Clinical History and Imaging
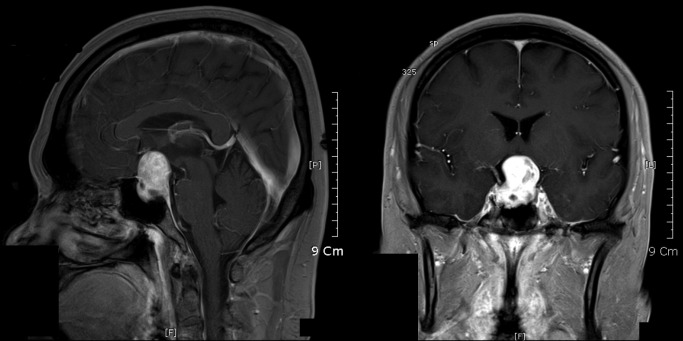
This 34 year‐old man presented with a five month complaint of bitemporal hemianopsia. For two years he had decreased visual acuity and increased intraocular pressure treated medically. Magnetic resonance imaging revealed widening of the pituitary fossa and an intrasellar, dumbbell shaped, enhancing mass 3 cm in diameter, extending into the suprasellar region pushing on the optic chiasm (Figure 1a and 1b). The mass was partially excised, but regrew in three months causing the same symptoms. A second excision was performed. Three months later the tumor again regrew with extension into the sphenoid sinus, and the patient underwent a third excision. Following surgery, the patient was given radiotherapy and one cycle of chemotherapy (adriamycin, dacabarzine, and ifosfamide). Follow‐up PET‐CT three months after the third surgery showed no evidence of hypermetabolic residual/recurrent tumor.
Figure 1.
Pathological Findings
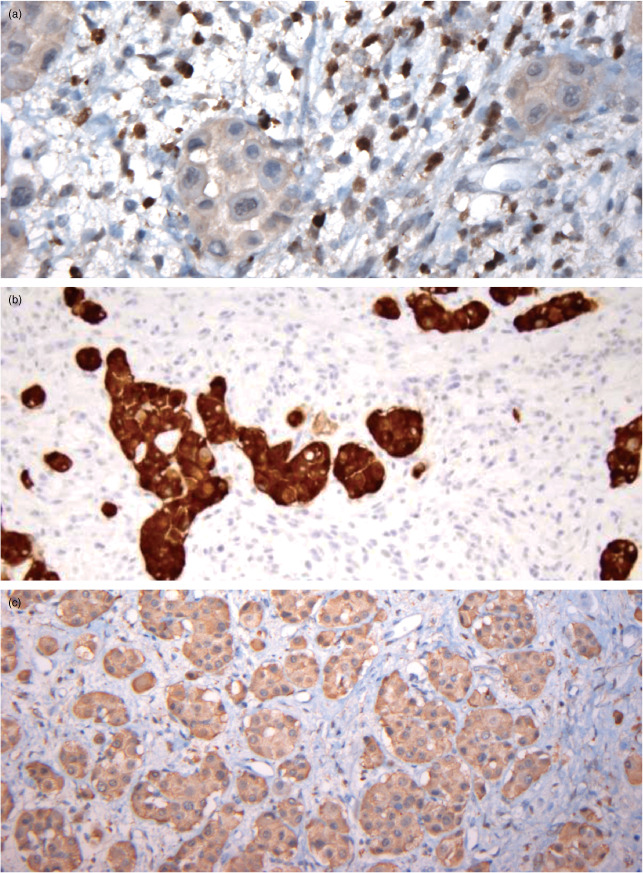
Both the first and second excisions show small, spindled cells with interdigitating elongated eosinophilic cells (Figure 2a). In addition, there are scattered glandular groups of monomorphic round cells with large amounts of eosinophilic cytoplasm (Figures 2a and 2b). In some areas there are primitive cells with small round nuclei, scant cytoplasm, and numerous mitoses and apoptotic cells (Figure 2b) and occasional cells with striations (Figure 2c). The small spindle cells and striated cells are positive for desmin and have nuclear positivity for myogenin (Figure 3a) and myo‐D1 (not shown). The islands of monomorphic large eosinophilic cells are positive for synaptophysin (Figure 3b) and ACTH (Figure 3c) and negative for prolactin. They are also positive for chromogranin, CK 5.2, pan keratin, and NSE (not shown).
Figure 2.
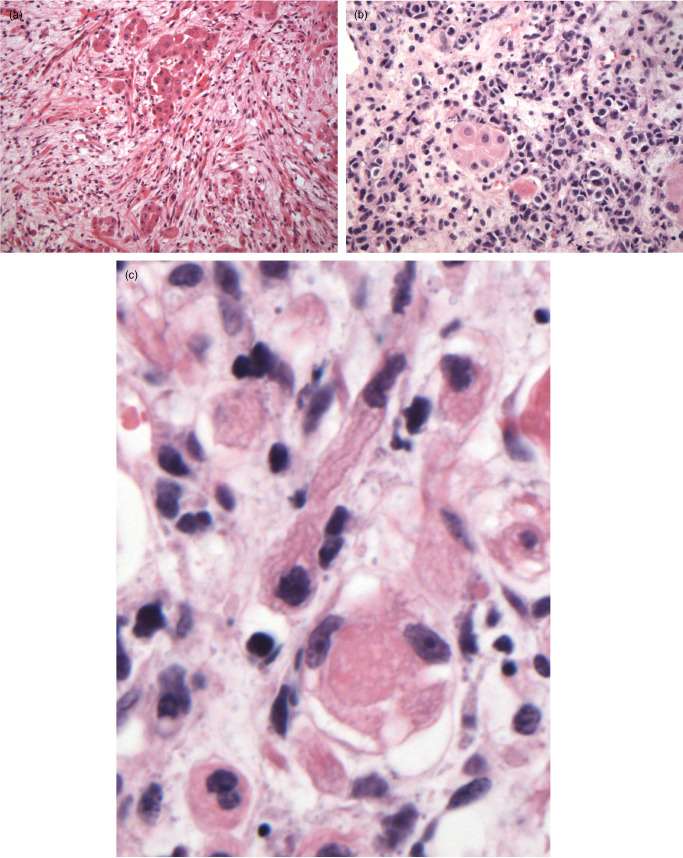
Figure 3.
The third excision reveals similar findings (not shown). The tumor invades the sphenoid sinus and is positive for Myo‐D1. The Ki‐67 proliferation index is markedly elevated within the primitive, anaplastic regions. Again, there are elongated striated cells and foci of anaplastic small cells as well as admixtures of the large eosinophilic cells, which are positive for keratin, synaptophysin, and ACTH (not shown). What is your diagnosis?
Diagnosis
Embryonal rhabdomyosarcoma arising within the pituitary gland.
Discussion
Embryonal rhabdomyosarcoma is a primitive sarcoma that mimics the features of embryonic skeletal muscle. It most commonly affects the extracranial regions of the head including the soft tissues surrounding the orbit, nasopharynx, and nasal cavity. Nonorbital rhabdomyosarcomas can extend intracranially. However, only a few cases of primary intracranial rhabdomyosarcoma have been reported and only two cases have been reported originating primarily within the sella turcica 1, 3.
This patient was originally presumed to have juvenile‐onset primary open‐angle glaucoma due to his high intraocular pressure 2. However, his visual field defects progressed despite medical therapy and a brain MRI revealed the large intrasellar mass that was subsequently resected.
Histologically, the spindled and primitive tumor cells surrounded clusters of large epithelioid pituitary cells. The pituitary cells were diffusely positive for ACTH and negative for prolactin suggesting a proliferation of ACTH cells and possibly an associated ACTH‐secreting pituitary adenoma within the rhabdomyosarcoma. The fact that these ACTH positive cells were present with each recurrence of the tumor further supports the idea that these pituitary cells represent an associated hyperplastic or neoplastic process.
Rhabdomyosarcomas are aggressive tumors, and the older age of this patient as well as the parameningeal growth, initial incomplete resection, and invasion of the sphenoid sinus suggest a poor survival rate. Thus, the patient was treated with an intensive combination of radiation and chemotherapy. Nine months after the patient's first excision, a follow‐up PET‐CT did not show any evidence of residual or recurrent tumor.
References
- 1. Arita K, Sugiyama K, Tominaga A, Yamasaki F (2001) Intrasellar rhabdomyosarcoma: case report. Neurosurgery 48(3):677–680. [DOI] [PubMed] [Google Scholar]
- 2. Suh Y‐W, Yoo C, Park J‐H, Jung JH, Kim YY (2011) Chiasm‐compressing rhabdomyosarcoma in a patient presumed to have juvenile‐onset open‐angle glaucoma. Clin. Experiment. Ophthalmol 39(2):181–184. [DOI] [PubMed] [Google Scholar]
- 3. Zhong J, Li S‐T, Yao X‐H, Jin B, Wan L (2007) An intrasellar rhabdomyosarcoma misdiagnosed as pituitary adenoma. Surg Neurol 68 Suppl 2:S29–33. [DOI] [PubMed] [Google Scholar]


