Clinical History
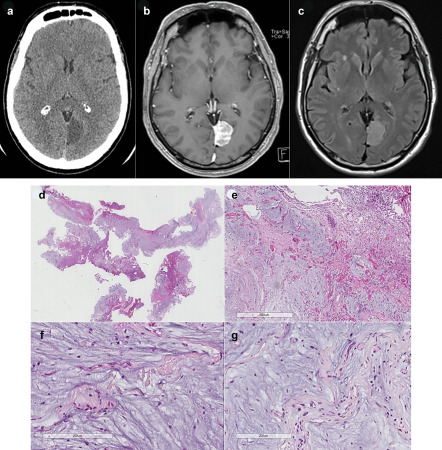
A 50‐year‐old man was followed for 4 years for a radiological diagnosis of meningiomas of the falx cerebri. He was admitted for an evaluation of the mass that had slightly increased in the last year prior to this presentation. General examination disclosed nothing. Computed tomography showed a large hypodense well‐circumscribed mass attached by a broad base to the falx cerebri (Figure 1a). On MRI of the head, the tumor measured 3.5 cm and appeared hypointense on T1‐weighted images and hyperintense on T2‐weighted images. It was uniformly enhanced by Gadolinium contrast injection (Figure 1b) and hyperinstense on T2‐Flair (Figure 1c). There was no parenchymal abnormality. The radiologist interpreted the imaging as suspicious for a meningioma. Due to the recent enlargement of the tumor, a total resection was performed. Intra‐operatively, the lesion was defined by the surgeon as a lesion with a dural‐based attachment suggesting a meningioma.
Figure 1.
Microscopic Pathology
Histopathological examination evidenced a well‐delineated myxoid lesion adhering to the meninges without infiltration (Figure 1d). It was lobulated by thin fibrovascular septa fibrous (Figure 1e). In this myxoid matrix, some mast cells, spindle cells and fibroblasts intertwined with lymphocytes (Figure 1f,g). There was no atypia, no mitotic activity, and no necrosis (Figure 1f,g). On immunohistochemical analysis, there was no staining for GFAP, cytokeratins, muscular markers (smooth muscle actin, desmin) and nuclear receptor of progesterone. Mast cells were immunoreactive for epithelial membrane antigen (EMA) and S‐100 protein. Fibroblasts and endothelial cells were immunostaining by CD34. MIB‐1 was low (inferior to 1%). What is your diagnosis?
Diagnosis
Based on the histopathological findings, the final diagnosis was angiomyxofibroma. The postoperative course was uneventful. There was no recurrence after 1 year of follow‐up.
Discussion
Myxoid lesions include a large and heterogeneous spectrum of entities with an abundant mucopolysaccharidic matrix.
The Angiomyxofibroma of the meninges is an exceptional lesion, only one case having been reported [Medeiros et al in 2006 3].
As in our case, it affected a middle‐age patient (48‐year old women) 3. The tumor was also localized in the falx cerebri 3.
MRI with contrast demonstrates the connection of the mass to the dura‐mater 3.
Histologically, the lesion is compound of an abundant myxoid matrix surrounding by fibrous septa containing a proliferation of small vessels associated with spindle cells, fibroblasts, mast cells and some inflammatory infiltrates, without atypia or mitotic activity 3. The lesion is well‐circumscribed, adherent to the dura‐mater 3.
As in our case, it has been successfully treated by total resection and no recurrence was observed after 6 years of follow‐up.
Differential diagnoses are histopathological including myxoid meningiomas, intracranial myxoma, angiomyxoma, and myxofibrosarcoma.
Despite the dural attachment, the absence of meningothelial features and immunoreactivity for EMA and nuclear receptor of progesterone argue against a myxoid meningioma 2. Myxoid metaplastic meningiomas are very rare WHO Grade I tumors. Only six cases have been reported in the literature. Myxoid meningiomas evidenced typical features of meningiomas such as spindle cells with oval nuclei, along with nuclear pseudoinclusions. They do not present malignant features such as hypercellularity, mitotic figures and necrosis. The myxoid background stains strongly with Alcian blue. The myxoid matrix is due to the excessive presence of hyaluronic acid and chondroitin sulfate. Immunohistochemical staining reveals strong immunoreactivity for EMA and nonspecific cytoplasmic staining for S‐100 protein. The MIB‐1 shows a low proliferation index in all reported cases.
Intracranial myxomas are very rare with only three cases described in the literature 1. Myxomas are benign tumors of primitive mesenchymal tissue, and are usually found in the heart, bones, genitourinary system, and soft tissues. These tumors may be primary or embolic from an underlying cardiac myxoma. There are only a few cases concerning primary intracranial myxomas that have been published in the literature. Primary CNS myxoma is less common than metastatic brain myxoma.
Histological examination of myxomas shows characteristic hypocellular areas of sparse strands of cells suspended in a rich myxoid matrix, strongly positive on Alcian blue stain. Myxomas do not evidence malignant features such as nuclear pleomorphism, hyperchromasia and mitotic activity. Immunohistochemical analysis characteristically shows immunoreactivity for vimentin but no expression of S‐100 protein and EMA. The diagnosis of pure myxoma was dismissed because of the presence of a vascular component described herein 4.
Angiomyxomas are exclusively described in the dermis or subcutaneous tissues or in the female pelvic region 4. Metastatic cases have been reported but no intracranial localization has been described. The tumor is composed of spindle and stellate cells with ill‐defined cytoplasm in an abundant myxoid stroma. Cellularity is low with perivascular densification. Cells have round or oval nuclei, with small, centrally located nucleoli. The stroma is abundant, with prominent myxoid changes. Vascularization is abundant, with variably sized vessels, ranging from small thin‐walled capillaries to larger vessels with medial hypertrophy. Angiomyxomas do not present malignant features such as hypercellularity, mitotic figures and necrosis. Immunostaining is negative for S‐100 protein but nuclear progesterone receptors show high, diffuse positivity. Several studies have demonstrated the implication of HMGA2 rearrangements in the tumorigenesis of aggressive angiomyxomas of the genital tract. In our case, there was no immunohistochemical expression of HMGA2.
Finally, the absence of atypia and mitotic activity does not argue for a myxofibrosarcoma. Primary intracranial myxofibrosarcomas are very rare with less than 10 published cases in the literature. Myxofibrosarcoma is composed of spindle, stellated, and multinucleated cells embedded in a myxoid background. Foci of increased cellularity, pleomorphism, and mitotic figures are present. Immunohistochemical staining shows immunoreactivity for vimentin and CD34.
In conclusion, angiomyxofibroma is a rare entity. Our case illustrates an exceptional case in the meninges.
References
- 1. Graham JF, Loo SY, Matoba A (1999) Primary brain myxoma, an unusual tumor of meningeal origin: case report. Neurosurgery 45:166–169. [DOI] [PubMed] [Google Scholar]
- 2. Krisht KM, Altay T, Couldwell WT (2012) Myxoid meningioma: a rare metaplastic meningioma variant in a patient presenting with intratumoral hemorrhage. J Neurosurg 116:861–865. [DOI] [PubMed] [Google Scholar]
- 3. Medeiros F, Scheithauer BW, Oliveira AM, Gregory RS (2006) Angiomyxofibromatous tumor of the falx cerebri. Am J Surg Pathol 30:545–547. [DOI] [PubMed] [Google Scholar]
- 4. Rawlinson NJ, West WW, Nelson M, Bridge JA (2008) Aggressive angiomyxoma with t(12;21) and HMGA2 rearrangement: report of a case and review of the literature. Cancer Genet Cytogenet 181:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]


