Abstract
Background
COVID-19 was first recognized in late 2019 in China, at which time school closures forced most students to isolate at home or maintain social distance, both of which increased smartphone use, daytime sleepiness and post traumatic disorder (PTSD) risks. However, to date, no research has fully explored these behavioral risks or the consequences.
Methods
Two thousand and ninety home-confined students from two Chinese high schools participated in an online-based questionnaire battery that assessed their sociodemographic characteristics, COVID-19 related exposures, daytime sleepiness, problematic smartphone use, and PTSD. The subsequent data were subjected to mediation analysis, and structural equation models (SEM) were employed to explore the variable relationships.
Results
The problematic smartphone use, daytime sleepiness and PTSD prevalence were respectively 16.4%, 20.2% and 6.9%. The number of COVID-19 related exposure was directly associated with problematic smartphone use and PTSD symptoms. Problematic smartphone use was found to be a mediator between COVID-19 related exposure and PTSD symptoms, and daytime sleepiness was found to partially mediate the associations between problematic smartphone use and PTSD.
Conclusions
The more exposure associated with the pandemic, the more psychological and behavioral problems the adolescents had. The relatively high rate of problematic smartphone use in home isolated adolescents possibly increased the risk of daytime sleepiness and psychological problems. Therefore, targeted improvements are needed to reduce the risk of psychological problems and daytime sleepiness in adolescents.
Keywords: PTSD, Adolescent, COVID-19, Daytime sleepiness, Problem smartphone use
1. Introduction
From late 2019 until 15 January 2021, COVID-19 infected about 98,329 people in China and resulted in 4,803 deaths (http://www.nhc.gov.cn, 2021). Globally, over 93 million people have been infected by COVID-19 and there have been 1,999,269 confirmed deaths as at 15 January 2021(https://www.jhu.edu, 2021). To control the COVID-19 transmissions, the Chinese Government implemented strict lock-downs and domestic quarantine policies on 21 January, 20. A nationwide school closure was put in place as an emergency measure to prevent the spread of the infection, which confined around 220 million children and adolescents to their homes according to Chinese Ministry of Education estimates. Although these measures were designed to stop the virus spread, they had a negative psychological impact on the people quarantined at home (Duan et al., 2020, Golberstein et al., 2020, Guessoum et al., 2020, Kapasia et al., 2020, Yeasmin et al., 2020, Zhou et al., 2020).
1.1. Pandemic and post-traumatic related problems
Nearly one-third of the children who experienced isolation or quarantine conditions in the areas most severely impacted by the 2009 H1N1 (swine flu) outbreak in China were found to have post-traumatic disorder (PTSD) symptoms(Sprang & Silman, 2013), and a new Italian COVID-19 study found that during the lockdown and home quarantine period in Italy, younger people were prone to anxiety, psychological distress and sleep disturbances (Casagrande, Favieri, Tambelli, & Forte, 2020). A recent Chinese study found that long-term home confinement had had significant adverse psychological impacts on adolescents from regions that had a high incidence of COVID-19 (Qu, Yang, Cao, Si, Wang, Xiu, Kosten, & Zhang, 2020), and another study found that 22.6% and 18.9% of adolescent sample had depressive or anxiety symptoms during the COVID-19 lockdown period due to a reduction in outdoor activities and peer interaction (Xie et al., 2020). In a recent Lancet paper looking at possible psychological impact of quarantine, Brooks et al. (2020) identified the main stressors during quarantine to be long quarantine duration, fear of infection, and a lack of face to face contact with social networks (Brooks et al., 2020). According to the dose of exposure model (Kaysen, Rosen, Bowman, & Resick, 2010), the more traumatic exposure, the more PTSD symptoms. Previous trauma studies on earthquakes have shown that the high-exposure group had more severe psychological problems than low- exposure group (Roussos et al., 2005). Therefore, it is hypothesized that the more relevant exposure during the COVID-19 pandemic, the more psychological problems people may have.
As many past studies have identified PTSD to be the most common psychological disorder in adolescents after disasters and trauma (Giaconia et al., 1995, McLaughlin et al., 2013), it is necessary to confirm the PTSD incidence and risk factors in adolescents in pandemic situations. Further, as it is been surmised that the COVID-19 pandemic lock-down and home-quarantine could have affected the psychological well-being of children and adolescents, it is important to understand the possible psychological consequences. A recent COVID-19 study identified females as being at a higher risk of having depressive and/or anxiety symptoms during the outbreak (Zhou et al., 2020). However, while there have been some studies on depression and anxiety prevalence in epidemic contexts (Courtney et al., 2020, Oosterhoff et al., 2020), few studies have focused on the occurrence and development of PTSD in adolescents (Li, Duan, & Chen, 2020). Therefore, a better understanding of how the pandemic lockdown affected adolescent mental health and possible PTSD prevalence could assist in guiding future prevention strategies and interventions.
1.2. Problematic smartphone use risk and adolescent home confinement during the pandemic
Home confinement significantly affected the daily activities of all people, but especially children and youth as they were unable to go to school, join extracurricular activities, have their social interactions, or enjoy outdoor physical activities. Over longer periods, changes in their regular daily activities could result in social withdrawal (Morgan et al., 2019, Palermo et al., 2004), give rise to mental health conditions, increase the risks associated with longer screen time, and further entrench problematic smartphone use. For instance, previous studies have found that on weekends and holidays children are less physically active, spend much more time on screen time and have more irregular sleep patterns than on school days (Karaca et al., 2011, Olds et al., 2019), and it has been found that adolescents in South Korea would rather spend more time on their smart devices/phones than playing sports on the weekends and holidays, thereby increasing their risk of problematic smartphone use (Lee & Kim, 2017). Therefore, it was predicted that this situation would be worse during home quarantine as the adolescents were confined to their homes and had little face to face social interactions. However, to date, there have been no comprehensive studies on the effects of home quarantine on teenage problematic smartphone use.
1.3. Daytime sleepiness as a mediator
Daytime sleepiness is the irresistible urge to fall asleep during the daytime (Johns, 2009, Pagel, 2009), and is generally the primary symptom for a chronic lack of sleep and several sleep and circadian rhythm disorders (D. A. Cohen et al., 2010, Slater and Steier, 2012). The daytime sleepiness prevalence in adolescents has been estimated to range from 9.7 to 42.7% in different countries (Joo et al., 2005, Kilincaslan et al., 2014, Wang et al., 2019). Daytime sleepiness has also been linked with a poor quality of life (Gustafsson et al., 2016) and cognitive and behavioral declines (Goodlin‐Jones, Tang, Liu, & Anders, 2009); therefore, daytime sleepiness could be an important factor in home confined adolescent populations, especially if they are heavy smartphone users as this could lead to daytime sleepiness, as found in previous studies (Chung et al., 2018, Ng et al., 2020). For example, in a sample of Hong Kong school students, the problematic smartphone users reported a greater degree of daytime sleepiness and higher depression levels (Ng et al., 2020). Therefore, sleepiness as a potential adverse consequence of problematic smartphone use in the COVID-19 pandemic lockdown required study further investigation.
Daytime sleepiness has been associated with poor daytime functioning and mental health problems. For example, a study on Chinese adolescents found that daytime sleepiness was a predictor of poor emotional and academic performance outcomes (J. Liu et al., 2016). Moreover, daytime sleepiness was observed to be a significant predictor of mood and affective states in clinical samples (Lau, Eskes, Morrison, Rajda, & Spurr, 2013). In a longitudinal study, daytime sleepiness appeared to be a significant predictor of subsequent adolescent suicidal behavior (Liu et al., 2019). Furthermore, in a one-year prospective study, daytime sleepiness was associated with possible future depression and anxiety in adolescent sample (Luo, Zhang, Chen, Lu, & Pan, 2018). Thus, due to the long period of family self-isolation during the pandemic, it was surmised that teenage problematic smartphone use prevalence would increase, which would lead to an increase in daytime sleepiness, which in turn would result in the development of psychological problems such as PTSD. It was speculated that daytime sleepiness could act as a mediator between problematic smart phone use and PTSD in young people confined to home during the pandemic. Revealing the role that daytime somnolence plays in adolescent PTSD prevalence and problematic smartphone use could possible illuminate the mechanism for psychological problems in adolescents in the pandemic context and provide favorable guidance for prevention or interventions.
Despite the increasing evidence of the high depression and anxiety prevalence in children and adolescents due to COVID-19 (Oosterhoff et al., 2020, Orgilés et al., 2020, Zhou et al., 2020), there have been no epidemiological studies investigating adolescent daytime sleepiness and limited research on problematic smartphone use and how these factors can influence the relationship between home-quarantine and mental health problems. To go some way to filling this gap, this study explored the mediating role of daytime sleepiness on problematic smartphone use and PTSD symptoms, for which it was hypothesized:
H1. Home-quarantine and higher COVID-19 related exposure is associated with a greater level of problematic smartphone use and PTSD symptoms.
H2. Problematic smartphone use increases the risk of daytime sleepiness and PTSD.
H3. Problematic smartphone use mediates the association between number of COVID-19 related exposure and PTSD.
H4. Daytime sleepiness mediates the relationship between problematic smartphone use and PTSD symptoms.
2. Methods
2.1. Participants and procedures
To assess possible behavioral, sleep and mental health problems, this cross-sectional study was conducted by online survey from February 24 to February 28, 2020 using convenience sampling. Students from two senior high schools (12–18 years old) in Leshan and Jianyang in Sichuan province were invited to participate in this online survey through the Survey Star Website. At that time, Sichuan Province was classified as a moderate COVID-19 outbreak risk, with residents having been isolated at home and practicing social distancing from January 21, 2020 and ended on March 25.
The questionnaire was first approved by the participating schools and the local education bureau, after which it was pushed to the parents through a WeChat group. After the parents' informed consent was given online and the students' consent solicited, the questionnaire was completed anonymously. To conduct the follow-up evaluations, the students needed to provide their student number and the last four digits of their parents' phone number when completing the questionnaire for later verification.
This study was reviewed and approved by the Ethics Committee of the Sichuan University and Sichuan Psychology Association, China. This survey was part of the Surveys on the Behavior and Psychological Health Project affected by the COVID-19 (SBPHP_ COVID-19). Of the total 2,399 initial participants in these two senior high schools, 2,090 completed the questionnaire, a response rate of 87.1%.
2.2. Measures
2.2.1. Demographic variables and COVID-19 related exposure
Students were asked about: their age, gender, only child status, grade level, home isolation duration since the outbreak (none, one to two weeks, two to four weeks, and more than four weeks), and one subjective and four objective COVID-19 exposure related questions derived from previous traumatic studies (Roussos et al., 2005, Tang et al., 2018), all of which required yes or no answers. These questions were: whether the epidemic in their area was serious; whether a friend or relative had been infected with COVID-19; whether they lived in a community in which someone was infected; whether they had a friend or relative who had died of COVID-19; and whether they felt extreme fear (extreme fear is the highest level of fear you can experience) because of the pandemic. The level of exposure was determined by adding up the positive items for these items.
2.2.2. Problematic smartphone use
Adolescent problematic smartphone use was measured using the Chinese version of the Mobile Phone Addiction Index (MPAI) (Huang, Niu, Zhou, & Wu, 2014), which consists of 17 items (e.g., Someone said I spend too much time on my phone in the last month.). All items are evaluated with 5-point response options from 1 = almost none, to 5 = always. The total questionnaire scores were added (Range = 17– 85), with higher scores indicating a high degree of smartphone use. This scale was applied to problematic smartphone use in the past month. A score of 51 or above indicated problematic smartphone use. The Cronbach's alpha was 0.916.
2.2.3. Daytime sleepiness
The Chinese Adolescent Daytime Sleepiness Scale (CADSS) (Liu et al., 2017) was used to evaluate the participants' daytime sleepiness in the past month (e.g., feel sleepy during the day). The CADSS consists of seven statements assessed on a 5-point Likert scale: 1 = never, 2 = rarely (<1 time/week), 3 = sometimes (1–2 times/week), 4 = often (3–5 times/week), and 5 = almost every day (6–7 times/week): that inquire about drowsiness and dozing off events at different times in the previous month, with higher CADSS scores corresponding to more severe daytime sleepiness (Range = 7– 35), with a score greater than the 16 cut-off indicating excessive daytime sleepiness (Liu et al., 2017). The Cronbach's alpha with the present sample was 0.874.
2.2.4. PTSDxxx
The Children’s Revised Impact of Event Scale (CRIES) has 13 items assessing PTSD severity in children and adolescents (Smith, Perrin, Dyregrov, & Yule, 2003) which were scored on a 4-point Likert scale from ‘‘Not At All’’ (Coded 0) to ‘‘Severely’’ (Coded 5) (Range = 0–65). These items are basically a list of common PTSD symptoms, and participants were asked to indicate how much they had been bothered by the symptom in the past month, with a score greater than 30 indicating probable PTSD. Examples of the questionnaire in our study are “Do you try not talk about COVID-19 pandemic in the last month?” or “Do you stay away from reminders of COVID-19 pandemic in the last month?”. Satisfactory psychometric properties have been reported in previous studies using CRIES with Chinese adolescents (Tang et al., 2018, Zhang et al., 2015). The Cronbach's α in the current study was 0.894.
2.3. Data analyses
Pearson’s correlation coefficient was used to examine the research variable associations, and multivariate linear regression analyses were conducted to assess the factors associated with probable PTSD or problematic smartphone use. Structural equation modelling (SEM) was used to study the relationships between problematic smartphone use, daytime sleepiness, gender, exposure and PTSD, and PROCESS was employed to run mediation analyses (Hayes, Montoya, & Rockwood, 2017) to examine the mediating effects of daytime sleepiness on the associations between problematic smartphone use and PTSD symptoms. The indirect effect of problematic smartphone use, exposure and PTSD or daytime sleepiness was also examined. The indirect effect and 95% bootstrap confidence intervals (CI) were calculated based on 5000 bootstrapped samples. The statistical analyses were conducted using SPSS version 22.0 and Amos 20.0 software.
3. Results
3.1. Sample characteristics
The mean age of the 2,090 sample (range 12–18 years old) was 16.53 (SD = 0.97) years and 1304 (62.4%) were female. The detailed sample characteristics are presented in Table 1 .
Table 1.
Study Sample Demographic Characteristics (n = 2090).
| N | % | |
|---|---|---|
| Variable | ||
| Total | 2090 | 100 |
| Age, yr | ||
| 12–15 | 314 | 15.0 |
| 16 | 691 | 33.1 |
| 17 | 727 | 34.8 |
| 18 | 358 | 17.1 |
| Gender | ||
| Male | 786 | 37.6 |
| Female | 1304 | 62.4 |
| Only child | ||
| Yes | 530 | 25.4 |
| No | 1560 | 74.6 |
| Grade | ||
| 10 | 645 | 30.9 |
| 11 | 894 | 42.8 |
| 12 | 551 | 26.3 |
| Type of exposure | ||
| Felt extremely scared | ||
| Yes | 296 | 14.2 |
| No | 1794 | 85.8 |
| Living in the worst-hit areas | ||
| Yes | 58 | 2.8 |
| No | 2032 | 97.2 |
| Friend or relative infected | ||
| Yes | 17 | 0.8 |
| No | 2073 | 99.2 |
| Someone in their community was infected | ||
| Yes | 109 | 5.2 |
| No | 1981 | 94.8 |
| Friend or relative died of COVID-19 | ||
| Yes | 3 | 0.1 |
| No | 2087 | 99.9 |
| Home- quarantine duration | ||
| 1–2 weeks | 436 | 20.9 |
| 2–4 weeks | 1313 | 62.8 |
| >4 weeks | 341 | 16.3 |
3.2. COVID-19 related exposure
Of the 2,090 participants, 14.2% (n = 296) had experienced extreme fear, most (1654, 79.1%) had experienced at least two weeks home isolation, but only a small percentage (109, 5.2%) reported that someone in their community was infected, they were living in the worst-hit areas (58, 2.8%), or a friend or relative had been infected or died (20, 0.9%). These details are also shown in Table 1.
3.3. Prevalence of mental and behavior problems and main study variable correlations
The prevalence of problematic smartphone use, daytime sleepiness and PTSD were found to be 16.4%, 20.2% and 6.9%, respectively. The correlations for the main variables are shown in Table 2 . Significant correlations were found for gender, number of exposures, daytime sleepiness, problematic smartphone use and PTSD, which indicated that subsequent regression or structural equation modeling (SEM) analyses were needed.
Table 2.
Correlations for the main study variables (N = 2090).
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Number of COVID-related exposures | 1 | −0.015* | 0.139** | 0.124** | 0.245** |
| 2. Home-quarantine duration | 1 | −0.083** | −0.033 | 0.038 | |
| 3. Daytime sleepiness | 1 | 0.358** | 0.386** | ||
| 4. Problematic smartphone use | 1 | 0.352** | |||
| 5. PTSD | 1 |
Abbreviations: PTSD, Post-traumatic stress disorder.
*p < 0.05; **p < 0.01.
3.4. Regression model results
Multiple linear regressions were conducted to identify the potential PTSD and problematic smartphone use predictors (Table 3 ). Those who had experienced extreme fear were found to be most significantly associated with PTSD or problematic smartphone use, and having someone in their community infected were also found to be associated with PTSD. Females reported greater PTSD symptoms than males.
Table 3.
Multiple regression analysis of PTSD and problematic smartphone use among adolescents (n = 2090).
| PTSD (n = 144, 6.9%) |
Problematic smartphone use (n = 342, 16.4%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficients | Unstandardized Coefficients | Standardized Coefficients | ||||
| B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | |
| Female | 2.14 | 0.46 | 0.10 | <0.001 | 0.37 | 0.60 | 0.01 | 0.539 |
| Age | −0.46 | 0.35 | −0.04 | 0.193 | −0.21 | 0.46 | −0.02 | 0.655 |
| Grade | 1.33 | 0.44 | 0.10 | 0.003 | −0.15 | 0.58 | −0.01 | 0.800 |
| Only-child | −0.33 | 0.51 | −0.01 | 0.526 | 1.02 | 0.67 | 0.03 | 0.126 |
| People infected in their communities | 2.33 | 1.00 | 0.05 | 0.020 | 2.49 | 1.30 | 0.04 | 0.057 |
| Friend or relative infected | 3.03 | 2.46 | 0.03 | 0.218 | 2.12 | 3.21 | 0.01 | 0.509 |
| Felt extreme fear | 7.78 | 0.64 | 0.258 | <0.001 | 4.17 | 0.83 | 0.11 | <0.001 |
| Living in the worst-hit areas | 2.57 | 1.36 | 0.04 | 0.058 | 2.73 | 1.77 | 0.03 | 0.123 |
| Friend or relative died of COVID-19 | −4.68 | 5.83 | −0.017 | 0.422 | −4.39 | 7.58 | −0.01 | 0.563 |
| Home-quarantine duration | 0.51 | 0.36 | 0.03 | 0.162 | −0.65 | 0.47 | −0.03 | 0.172 |
Abbreviations: PTSD, Post-traumatic stress disorder.
3.5. SEM and mediation analysis results
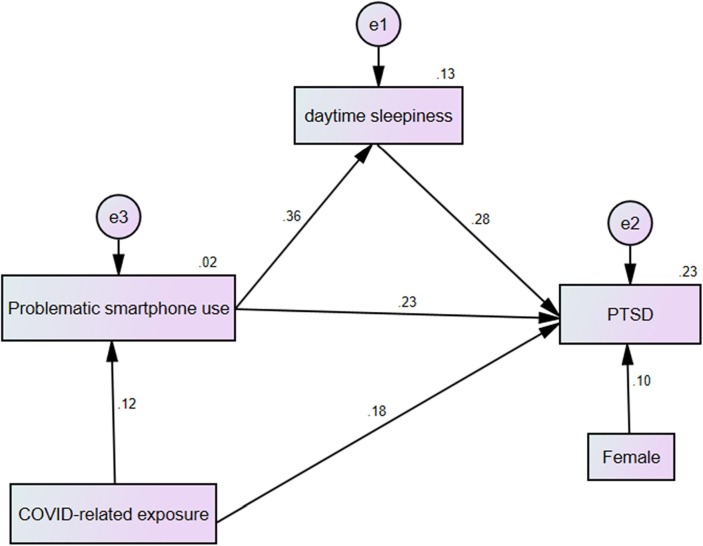
The structural equation model was found to be an acceptable fit to the data [GFI = 0.995, TLI = 0.935, NFI = 0.970, CFI = 0.974, and RMSEA = 0.072 (90%CI 0.036-0.073)] and the model was significant (χ2 = 27.75, df = 4, p < 0.001) (Fig. 1 ). Problematic smartphone use was observed to have a significant and partly indirect effect on PTSD via daytime sleepiness, that is, problematic smartphone use → daytime sleepiness (β = 0.36), and daytime sleepiness → PTSD (β = 0.28). Exposure was found to have a significant indirect effect on PTSD via problematic smartphone use, that is, exposure → smart phone addiction (β = 0.12), and smart phone addiction → PTSD (β = 0.23). Similar results were found in the mediation analysis (Table 4 ).
Fig. 1.
Path diagram showing the structural equation modeling analysis. A structural equation modeling (SEM) analysis was employed to determine the paths between COVID-related exposure, problematic smartphone use, daytime sleepiness and Post-traumatic stress disorder (PTSD). Abbreviations: PTSD, Post-traumatic stress disorder.
Table 4.
Mediation analyses to assess the direct and indirect effects between fear, daytime sleepiness, PTSD and problematic smartphone use.
| Path | Effect | SE | p | 95% CI |
|---|---|---|---|---|
| Fear(X) → Problematic smartphone use (M) → Daytime sleepiness (Y) | ||||
| Total effect of X on Y | 0.245 | 0.021 | <0.001 | 0.203–0.286 |
| Direct effect of X on Y | 0.204 | 0.020 | <0.001 | 0.165–0.244 |
| Indirect effect of X on Y | 0.041 | 0.009 | <0.001 | 0.024–0.058 |
| X → M | 0.124 | 0.022 | <0.001 | 0.082–0.167 |
| M → Y | 0.327 | 0.020 | <0.001 | 0.287–0.367 |
| Fear(X) → Problematic smartphone use (M) → PTSD (Y) | ||||
| Total effect of X on Y | 0.139 | 0.022 | <0.001 | 0.096–0.181 |
| Direct effect of X on Y | 0.096 | 0.021 | <0.001 | 0.055–0.136 |
| Indirect effect of X on Y | 0.043 | 0.009 | <0.001 | 0.026–0.062 |
| X → M | 0.124 | 0.022 | <0.001 | 0.082–0.167 |
| M → Y | 0.346 | 0.021 | <0.001 | 0.306–0.386 |
| Problematic smartphone use (X) → Daytime sleepiness (M) → PTSD(Y) | ||||
| Total effect of X on Y | 0.352 | 0.021 | <0.001 | 0.312–0.393 |
| Direct effect of X on Y | 0.246 | 0.021 | <0.001 | 0.205–0.287 |
| Indirect effect of X on Y | 0.107 | 0.012 | <0.001 | 0.085–0.131 |
| X → M | 0.358 | 0.020 | <0.001 | 0.318–0.398 |
| M → Y | 0.298 | 0.021 | <0.001 | 0.257–0.339 |
Abbreviations: PTSD, Post-traumatic stress disorder; SE, standard error; CI, confidence interval.
4. Discussion
The present study found that the problematic smartphone use, daytime sleepiness and PTSD prevalence were 16.4%, 20.2% and 6.9% in a sample of 2,092 Chinese high school students. A mediation model was constructed to determine the associations between exposure severity, problematic smartphone use and PTSD in a COVID-19 pandemic context, from which it was found that: daytime sleepiness partially mediated the association between problematic smartphone use and PTSD; COVID-19 related exposure, and especially locally infected people in the community and subjective extreme fear, increased the risk of PTSD symptoms; and problematic smartphone use mediated this relationship. Females reported a greater number of PTSD symptoms than males and more extreme subjective fear was found to be associated with problematic smartphone use. These findings extended previous research by identifying the possible processes and paths that link problematic smartphone use to PTSD symptoms in adolescents in the COVID-19 pandemic context, and more importantly, by revealing the potential mediating effect of daytime sleepiness.
It was revealed that about one in six of the adolescent participants were addicted to their smartphones during the pandemic, which was higher than the adolescent internet addiction problems (10.4%) in a random sample (n = 10158) of Chinese adolescents in 2016 (Wu et al., 2016) and much higher than another study in 2013 which found that only 6.0% were addicted (Tang et al., 2014). However, it was not possible to conclude that the pandemic lock-down and home-quarantine led to an increase in problematic smartphone use in the sample adolescents because of the lack of pre-pandemic comparisons. This study also found that the extreme subjective fear caused by the pandemic was a significant risk factor for problematic smartphone use. This may be because to assuage their fear, the participants were using their smartphones more than usual. Therefore, it could be concluded from these results that the fear caused by the pandemic increased the adolescent problematic smartphone use; however, this needs to be explored further in future studies.
Although this study found that the incidence of PTSD was low at 6.9%, it did demonstrate that in only a month after the pandemic outbreak, some adolescents were experiencing psychological effects such as pandemic-related nightmares, intrusive symptoms, flashbacks and negative emotions, all of which are the core PTSD symptoms. Past research has found that the immediate response to significantly stressful experiences typically involves intense feelings of fear, helplessness, anguish and possibly dissociative symptoms, with PTSD being the most clearly-defined trauma-induced mental disorder arising from these types of stress (Bryant, 2005). The study results were in accord with previous earthquake (Wang et al., 2011), hurricane (Galea, Tracy, Norris, & Coffey, 2008), and SARs (Wu, Chan, & Ma, 2005) trauma-related studies, all of which found that traumatic stress could have an instant psychological impact on adolescents, and concluded that it was necessary to identify early the trauma-exposed adolescents who were at a high risk of PTSD. As hypothesized, females reported a greater number of PTSD symptoms, which was also in line with previous adolescent studies on war stressors (Kolltveit et al., 2012), abuse and neglect (Ullman & Filipas, 2005), and earthquake (Geng et al., 2019) experiences. A recent study also found that females were more likely to show PTSD symptoms during the COVID-19 outbreak (Liang et al., 2020). These results highlighted the need for gender-specific interventions for pandemic-related PTSD.
It was found that problematic smartphone use mediated the association between COVID-19 related exposure and PTSD symptoms, which was in concert with a previous study that found that problematic smartphone use was significantly associated with PTSD clusters such as negative affect and arousal in trauma-exposed individuals (Contractor, Frankfurt, Weiss, & Elhai, 2017). It could be speculated, therefore, that excessive smartphone use could be as a coping mechanism for stressor-related distress such as PTSD symptoms. For instance, a previous study found that problematic smartphone use was a coping strategy for life stress in a university student sample (Chiu, 2014), and was also supported by the affective processing model that sees problematic smartphone use as a strategy to experientially avoid the negative emotions and thoughts related to traumatic events (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Therefore, in the COVID-19 context, problematic smartphone use may be an externalized and distraction-based coping method to help traumatized adolescents cope with physiological arousal and unpleasant internal/external stimuli. Further, the tendency to engage in impulsive sensation-seeking experiences by smartphone addicted adolescents has been found to be related to inhibition control deficiency (Gao et al., 2020), which could be seen to be related to the PTSD impaired fear inhibition biomarker (Jovanovic et al., 2010, van Rooij and Jovanovic, 2019). Therefore, it is possible that COVID-19 related exposure could increase excessive smartphone use, which in turn could have resulted in the development of PTSD symptoms during the COVID-19 pandemic.
The daytime sleepiness prevalence was found to be 20.2% in our sample, which was higher than reported in previous adolescent studies in Turkey (Kilincaslan et al., 2014) and Japan (Komada et al., 2016). However, the daytime sleepiness rate in this study was significantly lower than in a recent adolescent study from China (42.7%) using the same measurement tool (Wang et al., 2019). This anomaly may be due to the differences in the sample populations, such as age, gender or other risk factors (Cohen et al., 1993). For instance, in that previous study all the participants were girls (Wang et al., 2019), and the daytime sleepiness was mainly caused by menstrual irregularity and menstrual pain, while in the present study, the daytime sleepiness was mainly associated with excessive smartphone use. However, it is difficult to distinguish differences in sleepiness rates between these different samples, and future research is needed to clarify these differences.
The SEM modeling revealed that daytime sleepiness mediated the association between problematic smartphone use and PTSD. Similar results were reported in a study conducted in Hong Kong, in which it was found that daytime sleepiness mediated the relationship between problematic smartphone use and depression in adolescents (Ng et al., 2020). It is possible that problematic smartphone use could disrupt sleep–wake cycles and exacerbate normal adolescent circadian phase delay and cognitive overload, which would result in daytime sleepiness. For instance, it has been reported that excessive smartphone use has increasingly replaced zeitgeber reactions and alarm clocks (Montag et al., 2015) and therefore contributes to sleep debt and daytime sleepiness (Zion & Shochat, 2018). Problematic smartphone use has also been positively linked to cognitive failures in lower working memory capacity and poorer intentional daily life control (Hadlington, 2015) because of cognitive overload (Rutknowski & Saunders, 2019), which can lead to fatigue, exhaustion (Sert, Taskin Yilmaz, Karakoc Kumsar, & Aygin, 2019), sleep deprivation or poor sleep quality (Liu et al., 2017), which in turn would result in daytime sleepiness.
However, sleepiness could also precede PTSD symptoms. For instance, sleep disturbances such as insomnia and daytime sleepiness have also been found to be early predictors of PTSD in traumatized individuals (Koren et al., 2002, Kovachy et al., 2013). The rumination (Borders, Rothman, & McAndrew, 2015), stimulation or prolonged emotional and physical arousal from COVID-19 exposure could have exacerbated problematic smartphone use, which could have impaired executive control and suppressed negative stimuli (Nolen-Hoeksema, 2000), which in turn could have activated the development of PTSD symptoms. A recent cross-sectional study on veterans found that excessive daytime sleepiness was closely linked with PTSD (Pattinson et al., 2020), which means that daytime sleepiness increases the risk of developing PTSD in teenagers who overuse their smartphones.
Therefore, although the results in this paper are only preliminary, the study highlights the importance of the early monitoring of daytime sleepiness, especially in adolescents with PTSD symptoms. These findings could offer new insights into problematic smartphone use and negative health outcomes in adolescents in the home-confinement COVID-19 pandemic context.
4.1. Limitations and future directions
This study had several limitations, First, the study sample was from areas in which there was only a moderate risk of infections, so the results are not necessarily applicable to adolescents in other areas. Second, it is not possible to determine the causal relationships between variables in cross-sectional studies, for which longitudinal research studies are needed. Third, the research data were from self-evaluation reports; therefore, they may have been some self-report bias. In the future, both subjective and objective data should be collected to reduce bias. Fourth, the increasing use of smartphone may be related to online learning during the COVID-19 pandemic which these effects need to be taken into account in future studies. A further limitation is that we do not have information about these participants from before the pandemic and therefore you do not know the pre COVID extent of problematic smartphone use, daytime sleepiness, or PTSD symptoms in these participants. Future research needs to examine the effects of problematic smartphone use on daytime sleepiness and PTSD and the mediation between these relationships over time.
5. Conclusion and implications
Despite these limitations, there were several theoretical and practical implications. This is one of the few studies to examine the associations between COVID-19 pandemic exposure, smartphone use, daytime sleepiness and PTSD in adolescents during the COVID-19 home-confinement period in China. This study confirmed the role of subjective extreme fear on negative outcomes in previous trauma-related studies (Jovanovic et al., 2010, Wang et al., 2020) and recent COVID-19 related studies (Ornell et al., 2020, Tang et al., 2020) and found that exposure severity possibly increased the risk of excessive smartphone use in adolescents. These study results also complemented previous findings on negative somnolence (daytime sleepiness) and the behavioral consequences (problematic smartphone use) in the COVID-19 pandemic context and the emotion-related outcomes (PTSD).
The study data provides initial supporting evidence for the mediating role of daytime sleepiness on the association between excessive smartphone use and PTSD symptoms. The indirect effect found supported the notion that excessive smartphone use was more influential, which could help explain the unique contributing roles of PTSD symptoms. More importantly, the mediating role of daytime sleepiness was identified and empirical evidence provided to support the potential direct or exacerbating role of daytime sleepiness on problematic smartphone use and PTSD symptoms. These findings contribute to better understanding the process of PTSD symptoms and provide some guidance on early interventions focused on improving daytime sleepiness symptoms in adolescents with PTSD and enacting strategies or programming for parents to reduce teenage smartphone overuse to prevent negative outcomes.
6. Authorship and copyright
All authors confirm that the submitted manuscript is an original contribution and has not been previously published, that it is not under consideration for publication elsewhere, and that, if accepted, will not be published elsewhere in similar form in any language, without the consent of Elsevier B.V.. We also confirm that all authors contributed significantly to the study.
Ethical approval
All procedures complied with the ethical standards of the Research Ethics Committee of the Sichuan Psychology Association and the Research Ethics Committee of Sichuan University and the latest version of the Helsinki Declaration.
Funding
This research was supported by grants to Dr. Wanjie Tang from National Planning Office of Philosophy and Social Science of China (18BSH121).
CRediT authorship contribution statement
Tao Hu: Writing - original draft, Investigation, Data curation, Visualization, Resources, Software, Writing - review & editing. Ying Wang: Investigation, Software, Formal analysis, Writing - review & editing. Ling Lin: Investigation, Software, Formal analysis, Writing - review & editing. Wanjie Tang: Investigation, Data curation, Funding acquisition, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors wish to thank all study participants.
References
- Baker T.B., Piper M.E., McCarthy D.E., Majeskie M.R., Fiore M.C. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111(1):33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Borders A., Rothman D.J., McAndrew L.M. Sleep problems may mediate associations between rumination and PTSD and depressive symptoms among OIF/OEF veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 2015;7(1):76–84. doi: 10.1037/a0036937. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant R.A. Predicting posttraumatic stress disorder from acute reactions. Journal of Trauma & Dissociation. 2005;6(2):5–15. doi: 10.1300/J229v06n02_02. [DOI] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu S.-I. The relationship between life stress and smartphone addiction on Taiwanese university student: A mediation model of learning self-efficacy and social self-efficacy. Computers in Human Behavior. 2014;34:49–57. [Google Scholar]
- Chung J.E., Choi S.A., Kim K.T., Yee J., Kim J.H., Seong J.W., Seong J.M., Kim J.Y., Lee K.E., Gwak H.S. Smartphone addiction risk and daytime sleepiness in Korean adolescents. Journal of Paediatrics and Child Health. 2018;54(7):800–806. doi: 10.1111/jpc.13901. [DOI] [PubMed] [Google Scholar]
- Cohen P., Cohen J., Kasen S., Velez C.N., Hartmark C., Johnson J., Rojas M., Brook J., Streuning E. An epidemiological study of disorders in late childhood and adolescence—I. Age-and gender-specific prevalence. Journal of Child Psychology and Psychiatry. 1993;34(6):851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Cohen D.A., Wang W., Wyatt J.K., Kronauer R.E., Dijk D.-J., Czeisler C.A., Klerman E.B. Uncovering residual effects of chronic sleep loss on human performance. Science Translational Medicine. 2010;2(14):14ra3. doi: 10.1126/scitranslmed.3000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor A.A., Frankfurt S.B., Weiss N.H., Elhai J.D. Latent-level relations between DSM-5 PTSD symptom clusters and problematic smartphone use. Computers in Human Behavior. 2017;72:170–177. doi: 10.1016/j.chb.2017.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney D., Watson P., Battaglia M., Mulsant B.H., Szatmari P. COVID-19 impacts on child and youth anxiety and depression: Challenges and opportunities. The Canadian Journal of Psychiatry. 2020;65(10):688–691. doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Tracy M., Norris F., Coffey S.F. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2008;21(4):357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Gao L., Zhang J., Xie H., Nie Y., Zhao Q., Zhou Z. Effect of the mobile phone related-background on inhibitory control of problematic mobile phone use: An event-related potentials study. Addictive Behaviors. 2020;108:106363. doi: 10.1016/j.addbeh.2020.106363. [DOI] [PubMed] [Google Scholar]
- Geng F., Zhou Y., Liang Y., Zheng X., Li Y., Chen X., Fan F. Posttraumatic stress disorder and psychiatric comorbidity among adolescent earthquake survivors: A longitudinal cohort study. Journal of Abnormal Child Psychology. 2019;47(4):671–681. doi: 10.1007/s10802-018-0462-2. [DOI] [PubMed] [Google Scholar]
- Giaconia R.M., Reinherz H.Z., Silverman A.B., Pakiz B., Frost A.K., Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(10):1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020;174(9):819. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Goodlin-Jones B., Tang K., Liu J., Anders T.F. Sleep problems, sleepiness and daytime behavior in preschool-age children. Journal of Child Psychology and Psychiatry. 2009;50(12):1532–1540. doi: 10.1111/j.1469-7610.2009.02110.x. [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson M.L., Laaksonen C., Aromaa M., Asanti R., Heinonen O.J., Koski P., Koivusilta L., Löyttyniemi E., Suominen S., Salanterä S. Association between amount of sleep, daytime sleepiness and health-related quality of life in schoolchildren. Journal of Advanced Nursing. 2016;72(6):1263–1272. doi: 10.1111/jan.12911. [DOI] [PubMed] [Google Scholar]
- Hadlington L.J. Cognitive failures in daily life: Exploring the link with Internet addiction and problematic mobile phone use. Computers in Human Behavior. 2015;51:75–81. [Google Scholar]
- Hayes A.F., Montoya A.K., Rockwood N.J. The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australasian Marketing Journal (AMJ) 2017;25(1):76–81. [Google Scholar]
- Huang H., Niu L.-Y., Zhou C.-Y., Wu H. Reliability and validity of mobile phone addiction index for Chinese college students. Chinese Journal of Clinical Psychology. 2014;22(5):835–838. [Google Scholar]
- Johns M.W. What is excessive daytime sleepiness. Sleep Deprivation: Causes, Effects and Treatment. 2009:59–94. [Google Scholar]
- Joo S., Shin C., Kim J., Yi H., Ahn Y., Park M., Kim J., Lee S. Prevalence and correlates of excessive daytime sleepiness in high school students in Korea. Psychiatry and Clinical Neurosciences. 2005;59(4):433–440. doi: 10.1111/j.1440-1819.2005.01396.x. [DOI] [PubMed] [Google Scholar]
- Jovanovic T., Norrholm S.D., Blanding N.Q., Davis M., Duncan E., Bradley B., Ressler K.J. Impaired fear inhibition is a biomarker of PTSD but not depression. Depression and Anxiety. 2010;27(3):244–251. doi: 10.1002/da.20663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapasia N., Paul P., Roy A., Saha J., Zaveri A., Mallick R., Barman B., Das P., Chouhan P. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Children and Youth Services Review. 2020;116:105194. doi: 10.1016/j.childyouth.2020.105194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca A., Caglar E., Bilgili N., Ayaz S. Screen time of adolescents in an economically developing country: The case of Turkey. Annals of Human Biology. 2011;38(1):28–33. doi: 10.3109/03014460.2010.486383. [DOI] [PubMed] [Google Scholar]
- Kaysen D., Rosen G., Bowman M., Resick P.A. Duration of exposure and the dose-response model of PTSD. Journal of Interpersonal Violence. 2010;25(1):63–74. doi: 10.1177/0886260508329131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilincaslan A., Yilmaz K., Batmaz Oflaz S., Aydin N. Epidemiological study of self-reported sleep problems in T urkish high school adolescents. Pediatrics International. 2014;56(4):594–600. doi: 10.1111/ped.12287. [DOI] [PubMed] [Google Scholar]
- Kolltveit S., Lange-Nielsen I.I., Thabet A.A.M., Dyregrov A., Pallesen S., Johnsen T.B., Laberg J.C. Risk factors for PTSD, anxiety, and depression among adolescents in Gaza. Journal of Traumatic Stress. 2012;25(2):164–170. doi: 10.1002/jts.21680. [DOI] [PubMed] [Google Scholar]
- Komada Y., Breugelmans R., Drake C.L., Nakajima S., Tamura N., Tanaka H., Inoue S., Inoue Y. Social jetlag affects subjective daytime sleepiness in school-aged children and adolescents: A study using the Japanese version of the Pediatric Daytime Sleepiness Scale (PDSS-J) Chronobiology International. 2016;33(10):1311–1319. doi: 10.1080/07420528.2016.1213739. [DOI] [PubMed] [Google Scholar]
- Koren D., Arnon I., Lavie P., Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: A 1-year prospective study of injured survivors of motor vehicle accidents. American Journal of Psychiatry. 2002;159(5):855–857. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- Kovachy B., O'Hara R., Hawkins N., Gershon A., Primeau M.M., Madej J., Carrion V. Sleep disturbance in pediatric PTSD: Current findings and future directions. Journal of Clinical Sleep Medicine. 2013;09(05):501–510. doi: 10.5664/jcsm.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau E.Y.Y., Eskes G.A., Morrison D.L., Rajda M., Spurr K.F. The role of daytime sleepiness in psychosocial outcomes after treatment for obstructive sleep apnea. Sleep Disorders. 2013 doi: 10.1155/2013/140725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C., Kim O. Predictors of online game addiction among Korean adolescents. Addiction Research & Theory. 2017;25(1):58–66. [Google Scholar]
- Li Y., Duan W., Chen Z. Latent profiles of the comorbidity of the symptoms for posttraumatic stress disorder and generalized anxiety disorder among children and adolescents who are susceptible to COVID-19. Children and Youth Services Review. 2020;116:105235. doi: 10.1016/j.childyouth.2020.105235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of COVID-19 on youth mental health. Psychiatric Quarterly. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Liu X., Ji X., Wang Y., Zhou G., Chen X. Sleep disordered breathing symptoms and daytime sleepiness are associated with emotional problems and poor school performance in children. Psychiatry Research. 2016;242:218–225. doi: 10.1016/j.psychres.2016.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Liu Z.-Z., Wang Z.-Y., Yang Y., Liu B.-P., Jia C.-X. Daytime sleepiness predicts future suicidal behavior: A longitudinal study of adolescents. Sleep. 2019;42(2):zsy225. doi: 10.1093/sleep/zsy225. [DOI] [PubMed] [Google Scholar]
- Liu X., Yang Y., Liu Z.-Z., Chen H., Fan F., Jia C.-X. Psychometric assessment of the Chinese adolescent daytime sleepiness scale (CADSS) Sleep and Biological Rhythms. 2017;15(3):207–216. [Google Scholar]
- Luo C., Zhang J., Chen W., Lu W., Pan J. Course, risk factors, and mental health outcomes of excessive daytime sleepiness in rural Chinese adolescents: A one-year prospective study. Journal of Affective Disorders. 2018;231:15–20. doi: 10.1016/j.jad.2018.01.016. [DOI] [PubMed] [Google Scholar]
- McLaughlin K.A., Koenen K.C., Hill E.D., Petukhova M., Sampson N.A., Zaslavsky A.M., Kessler R.C. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(8):815–830.e14. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montag C., Kannen C., Lachmann B., Sariyska R., Duke É., Reuter M., Markowetz A. The importance of analogue zeitgebers to reduce digital addictive tendencies in the 21st century. Addictive Behaviors Reports. 2015;2:23–27. doi: 10.1016/j.abrep.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan K., Melendez-Torres G., Bond A., Hawkins J., Hewitt G., Murphy S., Moore G. Socio-economic inequalities in adolescent summer holiday experiences, and mental wellbeing on return to school: Analysis of the school health research network/health behaviour in school-aged children survey in Wales. International Journal of Environmental Research and Public Health. 2019;16(7):1107. doi: 10.3390/ijerph16071107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng K.C., Wu L.H., Lam H.Y., Lam L.K., Nip P.Y., Ng C.M., Leung K.C., Leung S.F. The relationships between mobile phone use and depressive symptoms, bodily pain, and daytime sleepiness in Hong Kong secondary school students. Addictive Behaviors. 2020;101:105975. doi: 10.1016/j.addbeh.2019.04.033. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109(3):504–511. [PubMed] [Google Scholar]
- Olds T., Maher C., Dumuid D. Life on holidays: Differences in activity composition between school and holiday periods in Australian children. BMC Public Health. 2019;19(2):450. doi: 10.1186/s12889-019-6765-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. Journal of Adolescent Health. 2020;67(2):179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C., & Espada, J. P. (2020). Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. [DOI] [PMC free article] [PubMed]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagel J. Excessive daytime sleepiness. American Family Physician. 2009;79(5):391–396. [PubMed] [Google Scholar]
- Palermo T.M., Witherspoon D., Valenzuela D., Drotar D.D. Development and validation of the Child Activity Limitations Interview: A measure of pain-related functional impairment in school-age children and adolescents. Pain. 2004;109(3):461–470. doi: 10.1016/j.pain.2004.02.023. [DOI] [PubMed] [Google Scholar]
- Pattinson C.L., Guedes V.A., Edwards K., Mithani S., Yun S., Taylor P., Dunbar K., Kim H.-S., Lai C., Roy M.J. Excessive daytime sleepiness is associated with altered gene expression in military personnel and veterans with posttraumatic stress disorder: An RNA sequencing study. Sleep. 2020;43(9) doi: 10.1093/sleep/zsaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu, M., Yang, K., Cao, Y., Si, T., Wang, X., Xiu, M. H., Kosten, T. R., & Zhang, X. Y. (2020). Mental Health Status of Adolescents after Family Confinement During the COVID-19 Outbreak. Available at SSRN 3594586. [DOI] [PMC free article] [PubMed]
- Roussos A., Goenjian A.K., Steinberg A.M., Sotiropoulou C., Kakaki M., Kabakos C., Karagianni S., Manouras V. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. American Journal of Psychiatry. 2005;162(3):530–537. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- Rutknowski A.F., Saunders C. Routledge; New York: 2019. Emotional and Cognitive Overload: The Dark Side of Information Technology, 1–16. [Google Scholar]
- Sert H., Taskin Yilmaz F., Karakoc Kumsar A., Aygin D. Effect of technology addiction on academic success and fatigue among Turkish university students. Fatigue: Biomedicine, Health & Behavior. 2019;7(1):41–51. [Google Scholar]
- Slater G., Steier J. Excessive daytime sleepiness in sleep disorders. Journal of Thoracic Disease. 2012;4(6):608. doi: 10.3978/j.issn.2072-1439.2012.10.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P., Perrin S., Dyregrov A., Yule W. Principal components analysis of the impact of event scale with children in war. Personality and Individual Differences. 2003;34(2):315–322. [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J., Yu Y., Du Y., Ma Y., Zhang D., Wang J. Prevalence of internet addiction and its association with stressful life events and psychological symptoms among adolescent internet users. Addictive Behaviors. 2014;39(3):744–747. doi: 10.1016/j.addbeh.2013.12.010. [DOI] [PubMed] [Google Scholar]
- Tang W., Zhao J., Lu Y., Zha Y., Liu H., Sun Y., Zhang J., Yang Y., Xu J. Suicidality, posttraumatic stress, and depressive reactions after earthquake and maltreatment: A cross-sectional survey of a random sample of 6132 Chinese children and adolescents. Journal of affective disorders. 2018;232:363–369. doi: 10.1016/j.jad.2018.02.081. [DOI] [PubMed] [Google Scholar]
- Ullman S.E., Filipas H.H. Gender differences in social reactions to abuse disclosures, post-abuse coping, and PTSD of child sexual abuse survivors. Child Abuse & Neglect. 2005;29(7):767–782. doi: 10.1016/j.chiabu.2005.01.005. [DOI] [PubMed] [Google Scholar]
- van Rooij S.J., Jovanovic T. Impaired inhibition as an intermediate phenotype for PTSD risk and treatment response. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2019;89:435–445. doi: 10.1016/j.pnpbp.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.-Y., Liu Z.-Z., Jia C.-X., Liu X. Age at menarche, menstrual problems, and daytime sleepiness in Chinese adolescent girls. Sleep. 2019;42(6):zsz061. doi: 10.1093/sleep/zsz061. [DOI] [PubMed] [Google Scholar]
- Wang B., Ni C., Chen J., Liu X., Wang A., Shao Z., Xiao D., Cheng H., Jiang J., Yan Y. Posttraumatic stress disorder 1 month after 2008 earthquake in China: Wenchuan earthquake survey. Psychiatry Research. 2011;187(3):392–396. doi: 10.1016/j.psychres.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Wang W., Wu X., Lan X. Rumination mediates the relationships of fear and guilt to posttraumatic stress disorder and posttraumatic growth among adolescents after the Ya’an earthquake. European Journal of Psychotraumatology. 2020;11(1):1704993. doi: 10.1080/20008198.2019.1704993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X.-S., Zhang Z.-H., Zhao F., Wang W.-J., Li Y.-F., Bi L., Qian Z.-Z., Lu S.-S., Feng F., Hu C.-Y. Prevalence of Internet addiction and its association with social support and other related factors among adolescents in China. Journal of Adolescence. 2016;52:103–111. doi: 10.1016/j.adolescence.2016.07.012. [DOI] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S., Banik R., Hossain S., Hossain M.N., Mahumud R., Salma N., Hossain M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: A cross-sectional study. Children and Youth Services Review. 2020;117:105277. doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Zhu S., Du C., Zhang Y. Posttraumatic stress disorder and somatic symptoms among child and adolescent survivors following the Lushan earthquake in China: A six-month longitudinal study. Journal of Psychosomatic Research. 2015;79(2):100–106. doi: 10.1016/j.jpsychores.2015.06.001. [DOI] [PubMed] [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020:1–10. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zion N., Shochat T. Cognitive functioning of female nurses during the night shift: The impact of age, clock time, time awake and subjective sleepiness. Chronobiology International. 2018;35(11):1595–1607. doi: 10.1080/07420528.2018.1497642. [DOI] [PubMed] [Google Scholar]