Clinical History
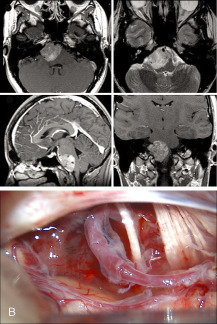
A 26‐year‐old female initially noted blurry vision when looking towards the right. Three months later, she noted diplopia when looking towards the right side. Right abducens nerve palsy was documented by her ophthalmologist. Initial brain MRI performed four months after the onset of blurry vision showed a 4 mm(AP)X3 mm(transverse)X5 mm (craniocaudal) area of enhancement anterior to the pons on the right side. Neurology coordinated an extensive serum screening for inflammatory, infectious, and metabolic causes, all of which came back negative. Two to three months later, she started experiencing daily pressure headaches felt mostly in the occipital and suboccipital regions. The follow‐up brain MRI showed the presence of a prepontine/premedullary mass, measuring 23 mm(AP)X34 mm(transverse)X29 mm (craniocaudal)(Figure 1a). This mass was mostly solid but presented some cystic necrotic areas. The lesion, believed to be extra‐axial, exerted mass effect on the pons and medulla without causing abnormal signal within the brainstem. The mass also caused asymmetry of the fourth ventricle without evidence of obstructive hydrocephalus. At the time of consultation with neurosurgery, approximately 7 months after the onset of her blurry vision, the patient reported difficulty swallowing solids for the last two weeks. Other than abducens nerve palsy, the rest of her physical exam was unremarkable. After review of the images with neuroradiology, the suspected diagnosis was a malignant nerve sheath tumor, most probably arising from the abducens cranial nerve. The patient underwent a resection of the prepontine and premedullary mass. The cerebellopontine angle was inspected under microscopic visualization. A reddish purple tumor could be seen between the trigeminal nerve and the 7th and 8th cranial nerve complex as well as between this complex and the region of the lower cranial nerves (Figure 1b). Intra‐operative frozen section analysis indicated a highly vascular and malignant appearing neoplasm. Because of its rapid growth rate, maximal safe debulking of the soft tumor was performed, realizing satisfactory decompression. All cranial nerves from trochlear to hypoglossal were seen during surgery, except the abducens nerve. A small amount of residual tumor was left, adherent to the 7th and 8th cranial nerve complex and the ventrolateral surface of the pons.
Figure 1.
Microscopic Pathology
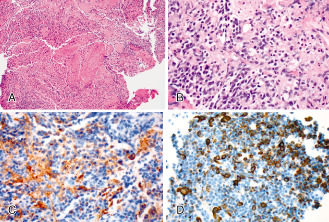
Standard hematoxylin and eosin studies showed a neoplasm of high cellularity with marked nuclear atypia, hyperchromasia, and high nuclear/cytoplasmic ratio (Figure 2a). A focus of spindled muscle fibers was also present within the neoplasm (Figure 2b). Immunohistochemistry using antibodies to synaptophysin showed patchy immunoreactivity in tumor cells (Figure 2c). Desmin immunoreactivity was evident in many areas (Figure 2d). MIB‐1 immunohistochemistry showed an elevated labeling index estimated to approximately 30%‐40% of positive tumor nuclei. Fluorescence in situ hybridization (FISH) studies using the probes to MYC‐N (Chromosome 2—centromere 2/2p24.1), MYC‐C (break apart—8q24), and EWSR1 (break apart—22q12) showed no aberrations in the tumor nuclei (300 tumor nuclei/probe). What is your diagnosis?
Figure 2.
Diagnosis
MEDULLOMYOBLASTOMA. Final pathology came back suggestive of a medullomyoblastoma. Given the rapid growth of the lesion and the regions of enhancement on the spinal MRI compatible with drop metastasis, craniospinal radiation was initiated 4 weeks after surgery, with boost radiation delivered at the surgical focus and at the level of the spinal enhancing foci. After intense neurorehabilitation, the patient was discharged home six weeks after surgery.
Discussion
Presentation with an isolated abducens nerve paresis progressing to complete palsy in the absence of other cranial nerve dysfunction or increased intracranial pressure should trigger a complete work‐up, including infectious, inflammatory/degenerative, and tumoral etiologies. Demonstration of an area of enhancement at the pontomedullary junction in a patient with an isolated abducens nerve paresis should evoke a tumor arising from the abducens nerve 2, 5. The rapid radiological progression documented on follow‐up raised the possibility of an aggressive nerve sheath tumor. In the present case, the intra‐operative frozen analysis was critical suggestive of an aggressive intraaxial lesion with an exophytic component. Final pathology assessment was suggestive of a medullomyoblastoma 3.
Cerebellar medulloblastomas are very rare lesions. Although they are more commonly encountered in the pediatric population as midline intraaxial posterior fossa lesions, in adults they are most often laterally located 4. The typical clinical manifestations of cerebellar medulloblastomas are headaches secondary to raised intracranial pressure as well as cranial nerves and cerebellar symptomatology 4, 6. The MRI appearance of cerebellar medulloblastomas and medullomyoblastomas is variable and non‐specific 1, 3. Their origin is thought to be from the lateral surface of the cerebellum with possible exophytic components extending in the cerebellopontine angle, or even with a primary extra‐axial location 1.
To the author's knowledge, this is the second reported case of medullomyoblastoma of the prepontine and premedullary cisterns and/or cerebellopontine angle, and the first report of a well‐documented paramedian site of origin 6. The histogenesis of the myogenic component of medullomyoblastomas remains not well understood. The muscle fibers in medullomyoblastoma are thought to arise either through the induction of pluripotential ectomesenchymal cells within or near the tumor, such as within the leptomeninges, or directly from primitive neuroepithelial cells themselves 8. The clinical behavior and prognosis of the myogenic component of medullomyoblastoma remains uncertain given the small number of reported cases 7. Although it has been suggested that the presence of foci of large cell and anaplastic changes, similar to classic medulloblastomas or de‐novo LC/A subtypes, confers a more aggressive clinical course to medullomyoblastomas, the significance of these findings in medullomyoblastomas is still under investigation 3.
In summary, this case describes a unique case of medullomyoblastoma that presented with an isolated abducens cranial nerve palsy. Early imaging documented a paramedian site of tumor origin, which later progressed to occupy the prepontine/premedullary cisterns. Its initial clinicoradiological features mislead us to suspect an abducens cranial nerve schwannoma with potential malignant features given its rapid growth and possible spinal associated lesions. Histopathological assessment was critical, documenting a rare medullomyoblastoma. Detailed documentation of such cases is important as their clinical significance is still under study.
References
- 1. Bonneville F, Savatovsky J, Chiras J (2007) Imaging of cerebellopontine angle lesions: an update. Part 2: intra‐axial lesions, skull base lesions that may invade the CPA region, and non‐enhancing extra‐axial lesions. Eur Radiol 17:2908–2920. [DOI] [PubMed] [Google Scholar]
- 2. Erlich SA, Tymianski M, Kiehl TR (2009) Cellular schwannoma of the abducens nerve: case report and review of the literature. Clin Neurol Neurosurg 111:467–471. [DOI] [PubMed] [Google Scholar]
- 3. Helton KJ, Fouladi M, Boop FA, Perry A, Dalton J, Kun L, Fuller C (2004) Medullomyoblastoma: a radiographic and clinicopathologic analysis of six cases and review of the literature. Cancer 101:1445–1546. [DOI] [PubMed] [Google Scholar]
- 4. Menon G, Krishnakumar K, Nair S (2008) Adult medulloblastoma: clinical profile and treatment results of 18 patients. J Clin Neurosci 15:122–126. [DOI] [PubMed] [Google Scholar]
- 5. Park JH, Cho YH, Kim JH, Lee JK, Kim CJ (2009) Abducens nerve schwannoma: case report and review of the literature. Neurosurg Rev 32:375–378. [DOI] [PubMed] [Google Scholar]
- 6. Park SY, Kim JH, Kim KT, Kim YJ, Kim TH, Hwang K, Sung KJ, Park KH (2004) A case of medullomyoblastoma of cerebellopontine angle mimicking acoustic neuroma. Yonsei Med J 45:719–722. [DOI] [PubMed] [Google Scholar]
- 7. Rao C, Friedlander ME, Klein E, Anzil AP, Sher JH (1990) Medullomyoblastoma in an adult. Cancer 65:157–163. [DOI] [PubMed] [Google Scholar]
- 8. Smith TW, Davidson RI (1984) Medullomyoblastoma. A histologic, immunohistochemical, and ultrastructural study. Cancer 54:323–332. [DOI] [PubMed] [Google Scholar]


