Clinical History and Radiology
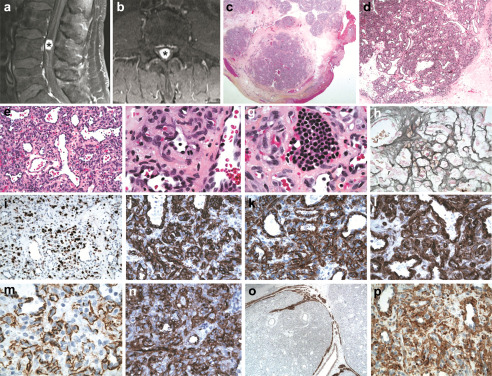
A 64‐year‐old man with a history of hyperlipidemia and hypertension presented to neurosurgery clinic with progressive pain in the left lower limb and mid‐back. Sagittal (Figure 1a) and axial (Figure 1b) T1‐weighted MRI of the lumbar spine showed a 1.3 × 1.1 × 1.2 cm homogeneously enhancing, intradural, ovoid and slightly lobulated solid mass at the L4 vertebral level. The lesion occupied the majority of the thecal sac, with resulting splaying and compression of the nerve roots of the cauda equina. The MRI features favored a nerve root meningioma with a differential of a schwannoma while metastatic disease was thought to be a less likely diagnostic consideration. The patient underwent elective lumbar laminectomy L3 through L5. The lesion was identified by ultrasound before opening the dura. The tumor was found to arise from a lumbosacral nerve root and had a purple‐brown appearance. It was elevated out of the cauda equina and the surrounding proximal and distal nerves were separated from the mass before its complete gross removal. The patient recovered uneventfully from the procedure with no neurological deficits and remains recurrence‐free 1 year after the diagnosis.
Figure 1.
Pathology
The mass was a tan, focally hemorrhagic nodule with a rubbery consistency, measuring 1.3 × 1.3 × 1.1 cm. Microscopic evaluation of hematoxylin‐phloxine‐saffron stained sections show a nodular lesion with numerous vessels (Figure 1c–f) some of which had a “staghorn” configuration (Figure 1d). The stromal cells had moderately pleomorphic oval to elongated medium‐sized nuclei, frequently containing small to intermediate sized nucleoli (Figure 1f). There were 3 mitoses per 10 HPF and small foci of erythropoiesis (Figure 1g). There was no necrosis. Reticulin staining highlighted the vascular network (Figure 1h). Ki‐67 immunostaining (Figure 1i) showed an approximately 30% proliferative index by visual assessment and 34% by ImageJ automated scoring. Immunostaining was positive for CD34 (Figure 1j), CD99 (Figure 1k) and BCL2 (Figure 1l) and vimentin. CD31 showed membranous staining of stromal cells (Figure 1m). These cells were positive for factor VIII (Figure 1n). Lesional cells also were positive for smooth muscle actin (SMA) (Figure 1o). The tumor cells were negative for desmin, MA, GFAP, NSE, synaptophysin, chromogranin, inhibin and pan‐cytokeratin. There were thin bundles of peripheral nerve highlighted by neurofilament (Figure 1p) and NSE immunostaining. What is your diagnosis?
Diagnosis
Capillary hemangioma.
Discussion
Capillary hemangioma is a benign vascular neoplasm commonly involving the skin, soft tissue and mucosal membranes of the head and neck region 4. Central nervous system (CNS) involvement is relatively uncommon, but is a recognized occurrence. Spinal intradural extramedullary capillary hemangiomas are extremely rare 3, Complete resection is the treatment of choice and follow‐up of 10 patients demonstrated no clinical recurrence in the neuraxis 1. However, amongst the additional nine cases reported since 2005 2, 4 is the recent case of recurrent capillary hemangioma of the spinal cord in a 48‐year‐old man that developed 6 months after the first operation.
Spinal level capillary hemangiomas have been reported in adults and adolescents. These tumors can occur in the thoracic area or in close relation to the conus medullaris and nerve roots of the cauda equina. Clinical presentation and radiologic appearance of spinal intradural extramedullary capillary hemangiomas are similar to those of more common intradural lesions of the same location 2. These lesions are usually encapsulated and well demarcated from the surrounding parenchyma of the spinal cord and affected nerve roots 4. Although the presence of enlarged vasculature may be a useful clue, the magnetic resonance imaging appearance is often nonspecific 2. Therefore, capillary hemangioma should be included in the differential diagnosis of any enhancing intradural extramedullary mass.
Several pathogenic mechanisms have been proposed for capillary hemangiomas of the CNS: (a) Impaired movement and differentiation of primitive mesoderm from the embryonic mesodermal plate during the early somitic differentiation (days 21–24 of embryogenesis); (b) Vascular tumors of the conus‐cauda region have been defined as hamartomas, implying their congenital origin; (c) Abnormal development of vascular structures within the epineurium of the nerve roots may be affected 4.
Histological and immunohistochemical features of CNS capillary hemangiomas have been reported to be similar to those arising in the skin. The CNS lesions showed a lobular architecture with fibrous tissue septa and highly cellular areas in six cases, whereas a blood‐filled cavernous space and fibroendothelial papillae mimicking papillary endothelial hyperplasia were seen in four cases. Immunohistochemistry demonstrated expression of vascular endothelial growth factor and glucocorticoid receptor 1. Our case showed the typical histologic features of a capillary hemangioma and the immunophenotype was characteristic for a vascular‐derived tumor.
The Ki‐67 proliferative index of CNS capillary hemangiomas has been reported to range from 2.2 to 12% (mean 5.6%) 1 while the recently reported case of recurrent capillary hemangioma had a proliferative index of 10%. Although the prognostic significance of the high proliferative index of 34% in our case is unclear, this finding indicates that close follow‐up of the patient may be warranted.
References
- 1. Abe M, Misago N, Tanaka S, Masuoka J, Tabuchi K (2005) Capillary hemangioma of the central nervous system: a comparative study with lobular capillary hemangioma of the skin. Acta Neuropathol 109:151–158. [DOI] [PubMed] [Google Scholar]
- 2. Alakandy LM, Hercules S, Balamurali G, Reid H, Herwadkar A, Holland JP (2006) Thoracic intradural extramedullary capillary haemangioma. Br J Neurosurg 20:235–238. [DOI] [PubMed] [Google Scholar]
- 3. Kasukurthi R, Ray WZ, Blackburn SL, Lusis EA, Santiago P (2009) Intramedullary capillary hemangioma of the thoracic spine: case report and review of the literature. Rare Tumors 1:e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nowak DA, Widenka DC (2001) Spinal intradural capillary haemangioma: a review. Eur Spine J 10:464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]


