Abstract
Aim
To assess the impact of the COVID-19 pandemic on patients with rheumatic and musculoskeletal diseases (RMDs).
Methods
REUMAVID is a cross-sectional study using an online survey developed by an international multidisciplinary patient-led collaboration across seven European countries targeting unselected patients with RMDs. Healthcare access, daily activities, disease activity and function, well-being (WHO Five Well-Being Index (WHO-5)), health status, anxiety/depression (Hospital Anxiety and Depression Scale (HADS)) and access to information were evaluated. Data were collected in April–July 2020 (first phase).
Results
Data from the first phase included 1800 patients with 15 different RMDs (37.2% axial spondyloarthritis, 29.2% rheumatoid arthritis, 17.2% osteoarthritis and others). Mean age was 53, 80% female and 49% had undertaken university studies. During the beginning of the pandemic, 58.4% had their rheumatology appointment cancelled and 45.6% reported not having received any information relating to the possible impact of SARS-CoV-2 infection in their RMDs, with the main source being patient organisations (27.6%).
Regarding habits, 24.6% increased smoking, 18.2% raised their alcohol consumption, and 45.6% were unable to continue exercising. Self-reported disease activity was high (5.3±2.7) and 75.6% reported elevated pain. Half the patients (49.0%) reported poor well-being (WHO-5) and 46.6% that their health had changed for the worse during lockdown. According to HADS, 57.3% were at risk of anxiety and 45.9% of depression.
Conclusion
Throughout the first wave of the COVID-19 pandemic, patients with RMDs have experienced disruption in access to healthcare services, poor lifestyle habits and negative effects on their overall health, well-being and mental health. Furthermore, information on COVID-19 has not reached patients appropriately.
Keywords: COVID-19, patient perspective, spondylitis, ankylosing, arthritis, rheumatoid, osteoarthritis
Key messages.
What is already known about this subject?
The COVID-19 pandemic has imposed a burden on healthcare systems worldwide that has led to the forced prioritisation of the management of patients affected by SARS-CoV-2 over that of chronic conditions, such as rheumatic and musculoskeletal diseases.
The public health emergency is paralleled by an economic and social crisis to which, according to research, patients with rheumatic and musculoskeletal diseases would be particularly vulnerable.
What does this study add?
The REUMAVID study provides evidence on how the COVID-19 pandemic has affected European rheumatic and musculoskeletal disease (RMD) patients’ physical and psychological health, well-being and lifestyle habits, access to healthcare and treatment as well as access to information and supportive services from the patient’s perspective using an interdisciplinary approach. This complements the already existing clinical body of data and provides a more holistic picture of how patients with RMDs were affected by the pandemic irrespective of whether they contracted COVID-19.
Key messages.
How might this impact on clinical practice?
Throughout the first wave of the COVID-19 pandemic, patients experienced disruptions in access to healthcare services, poor lifestyle habits and worsening physical health, well-being and mental health.
Understanding how patients with RMDs have experienced the COVID-19 pandemic will help to inform actionable strategies, such as the importance of collaborating with patient organisations, for clinicians to best support their patients throughout this and future public health crises.
Introduction
The rapid spread and evolution of the COVID-19 pandemic has marked an unprecedented public health crisis, affecting people worldwide and forcing governments to take harsh containment measures, including national lockdowns. The scientific community responded promptly to COVID-19 by initiating several actions focused on assessing its impact on patients with rheumatic and musculoskeletal diseases (RMDs), such as the EULAR COVID-19 database and the Global Rheumatology Alliance.1 2 In parallel, scientific societies at national and international level developed guidelines and recommendations for patients with RMDs.3–5
There is a concern that the pandemic and associated lockdowns have deeply affected the healthcare and management of RMDs and, subsequently, patient health, irrespective of whether they contracted the virus.6 In response, EULAR issued provisional recommendations to maintain adequate management while remaining sensitive to the healthcare systems; it advised physicians that, for patients with RMDs whose disease is controlled, in-person monitoring visits could be postponed once or twice during a maximum of 6 months and encouraged continued contact through telemedicine.3 Conversely, for patients whose disease is active, rheumatologists and patients should mutually agree on how the disease should be managed (face to face versus virtual) throughout the pandemic. In all cases, EULAR advised patients with RMDs who showed no symptoms of the SARS-CoV-2 virus to continue their treatment unchanged. EULAR acknowledged that despite the need for clear and prompt recommendations, it was unable to formulate definitive guidelines both because of the unprecedented nature of the pandemic and also due to the limited scientific knowledge.3
So far, the research designed to fill these knowledge gaps has been primarily driven by healthcare professionals which, although critical, suffers from an inherent clinical bias and may miss essential aspects relevant to patients. Among the few studies assessing patient experience,7 8 one found an unwillingness among patients with RMDs to attend in-person visits due to fear of contracting SARS-CoV-2.9 In the Netherlands, a study by Hooijberg et al10 found that persons with RMDs were almost twice as likely to adhere to strict isolation measures compared with healthy controls. Further study of patient experience and behaviour throughout the COVID-19 pandemic is equally important to ensure that the rheumatology community has a holistic perspective of patient perspectives and needs.
The present study aims to assess how patients with RMDs in Europe experienced the COVID-19 pandemic and associated national lockdown by using a holistic and interdisciplinary approach. It was our aim to understand the impact on access to healthcare and treatments, physical and psychological health, well-being and lifestyle factors, as well as information received and support services. Ultimately, REUMAVID aims to provide clear recommendations on how to maintain optimal health for persons with RMDs for the ongoing COVID-19 pandemic and future crises.
Methods
Study design
The study consists of a cross-sectional study using an online survey to gather data from persons with a self-reported clinician-provided diagnosis of 15 different RMDs.
Setting
REUMAVID is an international collaboration led by the Health & Territory Research group at the University of Seville (Spain), together with a multidisciplinary team including rheumatologists, psychologists, health researchers, patient research partners, and patient organisations from seven European countries, with the support of Novartis Pharma AG. Patient research partners, together with health researchers and rheumatologists, were involved in all steps of the REUMAVID project including study design, translation of the questionnaire, launching the survey, sample recruitment, and interpretation and dissemination of the results.
Prior to participating in the survey, participants provided informed consent.
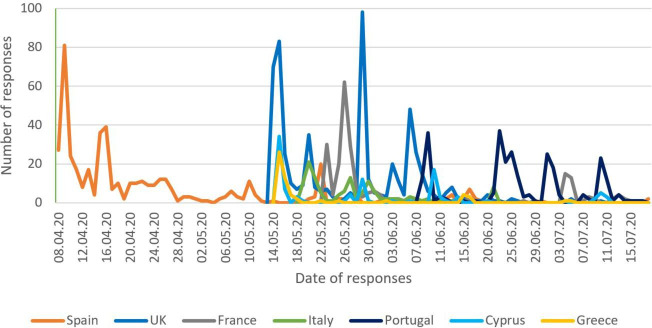
Data included in this study were collected during the first wave of the COVID-19 pandemic (April–July 2020). The survey was launched first in early April in Spain (8 April) and in mid-May in: UK (14 May), Cyprus (15 May), Greece (15 May), Italy (9 May) and France (12 May). Portugal started in early June (8 June). The survey period was closed in all countries on 20 July (figure 1). A second phase of the survey is currently taking place simultaneously in the seven European countries (February–April 2021).
Figure 1.
Number of responses by date and country.
Participants
Participants were recruited through national RMD patient organisations that disseminated the survey link across their channels, reaching both patient members and non-members. Eligible participants were adults older than 18 years of age at the time of study participation, with a self-reported clinician-made diagnosis of RMD and residing in a REUMAVID participating country. Diagnosis was ascertained through the following question: ‘Which of the following conditions were you diagnosed with by a physician?’. Available responses included a list of the following 15 RMDs: ankylosing spondylitis/axial spondyloarthritis (axSpA), fibromyalgia (FM), gout, juvenile idiopathic arthritis, myositis (polymyositis and dermatomyositis), osteoarthritis (OA), osteoporosis (OP), peripheral spondyloarthritis, polymyalgia rheumatica, psoriatic arthritis, rheumatoid arthritis (RA), synovitis, acne, pustulosis, hyperostosis and, osteitis (SAPHO), Sjögren’s syndrome, systemic lupus erythematosus, systemic sclerosis (or scleroderma) and vasculitis or arteritis. Furthermore, to participate, it was required to have had a visit with their rheumatologist in the previous 12 months (unless suspended due to the COVID-19 pandemic). Participants were volunteers, and no selection was intended.
Variables
To ensure that the questionnaire addressed topics that are most relevant to patients during the COVID-19 pandemic, the Spanish patient organisation (Spanish Federation of Spondyloarthritis Associations (CEADE)) shared the most frequently expressed COVID-19-related concerns and priorities from patients to their organisation. Based on this information, an extensive list of key issues was drawn up, creating a questionnaire of 120 items, grouped in the following domains: (1) sociodemographic characteristics, (2) lifestyle habits, (3) job status and working conditions, (4) disability and financial support, (5) patient organisations and institutional support, (6) physical activity and psychological care, (7) contact with COVID-19, (8) healthcare access and treatment and (9) health status. A summary of main indicators of the REUMAVID survey is shown in table 1.
Table 1.
Main areas of the REUMAVID survey and associated items
| Area | Variables/indicators |
| Sociodemographic characteristics | Gender, province and city/town of residence, educational level, marital status, no. of children, height and weight. |
| Habits and lifestyle | Smoking and drinking habits, social interaction, outdoor contact and groceries management. |
| Employment status and working conditions | Employment status, area of work, main occupation, key worker, and change in work situation (change). |
| Disability and financial support | Population at risk, entitlement to disability benefits, and financial support packages for COVID-19. |
| Patient organisations and institutional support | Patient organisation membership, support from patient organisation, source of information on COVID-19 (and quality of information), and frequency of COVID-19 information search. |
| Physical activity and psychological care | Physical activity, psychological/psychiatric care (type, discontinuation and consequences). |
| Contact with COVID-19 | Contact with COVID-19 and relatives with COVID-19. |
| Healthcare access and treatment | Visits to rheumatologist (frequency, discontinuation and reasons), access to rheumatologist (tries and results), access to GP, treatment (type, discontinuations and reasons), and difficulties getting medication. |
| Health status | Self-perceived health status, changes in health status, well-being (WHO-5), anxiety and depression (HADS), disease activity (VAS), pain (PASS), satisfaction with health status and comorbidities. |
HADS, Hospital Anxiety and Depression Scale; PASS, Patient Acceptable Symptom Scale; VAS, Visual Analogue Scale; WHO-5, WHO Five Well-Being Index.
The REUMAVID questionnaire was initially developed in Spanish and later translated into English, French, Greek, Italian and Portuguese. Patient organisations from participating countries were invited to revise and make minor changes to the questionnaire to ensure it reflected the national contexts and concerns of local patients.
Measurement
The questionnaire included a number of validated scales to measure well-being, risk of anxiety and depression, disease activity and functional limitation.
The WHO Five Well-Being Index (WHO-5): This scale is composed of five items that evaluate overall well-being through a 6-point Likert scale from 0 (all of the time) to 5 (at no time), resulting in a total score ranging from 0 to 100. Higher values represent a worse state of well-being.11 Further research has shown adequate validity as an outcome measure in a wide range of study fields.12
Hospital Anxiety and Depression Scale (HADS): the HADS questionnaire is composed of two parts. The first includes seven items to screen for depression; the second includes seven items to screen for anxiety disorders. A score between 0 and 3 is assigned to each item. The total score ranges from 0 to 21, and higher scores indicate the presence of anxiety and depression classified into three severity categories: no case (0–7), borderline case (8–10), and case (11–21).13 The HADS has been found to perform well in assessing symptom severity and the presence of anxiety and depression disorders in the general population.14
Visual Analogue Scale (VAS) for disease activity and Patient Acceptable Symptom Scale: two different scales ranging from 0 to 10 were introduced in the questionnaire to evaluate disease activity and pain. The use of this form of evaluation has been validated in international studies of different RMDs such as RA, AS, chronic back pain, hand OA, and hip and knee OA.15
Study size
A total of 2731 patients with RMDs participated in the first phase of the REUMAVID survey, of which 931 were discarded for failing to complete at least 70% of the survey questionnaire, resulting in a sample size of 1800 participants.
Statistical methods
The results are presented as summary statistics, with mean and SD for continuous variables, and frequency and percentages for categorical variables. For those survey items with missing values, reduced sample sizes are reported in order to eliminate unwanted bias. Data analysis was conducted using SPSS V.25.0.
Results
Of the total of 1800, 558 participants were from the UK (31.0%), 464 from Spain (25.8%), 264 from Portugal (14.7%), 229 from France (12.7%), 127 from Italy (7.1%), 101 from Cyprus (5.6%), and 57 from Greece (3.1%). As shown in the European map, there was a female predominance in all the countries (figure 2).
Figure 2.
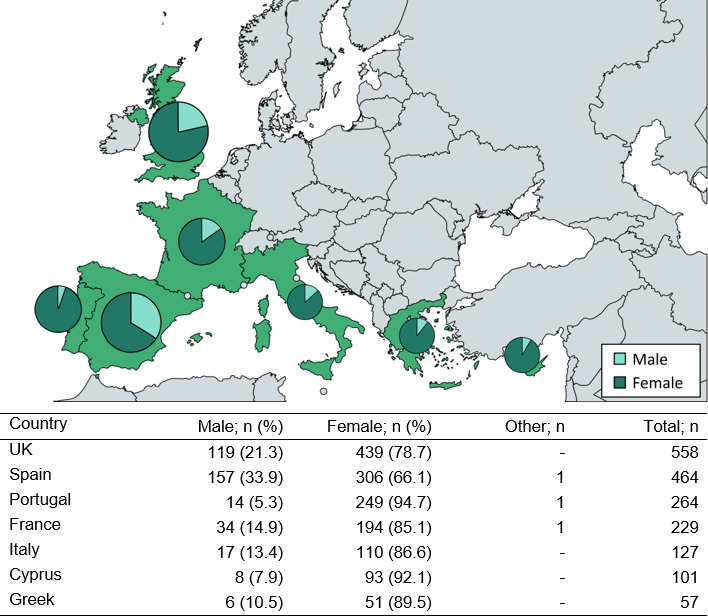
Gender distribution of REUMAVID participants by country (N=1800).
Sociodemographic characteristics
The RMD with highest representation in the sample was axSpA (37.2%) followed by RA (29.2%), FM (17.3%), and OA (17.2%). Although the majority of patients reported having only one RMD, a percentage of 26.3% (n=474) of patients reported having two or more rheumatic diseases. Online supplemental table 1 shows the distribution of each rheumatic disease in the different countries. The most frequent combination were RA and FM (5.1%; n=54), OA and OP (4.6%; n=22), and axSpA and FM (4.0%; n=19). Mean age was 52.6±13.2 (16.3% of patients were 67 years old or more), 80.1% were women, 48.6% had undertaken university studies, 69.6% were married or in a relationship, 34.7% were employed, and 22.4% retired (table 2).
Table 2.
Sociodemographic characteristics of the REUMAVID sample (N=1800, unless otherwise specified)
| Variables | n (%) or mean±SD |
| Rheumatic disease | |
| Axial spondyloarthritis | 670 (37.2) |
| Rheumatoid arthritis | 534 (29.2) |
| Fibromyalgia | 312 (17.3) |
| Osteoarthritis | 310 (17.2) |
| Psoriatic arthritis | 165 (9.1) |
| Osteoporosis | 114 (6.3) |
| Sjögren’s syndrome | 104 (5.8) |
| Systemic lupus erythematosus | 97 (5.4) |
| Peripheral spondyloarthritis | 50 (2.8) |
| Juvenile idiopathic arthritis | 38 (2.1) |
| Gout | 36 (2.0) |
| Systemic sclerosis (or scleroderma) | 30 (1.7) |
| Vasculitis or arteritis | 24 (1.3) |
| Polymyalgia rheumatica | 13 (0.7) |
| Myositis (polymyositis and dermatomyositis) | 7 (0.4) |
| SAPHO (only recorded in France) | 15 (0.8) |
| Age | 52.6±13.2 |
| Gender | |
| Male | 355 (19.7) |
| Female | 1442 (80.1) |
| Other | 3 (0.2) |
| Educational level | |
| No studies | 20 (1.1) |
| Primary school | 72 (4.0) |
| Secondary school | 307 (17.1) |
| Vocational qualification | 527 (29.3) |
| University studies | 874 (48.6) |
| Employment status | |
| Employed | 625 (34.7) |
| Temporary sick leave | 159 (8.8) |
| Permanent sick leave | 86 (4.8) |
| Retirement | 403 (22.4) |
| Early retirement | 60 (3.3) |
| Unemployed | 85 (4.7) |
| Furlought | 112 (6.2) |
| Housework | 64 (3.6) |
| Student | 19 (1.1) |
| Other | 187 (10.4) |
| Marital status | |
| Single | 287 (15.9) |
| Married/in a relationship | 1253 (69.6) |
| Separated/divorced | 195 (10.8) |
| Widower/widow | 65 (3.6) |
rmdopen-2020-001546supp001.pdf (58.5KB, pdf)
Access to healthcare, information resources and treatment
Regarding access to healthcare during lockdown, 1062 participants (59.0% of the total sample) did not have a follow-up appointment with their rheumatologist. Of those who did, more than half (58.4%, n=422) had their appointment cancelled. Of these, 54.4% (n=224) were offered a virtual or telephone consultation, whereas 35.2% (n=145) were given no alternative appointment or follow-up. A further 9.2% (n=38) of participants did not attend a scheduled appointment for fear of contracting COVID-19 and 1.2% (n=5) did not attend because they did not have the financial or transportation means.
A total of 430 participants tried to reach their rheumatology service for information on the possible effects of COVID-19 on their treatment, with 36.0% (n=155/430) unable to do so. A percentage of 42.4% (n=292) also reported being unable to contact their general practitioner (GP) and 51.7% (n=226) were unable to continue their psychological or psychiatric therapy, neither online nor by phone.
Of the 1718 REUMAVID participants who answered the question on information about how COVID-19 could affect their RMD, nearly half (45.6%, n=784) reported not having received any specific information. Those who did, reported patient organisations as the most frequent source (27.6%, n=475), followed by rheumatologists (24.3%, n=418), GPs (14.9%, n=256) and scientific rheumatology societies (11.1%, n=190).
With regards to medication, before the first lockdown, REUMAVID participants were receiving biologics (53.5%, n=963), non-steroidal anti-inflammatory drugs (NSAIDs) (39.2%, n=705), painkillers (33.3%, n=600), methotrexate (21.8%, n=393), and oral corticosteroids (18.6%, n=335). Of the 1707 participants answering this question, 15.8% (n=269) had their treatment changed. Participants could provide more than one reason for treatment change. Of the total of 281 answers provided, most of the cases were due to a decision by their healthcare team (65.5%, n=184), concerns about the increased risk of contracting COVID-19 (24.6%, n=69), inability to go to hospital for treatment (5.0%, n=14), followed by the inability to receive infusions in hospital (3.2%, n=9), and the shortage of available treatments (1.8%, n=5).
Lifestyle factors, daily activities and employment during lockdown
REUMAVID participants reported a number of behavioural changes during the COVID-19 pandemic and lockdown. Changes in lifestyle, daily activities and employment are depicted in table 3. On the one hand, an important percentage of participants declared a change for the worse in their lifestyle with physical exercise discontinuation, increasing drinking and smoking and weight gain. On the other hand, some participants reported to decrease their drinking and smoking habits but to a lesser extent. Ability to take outdoor walks during lockdown showed both extremes, with 27.2% (n=490) reporting daily walks and 25.3% (n=455) reporting no outdoor walks throughout lockdown.
Table 3.
Changes in lifestyle, daily activities and employment during COVID-19 lockdown (N=1800, unless otherwise specified)
| Lifestyle factors | N (%) |
| Continue to exercise at home during lockdown (n=1128) | |
| Yes | 444 (39.4) |
| No | 514 (45.6) |
| No, but compensates with another exercise | 170 (15.1) |
| Smoking habit during lockdown | |
| Yes | 373 (20.7) |
| No | 1427 (79.3) |
| Changes in smoking habit during lockdown (n=556) | |
| I've started smoking | 18 (3.2) |
| More than before | 137 (24.6) |
| Same as before | 187 (33.6) |
| Less than before | 57 (10.3) |
| I’ve quit smoking | 157 (28.2) |
| Changes in drinking habit during lockdown (n=1085) | |
| More than before | 197 (18.2) |
| The same amount as before | 404 (37.2) |
| Less than before | 136 (12.5) |
| I’m not drinking | 348 (32.1) |
| Weight change during lockdown | |
| I am gaining weight | 736 (40.9) |
| I'm maintaining my weight | 876 (48.7) |
| I'm losing weight | 188 (10.4) |
| Employment changes during COVID-19 pandemic | |
| How has your way of working been affected by the COVID-19 pandemic? (n=901) | |
| I'm still working in my regular workplace and workhours (as before COVID-19) | 132 (14.7) |
| I still come in person, with changes to time or place of work | 119 (13.2) |
| I am teleworking (working from home) | 359 (39.8) |
| Temporary sick leave caused by COVID-19 | 118 (13.1) |
| I've been fired because of COVID-19 | 33 (3.7) |
| I've had to close my business | 28 (3.1) |
| I have been furloughed | 112 (12.4) |
| Contact with outside during the COVID-19 pandemic lockdown | |
| Have you been out in any natural environment (eg, forest and parks)? (n=1429) | |
| Yes | 563 (39.4) |
| No | 866 (60.6) |
| How often did you go outside for a walk? (n=1800) | |
| Every day | 490 (27.2) |
| 5 days a week | 91 (5.1) |
| Between 2 and 4 days a week | 272 (15.1) |
| One day a week or less | 492 (27.3) |
| Never | 455 (25.3) |
| How are you managing to purchase your groceries? (n=591) | |
| I am going to the supermarket as usual | 209 (35.4) |
| Someone else in my household is going to the supermarket | 200 (33.8) |
| Someone from outside my household is bringing my groceries to me | 39 (6.6) |
| I am ordering my groceries online or by phone | 143 (24.2) |
With regard to work activity, 39.8% (n=359) reported teleworking from home, with only 14.7% (n=132) of participants reporting no change to their job routine. Of note, 343 (36.8%) declared themselves to be key workers during the COVID-19 pandemic.
Health status
Although it was not the main goal of the study, we asked participants whether they had contracted COVID-19. The majority declared that they had not contracted the SARS-CoV-2 (88.1%, n=1586), while approximately 10.8% (n=195) reported having experienced symptoms but without a test confirmation, and only 1.1% (n=19) having had a positive test.
Despite the low COVID-19 incidence in this population, nearly half of participants (46.6%; n=832) declared that their health worsened during lockdown. In addition, nearly half reported poor well-being according to the WHO-5 and three out of four declared high levels of pain. 21.2% (n=252) of patients presented sleep disorders. Moreover, mental health was also poor, with 57.3% (n=1013) at risk of anxiety (32.7% cases and 24.6% probable cases) and 45.9% (n=811) at risk of depression (21.1% cases and 24.8% probable cases), according to the HADS. Further characteristics on health status and well-being of REUMAVID participants are showed in table 4.
Table 4.
Self-perceived health, well-being, mental health and disease activity (N=1800, unless otherwise specified)
| Variables | n (%) or mean±SD |
| Self-perceived health status (n=1786) | |
| Very good | 125 (7.0) |
| Good | 519 (29.1) |
| Fair | 802 (44.9) |
| Bad | 293 (16.4) |
| Very bad | 47 (2.6) |
| Change in health status during lockdown | |
| Much worse than before | 182 (10.2) |
| Moderately worse | 650 (36.4) |
| Same as before | 843 (47.2) |
| Moderately better | 97 (5.4) |
| Much better than before | 14 (0.8) |
| Visual Analogue Scale for disease activity (0–10) (n=1756) | 5.3±2.7 |
| Patient Acceptable Symptom Scale | |
| Overall pain during last week (0–10) (n=1421) | 6.0±3.0 |
| Overall pain ≥4 (0–10) (n=1421) | 1074 (75.6) |
| Dissatisfaction with health status if prolonged in future months on lockdown (n=1421) | 743 (52.3) |
| WHO-5 (0–100) (n=1777) | 50.7±23.9 |
| Poor well-being (WHO-5 ≤50) | 870 (49.0) |
| Mental health (n=1769) | |
| HADS anxiety (0–21) | |
| No case (0–7) | 756 (42.7) |
| Borderline case (8–10) | 435 (24.6) |
| Case (11–21) | 578 (32.7) |
| HADS depression (0–21) | |
| No case (0–7) | 958 (54.2) |
| Borderline case (8–10) | 438 (24.8) |
| Case (11–21) | 373 (21.1) |
HADS, Hospital Anxiety and Depression Scale; WHO-5, WHO Five Well-Being Index.
Online supplemental table 2 shows the main sociodemographic and clinical characteristics of each of the rheumatic diseases, highlighting higher disease activity and pain in patients with gout and peripheral spondyloarthritis, higher risk of anxiety in patients with systemic sclerosis (or scleroderma) and FM, and higher risk of depression in patients with polymyalgia rheumatica and FM.
Discussion
The main study focus related to effects of the COVID-19 pandemic to date has been mostly on the infection and mortality rate at population level. Unfortunately, the broader implications of the pandemic and lockdown on patients affected by chronic diseases, such as RMDs, have been largely neglected. Results from REUMAVID, a international study including 1800 unselected patients with RMDs among which the prevalence of confirmed and suspected COVID-19 cases was low, show that the effects of the first wave of the pandemic and lockdown extended far beyond those directly impacted by SARS-CoV-2.
During the first COVID-19 related lockdowns in Europe, healthcare providers were required to balance continued access to care with the needs of a pressured healthcare system. A EULAR survey administered to rheumatologists and HCPs revealed that containment measures had led to a postponement of treatment decisions, negatively impacting both early treatment and treat-to-target strategies.16
We can see this strongly reflected in the REUMAVID results, with more than half of patients having had their routine rheumatologist appointment cancelled. Fortunately, half of these patients were then offered a tele-consultation, which is both in accordance with EULAR’s provisional guidance and a demonstration of fast adaptation among rheumatologists.3 6
However, despite this response, a third of patients had their appointment cancelled without being provided with an alternative follow-up. Taking this into consideration, patients’ reported limited physical activity, worsening health, and high levels of pain. This lack of follow-up leads to the question as to whether the decision to cancel was made together with the patient, as recommended by EULAR, or if the respective healthcare professionals were adequately or technologically equipped to continue supporting their patients. Both cases underline the importance of shared decision making and emerging telemedicine systems in facilitating ongoing patient–physician communication and optimising healthcare during crises.17 18
Another critical element to maintaining optimal health is access to reliable information. Unfortunately, nearly half of the participants in the REUMAVID study reported not having received information related to how COVID-19 may affect them. Some sought support from their GPs or rheumatologists for treatment-related questions but were not able to receive a response. As such, we can assume that the lack of trustworthy information plausibly played a role in the minority of patients who decided to stop/change their treatment without consulting their physician or who chose to not attend their appointments due to fear of contracting COVID-19. In addition, access to credible information about the effects of SARS-CoV-2 on patients with RMDs may have influenced them to better cope with uncertainty and make appropriate decisions, such as exercising or quitting smoking while in lockdown.
Nevertheless, it is true that neither the scientific nor the patient community could have foreseen the arrival of the COVID-19 pandemic. The REUMAVID results do show us that both were successful in disseminating credible information, with patients who received information having accessed it mainly from patient organisations and rheumatologists. Enabling both patient organisations and physicians to provide information is paramount; patient organisations in particular act in many ways as part of the extended healthcare team, offering information and access to supportive services like mental health counselling or virtual exercise classes despite suffering from limited resources.
With all of this in mind, it is not surprising that the COVID-19 pandemic and lockdown have negatively affected the health of patients with RMDs in this study. High levels of disease activity and pain, poor well-being and worsening health status were consistently reported. Furthermore, 57.3% (n=1013) of REUMAVID participants were at risk of anxiety (32.7% cases and 24.6% probable cases) and 45.9% (n=811) at risk of depression (21.1% cases and 24.8% probable cases), according to the HADS. These prevalences of anxiety and depression cases obtained in the present study are higher overall than those reported in prepandemic studies, using the same scale (HADS), and cut-off point among patients with RMDs without other complications or stressors as in our study. It is important to highlight that patients with FM tend to present higher rates of anxiety and depression. Thus, a multicentre study in Spanish patients with FM found anxiety cases from 18% to 26% and depression cases from 22% to 26%.19 However, in relation to RA, a single-centre study including 150 Canadian patients with RA found rates of 13.4% for anxiety cases and 9.3% for depression cases.20 Another study on Chinese patients with axSpA found rates of 15.6% for anxiety cases and 10.6% for depression cases.21
Furthermore, patients also reported increased smoking and alcohol consumption, weight gain and decreased physical activity, alongside the inability to continue with rehabilitation exercises or physiotherapy programmes. It is important here to reflect on the influence of factors such as weight gain, physical activity, and mental health on disease activity, since the majority of patients did not have their treatment changed. It is also possible that compliance with treatment, which was not measured in the study, may have reduced throughout this period of time, potentially as a result of the limited contact between patients and rheumatologists and an increased mental health risk.22
REUMAVID is the first international study that has addressed the consequences of the COVID-19 pandemic on patients with RMDs, accounting for the different spheres of life that are important from the patient’s perspective. Data were collected from seven European countries with different socioeconomic contexts, as well as a differing evolution and response to the pandemic, which may provide an accurate and unique profile of the reality of patients with RMDs at European level during the COVID-19 pandemic. Furthermore, the study was developed in partnership with patient organisations and rheumatologists, ensuring that the data were relevant both to patients and clinicians.
However, REUMAVID is not exempt from limitations. First, the survey was based on self-reported data, and the diagnosis of participants was not confirmed by medical records or examinations. Second, the distribution of RMDs does not match the prevalence of these diseases in the general population. Specifically, there is an over-representation of patients with axSpA, which is due to the higher presence of axSpA patient organisations involved in the dissemination of the survey. In particular: The National Axial Spondyloarthritis Society (NASS) in the UK and the Spanish Federation of Spondyloarthritis Associations (CEADE) in Spain. Further research is needed on the impact of the COVID-19 pandemic on patients with RMDs that are under-represented in the REUMAVID survey. Additionally, a descriptive analysis of this sample characteristics showed a larger representation of middle-aged, highly educated women. The reasons for this gender bias could be related to women's greater willingness to participate in online surveys.23 Gender bias could also be due to the higher female prevalence in some of the most represented RMDs such as RA,24 FM25 26 or OA.27 28 Moreover, it is important to highlight the over-representation of university-educated patients in the sample, which represent a population more capable to access credible information and self-help, in itself a mitigating factor against the social impact of the pandemic, suggesting that the results presented here may underestimate the reality of those with lower educational level. Nevertheless, the characteristics of this study population are consistent with those of previous survey cohorts. Furthermore, as the aim of the survey was to capture the patient’s perspective, reaching unattended patients and understand the limitations imposed by the pandemic itself, online recruitment through patient organisations was preferred.
Although the survey collected information between early April and mid-July 2020 from seven countries, the spread of the pandemic and lockdown measures varied between these countries, which may have affected the overall patient experience and, subsequently, the results. It is also true that the pandemic has had an uneven impactwithin countries (ie, sub-national differences between regions, between large cities versus rural areas, or between countries with centralised versus decentralised health systems).
Finally, RMDs were not uniformly represented, because although most patient organisations represented all rheumatic conditions in general, some deal specifically with axSpA and RA. This, together with the differences in prevalence, meant that diseases such as the axSpA, RA or OA were more strongly represented than the rest. In addition, results for disease activity should be interpreted with caution as the only instrument employed to assess this outcome was disease activity VAS.
In summary, REUMAVID highlighted the impact of the COVID-19 pandemic on the health and well-being of patients with RMDs. Although the percentage of patients who interrupted their pharmacological treatment was low, many could not be seen by their rheumatologist, nor could they continue with their physical exercise or therapy. These factors, together with an increase in unhealthy behaviours, may have led to the self-perceived worsening of health and increased risk of anxiety and depression. The COVID-19 pandemic has created an unprecedented crisis requiring urgent measures to support patients in remaining healthy, including the implementation of digital technologies that facilitate ongoing patient–physician communication, as well as ensuring access to credible information that enables patients to manage their health and participate in shared decision making. In addition, this study highlights the increasing role of patient organisations, acting as an extended member of the healthcare team and providing access to supportive services like virtual exercise courses or mental health counselling, which are especially critical for RMD patients in times of crisis.
Acknowledgments
We would like to thank all patients who completed the survey as well as all of the patient organisations that participated in the REUMAVID study including: the Cyprus League Against Rheumatism from Cyprus, the Association Française de Lutte Anti-Rhumatismale from France, the Hellenic League Against Rheumatism from Greece, the Associazione Nazionale Persone con Malattie Reumatologiche e Rare from Italy, the Portuguese League Against Rheumatic Diseases from Portugal, the Spanish Federation of Spondyloarthritis Associations, the Spanish Patients’ Forum, UNiMiD, Spanish Rheumatology League, Andalusian Rheumatology League, Catalonia Rheumatology League and Galician Rheumatology League from Spain, and the National Axial Spondyloarthritis Society, National Rheumatoid Arthritis and Arthritis Action from the UK.
Footnotes
Twitter: @MarcoGarridoCum, @carmona_loreto
Contributors: MG-C, HM-O, LC, JC-F, SS-G and VN-C contributed to study conception and design. All authors contributed to the analysis and interpretation of data, made significant contributions to drafting and revising the article, provided intellectual content of critical importance to the work and approved the final version to be published.
Funding: This study was supported by Novartis Pharma AG.
Disclaimer: The views expressed are those of the author and not necessarily those of the UK National Health Service (NHS), the NIHR or the UK Department of Health.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: HM-O reports grant/research support from: Janssen and Novartis, consultant for: AbbVie, Celgene, Janssen, Lilly, Novartis, Pfizer and UCB, speakers’ bureau: AbbVie, Biogen, Celgene, Janssen, Lilly, Novartis, Pfizer, Takeda and UCB. HM-O is supported
by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre.
LC is an employee of Novartis Pharma AG. CJ has received grant funding from Abbvie, Amgen, Biogen, Eli Lilly, Gilead, Janssen, Pfizer, Roche, Sanofi and UCB. DW has received grant funding from AbbVie, Biogen, Janssen, Lilly, Novartis and UCB. SI has received funding from the Coronavirus Community Support Fund, distributed by The National Lottery Community Fund. SM reports unrelated honoraria from Novartis, GSK and Bayer. EF-M has received support for specific activities: grants and non-financial from Pfizer, grants from Lilly Portugal, Sanofi, AbbVie, Novartis, Grünenthal. SA., MSD, Celgene, Medac, Janssen-Cilag, Pharmakern and GAfPA, and non-financial support from Grünenthal GmbH. VN-C reports honoraria/research support from: Abbvie, BMS, Janssen, Lilly, MSD, Novartis, Pfizer, Roche and UCB.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Deidentified participant data are available on reasonable request to MG-C.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
REUMAVID was first approved by the ethical committee of University Hospital La Paz under the code PI-4121 and was subsequently approved in all other participating countries as legally required.
References
- 1.EULAR . EULAR COVID-19 database, 2020. Available: https://www.eular.org/eular_covid19_database.cfm [Accessed 2 Jul 2019].
- 2.Robinson PC, Yazdany J. The COVID-19 global rheumatology alliance: collecting data in a pandemic. Nat Rev Rheumatol 2020;16:293–4. 10.1038/s41584-020-0418-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landewé RBM, Machado PM, Kroon F, et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann Rheum Dis 2020;79:851–8. 10.1136/annrheumdis-2020-217877 [DOI] [PubMed] [Google Scholar]
- 4.Richez C, Flipo R-M, Berenbaum F, et al. Managing patients with rheumatic diseases during the COVID-19 pandemic: the French Society of rheumatology answers to most frequently asked questions up to may 2020. Joint Bone Spine 2020;87:431–7. 10.1016/j.jbspin.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mikuls TR, Johnson SR, Fraenkel L, et al. American College of rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: version 2. Arthritis Rheumatol 2020;72:e1–12. 10.1002/art.41437 [DOI] [PubMed] [Google Scholar]
- 6.Kirby T. Rheumatologists rapidly adjust patient care during COVID-19 pandemic. Lancet Rheumatol 2020;2:e258. 10.1016/S2665-9913(20)30094-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sirotich E, Dillingham S, Grainger R, et al. Capturing Patient‐Reported outcomes during the COVID‐19 pandemic: development of the COVID‐19 global rheumatology alliance patient experience survey. Arthritis Care Res 2020;72:871–3. 10.1002/acr.24257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020;14:779–88. 10.1016/j.dsx.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seyahi E, Poyraz BC, Sut N, et al. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol Int 2020;40:1229–38. 10.1007/s00296-020-04626-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hooijberg F, Boekel L, Vogelzang EH, et al. Patients with rheumatic diseases adhere to COVID-19 isolation measures more strictly than the general population. Lancet Rheumatol 2020;2:e583–5. 10.1016/S2665-9913(20)30286-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organisation . Wellbeing Measures in Primary Health Care/ The Depcare Project. Rep a WHO Meet, 1998. Available: http://www.euro.who.int/__data/assets/pdf_file/0016/130750/E60246.pdf
- 12.Topp CW, Østergaard SD, Søndergaard S, et al. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom 2015;84:167–76. 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 14.Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 2002;52:69–77. 10.1016/s0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 15.Tubach F, Ravaud P, Martin-Mola E, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multina. Arthritis Care Res 2012;64:1699–707. 10.1002/acr.21747 [DOI] [PubMed] [Google Scholar]
- 16.Dejaco C, Alunno A, Bijlsma JW, et al. Influence of COVID-19 pandemic on decisions for the management of people with inflammatory rheumatic and musculoskeletal diseases : a survey among EULAR countries. Ann Rheum Dis 2020 10.1136/annrheumdis-2020-218697. [Epub ahead of print: 06 Nov 2020]. [DOI] [PubMed] [Google Scholar]
- 17.Santos-Moreno P, Chavez-Chavez J, Hernández-Zambrano SM, et al. Experience of telemedicine use in a big cohort of patients with rheumatoid arthritis during COVID-19 pandemic. Ann Rheum Dis 2020. 10.1136/annrheumdis-2020-218165. [Epub ahead of print: 25 Jun 2020]. [DOI] [PubMed] [Google Scholar]
- 18.Schulze-Koops H, Specker C, Krueger K. Telemedicine holds many promises but needs to be developed to be accepted by patients as an alternative to a visit to the doctor. Response to: ‘Patient acceptance of using telemedicine for follow-up of lupus nephritis in the COVID-19 outbreak’ by So et al. Ann Rheum Dis 2020. 10.1136/annrheumdis-2020-218235. [Epub ahead of print: 24 Jun 2020]. [DOI] [PubMed] [Google Scholar]
- 19.Luciano JV, Barrada JR, Aguado J, et al. Bifactor analysis and construct validity of the HADS: a cross-sectional and longitudinal study in fibromyalgia patients. Psychol Assess 2014;26:395–406. 10.1037/a0035284 [DOI] [PubMed] [Google Scholar]
- 20.Hitchon CA, Zhang L, Peschken CA, et al. Validity and reliability of screening measures for depression and anxiety disorders in rheumatoid arthritis. Arthritis Care Res 2020;72:1130–9. 10.1002/acr.24011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan CYY, Tsang HHL, Lau CS, et al. Prevalence of depressive and anxiety disorders and validation of the hospital anxiety and depression scale as a screening tool in axial spondyloarthritis patients. Int J Rheum Dis 2017;20:317–25. 10.1111/1756-185X.12456 [DOI] [PubMed] [Google Scholar]
- 22.Goh H, Kwan YH, Seah Y, et al. A systematic review of the barriers affecting medication adherence in patients with rheumatic diseases. Rheumatol Int 2017;37:1619–28. 10.1007/s00296-017-3763-9 [DOI] [PubMed] [Google Scholar]
- 23.Smith G, Smith WG. Does gender influence online survey participation?: a record-linkage analysis of university faculty online survey response behavior, 2008. Available: https://scholarworks.sjsu.edu/elementary_ed_pub [Accessed 2 Jul 2019].
- 24.Dougados M, Soubrier M, Antunez A, et al. Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Ann Rheum Dis 2014;73:62–8. 10.1136/annrheumdis-2013-204223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marques AP, Santo AdeSdoE, Berssaneti AA, et al. Prevalence of fibromyalgia: literature review update. Rev Bras Reumatol Engl Ed 2017;57:356–63. 10.1016/j.rbre.2017.01.005 [DOI] [PubMed] [Google Scholar]
- 26.Wolfe F, Walitt B, Perrot S, et al. Fibromyalgia diagnosis and biased assessment: sex, prevalence and bias. PLoS One 2018;13:e0203755–14. 10.1371/journal.pone.0203755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol 2018;30:160–7. 10.1097/BOR.0000000000000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pereira D, Peleteiro B, Araújo J, et al. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage 2011;19:1270–85. 10.1016/j.joca.2011.08.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2020-001546supp001.pdf (58.5KB, pdf)
Data Availability Statement
Deidentified participant data are available on reasonable request to MG-C.