Clinical History
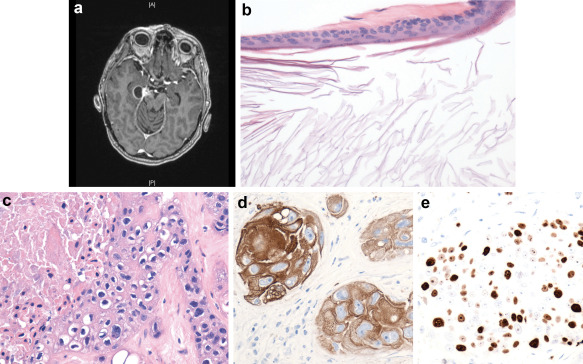
This 65‐year‐old female who was diagnosed with a right CP angle tumor after an MRI was done to investigate facial pain in 1999. In 2006, her pain became quite severe and she developed numbness in all three divisions of the trigeminal nerve along with decreased corneal reflex and facial paresis on the right side. The lesion was partially resected at the time by right retrolabyrinthine approach with presigmoid and postsigmoid craniectomy. The patient recovered uneventfully except for wound infection, which required debridement. In 2012, she presented with left sided weakness and gait instability. MRI with gadolinium showed a recurrent hypointense lesion with rim enhancement as well as an enhancing nodule at the tentorial incisura on the right side (Figure 1a). A subtemporal approach was undertaken with subtotal resection of tumor that encircled the right posterior cerebral artery. Postoperatively, she received stereotactic radiosurgery with Cyberknife for a total of 2500 cGy. In spite of this, her lesion progressed. She continued to worsen neurologically and an Ommaya reservoir was inserted for aspiration of the cystic portion of the lesion. She has since begun a radiation boost to the area of 54 Gy in thirty fractions.
Figure 1.
Pathology
The specimen from the surgery in 2006 consisted of multiple gray‐white feathery portions of tissue measuring 0.1–1.0 cm in diameter. Microscopic examination revealed fragments of thin layers of connective tissue capsule lined by squamous epithelium, and filled with keratin flakes (Figure 1b). The specimen from the second surgery in 2012 consisted of multiple fragments of firm tan‐white tissue measuring 2.0 × 1.5 × 0.3 cm. Microscopic examination revealed highly anaplastic keratin positive squamous epithelium infiltrating underlying connective tissue and brain (Figure 1c,d). The epithelium showed a marked degree of nuclear hyperchromasia and atypia with a very high proliferation rate, which was confirmed by MIB‐1 (Figure 1e). Immunostaining for melanin and p53 was negative. What is your diagnosis?
Diagnosis
Epidermoid cyst with malignant transformation to squamous cell carcinoma.
Discussion
Intracranial epidermoid cysts are benign, congenital inclusion tumors which account for 0.2%–1.8% of all intracranial lesions. They commonly occur in the cerebellopontine angle, although the petrous apex and suprasellar region are also favored sites. They tend to be slow growing masses and presentation is dependent on the site of the lesion. Malignant transformation to a squamous cell carcinoma is an exceptionally rare event and should be thought of in the face of rapid progression of a patient's symptomatology 3.
Epidermoid cysts are best investigated with MRI where they appear hypo or isointense on T1, hyperintense on T2 and show minimal or no enhancement with gadolinium 4. They tend to be well demarcated and show an absence of edema 3. A dermoid cyst should also be included in the differential diagnosis while schwannoma or meningioma is far less likely as both tend to enhance brightly with gadolinium. Enhancement after gadolinium administration, rapid growth with an irregular margin along with rapid progression of the patient's signs and symptoms should alert the clinician to a possible malignant transformation 3, 4.
On gross histology, epidermoid cysts have a pearly white appearance. Histopathologically, an epidermoid cyst is comprised of benign keratinizing stratified squamous epithelium lining with a low proliferative index and desquamated cellular debris (8). In contrast, a squamous cell carcinoma (SCC) tends to have a grayish appearance with thickened walls, a solid component and unclear margins due to tumor infiltration of surrounding structures 1. On microscopic examination, dysplastic squamous epithelium with enlarged pleomorphic nuclei and a high proliferative index will be seen.
Malignant transformation of a benign epidermoid cyst was first described in 1912. This is a rare but well described event in the literature with our case being the 48th one.
In 1981, Garcia et al recommended definite criteria for the definition of a primary intracranial squamous cell carcinoma: (a) the tumor has to be restricted to the intracranial, intradural compartment without invasion or extension beyond the dura or cranial bones, and (b) there must be no extension or invasion through intracranial orifices, nor communication or connection with the middle ear, air sinuses or sella turcica and no evidence of nasopharyngeal tumor. These criteria exclude all possibilities of tumors arising outside the dura with secondary invasion of the brain 1.
In 2003, Hamlat et al classified these carcinomas into five groups 2:
-
(1)
Initial malignant transformation of an epidermoid cyst
-
(2)
Malignant transformation from a remnant epidermoid cyst
-
(3)
Malignant transformation with leptomeningeal carcinomatosis
-
(4)
Squamous cell carcinoma arising from other benign cysts
-
(5)
Other malignancies arising from benign cyst
Our case qualifies as type 2 according to Hamlat's classification.
In conclusion, we report a case of a primary intracranial squamous cell carcinoma due to malignant transformation of a previously partially resected CP angle epidermoid cyst. This is the 48th reported case in the literature. Mainstay of treatment is surgical resection followed by radiation. Despite this treatment, prognosis remains poor.
References
- 1. Garcia C, McGarry P, Rodriguez F (1981) Primary intracranial squamous cell carcinoma of the right cerebellopontine angle. J Neurosurg 54:824–828. [DOI] [PubMed] [Google Scholar]
- 2. Hamlat A, Hua ZF, Saikali S, Egreteau J, Guegan Y (2003) Malignant transformation of intracranial epidermoid cyst with leptomeningeal carcinomatosis: case report. Acta Neurol Belg 103:221–224. Dec [PubMed] [Google Scholar]
- 3. Lakhdar F, Hakkou EM, Gana R et al (2011) Malignant transformation six months after removal of intracranial epidermoid cyst: a case report. Case Rep Neurol Med 2011:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Murase S, Yamakawa H, Ohkuma A et al (1999) Primary intracranial squamous cell carcinoma. Neurol Med Chir (Tokyo) 39:49–54. [DOI] [PubMed] [Google Scholar]


