Abstract
Purpose:
Health insurance reimbursement structure has evolved with patients becoming increasingly responsible for their healthcare costs through rising out-of-pocket (OOP) expenses. High levels of cost sharing can lead to delays in access to care, influence treatment decisions, and cause financial distress for patients.
Methods:
Patients undergoing the most common outpatient reconstructive plastic surgeries were identified using Truven MarketScan databases from 2009–2017. Total cost of the surgery paid to the insurer and OOP expenses, including deductible, copayment, and coinsurance, were calculated. Multivariable generalized linear modelling with log link and gamma distribution was used to predict adjusted total and OOP expenses. All costs were inflation adjusted to 2017 dollars.
Results:
We evaluated 3,181,125 outpatient plastic and reconstructive surgical procedures between 2009 and 2017. From 2009 to 2017, total costs had a significant increase of 23%, and OOP expenses had a significant increase of 54%. Using generalized linear modeling, procedures performed in outpatient hospitals conferred an additional $1,999 in total costs (95%CI: $1,978-$2,020) and $259 in OOP expenses (95%CI: $254-$264) compared to office procedures. Ambulatory surgical center procedures conferred an additional $1,698 in total costs (95%CI: $1,677-$1,718) and $279 in OOP expenses (95%CI: $273-$285) compared to office procedures.
Conclusion:
For outpatient plastic surgery procedures, OOP expenses are increasing at a faster rate than total costs, which may have implications for access to care and timing of surgery. Providers should realize the increasing burden of OOP expenses and the implications of surgical location on patients’ costs when possible.
Keywords: cost, out-of-pocket expenses, plastic surgery
Introduction
In 2017, plastic surgeons performed approximately 5.8 million reconstructive procedures with insurance paying for the majority of these procedures.1 However, even in these instances of insurance coverage, patients are becoming increasingly financially responsible for a greater portion of their surgical care. Healthcare reimbursement structure in the United States has changed considerably with costs being passed on to patients through rising deductibles, coinsurance, and copayments. There is a lack of transparency in out-of-pocket (OOP) expenses for healthcare. Patients and providers have a limited understanding of healthcare costs, which may lead to unintended financial burden for patients.2,3 Large OOP expenses have been associated with treatment non-adherence and worse health-related outcomes.4–7 Moreover, OOP expenses have implications for delays in treatment and access to care.8–10 With a push towards patient-centered care, understanding cost from the patient’s perspective has implications for shared-decision making and alleviating potential financial burden.
Recent studies have shown the substantial growth in OOP expenses for pharmaceuticals and inpatient hospitalizations.11,12 National studies of hospitalizations have shown an average rise of 86% for deductibles and a 33% increase in co-insurance,11 varying across different medical diagnoses. However, little is known regarding the temporal trends of OOP expenses for surgical procedures. Specifically, for plastic surgery procedures, which are largely elective, understanding changes in OOP expenses over time can help surgeons understand the financial burden placed on patients and incorporate cost in the decision-making process to mitigate this harm. Furthermore, these temporal trends in OOP expenses may impact surgical timing, treatment decisions, and access to care.
Given the possible negative effects of OOP expenses on the patient, understanding the temporal trends of OOP expenses for the most common outpatient reconstructive procedures warrants further investigation. These data will help equip providers and policymakers with vital information regarding the financial burden placed on patients. Therefore, we aim to investigate the temporal trends of the total cost and OOP expenses for plastic and reconstructive procedures and to determine factors associated with increased cost sharing.
Methods
Data Source and Cohort Selection
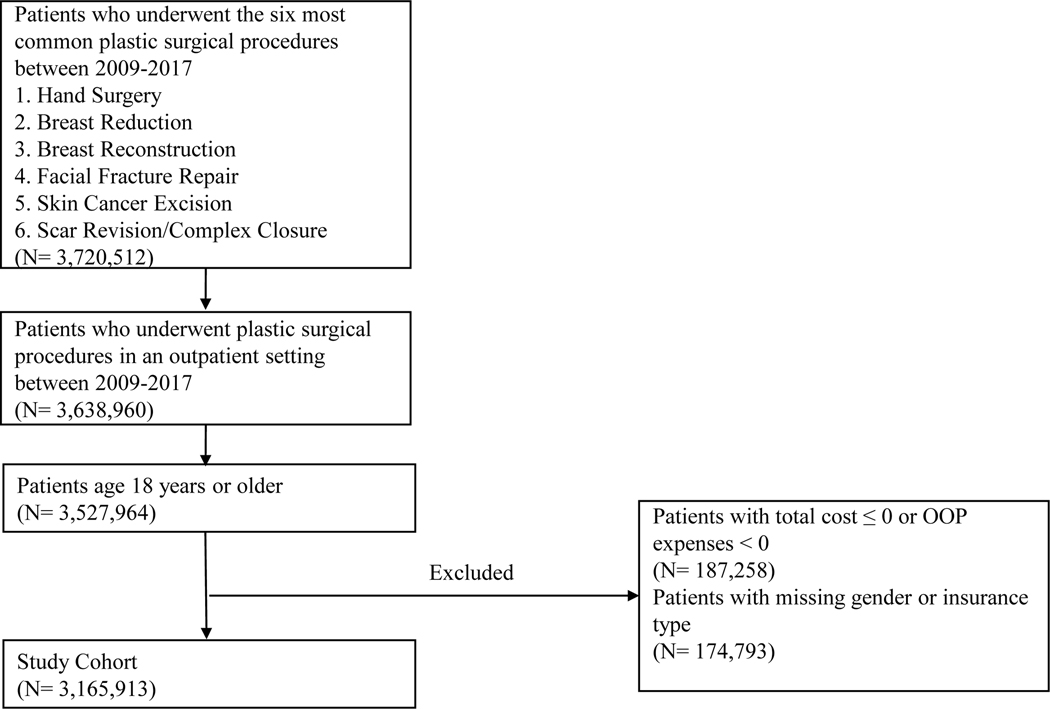
We used insurance claims data from 2009–2017 from the Truven MarketScan Research Databases to conduct a retrospective cohort study. These databases contain inpatient and outpatient information, pharmaceutical data, and patient-level costs for over 50 million patients with employer-sponsored insurance and patients with Medicare supplemental insurance.13 The study cohort comprised of patients, age 18 years or older, undergoing the most common outpatient reconstructive plastic surgical procedures: skin cancer excision with closure, breast reconstruction, breast reduction, hand surgery, facial fracture repair, and scar/complex closure.1 We identified patients using Current Procedural Terminology (CPT) codes (Appendix A) encompassing the surgical procedures of interest. We excluded patients who underwent these procedures in an inpatient setting or claims where the total costs paid by the insurer was less than or equal to zero or total cost sharing was less than zero. Figure 1 illustrates the full inclusion and exclusion criteria for this study. The study qualified for exempt status from the Institutional Review Board.
Figure 1:
Inclusion and Exclusion Criteria
Outcome Variables
Our primary outcome was OOP spending for the outpatient surgical procedure. OOP spending included the cost of surgical care that the patient incurred comprising of copayments, deductibles, and coinsurance payments. We also collected total cost of the surgery claim, which was defined as the total amount paid by the insurer plus patient out of pocket expenses. We inflation adjusted all costs to 2017 United States dollar.
Explanatory Variables
We collected patient-level sociodemographic information including age, gender, median household income, geographic region, and insurance type. Insurance type was categorized into four groups: fee-for-service, managed care, Medicare-fee-for-service, and Medicare-managed care. Managed care organizations were defined as either partially of fully capitated plans including health maintenance organizations and preferred provider organizations. Fee-for-service plans included comprehensive plans, basic or major medical plans, exclusive provider organizations, preferred provider organizations without capitation, and consumer-driven health plans. Enrollment in a high-deductible health plan was also recorded. The Elixhauser Comorbidity score for each patient was calculated as a proxy for health status using International Classification of Disease, Ninth Revision and Tenth Revision (ICD-9/10) diagnosis codes.14,15 We also collected the location of the outpatient surgical procedure including ambulatory surgery center, outpatient hospital, or office. These locations distinctions were established by the Centers of Medicare and Medicaid16 and are captured in the dataset.
Statistical Analyses
We examined the predicted OOP expenses and total cost of outpatient plastic surgery procedures over time. We first performed bivariate comparisons to assess the relative change in OOP expenses and total costs based on demographic characteristics of patients undergoing outpatient plastic surgery procedures in 2009 and 2017 using the Chi-square test for categorical variables and Student’s two-tailed t-test for continuous variables.
Generalized linear regression models with log link and gamma distribution were performed to predict the change in OOP expenses and the total cost in 2017 based on independent patient and surgical characteristics. The regression coefficient with exponential transformation in the model represents the cost ratio, which is the multiplicative change in the outcome (OOP expenses or total costs) relative to the reference comparison group. For example, a coefficient of 1.5 for a variable subgroup means the subgroup has 1.5 times increase in the predicted outcome compared to the reference subgroup. In the models, we adjusted for patient gender, median household income, geographic region, Elixhauser Comorbidity score, insurance type, and surgical location. All variables in the model were assessed to ensure no multicollinearity was present. Average marginal effects were calculated to determine the absolute change in predicted costs in dollars, while adjusting for the included explanatory variables. To examine the association between procedure type and location, we performed sensitivity analyses using a sample restricted to each specific surgical type. Significance level of P<0.05 was used for all analyses. Analyses were performed using SAS software (version 9.4; SAS Institute Inc.).
Results
Among the plastic surgery procedures of interest, 3,165,913 outpatient claims were identified for inclusion between January 1, 2009 and December 31, 2017. Table 1 describes the sociodemographic characteristics of patients in the final cohort and patients receiving surgery specifically in 2009 and 2017. When comparing 2009 and 2017, there was an increase in the number of high-deductible health plans in 2017 (3.8% in 2009 vs. 16.2% in 2017, P<0.001), and a higher percentage of procedures were performed in the office in 2017 (54.8% in 2009 vs. 57.1% in 2017, P<0.001).
Table 1:
Sociodemographic Characteristics of Patients Undergoing Outpatient Plastic Surgery (N=3,165,913)
| Patient Characteristics | Overall Number (%) | 2009 Number (%) | 2017 Number (%) | P-value |
|---|---|---|---|---|
| Total | 3,165,913 | 399,014 | 207,849 | |
| Gender | <.001 | |||
| Female | 1,484,831 (46.9) | 185,801 (46.6) | 95,059 (45.7) | |
| Male | 1,681,082 (53.1) | 213,213 (53.4) | 112,790 (54.3) | |
| Age | <.001 | |||
| 18–34 | 204,091 (6.4) | 28,572 (7.2) | 13,713 (6.6) | |
| 35–44 | 256,517 (8.1) | 36,638 (9.2) | 17,534 (8.4) | |
| 45–54 | 550,418 (17.4) | 76,604 (19.2) | 38,023 (18.3) | |
| 55–64 | 860,366 (27.2) | 106,329 (26.6) | 69,551 (33.5) | |
| ≥65 | 1,294,521 (40.9) | 150,871 (37.8) | 69,028 (33.2) | |
| Median Household Income | <.001 | |||
| <40,000 | 71,124 (2.2) | 8,786 (2.2) | 2,974 (1.4) | |
| 40,000–50,000 | 786,596 (24.8) | 91,361 (22.9) | 39,894 (19.2) | |
| 50,000–60,000 | 1,119,252 (35.4) | 145,864 (36.6) | 60,057 (28.9) | |
| 60,000–70,000 | 393,112 (12.4) | 49,647 (12.4) | 15,535 (7.5) | |
| >70,000 | 146,370 (4.6) | 24,280 (6.1) | 6,065 (2.9) | |
| Unspecified | 649,459 (20.5) | 79,076 (19.8) | 83,324 (40.1) | |
| Geographic Region | <.001 | |||
| Northeast | 530,148 (16.7) | 53,712 (13.5) | 36,279 (17.5) | |
| North Central | 704,932 (22.3) | 96,165 (24.1) | 42,520 (20.5) | |
| South | 1,282,280 (40.5) | 162,889 (40.8) | 97,635 (47.0) | |
| West | 577,922 (18.3) | 71,223 (17.8) | 31,090 (15.0) | |
| Unknown | 70,631 (2.2) | 15,025 (3.8) | 325 (0.2) | |
| Elixhauser Comorbidity Score | <.001 | |||
| 0 | 1,207,904 (38.2) | 126,949 (31.8) | 133,963 (64.5) | |
| 1–3 | 179,792 (5.7) | 20,224 (5.1) | 16,663 (8.0) | |
| 4–7 | 552,320 (17.4) | 68,290 (17.1) | 38,053 (18.3) | |
| ≥8 | 1,225,897 (38.7) | 183,551 (46.0) | 19,170 (9.2) | |
| Insurance Type | <.001 | |||
| FFS | 1,922,344 (60.7) | 242,479 (60.8) | 144,311 (69.4) | |
| MC | 234,365 (7.4) | 39,315 (9.9) | 16,373 (7.9) | |
| Medicare-FFS | 917,662 (29.0) | 105,730 (26.5) | 41,366 (19.9) | |
| Medicare-MC | 91,542 (2.9) | 11,490 (2.9) | 5,799 (2.8) | |
| HDHP | <.001 | |||
| Yes | 243,515 (7.7) | 15,044 (3.8) | 33,754 (16.2) | |
| Procedure Type | <.001 | |||
| Breast reconstruction | 101,418 (3.2) | 12,455 (3.1) | 6,914 (3.3) | |
| Breast reduction | 70,225 (2.2) | 11,085 (2.8) | 4,297 (2.1) | |
| Facial fracture repair | 55,764 (1.8) | 8,123 (2.0) | 3,242 (1.6) | |
| Hand surgery | 857,310 (27.1) | 109,311 (27.4) | 57,368 (27.6) | |
| Scar revision/ Complex closure | 849,975 (26.8) | 95,109 (23.8) | 65,269 (31.4) | |
| Skin cancer excision | 1,231,221 (38.9) | 162,931 (40.8) | 70,759 (34.0) | |
| Place of Service | <.001 | |||
| Office | 1,784,913 (56.4) | 218,497 (54.8) | 118,664 (57.1) | |
| Outpatient hospital | 932,340 (29.4) | 124,855 (31.3) | 57,542 (27.7) | |
| Ambulatory surgical center | 448,660 (14.2) | 55,662 (13.9) | 31,643 (15.2) |
FFS: fee-for-service; HDHP: high-deductible health plan; MC: managed care
Inflation rate adjusted to 2017 dollars.
Approximately 80% of scar revision/complex closures and 85% of skin cancer excisions were performed in the office (Table 2). For office-based procedures, skin cancer excisions were the most common (1,049,464 procedures), and breast reduction was the least common (1,903 procedures).
Table 2:
Frequency of Procedures Performed Stratified by Place of Service (2009–2017)
| Procedure Type | Office No. (%) | Outpatient Hospital No. (%.) | Ambulatory Surgery Center No. (%) |
|---|---|---|---|
| Breast Reconstruction | 5,638 (6%) | 78,852 (78%) | 16,928 (17%) |
| Breast Reduction | 1,903 (3%) | 51,664 (74%) | 16,658 (24%) |
| Facial fracture repair | 10,035 (18%) | 34,247 (61%) | 11,482 (21%) |
| Hand surgery | 33,983 (4%) | 508,627 (59%) | 314,700 (37%) |
| Scar revision/ Complex closure | 683,890 (80%) | 114,225 (13%) | 51,860 (6%) |
| Skin cancer excision | 1,049,464 (85%) | 144,725 (12%) | 37,032 (3%) |
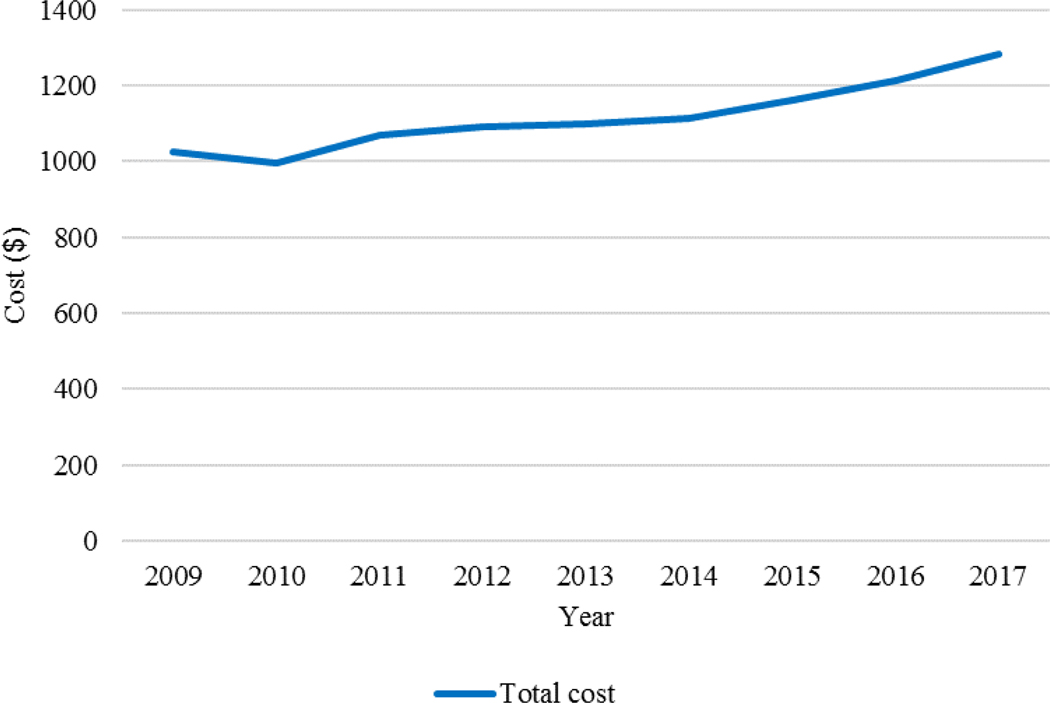
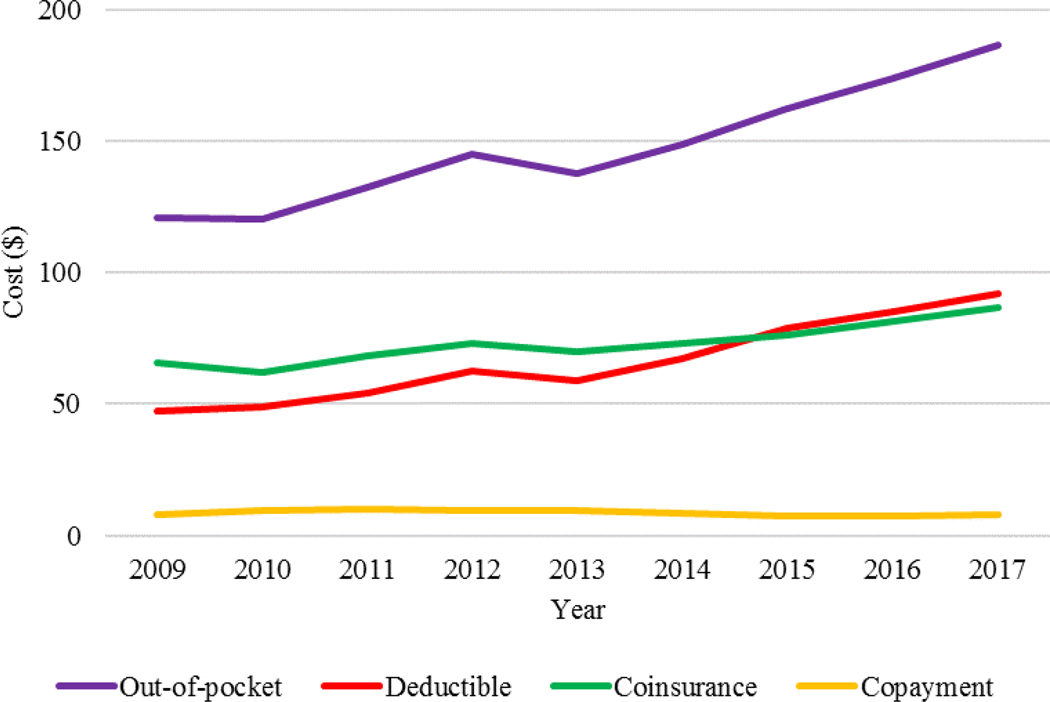
On average, total costs increased by 25% from 2009 until 2017, and Figure 2 depicts the change in total cost during this time period (Table 3). For OOP expenses, there was a 54% increase from 2009 to 2017 with deductibles and co-insurance accounting for the majority of this rising trend. In 2009, the average deductible payment was $47 compared to $92 in 2017 (P<0.001), and the average co-insurance payment was $66 in 2009 and $87 in 2017 (P<0.001). Figure 3 illustrates the change in total OOP expenses, deductibles, coinsurance, and copayments from 2009 to 2017. OOP expenses differed substantially based on procedure type with breast reductions having the highest OOP expenses (average $381) and skin cancer excisions having the lowest OOP expenses (average $80) (Table 3).
Figure 2:
Total Cost (2009–2017)
Table 3:
Total Cost and Out-of-Pocket Costs
| Characteristic | Total Cost | OOP Costs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean Total Cost, $* | Mean Cost 2009, $ | Mean Cost 2017, $ | 2009–2017, % change | P-Value | Mean Total OOP Expenses, $* | Mean OOP Costs 2009, $ | Mean OOP Costs 2017, $ | 2009–2017, % change | P-Value | |
| Total | 1,098 | 1,024 | 1,282 | 25 | <0.001 | 143 | 121 | 187 | 54 | <0.001 |
| Insurance Type | ||||||||||
| FFS | 1,276 | 1,159 | 1,393 | 20 | <0.001 | 199 | 164 | 241 | 47 | <0.001 |
| MC | 1,304 | 1,254 | 1,411 | 13 | <0.001 | 67 | 67 | 115 | 72 | <0.001 |
| Medicare-FFS | 701 | 656 | 911 | 39 | <0.001 | 83 | 52 | 46 | -12 | <0.001 |
| Medicare-MC | 805 | 790 | 816 | 3 | 0.133 | 51 | 35 | 44 | 26 | <0.001 |
| HDHP | ||||||||||
| Yes | 1,146 | 1,018 | 1,291 | 27 | <0.001 | 266 | 187 | 312 | 67 | <0.001 |
| No | 1,094 | 1,025 | 1,281 | 25 | <0.001 | 133 | 119 | 162 | 36 | <0.001 |
| Geographic Region | ||||||||||
| Northeast | 1,271 | 1,127 | 1,581 | 40 | <0.001 | 100 | 80 | 138 | 73 | <0.001 |
| North Central | 1,220 | 1,200 | 1,419 | 18 | <0.001 | 161 | 136 | 204 | 50 | <0.001 |
| South | 991 | 940 | 1,135 | 21 | <0.001 | 158 | 139 | 196 | 41 | <0.001 |
| West | 1,034 | 979 | 1,211 | 24 | <0.001 | 130 | 97 | 191 | 97 | <0.001 |
| Place of Service | ||||||||||
| Office | 420 | 418 | 439 | 5 | <0.001 | 76 | 68 | 102 | 50 | <0.001 |
| Outpatient Hospital | 2,035 | 1,774 | 2,525 | 42 | <0.001 | 215 | 179 | 272 | 52 | <0.001 |
| Ambulatory Surgical Center | 1,848 | 1,725 | 2,186 | 27 | <0.001 | 259 | 202 | 350 | 73 | <0.001 |
| Procedure Type | ||||||||||
| Breast Reconstruction | 3,003 | 2,674 | 3,379 | 26 | <0.001 | 200 | 174 | 224 | 29 | <0.001 |
| Breast Reduction | 4,186 | 3,904 | 4,663 | 19 | <0.001 | 381 | 328 | 465 | 42 | <0.001 |
| Facial Fracture Repair | 1,817 | 1,669 | 2,079 | 25 | <0.001 | 256 | 209 | 318 | 52 | <0.001 |
| Hand Surgery | 2,005 | 1,735 | 2,460 | 42 | <0.001 | 254 | 200 | 336 | 68 | <0.001 |
| Scar Revision/Complex Closure | 545 | 557 | 570 | 2 | <0.001 | 88 | 82 | 110 | 34 | <0.001 |
| Skin Cancer Excision | 483 | 466 | 538 | 15 | <0.001 | 80 | 69 | 109 | 58 | <0.001 |
FFS: fee-for-service, HDHP: high deductible health plan, MC: managed care, OOP: out-of-pocket
Figure 3:
Out-of-Pocket Expenses (2009–2017)
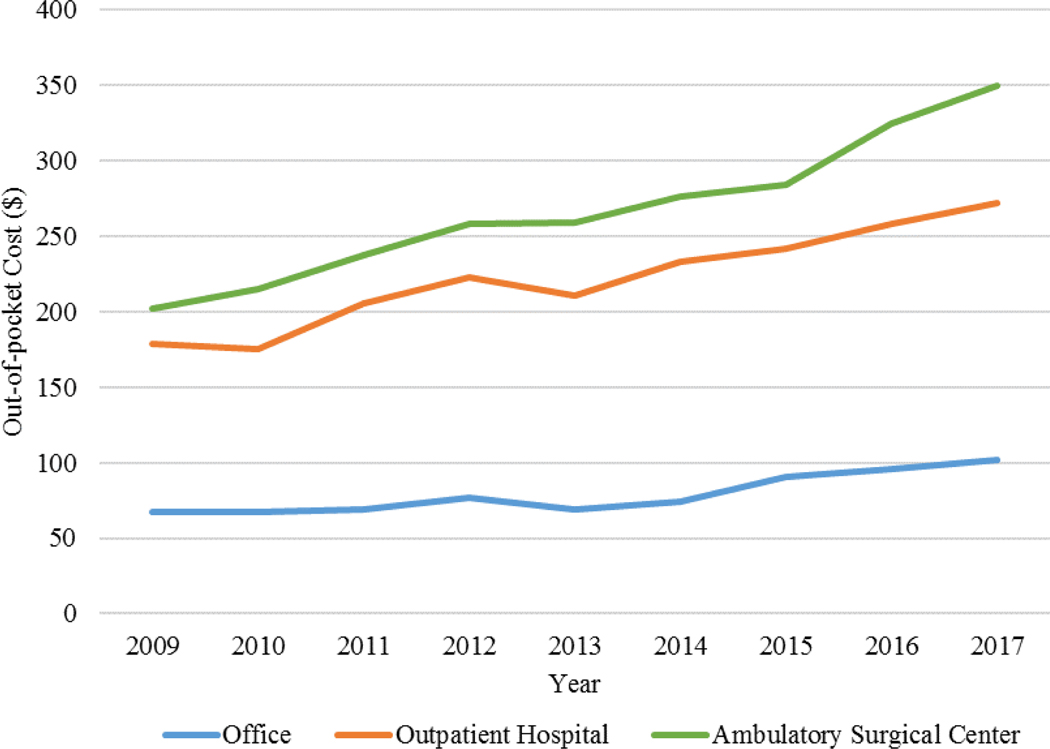
There was a significant association between the increase in total costs and place of service from 2009–2017 (5% increase for office procedures, 42% increase for outpatient hospitals, and 27% increase for ambulatory surgery centers, P<0.001 for all) (Table 3). Relative to total costs, OOP expenses also rose during the same time period but at a faster rate (office: increase of 50%, outpatient hospital: increase of 52%, ambulatory surgery centers: increase of 73%, P<0.001). Figure 4 describes the OOP expenses stratified by surgical location over time.
Figure 4:
Out-of-Pocket Expenses Stratified by Surgical Location (2009–2017)
Using multivariable regression models, total cost for managed care, Medicare-managed care, and Medicare-fee-for-service was 30–74% of the total cost for fee-for-service patients (Table 4). Patients who underwent surgery in an ambulatory surgery center had approximately 500% of the predicted total cost of patients who underwent surgery in the office (cost ratio: 4.93, 95% CI: (4.89–4.98), P<0.001) with an added cost of $1,698 (95% CI: $1,677 to $1,718). Similarly, procedures performed in an outpatient hospital conferred an additional $1,999 (95% CI: $1,978 to $2,020) compared to the office.
Table 4:
Generalized Linear Regression of Total Cost in 2017
| Characteristics | Cost Ratio (95% CI) | P-value | $ Change (95% CI)* |
|---|---|---|---|
| Gender | |||
| Female | 1[Reference] | - | - |
| Male | 1.10 (1.09–1.11) | <0.001 | 178 (166 to 190) |
| Median Household Income | |||
| <40,000 | 1[Reference] | - | - |
| 40,000–50,000 | 1.01 (0.99–1.04) | 0.37 | −13 (−61 to 35) |
| 50,000–60,000 | 1.07 (1.04–1.10) | <0.001 | 96 (48 to 144) |
| 60,000–70,000 | 1.04 (1.01–1.07) | 0.02 | 9 (−41 to 59) |
| >70,000 | 1.17 (1.13–1.21) | <0.001 | 99 (42 to 156) |
| Geographic Region | |||
| Northeast | 1[Reference] | - | - |
| North Central | 0.74 (0.73–0.74) | <0.001 | −344 (−366 to −322) |
| South | 0.68 (0.68–0.69) | <0.001 | −442 (−463 to −420) |
| West | 0.78 (0.77–0.79) | <0.001 | −287 (−312 to 263) |
| Elixhauser Comorbidity Score | |||
| 0 | 1[Reference] | - | - |
| 1–3 | 1.05 (1.04–1.06) | <0.001 | 55 (35 to 75) |
| 4–7 | 1.07 (1.06–1.08) | <0.001 | 61 (46 to 75) |
| ≥8 | 1.04 (1.03–1.06) | <0.001 | 20 (0 to 40) |
| Insurance Type | |||
| FFS | 1[Reference] | - | |
| MC | 1.01 (1.00–1.03) | 0.04 | −58 (−77 to −39) |
| Medicare-FFS | 0.94 (0.93–0.95) | <0.001 | −241 (−255 to −226) |
| Medicare-MC | 0.76 (0.74–0.77) | <0.001 | −483 (−505 to −460) |
| HDHP | |||
| No | 1[Reference] | - | |
| Yes | 0.99 (0.98–0.99) | 0.002 | −30 (−44 to −15) |
| Place of Service | |||
| Office | 1[Reference] | - | |
| Outpatient Hospital | 5.59 (5.54–5.63) | <0.001 | 1,999 (1,978 to 2,020) |
| Ambulatory Surgery Center | 4.93 (4.89–4.98) | <0.001 | 1,698 (1,677 to 1,718) |
FFS: fee-for-service; HDHP: high-deductible health plan; MC: managed care
Changes in total cost obtained using margins command for average marginal effect.
In the adjusted regression for OOP expenses, ambulatory surgery centers and outpatient hospitals had approximately 270–290% of the predicted OOP expenses of procedures performed in the office (P<0.001) (Table 5). On average, procedures performed in an outpatient hospital conferred an additional $259 (95% CI: $254 to $264) in OOP expenses compared to the office, and procedures performed in an ambulatory surgical center were associated with an added $279 (95% CI: $273 to 285) in OOP expenses. In the sensitivity analyses, scar revision/complex closures and skin cancer excisions, which can be performed in multiple locations, had significant differences in OOP expenses based on location. These procedures performed in ambulatory surgery centers and outpatient hospitals had approximately 170–240% of the predicted OOP expenses compared to procedures performed in the office (Appendix B).
Table 5:
Generalized Linear Regression of Out-of-Pocket Expenses in 2017
| Characteristics | Cost Ratio (95% CI) | P-value | $ Change (95% CI)* |
|---|---|---|---|
| Gender | |||
| Female | 1[Reference] | - | |
| Male | 1.03 (1.02–1.04) | <0.001 | 14 (11 to 18) |
| Median Household Income | |||
| <40,000 | 1[Reference] | - | |
| 40,000–50,000 | 0.99 (0.95–1.04) | 0.69 | −6 (−19 to 8) |
| 50,000–60,000 | 1.02 (0.98–1.07) | 0.29 | 1 (−13 to 14) |
| 60,000–70,000 | 1.01 (0.96–1.05) | 0.82 | −8 (−22 to 7) |
| >70,000 | 0.95 (0.91–0.99) | 0.10 | 7 (−11 to 25) |
| Geographic Region | |||
| Northeast | 1[Reference] | - | |
| North Central | 1.21 (1.19–1.23) | <0.001 | 58 (52 to 63) |
| South | 1.14 (1.13–1.16) | <0.001 | 45 (41 to 50) |
| West | 1.18 (1.15–1.20) | <0.001 | 56 (−46 to 29) |
| Elixhauser Comorbidity Score | |||
| 0 | 1[Reference] | - | |
| 1–3 | 0.87 (0.86–0.89) | <0.001 | −29 (−35 to −23) |
| 4–7 | 0.90 (0.88–0.91) | <0.001 | −29 (−33 to −24) |
| ≥8 | 0.77 (0.75–0.78) | <0.001 | −69 (−75 to −63) |
| Insurance Type | |||
| FFS | 1[Reference] | - | |
| MC | 0.74 (0.73–0.76) | <0.001 | −65 (−71 to −59) |
| Medicare-FFS | 0.31 (0.30–0.31) | <0.001 | −232 (−234 to −230) |
| Medicare-MC | 0.45 (0.43–0.47) | <0.001 | −165 (−172 to −157) |
| HDHP | |||
| No | 1[Reference] | - | |
| Yes | 1.49 (1.47–1.51) | <0.001 | 91 (86 to 96) |
| Place of Service | |||
| Office | 1[Reference] | - | |
| Outpatient Hospital | 2.76 (2.73–2.79) | <0.001 | 259 (254 to 264) |
| Ambulatory Surgery Center | 2.93 (2.89–2.97) | <0.001 | 279 (273 to 285) |
FFS: fee-for-service; HDHP: high-deductible health plan; MC: managed care
Changes in total cost obtained using margins command for average marginal effects
Sensitivity analyses revealed an inconsistent relationship between geographic region and predicted change in OOP expenses across the different procedure types. However, across all six procedure types, there was a consistent association between the change in cost ratios and subgroups based on procedure location and insurance type (Appendix B). Across all procedure types except for breast reduction, OOP expenses were significantly higher for procedures performed in an outpatient hospital or ambulatory surgery center.
Discussion
In this nationwide analysis of the temporal trends of the total cost and OOP expenses of outpatient plastic and reconstructive surgical procedures, OOP expenses are increasing at a faster rate than total insurance reimbursement paid to the provider and facility. Moreover, insurance type and surgical procedure location were associated with significant differences in total cost and OOP expenses. In order to improve value from the patient’s perspective, providers must realize the impact of surgical location on the financial burden placed on patients and should improve their awareness regarding OOP expenses when conferring care.
Previous research has demonstrated that most patients have a poor understanding of health insurance and OOP expenses. In a study by Loewenstein et al., 78% of patients surveyed had an actual understanding of the concept of a deductible compared to only 34% for the concept of coinsurance. Overall, these surveys demonstrated that patients may not fully comprehend current health insurance plans, and the authors suggested that simplifying health insurance plans may help bridge this gap in understanding.17 Other studies have corroborated these findings, specifically for outpatient services, with patients unable to determine if services would be covered by insurance and how much they would have to pay out-of-pocket.18 Given the lack of understanding of OOP expenses, the growing rates of OOP expenses have implications for possible financial harm to patients. This study shows that patients are bearing more of the financial burden of outpatient plastic and reconstructive surgical procedures with OOP expenses growing at a faster rate than total cost. We found a 54% increase in OOP expenses from 2009 to 2017, which may have unintended financial consequences. According to the Kaiser Family Foundation, approximately 26% of adults in the United States had problems paying their medical bills, either personally or by someone in their household. Of these people, 19% had employer-based health insurance.19 Therefore, OOP expenses should be incorporated in the decision making process when conferring care.
During surgical consultation, discussing OOP expenses may lead to better patient-centered care. Both providers and patients desire communication regarding costs.20 However, many providers fail to discuss cost with patients or consider cost when delivering care.21,22 The barriers to discussion of cost include failure to identify patient’s financial concerns, quick dismissal of these concerns, and the lack of price transparency in the health system.23 Despite these barriers, providers should have honest conversations with patients regarding costs to minimize financial burden on the patient, enhance medication adherence, decrease delays in treatment, and close the gap of socioeconomic inequalities.24 According to the American Medical Association, providers can help patients navigate healthcare costs by providing patients with materials to help improve health literacy, making cost information available for common procedures, and discussing the hospital charges or commonly negotiated costs to permit price transparency.25 Additionally, discussing modifiable OOP cost characteristics may aid in shared decision-making. However, all health care stakeholders including insurers, hospitals, providers, and policy makers should strive for price transparency to decrease the burden of OOP expenses.
In this nationwide study, we found that patients who underwent procedures in the office had significantly less OOP expenses than those who had procedures in surgical centers or the hospital, highlighting one potentially modifiable factor to decrease OOP expenses. However, not all procedures can be performed in the office, and more expensive procedures are commonly performed in surgery centers or the hospital. Additionally, providers may choose to perform surgeries in different locations because of multiple reasons. Studies of physician ownership of ambulatory surgery centers has revealed that ownership is associated with an increased frequency of procedures performed at those centers.26,27 There is also an up-front cost to providers in effort and equipment to be able to perform procedures in an office setting. This may be a barrier to many surgeons, who by nature are already able to perform procedures of varying complexity in an ambulatory surgery or outpatient hospital setting. Furthermore, providers or patients may choose anesthesia services for simpler procedures that can be done in the office, yet providers must educate patients on the increased OOP costs for the use of anesthesia and for fees associated with different surgical location.
In our sensitivity analysis, even for simpler procedures such as scar revision/complex closure and skin cancer excision, patients who received surgery in ambulatory surgery centers and the hospital had notably higher total costs and OOP expenses. For procedures that have the option to be performed in multiple surgical locations, such as scar revisions, small skin cancer excisions or minor hand surgery procedures, providers should make an effort to perform these minor procedures in less costly venues and help to promote systems level reforms to encourage cost transparency for patients. Moreover, in this analysis, we found that the OOP expenses associated with procedures performed in ambulatory surgery centers and outpatient hospital settings are increasing substantially more than OOP expenses for procedures performed in the office. Ambulatory surgery centers and outpatient hospitals are in direct competition with one another, which may lead to similar increases in costs. There has also been a surge in the market penetration of ambulatory surgery centers, which has led to an increased bargaining power if ambulatory surgery centers and subsequently higher costs for patients.28 Surgical location may be a modifiable cost contributor that can help decrease the financial burden placed on patients.
In this nationwide study of employer-based insurance, our findings show an increase in OOP expenses for outpatient plastic and reconstructive surgical procedures even during the time period of implementation of the Affordable Care Act (ACA). The ACA enacted provisions to change insurance cost structure in attempts to limit OOP maximums and increase price transparency.29 Studies have shown that the ACA reduced overall OOP expenses, more specifically for low-income patients.30,31 Despite the provisions of the ACA and prior studies, we found that OOP expenses continued to increase for employer-based health insurance plans. This may occur if OOP maximums are greater than the OOP costs for these plastic surgical outpatient procedures. For example, in 2019, the OOP maximum is $7,900 for an individual and $15,800 for a family.32 In comparison, the mean OOP expense for a plastic surgery procedure from 2009 to 2017 was $143, although this differed based on the type of surgical procedure (mean of $381 for breast reduction versus $80 for skin cancer excision). Additionally, out of network costs, premiums, and costs that are not part of the essential health benefits may not be included in these OOP maximums. Therefore, the increase in OOP expenses for outpatient surgeries should be considered when developing cost reduction policies to alleviate the financial burden placed on the patient.
Our study has several limitations inherent to administrative claims data. The validity of any claims-based data analysis requires accurate coding of billing data, and the accuracy of this coding could not be assessed. The Truven MarketScan databases include employer-sponsored private health insurance, for which OOP expenses are substantially different than with government-sponsored health insurance. For example, Medicaid has minimal cost sharing with a cap on OOP expenses to 5% of the household income.33 Therefore, these findings are not generalizable to patients with Medicare or Medicaid, ACA marketplace plans, and the uninsured. Moreover, this study lacks data on insurance premium costs, which may have added implications on the financial burden of surgery. Lastly, we restricted our sample to outpatient surgeries, thereby limiting the generalizability of this study to surgeries requiring inpatient hospitalization and is likely an underestimation of the OOP expenses for plastic surgical care more globally.
OOP expenses for outpatient plastic and reconstructive surgical procedures have grown at a more substantial rate than total costs of surgery between 2009 and 2017. Surgical location in ambulatory surgery centers and outpatient hospitals and fee-for-service insurance type were predictive of a higher burden of OOP expenses. Given these increases in OOP expenses for outpatient plastic and reconstructive surgical procedures, providers and health systems should be more transparent in sharing cost information with patients, which have a direct impact on OOP expenses that patients experience with differing insurance plans. Providers must be aware of the impact of the procedural setting on cost when conferring care. Moreover, policymakers should consider OOP expenses when evaluating cost reduction reforms to minimize the financial burden placed on patients and fully consider healthcare value from the patient perspective.
Supplementary Material
Acknowledgements/Funding:
Dr. Erika D. Sears is supported by a Career Development Award Number IK2 HX002592 from the United States (U.S.) Department of Veterans Affairs Health Services R&D (HSRD) Service. The authors wish to acknowledge the support of the Maintenance Project of the Center in Artificial Intelligence in Medicine (Grant CIRPG3H0021) at Chang Gung Memorial hospital. The funding organizations had no role in the design and conduct of the study, including collection, management, analysis, and interpretation of the data.
Footnotes
Presentation: Will be presented at Plastic Surgery The Meeting 2019, San Diego, California
References
- 1.American Society of Plastic Surgeons. 2017. Plastic Surgery Statistics Report. 2017; https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. [Google Scholar]
- 2.Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or Debt? National Estimates of Financial Toxicity in Persons with Newly-Diagnosed Cancer. Am J Med. 2018;131(10):1187–1199 e1185. [DOI] [PubMed] [Google Scholar]
- 3.Narang AK, Nicholas LH. Out-of-Pocket Spending and Financial Burden Among Medicare Beneficiaries With Cancer. JAMA Oncol. 2017;3(6):757–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelley RK, Venook AP. Nonadherence to imatinib during an economic downturn. New England Journal of Medicine. 2010;363(6):596–598. [DOI] [PubMed] [Google Scholar]
- 5.Hirth RA, Greer SL, Albert JM, Young EW, Piette JD. Out-of-pocket spending and medication adherence among dialysis patients in twelve countries. Health Aff (Millwood). 2008;27(1):89–102. [DOI] [PubMed] [Google Scholar]
- 6.Bibeau WS, Fu H, Taylor AD, Kwan AY. Impact of Out-of-Pocket Pharmacy Costs on Branded Medication Adherence Among Patients with Type 2 Diabetes. J Manag Care Spec Pharm. 2016;22(11):1338–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket costs as side effects. New England Journal of Medicine. 2013;369(16):1484–1486. [DOI] [PubMed] [Google Scholar]
- 8.Fung V, Graetz I, Galbraith A, et al. Financial barriers to care among low-income children with asthma: health care reform implications. JAMA pediatrics. 2014;168(7):649–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solomon MD, Goldman DP, Joyce GF, Escarce JJ. Cost sharing and the initiation of drug therapy for the chronically ill. Archives of internal medicine. 2009;169(8):740–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Rowas S, Rothberg MB, Johnson B, et al. The association between insurance type and cost-related delay in care: a survey. The American journal of managed care. 2017;23(7):435. [PMC free article] [PubMed] [Google Scholar]
- 11.Adrion ER, Ryan AM, Seltzer AC, Chen LM, Ayanian JZ, Nallamothu BK. Out-of-Pocket Spending for Hospitalizations Among Nonelderly Adults. JAMA Intern Med. 2016;176(9):1325–1332. [DOI] [PubMed] [Google Scholar]
- 12.Song H, Adamson A, Mostaghimi A. Medicare Part D Payments for Topical Steroids: Rising Costs and Potential Savings. JAMA Dermatol. 2017;153(8):755–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danielson E Health Research Data for the Real World: The MarketScan Databases (White Paper; ). 2014. [Google Scholar]
- 14.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical care. 2009;47(6):626–633. [DOI] [PubMed] [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 16.Centers of Medicare and Medicaid. Place of Service Code Set. https://www.cms.gov/medicare/coding/place-of-service-codes/place_of_service_code_set.html. Accessed May 16, 2019. [Google Scholar]
- 17.Loewenstein G, Friedman JY, McGill B, et al. Consumers’ misunderstanding of health insurance. J Health Econ. 2013;32(5):850–862. [DOI] [PubMed] [Google Scholar]
- 18.Marquis MS. Consumers’ knowledge about their health insurance coverage. Health Care Financing Review. 1983;5(1):65. [PMC free article] [PubMed] [Google Scholar]
- 19.Hamel L, Norton M, Pollitz K, Levitt L, Claxton G, Brodie M. The Burden of Medical Debt: Results from the Kaiser Family Foundation/New York Times Medical Bills Survey. Kaiser Family Foundation. 2016. [Google Scholar]
- 20.Alokozai A, Crijns TJ, Janssen SJ, et al. Cost in Hand Surgery: The Patient Perspective. J Hand Surg Am. 2019. [DOI] [PubMed] [Google Scholar]
- 21.Altomare I, Irwin B, Zafar SY, et al. Physician Experience and Attitudes Toward Addressing the Cost of Cancer Care. J Oncol Pract. 2016;12(3):e281–288, 247–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290(7):953–958. [DOI] [PubMed] [Google Scholar]
- 23.Ubel PA, Zhang CJ, Hesson A, et al. Study Of Physician And Patient Communication Identifies Missed Opportunities To Help Reduce Patients’ Out-Of-Pocket Spending. Health Aff (Millwood). 2016;35(4):654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riggs KR, Ubel PA. Overcoming barriers to discussing out-of-pocket costs with patients. JAMA internal medicine. 2014;174(6):849–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Medical Association. Strategies to Increase Health Care Price Transparency. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/about-ama/councils/Council%20Reports/council-on-medical-service/issue-brief-strategies-increase-health-care-price-transparency.pdf. Accessed July 22, 2019. [Google Scholar]
- 26.Strope SA, Daignault S, Hollingsworth JM, Ze Z, Wei JT, Hollenbeck BK. Physician ownership of ambulatory surgery centers and practice patterns for urological surgery: evidence from the state of Florida. Medical care. 2009;47(4):403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell JM. Do financial incentives linked to ownership of specialty hospitals affect physicians’ practice patterns? Medical care. 2008;46(7):732–737. [DOI] [PubMed] [Google Scholar]
- 28.Carey K Ambulatory Surgery Centers and Prices in Hospital Outpatient Departments. Med Care Res Rev. 2017;74(2):236–248. [DOI] [PubMed] [Google Scholar]
- 29.Henry J Kaiser Family Foundation. Explaining health care reform: medical loss ratio (MLR). 2012; https://www.kff.org/health-reform/fact-sheet/explaining-health-care-reform-medical-loss-ratio-mlr/. Accessed May 7, 2019. [Google Scholar]
- 30.Glied S, Solís-Román C, Parikh S. How the ACA’s Health Insurance Expansions Have Affected Out-of-Pocket Cost-Sharing and Spending on Premiums. Issue brief (Commonwealth Fund). 2016;28:1–16. [PubMed] [Google Scholar]
- 31.Goldman AL, Woolhandler S, Himmelstein DU, Bor DH, McCormick D. Out-of-pocket spending and premium contributions after implementation of the affordable care act. JAMA internal medicine. 2018;178(3):347–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Healthcare.gov. Out-of-pocket maximum/limit. https://www.healthcare.gov/glossary/out-of-pocket-maximum-limit/. Accessed May 7, 2019. [Google Scholar]
- 33.Brooks T, Wagnerman K, Artiga S, Cornachione E, Ubri P. Medicaid and chip eligibility, enrollment, renewal, and cost sharing policies as of january 2017: Findings from a 50-state survey. Washington: Kaiser Family Foundation. 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.