Abstract
Ethnic differences in the profiles of hypertension and cardiovascular risk have been reported between Asians and Westerners. However, blood pressure (BP) profiles and the risk factors for cardiovascular disease might differ even among different Asian populations because of the diversity of cultures, foods, and environments. We retrospectively examined differences in 24‐h BP profiles between 1051 Japanese (mean age, 62.5 ± 12.4 years; medicated hypertension, 75.7%) and 804 Thai (mean age, 56.9 ± 18.5 years; medicated hypertension, 65.6%) by using the Japanese and Thai ambulatory BP monitoring (ABPM) databases, in order to check the BP control status in treated hypertensives and to inform the clinical diagnosis of hypertension. The two populations had similar office systolic BP (SBP) (142.7 ± 20.0 vs 142.3 ± 20.6 mm Hg, p = .679). However, the Japanese population had higher 24‐hr average and daytime SBP, and the Thai population had higher nighttime SBP even after adjusting for cardiovascular risk factors (all p < .05). Greater morning BP surge was observed in Japanese (31.2 vs 22.8 mm Hg, p < .001). Regarding nocturnal BP dipping status, the prevalence of riser status (higher nighttime than daytime SBP) was higher in the Thai population (30.5% vs 10.9%). These findings suggest that a substantial difference in 24‐hr BP profiles exists between even neighboring countries in Asia.
Keywords: ambulatory blood pressure, Asian population, hypertension, racial difference
1. INTRODUCTION
Hypertension is an important global health issue. It has been well established that elevated blood pressure (BP) is associated with cardiovascular disease. 1 Asian populations are at greater cardiovascular disease risk related to hypertension compared with Western populations. 2 Previous studies have demonstrated the existence of ethnic differences in BP profiles. For example, one study reported that diurnal BP variability detected by an ambulatory BP monitoring (ABPM) device was greater in Japanese compared with black and white patients. 3 Another reported that morning BP surge was higher in Japanese than European patients. 4 In addition to these ethnic differences, BP profiles might differ even among populations of the same ethnicity, if they have different lifestyles, foods, cultures, and environments.
We recently conducted the AsiaBP@Home study, which analyzed data collected using the same home BP monitoring device in 1443 medicated hypertensive patients from 15 Asian specialist centers in 11 countries/regions. The AsiaBP@Home study demonstrated that home BP is relatively well controlled at hypertension specialist centers in Asia, but almost half of patients remain uncontrolled for morning BP according to a strict BP threshold (systolic/diastolic BP: 130/80 mm Hg), with significant country/regional differences. 5 , 6 The country/regional differences in the profile of hypertension and its risk factors should be carefully considered in clinical practice. However, specific differences in the 24‐h BP profiles between countries in different regions of Asia remain incompletely investigated.
The aim of this study was to determine the difference in BP profiles measured by ABPM between Japan and Thailand, which are located in East Asia and Southeast Asia, respectively.
2. METHODS
2.1. Study design and data collection
The present study is a retrospective analysis comparing the data of the Japanese and Thai ABPM, which were conducted to check the BP control status in treated hypertensives and to gain information that could inform the clinical diagnosis of hypertension. The Japanese database includes 1051 subjects who underwent ABPM between 2005 and 2015 at Jichi Medical University Hospital (located in East Japan), and the Thai database consists of 804 subjects who underwent ABPM between 2015 and 2018 at Mahidol University, Siriraj Hospital (located in Central Thailand). The protocol was approved by the Institutional Review Board of Jichi Medical School, Tochigi, Japan. Data on age, sex, comorbidity, and current medications were collected from medical records.
2.2. Blood pressure measurements
Ambulatory blood pressure was measured using a validated device (Japanese data: TM‐2425/2431 [A&D, Saitama, Japan], Thai data: Welch Allyn ABPM 6100 [Welch Allyn Co]) 7 programmed to take readings every 30 minutes for at least 24 h. 8 Subjects were asked to record their sleep and wake times in a diary. Nighttime readings were defined as those taken from the time of falling asleep to the time of waking; all other readings were defined as daytime values.
Morning BP was defined as the average of the ambulatory BP values over the two hours after waking (based on the patients’ diaries). Daytime BP and nighttime BP were also calculated based on the patients’ diaries and defined as the average of BP measurements during the daytime (from awakening to going to bed) and nighttime (from going to bed to awakening), respectively. The lowest nighttime systolic BP (SBP) was defined as the lowest 1‐hour moving average of consecutive nighttime SBP values. Morning BP surge was calculated as the average morning SBP minus the moving lowest nighttime SBP. Exaggerated morning BP surge was defined as a degree of morning BP surge ≥ 55 mm Hg. 9
Patients were classified into four groups based on the nocturnal fall in SBP ([1 minus average nighttime SBP/average daytime SBP] multiplied by 100) at baseline: Extreme dippers (20% or more); Dippers (10% to below 20%); Non‐dippers (0% to below 10%); and Risers (any increase). 8
Office BP was defined as the average of two consecutive BP readings measured at the hospital on the day of starting 24‐hour ABPM measurement.
The classification of nocturnal dipping status is defined by SBP, and the association between BP and the cardiovascular disease risk in older adults is mostly discussed by SBP; therefore, we have mainly focused on SBP in the present analysis.
2.3. Statistical analyses
Results are expressed as numbers, percentages, mean ± SD, or adjusted mean ± SE. An unpaired t test and Fisher's exact test were used to assess the differences of mean values and prevalence rates between the Japanese and Thai group. A multivariable regression model was used to compare between‐group differences of blood pressure parameters after adjusting for age, sex, body mass index (BMI), and the prevalence of current smoking, medicated hypertension, diabetes mellitus, hyperlipidemia, previous coronary artery disease, and previous stroke.
In a sensitivity analysis, we performed similar analysis in the propensity score‐matched population to accounts for the effects of between‐group differences. We computed the propensity score by using a logistic regression model adjusted for age, sex, BMI, and the prevalence of current smoking, medicated hypertension, diabetes mellitus, hyperlipidemia, previous coronary artery disease, and previous stroke. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute, Cary, NC).
3. RESULTS
3.1. Characteristics of the study subjects
The characteristics of the Japanese and Thai study subjects are shown in Table 1. Compared with the Thai group, the Japanese group was significantly older and had a higher prevalence of male subjects and higher rates of smoking, past history of coronary artery disease, and medicated hypertension. The Thai subjects had a significantly higher BMI and higher rates of dyslipidemia and past history of stroke. The use of antihypertensive medication was also different between countries.
Table 1.
Characteristics of study subjects
|
Japanese Group (N = 1051) |
Thai Group (N = 804) |
p value | |
|---|---|---|---|
| Age, years | 62.5 ± 12.4 | 56.9 ± 18.5 | <.001 |
| Body mass index, kg/m2 | 24.5 ± 3.7 | 25.4 ± 4.7 | <.001 |
| Male, % | 52.1 | 37.1 | <.001 |
| Current smoking, % | 11.4 | 1.7 | <.001 |
| Diabetes mellitus, % | 22.4 | 20.3 | .304 |
| Hyperlipidemia, % | 39.9 | 61.6 | <.001 |
| Past history of CAD, % | 10.8 | 7.0 | .006 |
| Past history of stroke, % | 2.4 | 5.4 | .001 |
| Medicated hypertension, % | 75.7 | 65.6 | <.001 |
| Number of drugs for hypertension | 2.0 ± 1.0 | 2.5 ± 1.3 | <.001 |
| ACE inhibitor, % | 9.2 | 17.1 | <.001 |
| Alpha blocker, % | 7.4 | 26.2 | <.001 |
| ARB, % | 60.1 | 46.9 | <.001 |
| Beta blocker, % | 24.3 | 45.2 | <.001 |
| CCB, % | 67.2 | 67.7 | .878 |
| Diuretics, % | 34.1 | 17.3 | <.001 |
| Others, % | 0.9 | 11.8 | <.001 |
| Office blood pressure monitoring | |||
| SBP, mm Hg | 142.7 ± 20.0 | 142.3 ± 20.6 | .679 |
| DBP, mm Hg | 81.3 ± 13.3 | 76.0 ± 13.5 | <.001 |
| HR, bpm | 72.8 ± 12.9 | 76.0 ± 13.3 | <.001 |
| Ambulatory blood pressure monitoring | |||
| 24‐h SBP, mm Hg | 133.4 ± 14.8 | 131.7 ± 16.5 | .023 |
| 24‐h DBP, mm Hg | 78.6 ± 10.0 | 73.5 ± 11.8 | <.001 |
| 24‐h HR, bpm | 68.3 ± 9.1 | 70.8 ± 10.3 | <.001 |
| Daytime SBP, mm Hg | 137.9 ± 15.3 | 133.3 ± 16.4 | <.001 |
| Daytime DBP, mm Hg | 81.4 ± 10.5 | 75.2 ± 12.4 | <.001 |
| Daytime HR, bpm | 71.6 ± 9.6 | 74.1 ± 11.5 | <.001 |
| Nighttime SBP, mm Hg | 123.4 ± 16.7 | 127.8 ± 20.1 | <.001 |
| Nighttime DBP, mm Hg | 72.2 ± 10.4 | 70.2 ± 12.3 | <.001 |
| Nighttime HR, bpm | 60.8 ± 9.0 | 63.0 ± 9.3 | <.001 |
| Morning SBP, mm Hg | 139.8 ± 18.5 | 137.6 ± 20.7 | .019 |
| Morning DBP, mm Hg | 83.2 ± 12.1 | 79.0 ± 13.9 | <.001 |
| Morning HR, bpm | 68.8 ± 11.4 | 74.4 ± 12.6 | <.001 |
Data are presented as mean ± standard deviation or percentage.
Abbreviations: ACE, Angiotensin‐converting enzyme; ARB, Angiotensin‐receptor blocker; CCB, Calcium‐channel blocker; CAD, coronary artery disease (including angina and myocardial infarction); SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate.
3.2. Blood pressure parameters and heart rate
There was no significant difference in office SBP between the Japanese and Thai groups (142.7 ± 20.0 mm Hg vs 142.3 ± 20.6 mm Hg, p = .679), whereas significant differences were observed in the ambulatory SBP parameters. The averages of 24‐h, daytime, and morning SBP values were significantly higher in the Japanese group than in the Thai group (24‐hr: 133.4 ± 14.8 mm Hg vs 131.7 ± 16.5 mm Hg; daytime: 137.9 ± 15.3 mm Hg vs 133.3 ± 16.4 mm Hg; morning: 139.8 ± 18.5 mm Hg vs 137.6 ± 20.7 mm Hg; all p < .05). However, nighttime SBP was significantly higher in the Thai group (Japanese: 123.4 ± 16.7 mm Hg; Thai: 127.8 ± 20.1 mm Hg; p < .001) (Table 1). These between‐group differences in 24‐h, daytime, and nighttime SBP remained significant even after adjusting for age, sex, BMI, and the prevalence of current smoking, medicated hypertension, diabetes mellitus, hyperlipidemia, previous coronary artery disease, and previous stroke (Figure 1).
Figure 1.
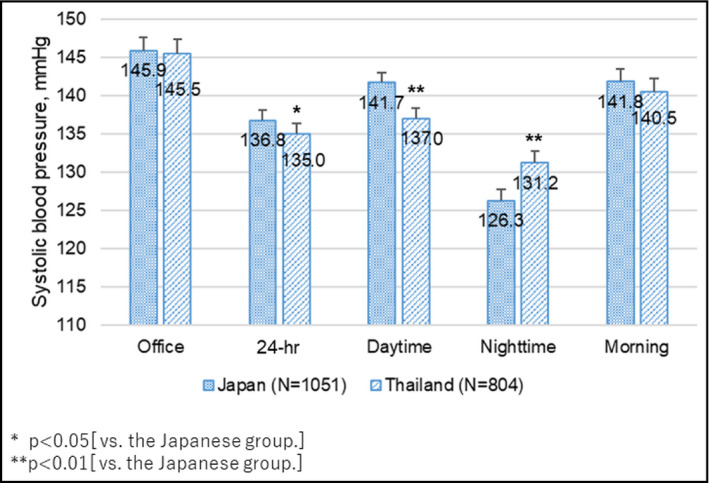
Systolic blood pressure parameters in the Japanese and Thai groups. Mean values (inside the bar) and standard error (expressed as error bar), adjusted for age, sex, body mass index, current smoking, medicated hypertension, diabetes mellitus, hyperlipidemia, past history of coronary artery disease, and past history of stroke. *p < .05( vs the Japanese group). **p < .01 ( vs the Japanese group)
Office and ambulatory diastolic BP (DBP) parameters were significantly higher in the Japanese group than in the Thai group (all p < .001). Office and ambulatory heart rate (HR) parameters were significantly higher in the Thai group than in the Japanese group (all p < .001).
3.3. Diurnal blood pressure variability
Table 2 shows the diurnal BP variability evaluated by ABPM. Morning BP surge (average morning SBP minus moving lowest nighttime SBP) was significantly higher in the Japanese than in the Thai group (31.4 ± 15.9 mm Hg vs. 22.4 ± 16.9 mm Hg, P < .001). Even after adjusting for the related cardiovascular risk factors, this between‐group difference in morning BP surge remained significant (data not shown). The prevalence of exaggerated morning BP surge (morning BP surge ≥ 55 mm Hg) was also higher in the Japanese group (6.7% vs. 2.9%, P < .001).
Table 2.
Diurnal blood pressure variability
|
Japanese Group (N = 1051) |
Thai Group (N = 804) |
p value |
Estimated OR (95%CI) |
p for OR | |
|---|---|---|---|---|---|
| Morning BP surge | |||||
| Morning BP surge, mm Hg | 31.4 + 15.9 | 22.4 ± 16.9 | <.001 | ‐ | ‐ |
| Exaggerated morning BP surge, % | 6.7 | 2.9 | <.001 | 0.50 (0.30 ‐ 0.84) | .009 a |
| Nocturnal BP dipping | |||||
| 4 Nocturnal dipping patterns, % | <.001 | ||||
| Extreme dipper | 12.3 | 2.0 | 0.19 (0.10 ‐ 0.37) | <.001 b | |
| Dipper | 41.0 | 24.2 | ‐ | ‐ | |
| Non‐dipper | 35.9 | 43.3 | 3.06 (2.32 ‐ 4.05) | <.001 b | |
| Riser | 10.9 | 30.5 | 7.59 (5.24 ‐ 11.0) | <.001 b | |
| Non‐dipper/Riser, % | 46.7 | 73.9 | <0.001 | 4.41 (3.38 ‐ 5.75) | <.001 c |
Data are presented as mean ± SD, or a percentage. “Exaggerated morning surge” was defined as percentage of unadjusted morning surge ≥ 55 mm Hg.
Abbreviations: BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; OR, odds ratio; SBP, systolic blood pressure.
Estimated odds ratios and their 95% confidence intervals for exaggerated morning surge in Thai vs. Japanese data based on multivariable logistic regression model adjusted for age, sex, BMI, current smoking, medicated hypertension, diabetes mellitus, hyperlipidemia, past history of CAD, and past history of stroke (model A).
Estimated odds ratios and their 95% confidence intervals for each nocturnal dipping pattern (reference: Dipper) in Thai vs. Japanese data based on multinomial logistic regression model B adjusted for the covariates in model A and nighttime SBP average.
Estimated odds ratios and their 95% confidence intervals for the Non‐dipper/Riser pattern in Thai vs. Japanese data based on multivariable logistic regression model B.
Regarding the nocturnal BP fall, the prevalence of the 4 nocturnal dipping patterns was remarkably different between countries (p < .001). The prevalence of subjects with extreme‐dipper status was higher in the Japanese group (Japanese [J]:12.3% vs. Thai [T]: 2.0%), while the prevalence of non‐dippers (J: 35.9% vs. T: 43.3%) and that of risers (J: 10.9% vs. T:30.5%) was higher in the Thai group. The prevalence of the less nocturnal dipping patterns (ie, the Non‐dippers and the Risers) was higher in the Thai group (73.9% vs 46.7%, p < .001; odds ratio: 4.41).
3.4. Propensity score matching
Table S1 shows the results of the propensity score‐matched analysis. Nighttime SBP was significantly higher in the Thai group (Japanese: 123.7 ± 17.0 mm Hg; Thai: 128.7 ± 20.4 mm Hg; p < .001), even though the other ambulatory SBP parameters were higher in the Japanese group. Similar to the results of the whole population analysis, the morning BP surge was significantly greater in the Japanese group (30.7 ± 16.0 mm Hg vs. 22.1 ± 17.3 mm Hg, p < .001). The prevalence of non‐dipper and riser was higher in the matched‐Thai group (Table S1).
4. DISCUSSION
This retrospective comparison of the ABPM data for 1051 Japanese and 804 Thai individuals revealed that significant differences in 24‐h BP profiles may exist even between neighboring countries in Asia. Among the patients controlled to a similar office BP level, nighttime BP was high and less nocturnal BP fall was observed in the Thai population. The Japanese population showed higher 24‐hr and daytime BP and greater morning BP surge compared with the Thai population. A previous report showed that there are differences in the prevalence of cardiovascular disease among Asian countries. The East Asian population, including Japanese, had higher prevalence of stroke mortality than coronary artery disease, whereas the Southeast Asian population, including Thai, had higher prevalence of coronary artery disease mortality than stroke. 10 The differences in ambulatory BP parameters between the Japanese and Thai populations found in our study may have partly contributed to the differences in cardiovascular mortality.
4.1. Blood pressure values
As shown in Figure 1, the nighttime SBP was significantly higher in the Thai group, and the average SBP over 24‐hour and especially daytime SBP were significantly higher in the Japanese group, even after adjusting for the cardiovascular risk factors including all the demographic differences shown between the study populations. In this study, the office SBP levels, which are a basic guide to diagnosing hypertension or evaluating BP control, were similar between the Japanese and Thai subjects.
A recently published Japanese ABPM study found that increased nighttime SBP was significantly associated with the risk of atherosclerotic cardiovascular disease and heart failure, while increased daytime SBP was associated with the risk of atherosclerotic cardiovascular disease, but not heart failure, independent of office SBP. Therefore, the increase in out‐of‐office BP over a different time window which was observed in our present study might have contributed to the different types of cardiovascular disease risk. 11
4.2. 24‐h circadian BP profile
Excessive morning BP surge and nighttime BP increase with abnormal nocturnal BP falls are well known to be cardiovascular risks. 9 , 11 , 12 , 13 , 14 , 15 Previous reports have concluded that Asian populations are more likely to have abnormal patterns of BP variability, such as nocturnal hypertension and excessive morning BP surge, than Western populations. 3 , 4 Our present findings expand this information by adding evidence that the prevalence of disrupted circadian rhythm (ie, exaggerated morning BP surge, and extreme dipper, non‐dipper, and riser patterns) was different between the Japanese and Thai populations, despite the relative proximity of Japan and Thailand.
4.2.1. Nocturnal BP fall
In the present study, the Thai population had significantly higher nighttime BP and a higher prevalence of non‐dipper/riser pattern compared with the Japanese population, whereas the Japanese population showed a higher prevalence of extreme dipping. Even in the comparison between the propensity score‐matched populations, the same nocturnal dipping tendency was found. The risk of abnormal nocturnal BP falls has been studied by many investigators, but the results are inconsistent. Previous studies reported that extreme dipping was associated with stroke, 11 , 16 but a meta‐analysis showed that the risk of extreme‐dipper status for cardiovascular events disappeared with antihypertensive treatment. 13 On the other hand, riser and non‐dipper patterns have been consistently reported to pose a cardiovascular risk. 15 , 16 A Swedish study and a recent Japanese study demonstrated that a riser pattern was a significant predictor of heart failure. 11 , 17 It is therefore important to restore the impaired nocturnal circadian rhythm in order to prevent the development of cardiovascular events and heart failure.
Increased nighttime BP and decreased nocturnal BP fall coexist and are considered to be related to increased circulation volume, salt intake, and salt sensitivity. 18 , 19 , 20 Salt intake in Japanese was reported to be 10.4 g/person/d and that in Thai was reported to be 10.8 g/person/d. 21 Thus, the difference in salt intake between the two countries was not very large. In addition, the Thai subjects had higher HR throughout 24‐hour both in an office and an out‐of‐office setting. In a tropical climate, sweating may cause a decrease in circulating volume and, as a compensatory mechanism, an increase in sympathetic nerve activation, which may result in a higher heart rate, nighttime BP increase and a nocturnal BP non‐dipper/riser pattern. In addition, lower rates of diuretic use in Thailand (shown in Table 1) might contribute to these differences.
4.2.2. Morning BP surge
In the present study, the Japanese subjects had remarkably greater morning BP surge (9 mm Hg greater) than the Thai subjects and also a high prevalence of exaggerated morning BP surge. Excessive morning BP surge has been reported to be a predictor of stroke events. 9 , 15 In addition, a previous study comparing Japanese and European hypertensive patients concluded the existence of ethnic difference in the degree of morning BP surge between Asians and Westerners. 4 Our results suggest that there may exist differences in morning BP profile between countries/regions even among Asians.
Aging and increased arterial stiffness are known to be associated with morning BP increase and morning BP surge. 20 One possible explanation of the higher morning BP surge in Japanese is that the Japanese subjects in this study were older and thus their arterial stiffness might have been increased. However, the between‐group difference in morning BP surge remained significant even after adjusting for cardiovascular risk factors including age. Additional propensity score‐matched analysis indicated that the greater morning BP surge found in the Japanese group is a Japanese specific feature independent from aging.
Another possibility could be an environmental factor. Morning BP surge is reportedly augmented over the winter (cold temperature). 22 In the area where the Japanese study subjects live in Japan, the minimum temperature falls below 0ºC in the winter and there is a large diurnal temperature difference (more than 10ºC) in the spring and fall. The difference in morning BP profile between the Japanese and Thai populations might be partly due to this difference in temperature.
4.2.3. Management of BP circadian rhythm
Taken together, these results show that patients with similar office BP level may have different patterns of disrupted BP circadian rhythm, and these differences, in turn, may arise from differences in their ethnicities, lifestyles and environments. If individuals having specific ethnicities, lifestyles, and environments are prone to certain disruptions in BP circadian patterns, then any hypertension treatment should take these features into consideration. To detect and assess the disrupted circadian rhythms, out‐of‐office BP measurement by ABPM is essential.
5. LIMITATIONS
There are several possible limitations to our study. Our retrospective study was conducted by comparing two datasets of subjects’ characteristics and ABPM parameters measured in clinical practice. Different types of ABPM devices were used in each population, and this may have made a contribution to the differences in ABPM parameters. However, all devices used in this study had been previously validated according to international protocols and found to be accurate. In addition, we are unable to determine the cause of the difference in BP profile between the Japanese and Thai populations because the databases used included no data on vascular stiffness and sodium intake. Further studies will be needed to confirm the country‐specific or region‐specific features in BP profile.
6. CONCLUSIONS
There were significant differences in the 24‐h BP profiles between Japanese and Thai populations even when they had similar levels of office BP. Our results indicate that differences in environment and lifestyle might contribute to specific differences in the profile of hypertension and its risks even between neighboring countries. Measurement of out‐of‐office BP using ABPM is useful to assess country‐specific or region‐specific features and could lead to an individualized 24‐h BP control management.
CONFLICT OF INTEREST
K. Kario has received research grants from Omron Healthcare, A&D, and Fukuda Denshi. N. Tomitani was the recipient of a grant from the Kanae Foundation for the Promotion of Medical Science.
AUTHOR CONTRIBUTIONS
N. Tomitani analyzed the data and wrote the Introduction, Methods, Results, and Discussion sections. S. Hoshide and N. Tomitani collected the Japanese data. S. Wanthong collected the Thai data. W. Roubsanthisuk, P. Buranakitjaroen, S. Hoshide, and K. Kario reviewed/edited the manuscript.K. Kario supervised the conduct of the study and data analysis.
Supporting information
Table S1
Tomitani N, Wanthong S, Roubsanthisuk W, Buranakitjaroen P, Hoshide S, Kario K. Differences in ambulatory blood pressure profiles between Japanese and Thai patients with hypertension /suspected hypertension. J Clin Hypertens. 2021;23:614–620. 10.1111/jch.14107
Funding informationThis study was financially supported by a grant from the Kanae Foundation for the Promotion of Medical Science.
REFERENCES
- 1. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta‐analysis. Lancet. 2016;387:957‐967. [DOI] [PubMed] [Google Scholar]
- 2. Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S. The burden of blood pressure‐related disease: a neglected priority for global health. Hypertension. 2007;50:991‐997. [DOI] [PubMed] [Google Scholar]
- 3. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic diurnal blood pressure variability between japanese and American treatment‐resistant hypertensive populations. Circ J. 2017;81:1337‐1345. [DOI] [PubMed] [Google Scholar]
- 4. Hoshide S, Kario K, de la Sierra A, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015;66:750‐756. [DOI] [PubMed] [Google Scholar]
- 5. Kario K, Tomitani N, Buranakitjaroen P, et al. Rationale and design for the Asia BP@Home study on home blood pressure control status in 12 Asian countries and regions. J Clin Hypertens (Greenwich). 2018;20:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kario K, Tomitani N, Buranakitjaroen P, et al. Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: Results of the Asia BP@Home study. J Clin Hypertens (Greenwich). 2018;20:1686‐1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Palatini P, Frigo G, Bertolo O, Roman E, Da Corta R, Winnicki M. Validation of the A&D TM‐2430 device for ambulatory blood pressure monitoring and evaluation of performance according to subjects' characteristics. Blood Press Monit. 1998;3:255‐260. [PubMed] [Google Scholar]
- 8. Kario K, Shin J, Chen CH, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: The HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:1250‐1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401‐1406. [DOI] [PubMed] [Google Scholar]
- 10. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702‐2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kario K, Hoshide S, Mizuno H, et al. Nighttime blood pressure phenotype and cardiovascular prognosis. Circulation. 2020;142(19):1810‐1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boggia J, Li Y, Thijs L, et al. International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes i. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219‐1229. [DOI] [PubMed] [Google Scholar]
- 13. Salles GF, Reboldi G, Fagard RH, et al. Prognostic Effect of the Nocturnal Blood Pressure Fall in Hypertensive Patients: The Ambulatory Blood Pressure Collaboration in Patients With Hypertension (ABC‐H) Meta‐Analysis. Hypertension. 2016;67:693‐700. [DOI] [PubMed] [Google Scholar]
- 14. Yang WY, Melgarejo JD, Thijs L, et al. International database on ambulatory blood pressure in relation to cardiovascular outcomes i. association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA. 2019;322:409‐420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Metoki H, Ohkubo T, Kikuya M, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149‐154. [DOI] [PubMed] [Google Scholar]
- 16. Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852‐857. [DOI] [PubMed] [Google Scholar]
- 17. Ingelsson E, Bjorklund‐Bodegard K, Lind L, Arnlov J, Sundstrom J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859‐2866. [DOI] [PubMed] [Google Scholar]
- 18. Bankir L, Bochud M, Maillard M, Bovet P, Gabriel A, Burnier M. Nighttime blood pressure and nocturnal dipping are associated with daytime urinary sodium excretion in African subjects. Hypertension. 2008;51:891‐898. [DOI] [PubMed] [Google Scholar]
- 19. Kimura G. Kidney and circadian blood pressure rhythm. Hypertension. 2008;51:827‐828. [DOI] [PubMed] [Google Scholar]
- 20. Kario K. Proposal of RAS‐diuretic vs. RAS‐calcium antagonist strategies in high‐risk hypertension: insight from the 24‐hour ambulatory blood pressure profile and central pressure. J Am Soc Hypertens. 2010;4:215‐218. [DOI] [PubMed] [Google Scholar]
- 21. Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world ‐ a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Modesti PA, Morabito M, Bertolozzi I, et al. Weather‐related changes in 24‐hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155‐161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


