Abstract
Background/purpose
Multisystem inflammatory syndrome in children (MIS-C) is a potentially life-threatening condition occurring 2–6 weeks after Coronavirus disease 2019 (COVID-19) in previously healthy children and adolescents, characterized by clinical and laboratory evidence of multiorgan inflammation. We reported the case of a 6-year-old child presented with acute abdomen and then diagnosed with MIS-C. In addition, to better portray this new entity, we performed a systematic review of MIS-C gastrointestinal features and particularly on those mimicking surgical emergencies.
Methods
We described the clinical presentation, the diagnostic approach and the therapeutic outcomes of our MIS-C patient. Parallel to this, we conducted a systematic literature search using Google Scholar, PubMed, EMBASE, Scopus, focusing on gastrointestinal MIS-C.
Results
Our patient was initially assessed by the surgical team due to his query acute abdomen. Following the diagnosis of MIS-C with myocarditis, intravenous methylprednisolone (2 mg/Kg/day) and intravenous immunoglobulins (2 gr/Kg single infusion) were promptly started, leading to clinical improvement. According to our literature search, patients with MIS-C have a high rate of severe abdominal symptoms resembling surgical emergencies (appendicitis, obstruction, etc.) and a not negligible number of those patients have been surgically explored with variable findings.
Conclusions
We encourage pediatric surgeons in the upcoming months of COVID-19 pandemic to evaluate myocardial function prior to surgical abdominal exploration. In children with query acute abdomen, MIS-C should be promptly ruled out in order to avoid unnecessary surgeries that could worsen the already frail outcome of this new syndrome. Nevertheless, it should be considered that MIS-C might well encompass complications (e.g. appendicitis, segmental intestinal ischemia) which need swift surgical treatment.
Keywords: Multisystem inflammatory syndrome in children, COVID-19, Gastrointestinal, Acute abdomen, Emergency surgery
1. Introduction
Multisystem Inflammatory Syndrome in Children (MIS-C) related to SARS-CoV-2 has been increasingly reported. It could be a life-threatening condition occurring 2–6 weeks after Coronavirus disease 2019 (COVID-19), in previously healthy children and adolescents. It is characterized by fever, laboratory evidence of inflammation (including increased ferritin and IL-6) and clinically severe illness requiring hospitalization with multisystem (>2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic or neurological); moreover, no alternative plausible diagnoses should be accountable and somewhat marker for current or recent SARS-CoV-2 infection should be present (RT-PCR, serology or antigen test) or COVID-19 exposure should fall within the 4 weeks prior to the onset of symptoms (Table 1 ) [1,2].
Table 1.
Case definition for Multisystem Inflammatory Syndrome in Children (MIS-C) according to Center for Disease Control (CDC) criteria
| 1) An individual aged < 21 years with: 2) Clinical criteria:
|
Initially, MIS-C was considered as Kawasaki-like because some clinical findings were reminiscent of Kawasaki's disease (KD) [3]. However, current data evidence some difference between these two conditions, such as the age of presentation: the majority of children with KD present before 5 years of age whereas MIS-C affects older children, with a mean age of 8 years [4].
Gastrointestinal symptoms are the most common clinical manifestations of MIS-C (87% of children), followed by muco-cutaneous (73%), cardiovascular (71%), respiratory (47%) and neurologic symptoms in 22% [5].
Abdominal pain, vomiting and diarrhea are particularly common and prominent, with the presentation in some children mimicking acute abdomen. Some children have been noted to have mesenteric adenitis, terminal ileitis and/or colitis on abdominal imaging [[6], [7], [8]]. An increasing number of children referred for suspected appendicitis or acute abdomen are subsequently diagnosed as MIS-C, often after undergoing surgery or after needing intensive care [9,10]. Cardiac involvement includes ventricular dysfunction, coronary artery dilation or aneurysm, and arrhythmias [11].
Coronary arteries may not be frequently affected in the acute phase and in the early follow-up period of MIS-C. The major finding during the acute phase of MIS-C is a myocarditis-like picture, which may remain subtle and subclinical [12].
Severe pulmonary involvement (e.g. acute respiratory distress syndrome) is rather uncommon; however, when present, respiratory symptoms (tachypnea, dyspnea) are most often due to severe shock [13,14].
Neurocognitive symptoms are also frequent and may include headache, lethargy, confusion or irritability. A minority of patients presents with more severe neurologic manifestations, including encephalopathy, seizures, coma, meningoencephalitis, muscle weakness and brainstem/cerebellar signs [15].
Herein we describe a new case of MIS-C presenting as acute abdomen and we outline a systematic review of the available literature on abdominal features of this condition.
The practical aim of this work is specifically to highlight MIS-C presenting as acute abdomen, a truly diagnostic and therapeutic dilemma for both pediatric surgeons and pediatric emergency physicians in the COVID-19 era.
LIST OF ABBREVIATION: MIS-C: Multisystem inflammatory syndrome in children; COVID-19: Coronavirus disease 2019; RT-PCR: Reverse transcriptase-polymerase chain reaction; KD: Kawasaki's disease; pAMY: pancreatic amylase; LDH: Lactate dehydrogenase; CPK: creatine phosphokinase; CDC: Centers for Disease Control; BNP: B Natriuretic Peptide; IL-6: interleukin 6.
2. Case presentation
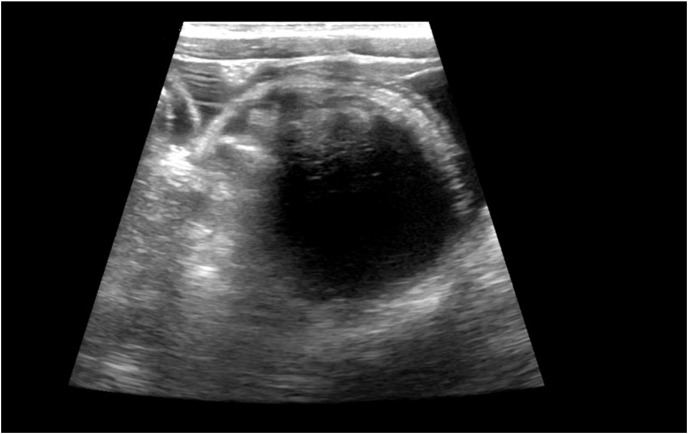
We report the case of a 6-year-old child who was admitted to a secondary-care hospital for fever (up to 40 °C) lasting for five days and intermittent diarrhea. At admission he was pale, with palmar hyperemia; he presented regular cardio-respiratory activity, tense and painful abdomen, with signs of defense in the lower right quadrant; no lymphadenopathy was detected. Sars-Cov-2 testing through both antigenic and molecular nasopharyngeal swab resulted negative. Laboratory tests showed white blood cell count 7850/μL (neutrophils 83%, lymphocytes 10.6%), Hb 11.1 g/dl, platelets 114000/μL, Na+ 126 mEq/L, K+ 3.5 mEq/L, procalcitonin 14.6 ng/mL, C-reactive protein 16.10 mg/dl, fibrinogen 518 mg/dl, albumin 3.5 g/dl, liver function tests were within normal range. Anti- Sars-Cov-2 IgG antibodies were found positive. Ultrasonography evaluation of the abdomen highlighted free pelvic fluid and a non-visible appendix; a plain X-ray showed multiple hydro-aerial levels. This imaging, combined to clinical features and increased inflammatory indices, left the query appendicitis unsolved (Fig. 1 A and B).
Fig. 1.
1A. X-Ray showing marked bowel distension due to paralytic ileus; 1B: US showing free fluid in the pelvis (appendix not visible).
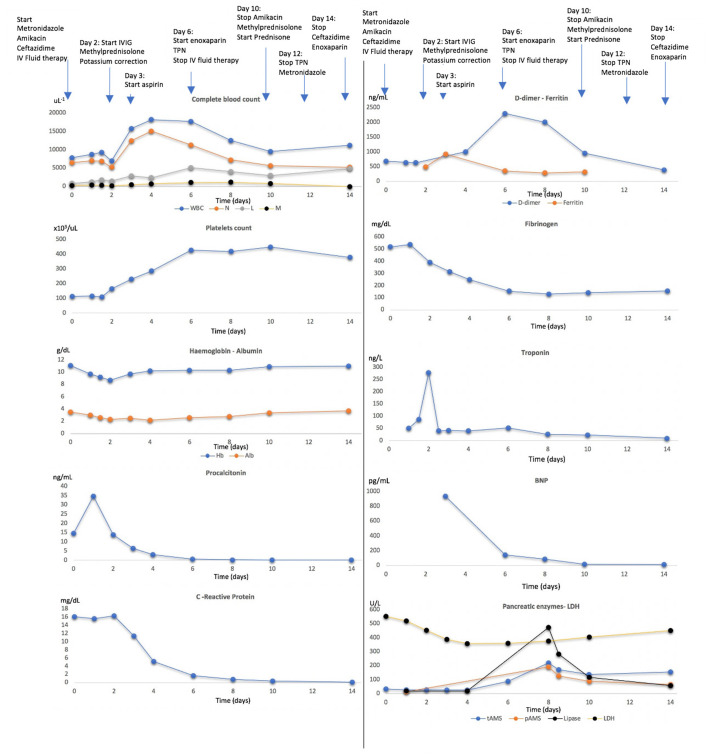
Surgical consult suggested to prescribe i.v. Ceftazidime, Amikacin and Metronidazole along with watchful monitoring. Given his clinical worsening, a CT scan was performed, showing gas distension of the small bowel and free pelvic fluid; incidentally, pleural and pericardial effusions were found at once. The ECG showed an inversion of T wave. A cardiac ultrasound revealed a slight reduction in the ejection fraction (52%); all coronaries had normal diameter. Testing for cardiac cytolysis enzyme revealed increasing Troponin (278 ng/L), increased B-Natriuretic peptide (935 pg/ml) but normal LDH (551 IU/L) and CPK-mb (3.9 ng/ml). Therefore, MIS-C was highly suspicious and he underwent medical treatment with Methylprednisolone (2 mg/Kg/day) and intravenous immunoglobulins (2 gr/Kg single infusion), on the basis of reported guideline [1], with progressive clinical and biochemical improvement. Laboratory tests over time were summarized in Fig. 2 .
Fig. 2.
Biochemical parameters in response to supportive therapies. TPN: total parenteral nutrition. IV: intravenous.
Although the clinical condition improved and cardiac function fully restored, he presented a persistent tense abdomen and weak peristalsis. Due to the lack of bowel movements and feeding intolerance, he received parenteral nutrition for 7 days. On day 8, we observed transient elevation of pancreatic enzymes (pAMY 192 IU/L lipase 474 IU/L). Liver and renal function remained within the normal range. As D-dimer increased (2311 ng/ml), he was started on subcutaneous Enoxaparin. After day 12 of hospital stay, the patient was able to fully tolerate oral feeding and was discharged with aspirin (3 mg/kg/day) and oral Prednisone (2 mg/kg/day) then tapered in 15 days. Two weeks after discharge laboratory parameters, ECG, echocardiography and abdomen ultrasound were normal.
Serum IL-6 was tested on serum samples collected at entry and after treatment (297.4 pg/ml and 3.42 pg/ml, respectively; reference range 5.3–7.5 pg/ml).
3. Search strategy and selection criteria
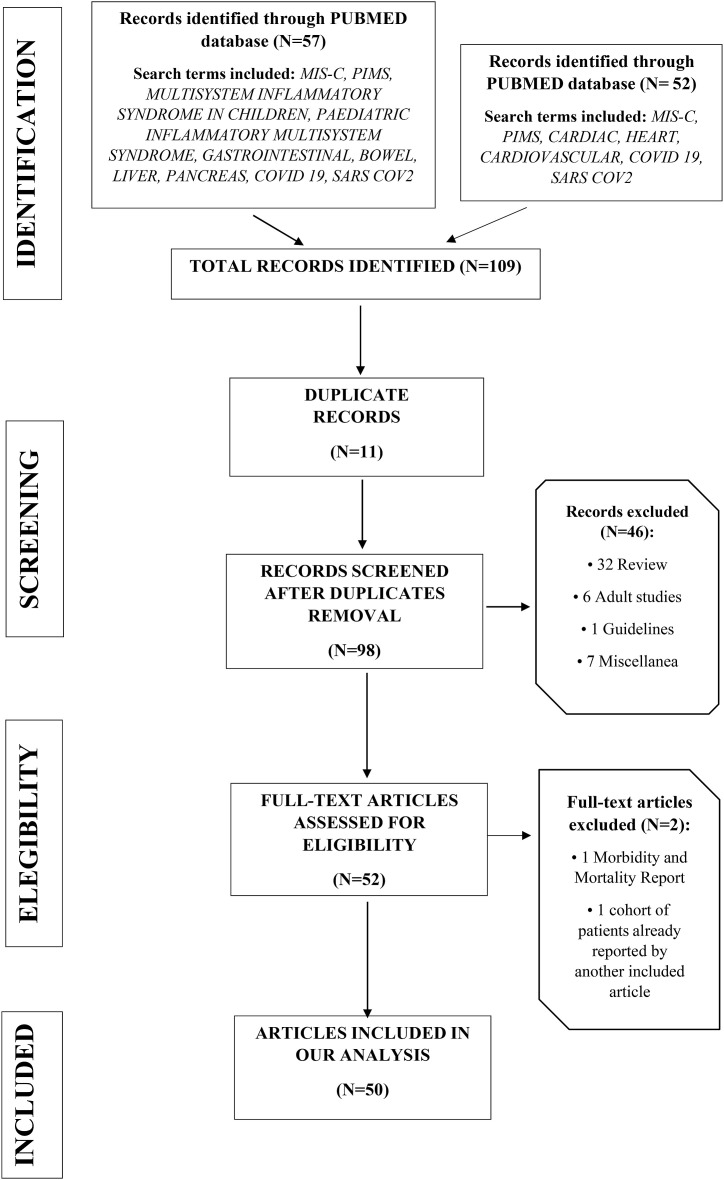
The literature research was conducted from November 27 to January 27 on Google Scholar, Pub Med, EMBASE, Scopus using key-words as follows (Table 2 ):MIS-C; PIMS; Multisystem inflammatory syndrome in children; pediatric inflammatory multisystem syndrome; cardiac; hearth; cardiovascular; gastrointestinal; bowel; liver; pancreas.
Table 2.
Flow diagram regarding study selection.
4. Results
A total of 109 articles was retrieved from two authors blinded search, of which eleven were duplicate. Forty-eight were excluded as they were reviews, adult studies (>18 years), guidelines, commentaries, letters, morbidity/mortality report, case-series already reported in another paper included. A final set of 50 articles were suitable for the scope of our review.
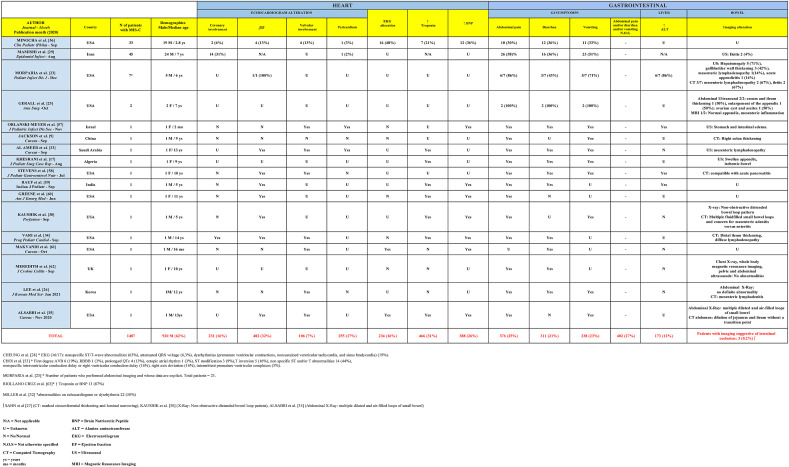
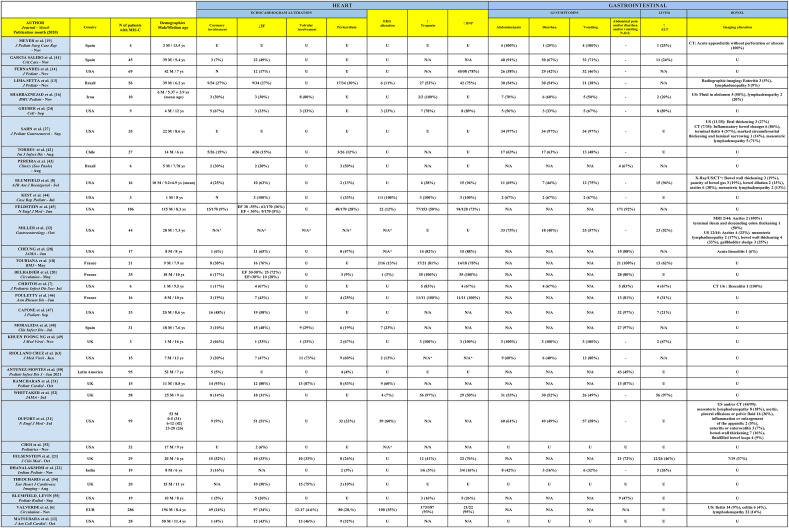
Main clinical features of MIS-C reported patients are summarized (Table 3 ).
Table 3.
When focusing on severe abdominal manifestations, we found nine patients affected by MIS-C who underwent exploratory laparotomies: two children with a healthy appendix as finding (“pseudo appendicular syndrome”) [16,17], one with aseptic peritonitis [18], four with appendicitis [19] and two with mesenteric lymphadenitis [20]. Appendicitis was initially suspected in roughly 5–30% [16,18,[20], [21], [22], [23], [24]] of the reviewed case series and in four case reports [9,17,25,26]. Three patients underwent intestinal resection with re-anastomosis due to segmental inflammation with necrosis of terminal ileum [9,17,27].
When considering imaging studies, ileitis or colitis were present approximately in 4–28% of cases [6,7,13,23,[27], [28], [29], [30], [31]]. Moreover, a diagnosis of mesenteric adenitis in MIS-C has been accounted by 8 case-series, with a prevalence of 9–20% of the abdominal imaging studies [6,8,13,16,23,27,31,32]. In addition, the latter condition has been also described in six recent case-reports from different geographic areas [9,25,26,30,33,34]: notably, in one of those patients mesenteric lymphadenitis was even confirmed on surgical specimens by pathologists [9].
Vomiting and diarrhea were common presenting features, respectively in 23% and 21% of patients from the available literature.
Albeit predominant in our patient, intestinal occlusion was far less common and has been reported in 3 other patients so far [27,30,35].
5. Discussion
The impact of COVID-19 on pediatric population can be considered relatively milder than adults [36]. Furthermore, the concern of contracting Covid-19, stay-at-home orders and population lockdowns have brought to a massive decrease of hospital accesses for children [37]. Notwithstanding this, the fear of SARS-CoV-2 has often delayed pediatric consultations, thus leading to worse clinical outcomes [38].
In this epidemiological framework, an increasing number of children has been described with a severe inflammatory disease characterized by fever, hyperinflammation and multiorgan involvement as short-medium term consequence of Sars-Cov2 infection, namely MIS-C. It is important to note that this newly recognized syndrome is most frequently post-infectious (related to an immune dysregulation induced by the virus, i.e. molecular mimicry) rather than related to acute infection [39].
According to CDC criteria [2], our patient could be fully labeled as MIS-C with acute abdomen and early myocarditis.
In this review of the literature, we summarized the features of MIS-C with a special focus on gastrointestinal involvement, thus addressing the need for an appropriate differential diagnosis both in the Emergency Room and during the early stages of hospital stay.
Quite surprisingly, in fact, patients with MIS-C have a high rate of gastrointestinal complaints.
Several authors reported acute abdomen presentation in a not negligible number of patients. Our systematic review of literature evidenced acute abdomen presentation up to 30% [16,18,[20], [21], [22], [23], [24]]. It is attractive to speculate that vascular damage could probably play a role as well with this regard. Indeed, Khesrani et al. reported a case of ischemic lesions complicating MIS-C syndrome and formulated the hypothesis of an underlying severe intestinal vasculitis [17].
A case report by Cazzaniga et al. described a child with KD complicated by the onset of paralytic ileus: this patient also resulted positive for SARS-COV-2 and his X-ray showed ileocolic meteorism with diffuse air-fluid levels, compatible indeed with paralytic ileus associated to intestinal vasculopathy [40]. Nonetheless, it should be noted that this case was not an outcome of our search nor present in Table 3 because classified as KD rather than MIS-C.
In our opinion, for these unclear cases it is definitely valuable a period of watchful monitoring in a hospital setting. Subsequently, if the clinical picture does not improve, a different abdominal imaging might be required. Should patient's clinical status worsen further, an extensive abdominal imaging (MR angiogram preferably or CT angiogram) must be considered, as well as to promptly establish the best treatment and to avoid complications.
Given the high rate of severe abdominal symptoms resembling surgical emergencies (query appendicitis or obstruction) in MIS-C, we encourage pediatric surgeons in the upcoming months to evaluate myocardial function prior to surgical abdominal exploration. Few laboratory and imaging tools should become full part of the initial diagnostic panoply. A preliminary assessment of troponin, BNP, D-Dimer, ferritin and echocardiography are definitely of value to establish a precise differential diagnosis in children with acute abdomen, as it was in our case. Considering the high overlap between gastrointestinal and cardiac involvement in MIS-C, evolution towards cardiogenic shock should not be neglected, especially when avoidable surgery might worsen its already frail outcomes. Nevertheless, it must be acknowledged that several cases of MIS-C do evolve in insidious surgical complications such as appendicitis and vasculopathy-related segmental intestinal infarction. Rather than being ancillary, the role of pediatric surgeons in MIS-C is thus key and so it will be in the months ahead of current pandemic.
In conclusion, the awareness on the high rate of gastrointestinal complaints in MIS-C is definitely an added value for both pediatricians and pediatric surgeons. A multidisciplinary approach is more than desirable for these children, with both team's side-by-side against possible confounders and hazardous complications, always aiming to the best therapeutic outcome.
Author statement
Study conception and design: Francesco Valitutti, Angela Pepe, Claudia Mandato
Data acquisition: Edoardo Sorrentino, Deborah Veneruso, Giusy Ranucci
Analysis and data interpretation: Angela Pepe, Alessandre Verde,Edoardo Sorrentino, Deborah Veneruso, Francesca Orlando, Augusto Mastrominico, Mia Giovanna Grella, Giusy Ranucci
Drafting of the manuscript: Francesco Valitutti, Angela Pepe, Alessandre Verde, Claudia Mandato
Critical revision: Augusto Mastrominico, Mia Giovanna Grella, Francesca Orlando Submit this form with the manuscript.
Funding
The APC for this project was supported by the regional fund POR FESR CAMPANIA 2014-2020 – G58D20000240002.
Patient Consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Declaration of competing interest
All the authors have no interest to disclose.
Acknowledgements
All the authors warmly thank Prof. Pietro Vajro for his expert supervision and fruitful discussion on both patient case and manuscript preparation. The authors thank the regional fund POR FESR CAMPANIA 2014-2020 (G58D20000240002) for the support of the APC.
References
- 1.Henderson L.A., Canna S.W., Friedman K.G., et al. American college of rheumatology clinical guidance for pediatric patients with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 and hyperinflammation in COVID-19. Version 2. Arthritis Rheum. 2020 doi: 10.1002/art.41616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Emergency preparedness and response: health alert network. 2020. https://emergency.cdc.gov/han/2020/han00432.asp
- 3.Henderson L.A., Yeung R.S.M. MIS-C: early lessons from immune profiling. Nat Rev Rheumatol. 2020:1–2. doi: 10.1038/s41584-020-00566-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Health department-reported cases of multisystem inflammatory syndrome in children (MIS-C) in the United States. 2021. https://www.cdc.gov/mis-c/cases/index.html
- 5.Abrams J.Y., Godfred-Cato S.E., Oster M.E., et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2: a systematic review. J Pediatr. 2020;226:45–54. doi: 10.1016/j.jpeds.2020.08.003. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valverde I., Singh Y., Sanchez-de-Toledo J., et al. Acute cardiovascular manifestations in 286 children with multisystem inflammatory syndrome associated with COVID-19 infection in europe. Circulation. 2021;143:21–32. doi: 10.1161/CIRCULATIONAHA.120.050065. [DOI] [PubMed] [Google Scholar]
- 7.Chiotos K., Bassiri H., Behrens E.M., et al. Multisystem inflammatory syndrome in children during the coronavirus 2019 pandemic: a case series. J Pediatric Infect Dis Soc. 2020;9:393–398. doi: 10.1093/jpids/piaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blumfield E., Levin T.L., Kurian J., et al. Imaging findings in multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease (COVID-19) AJR Am J Roentgenol. 2020:1–11. doi: 10.2214/AJR.20.24032. [DOI] [PubMed] [Google Scholar]
- 9.Jackson R.J., Chavarria H.D., Hacking S.M. A case of multisystem inflammatory syndrome in children mimicking acute appendicitis in a COVID-19 pandemic area. Cureus. 2020;12 doi: 10.7759/cureus.10722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tullie L., Ford K., Bisharat M., et al. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. Lancet Child Adolesc Health. 2020;4:e19–e20. doi: 10.1016/S2352-4642(20)30165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sperotto F., Friedman K.G., Son M.B.F., et al. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. Eur J Pediatr. 2021;180:307–322. doi: 10.1007/s00431-020-03766-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsubara D., Kauffman H.L., Wang Y., et al. Echocardiographic findings in pediatric multisystem inflammatory syndrome associated with COVID-19 in the United States. J Am Coll Cardiol. 2020;76:1947–1961. doi: 10.1016/j.jacc.2020.08.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lima-Setta F., Magalhães-Barbosa M.C., Rodrigues-Santos G., et al. Multisystem inflammatory syndrome in children (MIS-C) during SARS-CoV-2 pandemic in Brazil: a multicenter, prospective cohort study. J Pediatr. 2020 doi: 10.1016/j.jped.2020.10.008. S0021-7557:30225-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernandes D.M., Oliveira C.R., Guerguis S., et al. Severe acute respiratory syndrome coronavirus 2 clinical syndromes and predictors of disease severity in hospitalized children and youth. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.11.016. S0022-3476:31393-31397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin J.E., Asfour A., Sewell T.B., et al. Neurological issues in children with COVID-19. Neurosci Lett. 2020;743:135567. doi: 10.1016/j.neulet.2020.135567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahbaznejad L., Navaeifar M.R., Abbaskhanian A., et al. Clinical characteristics of 10 children with a pediatric inflammatory multisystem syndrome associated with COVID-19 in Iran. BMC Pediatr. 2020;20:513. doi: 10.1186/s12887-020-02415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khesrani L.S., Chana K., Sadar F.Z., et al. Intestinal ischemia secondary to Covid-19. J Pediatr Surg Case Rep. 2020;61:101604. doi: 10.1016/j.epsc.2020.101604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toubiana J., Poirault C., Corsia A., et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. doi: 10.1136/bmj.m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer J.S., Robinson G., Moonah S., et al. Acute appendicitis in four children with SARS-CoV-2 infection. J Pediatr Surg Case Rep. 2021;64:101734. doi: 10.1016/j.epsc.2020.101734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Belhadjer Z., Méot M., Bajolle F., et al. Acute heart failure in multisystem inflammatory syndrome in children in the context of global SARS-CoV-2 pandemic. Circulation. 2020;142:429–436. doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- 21.Felsenstein S., Willis E., Lythgoe H., et al. Presentation, treatment response and short-term outcomes in paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS) J Clin Med. 2020;9:3293. doi: 10.3390/jcm9103293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhanalakshmi K., Venkataraman A., Balasubramanian S., et al. Epidemiological and clinical profile of pediatric inflammatory multisystem syndrome - temporally associated with SARS-CoV-2 (PIMS-TS) in Indian children. Indian Pediatr. 2020;57:1010–1014. doi: 10.1007/s13312-020-2025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morparia K., Park M.J., Kalyanaraman M., et al. Abdominal imaging findings in critically ill children with multisystem inflammatory syndrome associated with COVID-19. Pediatr Infect Dis J. 2020;40:e82–e83. doi: 10.1097/INF.0000000000002967. [DOI] [PubMed] [Google Scholar]
- 24.Gruber C., Patel R., Trachman R., et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C) Cell. 2020;183:982–995. doi: 10.1016/j.cell.2020.09.034. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gerall C.D., Duron V.P., Griggs C.L., et al. Multisystem inflammatory syndrome in children mimicking surgical pathologies: what surgeons need to know about MIS-C. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004368. [DOI] [PubMed] [Google Scholar]
- 26.Lee J.H., Han H.S., Lee J.K. The importance of early recognition, timely management, and the role of healthcare providers in multisystem inflammatory syndrome in children. J Kor Med Sci. 2021;36:e17. doi: 10.3346/jkms.2021.36.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sahn B., Eze O.P., Edelman M.C., et al. Features of intestinal disease associated with COVID-related multisystem inflammatory syndrome in children. J Pediatr Gastroenterol Nutr. 2020 doi: 10.1097/MPG.0000000000002953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheung E.W., Zachariah P., Gorelik M., et al. Multisystem inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York city. J Am Med Assoc. 2020;324:294–296. doi: 10.1001/jama.2020.10374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mamishi S., Movahedi Z., Mohammadi M., et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. 2020;148:e196. doi: 10.1017/S095026882000196X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaushik S., Ahluwalia N., Gangadharan S., et al. ECMO support in SARS-CoV2 multisystem inflammatory syndrome in children in a child. Perfusion. 2020 doi: 10.1177/0267659120954386. 267659120954386. [DOI] [PubMed] [Google Scholar]
- 31.Dufort E.M., Koumans E.H., Chow E.J., et al. Multisystem inflammatory syndrome in children in New York state. N Engl J Med. 2020;383:347–358. doi: 10.1056/NEJMoa2021756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller J., Cantor A., Zachariah P., et al. Gastrointestinal symptoms as a major presentation component of a novel multisystem inflammatory syndrome in children that is related to coronavirus disease 2019: a single center experience of 44 cases. Gastroenterology. 2020;159:1571–1574. doi: 10.1053/j.gastro.2020.05.079. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al Ameer H.H., AlKadhem S.M., Busaleh F., et al. Multisystem inflammatory syndrome in children temporally related to COVID-19: a case report from Saudi arabia. Cureus. 2020;12 doi: 10.7759/cureus.10589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vari D., Miller J.M., Rellosa N., et al. Severe cardiac dysfunction in a patient with multisystem inflammatory syndrome in children associated with COVID-19: retrospective diagnosis of a puzzling presentation. A case report. Prog Pediatr Cardiol. 2020;58:101270. doi: 10.1016/j.ppedcard.2020.101270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alsabri M., Sakr M., Qarooni S., et al. COVID-19 infection in a child presenting with functional intestinal obstruction. Cureus. 2020;12:e11448. doi: 10.7759/cureus.11448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cruz A.T., Zeichner S.L. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0834. [DOI] [PubMed] [Google Scholar]
- 37.Valitutti F., Zenzeri L., Mauro A., et al. Effect of population lockdown on pediatric emergency Room demands in the era of COVID-19. Front Pediatr. 2020;8:521. doi: 10.3389/fped.2020.00521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lazzerini M., Barbi E., Apicella A., et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakra N.A., Blumberg D.A., Herrera-Guerra A., et al. Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management. Children. 2020;7:69. doi: 10.3390/children7070069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cazzaniga M., Baselli L.A., Cimaz R., et al. SARS-COV-2 infection and Kawasaki disease: case report of a hitherto unrecognized association. Front Pediatr. 2020;8:398. doi: 10.3389/fped.2020.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.García-Salido A., de Carlos Vicente J.C., Belda Hofheinz S., et al. Severe manifestations of SARS-CoV-2 in children and adolescents: from COVID-19 pneumonia to multisystem inflammatory syndrome: a multicentre study in pediatric intensive care units in Spain. Crit Care. 2020;24:666. doi: 10.1186/s13054-020-03332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Torres J.P., Izquierdo G., Acuña M., et al. Multisystem inflammatory syndrome in children (MIS-C): report of the clinical and epidemiological characteristics of cases in Santiago de Chile during the SARS-CoV-2 pandemic. Int J Infect Dis. 2020;100:75–81. doi: 10.1016/j.ijid.2020.08.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pereira M.F.B., Litvinov N., Farhat S.C.L., et al. Severe clinical spectrum with high mortality in pediatric patients with COVID-19 and multisystem inflammatory syndrome. Clinics. 2020;75 doi: 10.6061/clinics/2020/e2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kest H., Kaushik A., DeBruin W., et al. Multisystem inflammatory syndrome in children (MIS-C) associated with 2019 novel coronavirus (SARS-CoV-2) infection. Case Rep Pediatr. 2020;2020:8875987. doi: 10.1155/2020/8875987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feldstein L.R., Rose E.B., Horwitz S.M., et al. Multisystem inflammatory syndrome in U.S. Children and adolescents. N Engl J Med. 2020;383:334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pouletty M., Borocco C., Ouldali N., et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020;79:999–1006. doi: 10.1136/annrheumdis-2020-217960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Capone C.A., Subramony A., Sweberg T., et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020;224:141–145. doi: 10.1016/j.jpeds.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moraleda C., Serna-Pascual M., Soriano-Arandes A., et al. Multi-inflammatory syndrome in children related to SARS-CoV-2 in Spain. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ng K.F., Kothari T., Bandi S., et al. COVID-19 multisystem inflammatory syndrome in three teenagers with confirmed SARS-CoV-2 infection. J Med Virol. 2020;92:2880–2886. doi: 10.1002/jmv.26206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Antúnez-Montes O.Y., Escamilla M.I., Figueroa-Uribe A.F., et al. COVID-19 and multisystem inflammatory syndrome in Latin American children: a multinational study. Pediatr Infect Dis J. 2021;40:e1–e6. doi: 10.1097/INF.0000000000002949. [DOI] [PubMed] [Google Scholar]
- 51.Ramcharan T., Nolan O., Lai C.Y., et al. Paediatric inflammatory multisystem syndrome: temporally associated with SARS-CoV-2 (PIMS-TS): cardiac features, management and short-term outcomes at a UK tertiary paediatric hospital. Pediatr Cardiol. 2020;41:1391–1401. doi: 10.1007/s00246-020-02391-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Whittaker E., Bamford A., Kenny J., et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. J Am Med Assoc. 2020;324:259–269. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Choi N.H., Fremed M., Starc T., et al. MIS-C and cardiac conduction abnormalities. Pediatrics. 2020;146 doi: 10.1542/peds.2020-009738. [DOI] [PubMed] [Google Scholar]
- 54.Theocharis P., Wong J., Pushparajah K., et al. Multimodality cardiac evaluation in children and young adults with multisystem inflammation associated with COVID-19. Eur Heart J Cardiovasc Imaging. 2020 doi: 10.1093/ehjci/jeaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blumfield E., Levin T.L. COVID-19 in pediatric patients: a case series from the Bronx, NY. Pediatr Radiol. 2020;50:1369–1374. doi: 10.1007/s00247-020-04782-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Minocha P.K., Phoon C.K.L., Verma S., et al. Cardiac findings in pediatric patients with multisystem inflammatory syndrome in children associated with COVID-19. Clin Pediatr. 2020 doi: 10.1177/0009922820961771. 9922820961771. [DOI] [PubMed] [Google Scholar]
- 57.Orlanski-Meyer E., Yogev D., Auerbach A., et al. Multisystem inflammatory syndrome in children associated with SARS-CoV-2 in an 8-week old infant. J Pediatric Infect Dis Soc. 2020 doi: 10.1093/jpids/piaa137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stevens J.P., Brownell J.N., Freeman A.J., et al. COVID-19-Associated multisystem inflammatory syndrome in children presenting as acute pancreatitis. J Pediatr Gastroenterol Nutr. 2020 doi: 10.1097/MPG.0000000000002860. [DOI] [PubMed] [Google Scholar]
- 59.Rauf A., Vijayan A., John S.T., et al. Multisystem inflammatory syndrome with features of atypical Kawasaki disease during COVID-19 pandemic. Indian J Pediatr. 2020;87:745–747. doi: 10.1007/s12098-020-03357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Greene A.G., Saleh M., Roseman E., et al. Toxic shock-like syndrome and COVID-19: multisystem inflammatory syndrome in children (MIS-C) Am J Emerg Med. 2020;38:2492. doi: 10.1016/j.ajem.2020.05.117. e5-e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Makvandi S., Alibrahim O., Abdul-Aziz R., et al. A rare presentation of multi-system inflammatory disease in children associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Cureus. 2020;12 doi: 10.7759/cureus.10892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meredith J., Khedim C.A., Henderson P., et al. Paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in a patient receiving infliximab therapy for inflammatory bowel disease. J Crohns Colitis. 2020 doi: 10.1093/ecco-jcc/jjaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Riollano-Cruz M., Akkoyun E., Briceno-Brito E., et al. Multisystem inflammatory syndrome in children related to COVID-19: a New York City experience. J Med Virol. 2020 doi: 10.1002/jmv.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]