis. The GRADE assessment for quality of evidence for each outcome is shown in Table 4. Unfortunately, the quality of evidence of the outcomes in this meta-analysis was determined to be very low.
Table 4.
GRADE Assessment for Quality of Evidence
| Index |
Study Design |
Downgrade |
Upgrade |
Overall Quality |
||||
| Limitations |
Inconsistency |
Indirectness |
Imprecision |
Publication Bias |
||||
| SNA | 3 RCTs 3 prospective CCTs | Serious | Serious | None | Serious | None | None | Very low |
| SNB | 3 RCTs 3 prospective CCTs | Serious | Very serious | None | Very serious | None | None | Very low |
| ANB | 3 RCTs 3 prospective CCTs | Serious | Very serious | None | Very serious | Likely | None | Very low |
| Co-Po | 2 RCTs 3 prospective CCTs | Serious | Very serious | None | Very serious | Likely | None | Very low |
| SN-MP | 3 RCTs 3 prospective CCTs | Serious | Serious | None | Serious | None | None | Very low |
| L1-MP | 1 RCT 3 prospective CCTs | Serious | Serious | None | Very serious | None | None | Very low |
| Overjet | 1RCT 3 prospective CCTs | Serious | Very serious | None | Very serious | None | None | Very low |
| Overbite | 1 RCT 3 prospective CCTs | Serious | Very serious | None | Serious | None | None | Very low |
| SN-OP | 2 prospective CCTs | Serious | Serious | None | Very serious | None | None | Very low |
| Nasolabial angle | 1 RCT | None | None | None | Very serious | None | None | Very low |
CCT controlled clinical trial; RCT, randomized controlled trial.
Meta-analysis
For skeletal outcomes (Figure 2), six studies8–13 investigated SNA, SNB, and ANB angle, which had pooled MDs of −0.27° (95% confidence interval [CI]: −0.59, 0.05), 0.58° (95% CI: −0.07, 1.23), and –0.86° (95% CI: −1.74, –0.03), respectively. Five studies8,10–13 investigated Co-Po, which had a pooled MD of 1.63 mm (95% CI: 0.46, 2.80). Six studies8–13 investigated SN-MP, which had a pooled MD of 0.75° (95% CI: 0.28, 1.23).
Figure 2.
Forest plots of pooled MD of skeletal outcomes (SNA, SNB, ANB, Co-Po, and SN-MP) for the TAD-FFAs group versus control group.
For dental outcomes (Figure 3), four studies8,10–12 investigated L1-MP, which had a pooled MD of –7.56° (95% CI: −11.37, −3.76). Four studies8,11–13 investigated overjet and overbite, which had pooled MDs of 0.47 mm (95% CI: −0.98, 1.91) and 0.39 mm (95% CI: −0.57, 1.35), respectively. Two studies8,12 investigated SN-OP, which had a pooled MD of −1.84° (95% CI: −5.15, 1.47).
Figure 3.
Forest plots of pooled MD of dental outcomes (L1-MP, overjet, overbite, and SN-OP) for the TAD-FFAs group versus control group.
For soft-tissue outcome (Figure 4), one study13 investigated nasolabial angle, which was 4.97° (95% CI: –1.22, 11.17).
Figure 4.
Forest plots of pooled MD of soft-tissue outcome (nasolabial angle) for the TAD-FFAs group versus control group.
Sensitivity Analysis and Subgroup Analysis
Due to the small sample size in Gandedkar et al.,11 sensitivity analysis was performed by excluding this study from the meta-analysis. Stable results were found except for Co-Po (MD = 1.34; 95% CI: –0.36 ∼ 3.04).
Subgroup analysis was performed since different study designs, TADs, and radiographic modalities could influence the results of the meta-analysis (Table 5).
Table 5.
Results of Subgroup Analysisa
| Index |
Original result |
Study Design |
TADs |
Radiography |
|||
| Prospective CCT |
RCT |
Miniscrew |
Miniplate |
Lateral Cephalometric |
CBCT |
||
| SNA | −0.27 (−0.59, 0.05) | –0.21 (−0.94, 0.51) | –0.28 (−0.56, 0.00) | –0.23 (−0.47, 0.01) | –0.32 (−1.16, 0.53) | –0.05 (–0.54, 0.44) | –0.49 (−0.90, – 0.07) |
| SNB | 0.58 (−0.07, 1.23) | 0.83 (−0.84, 2.50) | 0.31 (−0.03, 0.65) | 0.15 (−0.13, 0.42) | 1.13 (−0.30, 2.56) | 0.00 (−0.30, 0.29) | 1.19 (−0.08, 2.47) |
| ANB | –0.86 (−1.74, –0.03) | –1.20 (−3.14, 0.74) | –0.51 (−1.07, 0.04) | –0.22 (−0.48, 0.03) | –1.58 (−3.36, 0.21) | –0.24 (−0.56, 0.09) | –1.56 (−3.42, 0.29) |
| Co-Po | 1.63 (0.46, 2.80) | 1.36 (0.06, 2.65) | 1.94 (−0.77, 4.65) | 0.25 (−0.92, 1.43) | 2.38 (1.32, 3.43) | 0.69 (−0.17, 1.55) | 2.85 (2.07, 3.64) |
| SN-MP | 0.75 (0.28, 1.23) | 0.59 (0.08, 1.09) | 0.92 (−0.01, 1.84) | 0.52 (0.06, 0.99) | 1.06 (0.11, 2.02) | 0.62 (0.08, 1.17) | 0.91 (0.04, 1.78) |
| L1-MP | –7.56 (−11.37, −3.76) | –6.43 (−10.04, −2.81) | –10.67 (−13.35, −8.00) | –5.68 (−8.73, −2.63) | –8.23 (−13.46, −3.00) | –8.01 (−12.74, −3.28) | –7.21 (−13.74, −0.68) |
| Overjet | 0.47 (−0.98, 1.91) | 1.03 (−1.04, 3.10) | –1.08 (−2.19, 0.03) | –0.75 (−1.62, 0.13) | 1.68 (−1.92, 5.29) | 0.74 (−1.99, 3.47) | –0.08 (−0.33, 0.17) |
| Overbite | 0.39 (−0.57, 1.35) | 0.81 (−0.43, 2.04) | –0.90 (−2.05, 0.25) | 0.15 (−1.86, 2.16) | 0.71 (−1.18, 2.60) | 0.66 (−0.88, 2.21) | –0.13 (−0.31, 0.05) |
| SN-OP | 1.84 (−5.15, 1.47) | 1.84 (−5.15, 1.47) | – | –0.12 (−2.36, 2.12) | –3.50 (−5.58, −1.42) | 1.84 (−5.15, 1.47) | – |
| Naslabial angle | 4.97 (–1.22, 11.17) | – | 4.97 (–1.22, 11.17) | 4.97 (–1.22, 11.17) | – | 4.97 (–1.22, 11.17) | – |
CBCT indicates cone-beam computed tomography; CCT, controlled clinical trial; N/A, not applicable; RCT, randomized controlled trial; TAD, temporary anchorage device.
Bold values indicate significant difference from the original estimates (P<0.05)
In terms of study designs, included studies were divided into two subgroups: CCTs8,11,12 and RCTs.9,10,13 Significant changes from original estimates were detected for ANB, Co-Po, and SN-MP.
For different types of TADs, two subgroups were analyzed: miniscrew8,9,13 and miniplate.10–12 The subgroup analysis revealed that ANB and Co-Po differed from original results for the subgroup of miniscrew, and ANB and SN-OP were different from original results for the miniplate subgroup.
For different modalities of radiography, the subgroup of lateral cephalometric8,12,13 and the subgroup of cone-beam computed tomography (CBCT)9–11 were available. ANB, Co-Po in the subgroup of lateral cephalometry, and SNA, ANB in the subgroup of CBCT were different from original results.
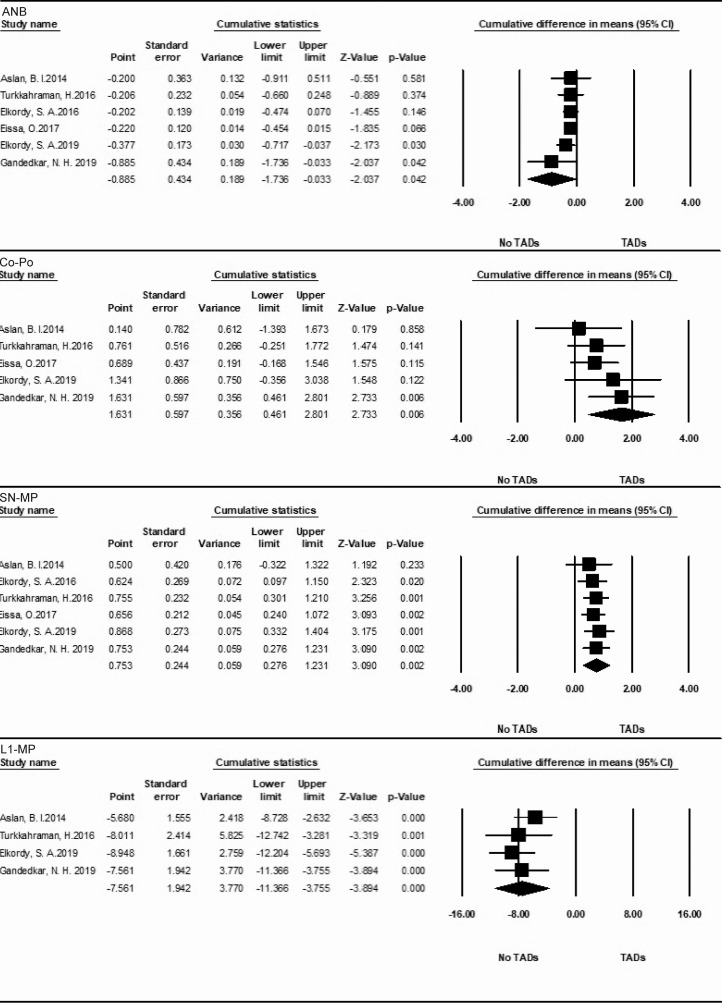
Cumulative Meta-analysis
Some of the important results of cumulative analysis are displayed in Figure 5. The results of SNA, SNB, L1-MP, overjet, SN-OP, and nasolabial angle were stable, while unstable results were found for ANB, Co-Po, SN-MP, and overbite.
Figure 5.
Cumulative meta-analysis of ANB, Co-Po, SN-MP, and L1-MP for the TAD-FFAs group versus control group.
Assessment of Publication Bias
The assessment of publication bias is shown in Table 6. Because of the limited number of studies that analyzed SN-OP and nasolabial angle, assessment of publication bias was not performed for these indices. For other indices, the Egger test and Begg test revealed no evidence of publication bias except for Co-Po.
Table 6.
Assessment of Publication Bias
| Index |
Begg Test |
Egger Test |
| SNA | 0.25966 | 0.57216 |
| SNB | 0.25966 | 0.44270 |
| ANB | 0.06029 | 0.28487 |
| Co-Po | 0.08641 | 0.00250 |
| SN-MP | 0.70711 | 0.55672 |
| L1-MP | 0.73410 | 0.13565 |
| Overjet | 0.30818 | 0.65692 |
| Overbite | 0.73410 | 0.43573 |
| SN-OP | – | – |
| Nasolabial angle | – | – |
Bold values indicate significant difference from the original estimates (P < 0.05).
DISCUSSION
In this systematic review, skeletal, dental, and soft-tissue outcomes were examined to compare the effectiveness of mandibular advancement with and without TADs. Despite heterogeneity among the studies included, subgroup analysis was performed to explore heterogeneity. Neither the Begg test nor the Egger test detected any evidence of publication bias except for Co-Po. In addition, although sensitivity and subgroup analyses revealed significant changes from original estimates, these significant changes could be explained. Thus, the results in this meta-analysis were robust.
As shown in Figure 2, the skeletal outcomes included SNA, SNB, ANB, Co-Po, and SN-MP. These skeletal outcomes could be subdivided into sagittal outcomes (SNA, SNB, ANB, and Co-Po) and vertical outcomes (SN-MP). The pooled SNA was −0.27° (95% CI: −0.59, 0.05), and sensitivity analysis revealed robust pooled results regarding SNA, indicating that the use of TADs failed to achieve additional maxillary restriction. However, the subgroup analysis on different radiographic modalities revealed that TADs could reduce SNA for the CBCT subgroup but not for the lateral cephalometric radiography subgroup (Table 5). This could be explained by the improved visualization of CBCT over lateral cephalometrics.22 Despite this, the reduction of SNA with the use of TADs for the CBCT subgroup (MD: –0.49; 95% CI: –0.90 ∼ –0.07) was of no clinical significance. Therefore, it is suggested that the additional use of TADs had no benefits in maxillary restriction compared with Forsus alone.
With regard to ANB, the meta-analysis revealed a significant difference between TADs and no TADs. Cumulative meta-analysis revealed no significant difference between TADs and no TADs before 2019, but the pooled ANB became significantly different afterward. This might be attributed to the use of miniplates. However, subgroup analysis showed no significantly different results in different types of study designs, TADs, or radiography, which indicated that the pooled result was unstable. This was in agreement with previous studies.8,9,12,13 Therefore, due to the unstable results for ANB, it cannot be determined whether Forsus + TADs could bring about more skeletal correction over Forsus only.
The pooled results regarding mandibular position were conflicting: the pooled SNB was indicative of no difference between TADs and no TADs, while the pooled Co-Po revealed a significant difference. For SNB, both sensitivity and subgroup analyses were indicative of the robustness of the pooled results (Table 5). However, sensitivity analysis on Co-Po revealed an unstable pooled result (MD: 1.34; 95% CI: −0.36 ∼ 3.04) after excluding Gandedkar et al.11 Then, subgroup analysis revealed that the results in different types of study design, TAD, and radiography were also unstable. This conflicting finding could be attributed to the instability of B point, which is not only a skeletal reference but also a dentoalveolar reference. Specifically, it has been shown that lower incisor proclination could cause an advancement of B point.23 Additionally, Forsus alone could lead to lower incisor proclination compared with the combined use of Forsus and TADs.8,10–12 It is suggested that the superiority of mandibular advancement by the combined use of Forsus and TADs could be offset by more advancement of B point (incisor proclination) by Forsus alone. Thus, due to the unstable pooled result, current evidence is unable to verify the clinical effect of TADs for mandibular advancement.
For vertical changes, a significant difference was found for SN-MP, indicating that Forsus with TADs could increase the mandibular plane angle compared with Forsus without TADs, which was in agreement with previous studies.9,10,12 The results of sensitivity analysis and subgroup analysis were mostly stable. From a biomechanical standpoint, Forsus alone caused lower incisor proclination, while Forsus with TADs avoided this side effect. As a result, the lower incisors were more upright in Forsus + TADs than in Forsus alone, which resulted in anterior occlusal interference and subsequent clockwise rotation of the mandibular plane in Forsus + TADs group. Therefore, it can be verified that Forsus with TADs can increase the mandibular angle compared with Forsus alone.
The dental outcomes including L1-MP, Overjet, Overbite and SN-OP are presented in Figure 3. There were significant results for L1-MP (MD = –7.56°, 95% CI: −11.37 ∼ −3.76), while there were no significant results for overjet, overbite and SN-OP.
Conventional Forsus exerts anterior forces on the mandibular dentition and the side effect is embodied in proclination of the lower incisors.7 The meta-analysis of L1-MP showed significant reduction of lower incisor proclination with the combination of TADs, which was consistent with previous studies.8,10–12 Both sensitivity and subgroup analyses were robust regarding the pooled results. In addition, cumulative meta-analysis showed that the pooled result was consistent with the original estimate. In particular, it is noteworthy that more reduction in incisor proclination was achieved by miniplates than miniscrews (Table 5). This could be explained by the direct (miniplate) vs indirect (miniscrew) anchorage preservation between the two modalities. Thus, it is suggested that TADs (both miniplates and miniscrews) with Forsus are able to prevent mandibular incisors from proclining compared with Forsus alone, with miniplates being more effective.
No significant results were detected for overjet and overbite, which can be explained by the requirements of study design: edge-to-edge relationship should be achieved at finish. Sensitivity and subgroup analyses were indicative of the robustness of the pooled results, so it is suggested that the additional use of TADs had no effect on overjet and overbite.
SN-OP was similar between TADs and no TADs (MD = 1.84; 95% CI: –5.15 ∼ 1.47). Interestingly, the subgroup analysis on miniplates detected a significant decrease of occlusal plane angle (MD = –3.50; 95% CI: –5.58 ∼ –1.42), while that on miniscrews did not (MD = –0.12; 95% CI: –2.36 ∼ 2.12). It was well documented that Forsus could exert intrusive forces on mandibular incisors and produce clockwise rotations of occlusal planes.24 The adjunctive use of miniplates could negate the intrusive forces of Forsus on the mandibular incisors and prevent the occlusal planes from undergoing clockwise rotation, which could produce an anticlockwise rotation of occlusal planes. This is beneficial for patients with Class II malocclusion (especially for hyperdivergent cases) needing mandibular advancement since occlusal planes are the sliding planes for mandibular advancement, and a flatter occlusal plane offers a more horizontal sliding plane for mandibular advancement. In contrast, the adjunctive use of miniscrews did not mitigate the intrusive forces on the lower incisors by Forsus and, thus, had no effect on the occlusal plane.
For soft-tissue outcomes (Figure 4), only nasolabial angle was examined among the studies included. The results revealed that the nasolabial angle was not significantly different between Forsus with and without TAD treatment. However, due to insufficient evidence, this finding should be interpreted with caution.
Limitations
In this meta-analysis, most of the studies included had a moderate sample size, but Gandedkar et al.11 had a small sample size (eight participants per group). The small sample size could cause strongly positive results and affect the pooled results. In addition, the sample sizes for quality assessment of the outcomes were small for most of the indices, and imprecision of the outcomes could be serious.
Different study designs might have had a confounding influence on the results of the outcomes. Thus, future RCTs with uniform study designs are warranted.
The included studies only examined short-term effects on mandibular advancement and dental side effects. Therefore, results of this meta-analysis cannot support conclusions on the long-term effects of Forsus with or without TADs.
CONCLUSIONS
On the basis of this review, we drew the following conclusions. However, due to the low quality of study outcomes, conclusions should be interpreted with caution:
Current evidence did not verify the additional sagittal skeletal effects of TADs in conjunction with Forsus appliances.
Forsus with TADs resulted in mandibular clockwise (opening) rotation compared with those without TADs.
Forsus with TADs could avoid lower incisor proclination; miniplates were more effective than miniscrews.
Miniplates could, while miniscrews could not, prevent the occlusal plane from being steepened.
The effects of TADs in conjunction with Forsus could not be determined for soft tissues.
ACKNOWLEDGMENTS
This study was supported by National Natural Science Foundation of China (No. 82071147, 81571004, and 81500884).
REFERENCES
- 1.Arici S, Akan H, Yakubov K, Arici N. Effects of fixed functional appliance treatment on the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133:809–814. doi: 10.1016/j.ajodo.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 2.McNamara JA., Jr Components of class II malocclusion in children 8-10 years of age. Angle Orthod. 1981;51:177–202. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Perillo L, Padricelli G, Isola G, et al. Class II malocclusion division 1: a new classification method by cephalometric analysis. Eur J Paediatr Dent. 2012;13:192–196. [PubMed] [Google Scholar]
- 4.Vaid NR, Doshi VM, Vandekar M. Class II treatment with functional appliances: a meta-analysis of short-term treatment effects. Semin Orthod. 2014;20:324–338. [Google Scholar]
- 5.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA., Jr Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599.e1–e12. doi: 10.1016/j.ajodo.2005.11.010. discussion e1–e6. [DOI] [PubMed] [Google Scholar]
- 6.Vogt W. The Forsus Fatigue Resistant Device. J Clinical Orthod. 2006;40:368–377. [PubMed] [Google Scholar]
- 7.Linjawi AI, Abbassy MA. Dentoskeletal effects of the Forsus™ fatigue resistance device in the treatment of class II malocclusion: a systematic review and meta-analysis. J Orthod Sci. 2018;7:5. doi: 10.4103/jos.JOS_80_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aslan BI, Kucukkaraca E, Turkoz C, Dincer M. Treatment effects of the Forsus Fatigue Resistant Device used with miniscrew anchorage. Angle Orthod. 2014;84:76–87. doi: 10.2319/032613-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elkordy SA, Abouelezz AM, Fayed MM, et al. Three-dimensional effects of the mini-implant-anchored Forsus Fatigue Resistant Device: a randomized controlled trial. Angle Orthod. 2016;86:292–305. doi: 10.2319/012515-55.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elkordy SA, Abouelezz AM, Fayed MMS, Aboulfotouh MH, Mostafa YA. Evaluation of the miniplate-anchored Forsus Fatigue Resistant Device in skeletal Class II growing subjects: a randomized controlled trial. Angle Orthod. 2019;89:391–403. doi: 10.2319/062018-468.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gandedkar NH, Shrikantaiah S, Patil AK, et al. Influence of conventional and skeletal anchorage system supported fixed functional appliance on maxillo-mandibular complex and temporomandibular joint: a preliminary comparative cone beam computed tomography study. Int Orthod. 2019;17:256–268. doi: 10.1016/j.ortho.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Turkkahraman H, Eliacik SK, Findik Y. Effects of miniplate anchored and conventional Forsus Fatigue Resistant Devices in the treatment of Class II malocclusion. Angle Orthod. 2016;86:1026–1132. doi: 10.2319/122515-887.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eissa O, Ei-Shennawy M, Gaballah S, El-Meehy G, El Bialy T. Treatment outcomes of Class II malocclusion cases treated with miniscrew-anchored Forsus Fatigue Resistant Device: a randomized controlled trial. Angle Orthod. 2017;87:824–833. doi: 10.2319/032717-214.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366 doi: 10.1136/bmj.l4898. l4898. [DOI] [PubMed] [Google Scholar]
- 15.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355 doi: 10.1136/bmj.i4919. i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias) J Clin Epidemiol. 2011;64:407–415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 18.Guyatt GH, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol. 2011;64:1277–1282. doi: 10.1016/j.jclinepi.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol. 2011;64:1283–1293. doi: 10.1016/j.jclinepi.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011;64:1294–1302. doi: 10.1016/j.jclinepi.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 21.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol. 2011;64:1303–1310. doi: 10.1016/j.jclinepi.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Hajeer MY, Millett DT, Ayoub AF, Siebert JP. Applications of 3D imaging in orthodontics: part I. J Orthod. 2004;31:62–70. doi: 10.1179/146531204225011346. [DOI] [PubMed] [Google Scholar]
- 23.Al-Abdwani R, Moles DR, Noar JH. Change of incisor inclination effects on points A and B. Angle Orthod. 2009;79:462–467. doi: 10.2319/041708-218.1. [DOI] [PubMed] [Google Scholar]
- 24.Linjawi AI, Abbassy MA. Dentoskeletal effects of the Forsus Fatigue Resistance Device in the treatment of class II malocclusion: a systematic review and meta-analysis. J Orthod Sci. 2018;7:5. doi: 10.4103/jos.JOS_80_17. [DOI] [PMC free article] [PubMed] [Google Scholar]