Abstract
The “triple burden” of aging population, hypertension, and mental health problems making elderly in Asia is more vulnerable. There is evidence of a bidirectional relationship between mental health and hypertension, which results in lower quality of life, lower rate of treatment adherence, and higher mortality among elderly individuals. It is essential to overcome known barriers and care for the elderly with high‐risk factors in order to address these burdens. This review revealed that elderly with hypertension were more likely to suffer from depression and anxiety. Therefore, debunking myths, creating awareness regarding mental health, and increasing access to mental health resources through holistic community‐based programs would greatly reduce such problems and optimize the chances of success in controlling hypertension‐related problems.
Keywords: Asia, elderly, hypertension, mental health
1. INTRODUCTION
The World Health Organization (WHO) defines health as “A state of complete physical, mental, and social well‐being and not merely the absence of disease or infirmity.” The elderly, who account for more than 700 million individuals in the global population, are at higher risk of hypertension (67%) and mental disorders (15%). 1 , 2 , 3 , 4
Increased life expectancy does not always signify an improvement in the quality of life. On the contrary, the elderly might occasionally experience a compromised and poor quality of life. Studies have reported both direct and indirect correlation between physical and mental health. 4 , 5 , 6 According to the WHO, South‐East Asia has the highest number of cases of depressive and anxiety disorders compared to other regions, accounting for 7.2% and 2.8% of all Years Lived with Disability (YLD), respectively. 7 In addition, several national reports from Asia have demonstrated that hypertension, depression, and anxiety disorders occur predominantly in older adults. 8 Therefore, the elderly, especially in Asia, are vulnerable to the burden of hypertension and mental health problems (Table 1).
Table 1.
Proportion of elderly individuals,and prevalence of hypertension and depressive and anxiety disorders in HOPE Asia Network countries
| Country | Proportion of the elderly in 2019 a , % | Hypertension prevalence in the elderly, % | Depressive disorders in the elderly, % | Anxiety disorders in the elderly, % | Life expectancy in 2018, years | Reference |
|---|---|---|---|---|---|---|
| China | 11.5 |
65‐74: 55.7 75+: 60.2 |
3.86‐13.01 | 41 | 76.4 | 9‐14 |
| Hong Kong | 17.5 | 64.8 | 4.7 | 5.5 |
Men: 82 Women: 88 |
9,10,15‐18 |
| India | 6.4 | 40.5 | 21.9 | 10.8 | 68.8 | 9,10,19‐21 |
| Indonesia | 6.1 | 65‐74: 63.2 75+: 69.5 | 65‐74: 8 75+: 8.9 | 65‐74: 12.8 75+:15.8 | 69.3 | 8‐10 |
| Japan | 28.0 |
65‐74 :66.8 75+ : 78.1 |
1.2 |
1.1 |
84.2 | 10,22,23 |
| Malaysia | 6.9 | 70‐74: 75.4 | 16.5 | 3.6‐38 | 75.3 | 9,10,24‐27 |
| Pakistan | 4.3 | 60‐69 :76.7 | 22.9 | N/A | 66.5 | 9,10,28,29 |
| Philippines | 5.3 | 81.5 | 6.6 | N/A | 69.3 | 9,10,30,31 |
| Singapore | 12.4 | 73.9 | 3.7 | 15.5 | 82.9 | 9,10,32‐34 |
| South Korea | 15.1 |
60‐69 :51.8 70+ : 67.5 |
29.8‐38.1 | 6‐36.7 | 82.7 | 9,10,35‐37 |
| Taiwan | 14.4 |
65‐74: 53.2 75+: 73.3 |
13.3 | N/A | 80.2 | 9,38‐41 |
| Thailand | 12.4 | 16.7‐47.2 | 23.7 | 6.4 | 75.5 | 9,10,42,43 |
| Vietnam | 7.6 |
65‐74 :56.2 75+ : 69.8 |
66.9 (urban) | N/A | 76.3 | 9,10,44‐46 |
Elderly ages 65 and above according to 2019 World Population Prospect World Bank. 9
2. MENTAL HEALTH PROBLEMS IN ASIA
Asia has the world's largest population and is a diverse continent; therefore, mental health problems vary between countries. Despite Western transformation in some Asian cultures and modernization of evidence‐based medicine, there are several myths and false practices, both in rural and urban areas. Some of these are illnesses as a result of supernatural phenomena such as demonic possession, punishment by god due to past and current sins or other spiritual causes, false perception that mental illness is an untreatable condition, and the wrong practice of restraining people with mental illnesses by considering them worthless. 47 , 48 , 49
Mental health problems among individuals in Asia are more complicated than in the West. Asians have more cultural barriers such as stigma and discrimination, false beliefs, poor health literacy; and structural barriers such as poor personal and financial resources, which prevent people from seeking help from mental health professionals. 50 , 51 , 52
3. MENTAL HEALTH PROBLEMS AND CARDIOVASCULAR DISEASES
Depressive disorders are associated with cardiovascular disease (CVD) and poor long‐term outcomes. 53 , 54 Depression could significantly increase the risk of stroke‐related morbidity and mortality, independent of other risk factors such as hypertension and diabetes. 55 , 56 This finding was consistent across subgroups, wherein the estimated absolute risk differences associated with depression were 106 cases of total stroke, 53 cases of ischemic stroke, and 22 cases of fatal stroke per 100,000 individuals per year. 55 Jackson et al also found that adults with high levels of anxiety and depression had a 30% and 44% greater risk of heart attack and stroke, respectively. 57 Anxiety, as a sign of poor emotional regulation, increases the risk of cardiac events and mortality. 58 Another study showed that women who had experienced significant psychological distress had a higher incidence of CVD, and this association was not observed in men. 59 However, the Japan Morning Surge Home Blood Pressure (J‐HOP) study found an association between depression and cardiovascular events among men as they tended to have higher blood pressure and were more likely to experience asymptomatic target organ damage. 54
Arup et al reported that major depressive disorder, which causes dysregulation of the sympathetic nervous system and the hypothalamic‐hypophysis‐adrenal axis, increases the risk of ventricular arrhythmia and myocardial infarction. Proposed mechanisms included hypertension, left ventricular hypertrophy, coronary vasoconstriction, endothelial dysfunction, thrombocyte activation, and pro‐inflammatory cytokine production. 60 Poor lifestyle associated with depressive disorders can also be a possible underlying pathogenetic mechanism of stroke. 56
4. DEPRESSION, ANXIETY, AND HYPERTENSION
Depression and anxiety are the most common mental disorders associated with various symptoms, ranging from mild to severe. 7 The association between depression and hypertension remains controversial. 61 Shin and Hwang did not report any difference between depressed and normal subjects. 35 Previous studies have reported that depressive symptoms were associated with low blood pressure and that the blood pressure was found to be lower in hypertensive participants who were not on antihypertensive medication. 62 , 63 , 64 There is evidence of a bidirectional relationship between depression and hypertension, which results in lower quality of life, lower rate of treatment adherence, and higher mortality among elderly individuals with hypertension. 61 , 65 , 66 , 67 Moreover, a non‐randomized study showed that hypertensive patients with depressive symptoms required more antihypertensive drugs to achieve good control of their home blood pressure. 68
A study conducted in Spain showed that moderate/severe (but not mild) hypertension was closely related to depression. 69 Other studies have reported a positive correlation between hypertension and depression wherein, depression increased the risk of hypertension and cerebrovascular disease, and in turn, hypertension increased the severity of depression. 70 , 71 , 72 Apart from factors such as genetics, hyperactivity of the sympathetic nervous system, and use of anti‐depressants, Kuo and Pu hypothesized that simultaneous effects of hypertension and depression could increase mortality. 65 , 72 Kayano et al also found higher variations in blood pressure of patients with depression. 73 Furthermore, patients with masked hypertension also had a higher risk of depression compared to those with controlled hypertension. 73 The results of this study complement those of a Mexican study on individuals with depressive disorders, which showed an increased risk of uncontrolled hypertension possibly due to loss of interest and subsequent lower adherence to treatment. 74
A cross‐sectional study conducted in Andkhoy showed that hypertensive patients who were old, women, smokers, and diabetic were more likely to be associated with anxiety. 71 Hypertension—white‐coat hypertension, nocturnal and morning blood pressure surge—was also found to be associated with anxiety through disruption of the autonomic nervous system, leading to higher variations in blood pressure and cardiovascular events. 61 , 75 , 76 , 77 Estrogen may weaken the neurohormonal mediators that cause non‐dipping pattern of nocturnal blood pressure; therefore, depressive symptoms and non‐dipping of nocturnal blood pressure are less likely to occur in women. 78 The HOPE Asia Network study reported a high prevalence of white‐coat hypertension (28%). 79 Research has also reported that elderly patients were more likely to be anxious, thus demonstrating an increase in blood pressure and white‐coat hypertension. For example, differences in results might have been influenced by the anxiety related to measurements being recorded by the doctors or nurses. 80 Another study in Japan found that awake systolic blood pressure and pulse rate correlated with anxiety in women, while diurnal blood pressure variation was associated with working men who suffered from depression. 78
Loneliness is associated with an increased risk of developing coronary heart disease and stroke. People with poor social relationships have a 29% and 32% higher risk of developing coronary heart disease and stroke, respectively. 81 , 82 A study reported that assessment of loneliness at the beginning of the study could predict the increment in systolic blood pressure in the second, third, and fourth years (B = 0.152, SE = 0.091, P <.05, one‐tailed). 83 This cumulative increase suggested that higher initial levels of loneliness were associated with a greater increment in systolic blood pressure over the study period of four years. 83 Association between loneliness and CVD remained significant after controlling for biological and behavioral CVD risk factors, such as depression, anxiety, self‐esteem, and other behaviors such as alcohol consumption and physical activity, suggesting a psychological pathway. 81
5. HYPERTENSION, CEREBROVASCULAR PATHOLOGY, AND LATE‐LIFE DEPRESSION
Depression in the elderly, or referred to as late‐life depression (LLD), commonly defined as any depressive episode occurring at age 65 or later, regardless of the age of onset. 84 The LLD is a heterogeneous condition with different etiologies, where genetics mostly influence early life and psychosocial contributes to later life. 85 Biological factors of LLD include cerebrovascular pathology, disorders of the endocrine system, presence of inflammatory processes, and nutritional status. 85 (Figure 1.)
Figure 1.
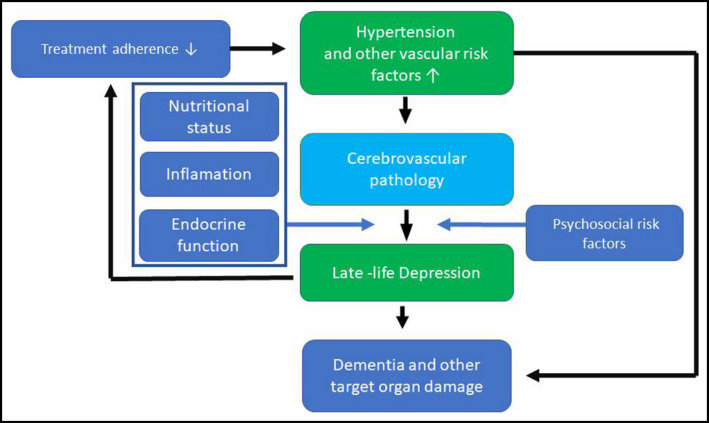
The biopsychosocial relationship between hypertension and depression
In contrast to depressive disorders in young adults, LLD is associated with cerebrovascular comorbidities, so‐called vascular depression. 84 Cerebrovascular pathology—such as white matter lesions—is strongly associated with hypertension as a risk factor. 85 , 86
A review by Baldwin RC, et al shows a close relationship between brain vascular disorders with mental health, especially depression; for example, depressions are more prominent in vascular dementia than Alzheimer's dementia. Patient with cerebrovascular disease, especially in anterior hemisphere lesions, often experiencing lability of the mood; on the other hand, silent stroke also mainly present in people with depression. 87
The development of neuroimaging techniques showed the bidirectional association between LLD with the cerebrovascular disease—measured as white matter hyperintensity (WMH) burden—and treatment responsiveness. 88 WMH histopathology studies reflect myelin damage and fluid accumulation among other underlying pathology. WMHs are associated with lower white matter microstructural integrity and altered brain function. 89 Other pathological features in poststroke depressed patients are gray matter loss, subcortical lacunes, microinfarcts and microbleeds, frontal and temporal (hippocampal) gray matter changes/atrophy, neurodegenerative pathologies, and related biochemical changes. 88 , 89
6. DEPRESSION AND MEDICAL ADHERENCE TO ANTIHYPERTENSIVE TREATMENT
Providers should assess treatment adherence, treatment recommendations for comorbid diseases, and identify depression in evaluating antihypertensive medications in patients with uncontrolled blood pressure. 90 Hypertension can cause pathological disorders in the brain with depressive symptoms; causing patients do not comply with treatment, resulting in uncontrolled hypertension, adding more risk to vascular disorders in the brain and more severe depression. (Figure 1) Hypertensive patients present with other chronic diseases may experience profound emotions which increase their risk for mental health disorders. Management of negative emotions that can influence adherence to therapies are important in the hypertension management. 91 Detection of depression in hypertensive patients would facilitate management of depression, resulting in improve medication adherence, depressive symptoms, and blood pressure control in those patients with both chronic illnesses. 90
Drawing a causal relationship between anxiety, depression, and stress in hypertension may be difficult; but, overlooking the association may further increase the burden of medication nonadherence. 91 Poor adherence to antihypertensive medications remains a significant challenge in the management of patients with hypertension. It has many serious effects on the prognosis of the illness and overall effectiveness of the health system. Nonadherence may signal that the patient and physician have different goals and priorities regarding the treatment and its schedule. 92
Depressive disorder in the elderly appears to be linked with self‐efficacy, which can be influenced by employment or physical functions, such as sight, hearing, and chewing. In a study performed in South Korea, where the prevalence of depressive disorder and nonadherence was 29.8% and 60%, respectively, worse adherence to medication was independently associated with depressive disorder. However, this association was primarily mediated by self‐efficacy. Considering that depression and self‐efficacy are the essential components associated with motivation for medication adherence, a more systematic approach would be required to resolve these barriers to improve control of hypertension in the elderly. 93
7. OVERCOMING THE “TRIPLE BURDEN” IN ASIA
The term of “triple burden” we meant is characterized by the coexistence of being elderly, along with hypertension and mental health problems (Figure 1). According to Age Concern and the Mental Health Foundation, the five key factors affecting mental health in the elderly are discrimination, meaningful participation, relationship, physical health, and poverty. 94 Known risk factors for this burden include age >80 years, female sex, being unmarried and living alone, low income, living in rural areas, frailty and low functional status, cognitive decline, poor family functioning, poor sleep quality, illiteracy, as well as stressful life events such as death of partner in the past two years, and recent separation, retirement, unemployment, and history of health problems or disability. 24 , 61 , 70 , 95 , 96 , 97 , 98 Diet restriction, such as spiritual fasting and physical activity, were found to be protective factors in patients with depressive disorders. 24 , 46
In addition, a systematic review conducted by Shi et al reported the possible barriers to help‐seeking behavior in people with mental illnesses as follows: 1) seeking help from alternative sources, 2) misconception, 3) self‐reliance and unwillingness to seek help, 4) low perceived need, 5) fear of stigma, 6) negative experiences and attitude toward treatments, 7) affordability and accessibility, 8) family opposition, 9) sociodemographic barriers, and 10) inability to recognize mental illness. 99
It is important to overcome known barriers and care for the elderly with high‐risk factors in order to address the “triple burden” (Figure 2). Screening individuals and promoting mental health awareness is important to reduce stigma, specifically among those living in rural areas. Furthermore, favorable attitude of physicians toward hypertensive patients with depressive symptoms and availability of social support are important to combat depressive disorders in the community and increase the treatment adherence. 54 , 68 , 74 , 92 , 100 , 101 , 102
Figure 2.
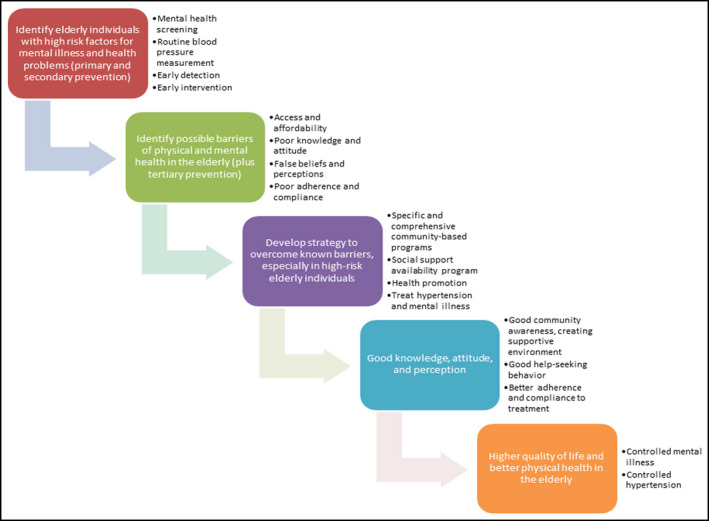
Overcoming the “triple burden” in Asia program
8. CONCLUSION
Mental health problems are strongly correlated with the success of hypertension management strategies. People with hypertension are more likely to suffer from depression and anxiety. Therefore, increasing awareness in the population regarding mental health and increasing access to mental health resources through concrete community‐based programs would greatly reduce such problems and optimize the chances of success in controlling hypertension‐related problems.
DISCLOSURE
YC Chia has received speakers’ honorarium and sponsorship to attend conferences and CME seminars from Abbott, Bayer, Boehringer Ingelheim Pharmaceuticals, GlaxoSmithKline, Menarini, Merck Sharp & Dohme, Novartis, Omron, Pfizer, and Sanofi and Xepa‐Soul Pattinson, and a research grant from Pfizer Inc J Shin has received lecture honoraria from Pfizer Inc, Hanmi Pharm. Co. Ltd., Yuhan Co. Ltd., Boryung Pharmaceutical Co. Ltd., consulting fees from Hanmi Pharm. Co. Ltd., and research grants from Sanofi Pharm. and Hanmi Pharm. Co. Ltd. CH Chen reports personal fees from Novartis, Sanofi, Daiichi Sankyo, Servier, and Boehringer Ingelheim Pharmaceuticals Inc S Park has received honoraria from Pfizer Inc, Daiichi Sankyo, Takeda Pharmaceuticals International, Daewon Pharmaceutical Company, Boryung Pharmaceutical Company, and Servier. S Park has also received a research grant from Daiichi Sankyo. S Siddique has received honoraria from Bayer, Novartis, Pfizer Inc, ICI, and Servier, and travel, accommodation, and conference registration support from Hilton Pharma, Atco Pharmaceutical, Highnoon Laboratories, Horizon Pharma, and ICI. HM Cheng has received speakers’ honorarium and sponsorship to attend conferences and CME seminars from Eli Lilly and AstraZeneca; Pfizer Inc, Bayer AG, Boehringer Ingelheim Pharmaceuticals Inc, Daiichi Sankyo, Novartis Pharmaceuticals Inc Servier, Sanofi, and Takeda Pharmaceuticals International, and has served as an advisor or consultant for ApoDx Technology Inc K Kario received a research grant from MSD K.K, Astellas Pharma Inc, Eisai Co., Otsuka Pharmaceutical Co., Sanwa Kagaku Kenkyusho Co., Daiichi Sankyo Co., Taisho Pharmaceutical Co., Ltd., Sumitomo Dainippon Pharma Co., Takeda Pharmaceutical Co., Teijin Pharma, Boehringer Ingelheim Japan Inc, Bristol‐Myers Squibb K.K, and Mochida Pharmaceutical Co. Ltd., and honoraria from Daiichi Sankyo Co. Ltd. and Mylan EPD. All other authors report no potential conflicts of interest in relation to this article.
AUTHOR CONTRIBUTIONS
Manuscript title: Mental health problems and hypertension in the elderly: Review from the HOPE Asia Network. Yuda Turana involved in conception and design of study, data analysis and/or interpretation, drafting and/or critical revision of manuscript, and approval of final version of manuscript. Jeslyn Tengkawan, Kazuomi Kario, and Yook Chin Chia involved in data analysis and/or interpretation, drafting and/or critical revision of manuscript, and approval of final version of manuscript. Jinho Shin, Chen‐Huan Chen, Sungha Park, Kelvin Tsoi, Peera Buranakitjaroen, Arieska Ann Soenarta, Saulat Siddique, Hao‐Min Cheng, Jam Chin Tay, Boon Wee Teo, and Tzung‐Dau Wang involved in data analysis and/or interpretation, drafting and/or critical revision of manuscript.
Contributor Information
Yuda Turana, Email: yuda.turana@atmajaya.ac.id.
Kazuomi Kario, Email: kkario@jichi.ac.jp.
REFERENCES
- 1. Constitution [Internet]. Accessed June 15, 2020. https://www.who.int/about/who-we-are/constitution
- 2. Our world is growing older: UN DESA releases new report on ageing [Internet]. UN DESA | United Nations Department of Economic and Social Affairs. 2019. https://www.un.org/development/desa/en/news/population/our-world-is-growing-older.html. Accessed June 15, 2020.
- 3. Lionakis N, Mendrinos D, Sanidas E, Favatas G, Georgopoulou M. Hypertension in the elderly. World J Cardiol. 2012;4(5):135‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mental health of older adults [Internet]. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults. Accessed June 15, 2020
- 5. Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: A mediation analysis. Soc Sci Med. 2017;1(195):42‐49. [DOI] [PubMed] [Google Scholar]
- 6. Min J‐A, Lee C‐U, Lee C. Mental Health Promotion and Illness Prevention: A Challenge for Psychiatrists. Psychiatry Investig. 2013;10(4):307‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . Depression and Other Common Mental Disorders: Global Health Estimates [Internet] (24 p). Geneva, Switzerland; 2017. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?sequence=1 [Google Scholar]
- 8. Ministry of Health and National Institute of Health Research and Development. National report on basic health research, Riskesdas, 2018. Jakarta, Indonesia, 2018.
- 9. Population ages 65 and above (% of total population) | Data [Internet]. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?end=2019&start=2018. Accessed June 15, 2020
- 10. World Life Expectancy [Internet] . World Life Expectancy. https://www.worldlifeexpectancy.com/. Accessed June 15, 2020
- 11. Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344‐2356. [DOI] [PubMed] [Google Scholar]
- 12. Li N, Pang L, Chen G, Song X, Zhang J, Zheng X. Risk factors for depression in older adults in Beijing. Can J Psychiatry. 2011;56(8):466‐473. [DOI] [PubMed] [Google Scholar]
- 13. Lim LL, Chang W, Yu X, Chiu H, Chong MY, Kua EH. Depression in Chinese elderly populations. Asia‐Pacific Psychiatry. 2011;23(3):46‐53. [Google Scholar]
- 14. Wang L, Shentu Q, Xu B, Liang Y. The prevalence of anxiety on the empty‐nest elders in China. J Health Psychol. 2020;25(2):152‐160. [DOI] [PubMed] [Google Scholar]
- 15. Hong Kong 2016 Population By‐census ‐ Thematic Report : Older Persons | Census and Statistics Department [Internet]. https://www.censtatd.gov.hk/hkstat/sub/sp459.jsp?productCode=B1120105. Accessed August 27, 2020
- 16. Centre for Health Protection ‐ Report of Population Health Survey 2014/15 [Internet]. https://www.chp.gov.hk/en/static/51256.html. Accessed August 27, 2020
- 17. Lam LC‐W, Wong CS‐M, Wang M‐J, et al. Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: the Hong Kong Mental Morbidity Survey (HKMMS). Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1379‐1388. [DOI] [PubMed] [Google Scholar]
- 18. Hong Kong Life Tables | Census and Statistics Department [Internet]. https://www.censtatd.gov.hk/hkstat/sub/sp190.jsp?productCode=B1120016. Accessed August 27, 2020
- 19. Subramanyam AA, Kedare J, Singh OP, Pinto C. Clinical practice guidelines for geriatric anxiety disorders. Indian J Psychiatry. 2018;60(7):371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chinnakali P, Mohan B, Upadhyay RP, Singh AK, Srivastava R, Yadav K. Hypertension in the Elderly: Prevalence and Health Seeking Behavior. North Am J Med Sci. 2012;4(11):558‐562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barua A, Ghosh MK, Kar N, Basilio MA. Prevalence of depressive disorders in the elderly. Ann Saudi Med. 2011;31(6):620‐624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ministry of Health, Labour and Welfare . National Health and Nutrition Survey 2018 [Internet]. https://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html. Accessed May 7, 2020
- 23. Kawakami N. World Mental Health Japan Survey 2 [Internet]. 2016 May [cited 2020 May 17] p. 1–168. http://wmhj2.jp/WMHJ2-2016R.pdf
- 24. Vanoh D, Shahar S, Yahya HM, Hamid TA. Prevalence and determinants of depressive disorders among community‐dwelling older adults: Findings from the towards useful aging study. Int J Gerontol. 2016;10(2):81‐85. [Google Scholar]
- 25. Prevalence of Loneliness, Anxiety, and Depression among Older People Living in Long‐Term Care: A Review | INTERNATIONAL JOURNAL OF CARE SCHOLARS. https://journals.iium.edu.my/ijcs/index.php/ijcs/article/view/44. Accessed July 17, 2020
- 26. Ab Majid NL, Omar MA, Khoo YY, et al. Prevalence, Awareness, Treatment and Control of hypertension in the Malaysian population: findings from the National Health and Morbidity Survey 2006–2015. J Hum Hypertens. 2018;32(8):617‐624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yusoff MFM, Chan YY, Man CS. Malaysia National Health and Morbidity Survey 2015. Ministry of Health Malaysia. 2015. [Google Scholar]
- 28. Ganatra HA, Zafar SN, Qidwai W, Rozi S. Prevalence and predictors of depression among an elderly population of Pakistan. Aging Ment Health. 2008;12(3):349‐356. [DOI] [PubMed] [Google Scholar]
- 29. Pakistan Health Research Council . Non‐communicable Diseases Survey – Pakistan. Islamabad, Pakistan: World Health Organization; 2016. [Google Scholar]
- 30. Arellano R, Ramos J, Delacruz M, Lequin R, Gregorio C, Dean M. Prevalence, awareness, treatment and control of hypertension and medication adherence among elderly in Barangay 836, Pandacan, manila, Philippines. Int J Res Pharm Chem. 2019;9(2):1‐6. https://www.ijrpc.com/files/01-06-19/01.pdf [Google Scholar]
- 31. Prevalence of Depression among the Elderly Population in Rizal Province Using the Geriatric Depression Scale – Geneva Health Forum Archive [Internet]. http://ghf.g2hp.net/2011/09/29/prevalence-of-depression-among-the-elderly-using-the-geriatric-depression-scale-sf-15-in-rizal-province-philippines/. Accessed July 18, 2020
- 32. Malhotra R, Chan A, Malhotra C, Østbye T. Prevalence, awareness, treatment and control of hypertension in the elderly population of Singapore. Hypertens Res. 2010;33(12):1223‐1231. [DOI] [PubMed] [Google Scholar]
- 33. Subramaniam M, Abdin E, Sambasivam R, et al. Prevalence of Depression among Older Adults‐Results from the Well‐being of the Singapore Elderly Study. Ann Acad Med Singapore. 2016;45(4):123‐133. [PubMed] [Google Scholar]
- 34. Chuan SK, Kumar R, Matthew N, Heok KE, Pin NT. Subsyndromal depression in old age: clinical significance and impact in a multi‐ethnic community sample of elderly Singaporeans. Int Psychogeriatr. 2008;20(1):188‐200. [DOI] [PubMed] [Google Scholar]
- 35. Shin S, Hwang E. Factors Influencing Depressive Symptoms among Korean Older Adults with Chronic Illnesses: Using the 2014 National Survey on Older Adults. Korean J Adult Nurs. 2018;30(6):577‐585. [Google Scholar]
- 36. Kang H‐J, Bae K‐Y, Kim S‐W, Shin I‐S, Yoon J‐S, Kim J‐M. Anxiety symptoms in Korean elderly individuals: a two‐year longitudinal community study. Int Psychogeriatr. 2016;28(3):423‐433. [DOI] [PubMed] [Google Scholar]
- 37. Kang S‐H, Kim S‐H, Cho JH, et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Korea. Sci Rep. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6662850/. Accessed July 18, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Taiwan now considered an “aged society” ‐ Xinhua | English.news.cn [Internet]. http://www.xinhuanet.com/english/2018-10/15/c_137534436.htm. Accessed June 15, 2020
- 39. Taiwan: life expectancy 2018 [Internet]. Statista. https://www.statista.com/statistics/861001/taiwan-life-expectancy/. Accessed June 15, 2020
- 40. Chuang S‐Y, Chang H‐Y, Cheng H‐M, Pan W‐H, Chen C‐H. Prevalence of Hypertension Defined by Central Blood Pressure Measured Using a Type II Device in a Nationally Representative Cohort. Am J Hypertens. 2018;31(3):346‐354. [DOI] [PubMed] [Google Scholar]
- 41. Tai S‐Y, Ma T‐C, Wang L‐C, Yang Y‐H.A Community‐Based Walk‐In Screening of Depression in Taiwan [Internet]. Vol. 2014, The Scientific World Journal. Hindawi; 2014. p. e184018. https://www.hindawi.com/journals/tswj/2014/184018/. Accessed July 18, 2020 [DOI] [PMC free article] [PubMed]
- 42. Viriyavejakul A, Senanarong V, Prayoonwiwat N, Praditsuwan R, Chaisevikul R, Poungvarin N. Epidemiology of stroke in the elderly in Thailand. J Med Assoc Thail Chotmaihet Thangphaet. 1998;81(7):497‐505. [PubMed] [Google Scholar]
- 43. Wongpakaran N, Wongpakaran T, Lerttrakarnnon P, et al. Prevalence, clinical and psychosocial variables of depression, anxiety and suicidality in geriatric tertiary care settings. Asian J Psychiatry. 2019;41:38‐44. [DOI] [PubMed] [Google Scholar]
- 44. Son PT, Quang NN, Viet NL, et al. Prevalence, awareness, treatment and control of hypertension in Vietnam—results from a national survey. J Hum Hypertens. 2012;26(4):268‐280. [DOI] [PubMed] [Google Scholar]
- 45. Table 4 Individuals who participated in the study and those with evidence of hypertension, awareness of their blood pressure condition, receiving treatment and with control of hypertension. https://www.nature.com/articles/jhh201118/tables/4. Accessed July 18, 2020
- 46. Dao ATM, Nguyen VT, Nguyen HV, Nguyen LTK.Factors Associated with Depression among the Elderly Living in Urban Vietnam [Internet]. Vol. 2018, BioMed Research International. Hindawi; 2018. p. e2370284. https://www.hindawi.com/journals/bmri/2018/2370284/. Accessed June 15, 2020 [DOI] [PMC free article] [PubMed]
- 47. Hartini N, Fardana NA, Ariana AD, Wardana ND. Stigma toward people with mental health problems in Indonesia. Psychol Res Behav Manag. 2018;31(11):535‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Choudhry FR, Mani V, Ming LC, Khan TM. Beliefs and perception about mental health issues: a meta‐synthesis. Neuropsychiatr Dis Treat. 2016;31(12):2807‐2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kishore J, Gupta A, Jiloha RC, Bantman P. Myths, beliefs and perceptions about mental disorders and health‐seeking behavior in Delhi. India. Indian J Psychiatry. 2011;53(4):324‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry Abingdon Engl. 2007;19(2):157‐178. [DOI] [PubMed] [Google Scholar]
- 51. Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help‐seeking amongst refugees: A systematic review. Clin Psychol Rev. 2020;1(75):101812. [DOI] [PubMed] [Google Scholar]
- 52. Chong SA, Abdin E, Picco L, et al. Recognition of mental disorders among a multiracial population in Southeast Asia. BMC Psychiatry. 2016;16(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365‐1372. [DOI] [PubMed] [Google Scholar]
- 54. Kabutoya T, Hoshide S, Davidson KW, Kario K. Sex differences and the prognosis of depressive and nondepressive patients with cardiovascular risk factors: the Japan Morning Surge‐Home Blood Pressure (J‐HOP) study. Hypertens Res Off J Jpn Soc Hypertens. 2018;41(11):965‐972. [DOI] [PubMed] [Google Scholar]
- 55. Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and the Risk of Stroke Morbidity and Mortality: A Meta‐analysis and Systematic Review. JAMA J Am Med Assoc. 2011;306(11):1241‐1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jia‐Yi D, Yong‐Hong Z, Jian T, Li‐Qiang Q. Depression and Risk of Stroke. Stroke. 2012;43(1):32‐37. [DOI] [PubMed] [Google Scholar]
- 57. Jackson CA, Sudlow CLM, Mishra GD. Psychological Distress and Risk of Myocardial Infarction and Stroke in the 45 and Up Study: A Prospective Cohort Study. Circ Cardiovasc Qual Outcomes [Internet]. 2018;11(9). https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.117.004500. Accessed June 17, 2020 [DOI] [PubMed] [Google Scholar]
- 58. Ouakinin SRS. Anxiety as a Risk Factor for Cardiovascular Diseases. Front Psychiatry [Internet]. 2016;7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4764710/. Accessed June 17, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pimple P, Lima BB, Hammadah M, et al. Psychological Distress and Subsequent Cardiovascular Events in Individuals With Coronary Artery Disease. J Am Heart Assoc [Internet]. 2019;8(9). https://www.ahajournals.org/doi/10.1161/JAHA.118.011866. Accessed June 17, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Dhar AK, Barton DA. Depression and the Link with Cardiovascular Disease. Front Psychiatry. 2016;21(7):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kabutoya T, Kario K. Depression in hypertension and blood pressure variability over shorter time periods. Hypertens Res. 2015;38(11):713‐715. [DOI] [PubMed] [Google Scholar]
- 62. Niu K, Hozawa A, Awata S, et al. Home blood pressure is associated with depressive symptoms in an elderly population aged 70 years and over: a population‐based, cross‐sectional analysis. Hypertens Res Off J Jpn Soc Hypertens. 2008;31(3):409‐416. [DOI] [PubMed] [Google Scholar]
- 63. Lenoir H, Lacombe J‐M, Dufouil C, et al. Relationship between blood pressure and depression in the elderly. The Three‐City Study J Hypertens. 2008;26(9):1765‐1772. [DOI] [PubMed] [Google Scholar]
- 64. Ng T‐P, Feng L, Niti M, Yap K‐B. Low blood pressure and depressive symptoms among Chinese older subjects: a population‐based study. Am J Med. 2010;123(4):342‐349. [DOI] [PubMed] [Google Scholar]
- 65. Kuo P‐L, Pu C. The contribution of depression to mortality among elderly with self‐reported hypertension: analysis using a national representative longitudinal survey. J Hypertens. 2011;29(11):2084‐2090. [DOI] [PubMed] [Google Scholar]
- 66. Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of Depression in Patients With Hypertension: A Systematic Review and Meta‐Analysis. Medicine (Baltimore). 2015;94(31):e1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Axon RN, Zhao Y, Egede LE. Association of depressive symptoms with all‐cause and ischemic heart disease mortality in adults with self‐reported hypertension. Am J Hypertens. 2010;23(1):30‐37. [DOI] [PubMed] [Google Scholar]
- 68. Kabutoya T, Ishikawa J, Hoshide S, Eguchi K, Shimada K, Kario K. Poor blood pressure and urinary albumin excretion responses to home blood pressure‐based antihypertensive therapy in depressive hypertensive patients. J Clin Hypertens Greenwich Conn. 2010;12(5):345‐349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lobo‐Escolar A, Roy JF, Saz P, De‐la‐Cámara C, Marcos G, Lobo A. Association of Hypertension with Depression in Community‐Dwelling Elderly Persons: Results from the ZARADEMP Project. Psychother Psychosom. 2008;77(5):323‐325. [DOI] [PubMed] [Google Scholar]
- 70. Ma L, Tang Z, Sun F, et al. Risk factors for depression among elderly subjects with hypertension living at home in China. Int J Clin Exp Med. 2015;8(2):2923‐2928. [PMC free article] [PubMed] [Google Scholar]
- 71. Hamrah MS, Hamrah MH, Ishii H, et al. Anxiety and Depression among Hypertensive Outpatients in Afghanistan: A Cross‐Sectional Study in Andkhoy City. Int J Hypertens. 2018;1(2018):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Peltzer K, Pengpid S.The Prevalence and Social Determinants of Hypertension among Adults in Indonesia: A Cross‐Sectional Population‐Based National Survey [Internet]. Vol. 2018, International Journal of Hypertension. Hindawi; 2018 [cited 2020 Jun 17]. p. e5610725. https://www.hindawi.com/journals/ijhy/2018/5610725/ [DOI] [PMC free article] [PubMed]
- 73. Kayano H, Koba S, Matsui T, et al. Impact of depression on masked hypertension and variability in home blood pressure in treated hypertensive patients. Hypertens Res Off J Jpn Soc Hypertens. 2015;38(11):751‐757. [DOI] [PubMed] [Google Scholar]
- 74. Rubio‐Guerra AF, Rodriguez‐Lopez L, Vargas‐Ayala G, Huerta‐Ramirez S, Serna DC, Lozano‐Nuevo JJ. Depression increases the risk for uncontrolled hypertension. Exp Clin Cardiol. 2013;18(1):10‐12. [PMC free article] [PubMed] [Google Scholar]
- 75. Kayano H, Koba S, Matsui T, et al. Anxiety Disorder Is Associated With Nocturnal and Early Morning Hypertension With or Without Morning Surge. Circ J. 2012;76(7):1670‐1677. [DOI] [PubMed] [Google Scholar]
- 76. Xu X‐J, Xing H‐Y, Wang Y‐Z. The effect of anxiety depression on morning blood pressure surge and heart rate variability in patients with hypertension. Int J Cardiol. 2009;137:S36. [Google Scholar]
- 77. Scalco AZ, Scalco MZ, Azul JBS, Lotufo NF. Hypertension and depression. Clin Sao Paulo Braz. 2005;60(3):241‐250. [DOI] [PubMed] [Google Scholar]
- 78. Kario K, Schwartz JE, Davidson KW, Pickering TG. Gender differences in associations of diurnal blood pressure variation, awake physical activity, and sleep quality with negative affect: the work site blood pressure study. Hypertens Dallas Tex 1979. 2001;38(5):997‐1002. [DOI] [PubMed] [Google Scholar]
- 79. Kario K, Tomitani N, Buranakitjaroen P, et al. Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: Results of the Asia BP@Home study. J Clin Hypertens. 2018;20(12):1686‐1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Cobos B, Haskard‐Zolnierek K, Howard K. White coat hypertension: improving the patient–health care practitioner relationship. Psychol Res Behav Manag. 2015;2(8):133‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. Eur J Prev Cardiol. 2018;25(13):1387‐1396. [DOI] [PubMed] [Google Scholar]
- 82. Boden‐Albala B, Litwak E, Elkind MSV, Rundek T, Sacco RL. Social isolation and outcomes post stroke. Neurology. 2005;64(11):1888‐1892. [DOI] [PubMed] [Google Scholar]
- 83. Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5‐year cross‐lagged analyses in middle‐aged and older adults. Psychol Aging. 2010;25(1):132‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Aizenstein HJ, Baskys A, Boldrini M, et al. Vascular depression consensus report ‐ a critical update. BMC Med. 2016;14(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Tiemeier H. Biological Risk Factors for Late Life Depression. Eur J Epidemiol. 2003;18(8):745‐750. [DOI] [PubMed] [Google Scholar]
- 86. Lazarus R, Prettyman R, Cherryman G. White matter lesions on magnetic resonance imaging and their relationship with vascular risk factors in memory clinic attenders. Int J Geriatr Psychiatry. 2005;20(3):274‐279. [DOI] [PubMed] [Google Scholar]
- 87. Baldwin RC, O’Brien J. Vascular basis of late‐onset depressive disorder. Br J Psychiatry J Ment Sci. 2002;180:157‐160. [DOI] [PubMed] [Google Scholar]
- 88. Santos M, Gold G, Kövari Enikö, et al. Differential impact of lacunes and microvascular lesions on poststroke depression. Stroke. 2009;40(11):3557‐3562. [DOI] [PubMed] [Google Scholar]
- 89. Smagula SF, Aizenstein HJ. Brain structural connectivity in late‐life major depressive disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016;1(3):271‐277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Krousel‐Wood MA, Frohlich ED. Hypertension and depression: coexisting barriers to medication adherence. J Clin Hypertens Greenwich Conn. 2010;12(7):481‐486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kretchy IA, Owusu‐Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti‐hypertensive medication adherence. Int J Ment Health Syst. 2014;21(8):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Lucca J, Ramesh M, Parthasarathi G, Ram D. Incidence and factors associated with medication nonadherence in patients with mental illness: A cross‐sectional study. J Postgrad Med. 2015;61(4):251‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Son Y‐J, Won MH. Depression and medication adherence among older Korean patients with hypertension: Mediating role of self‐efficacy. Int J Nurs Pract. 2017;23(3):e12525. [DOI] [PubMed] [Google Scholar]
- 94. Promoting Mental Health And Well‐being In Later Life [Internet]. Mental Health Foundation. 2006. https://www.mentalhealth.org.uk/publications/promoting-mental-health-and-well-being-later-life. Accessed June 15, 2020.
- 95. Quality statement 1: Identifying those at risk of a decline | Mental wellbeing and independence for older people | Quality standards | NICE [Internet]. NICE. https://www.nice.org.uk/guidance/qs137/chapter/Quality-statement-1-Identifying-those-at-risk-of-a-decline. Accessed June 15, 2020.
- 96. Zou C, Chen S, Shen J, et al. Prevalence and associated factors of depressive symptoms among elderly inpatients of a Chinese tertiary hospital. Clin Interv Aging. 2018;13:1755‐1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Ogbo FA, Mathsyaraja S, Koti RK, Perz J, Page A. The burden of depressive disorders in South Asia, 1990–2016: findings from the global burden of disease study. BMC Psychiatry. 2018;18(1):333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Manaf MRA, Mustafa M, Rahman MRA, Yusof KH, Aziz NAA. Factors Influencing the Prevalence of Mental Health Problems among Malay Elderly Residing in a Rural Community: A Cross‐Sectional Study. PLoS One. 2016;11(6):e0156937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Shi W, Shen Z, Wang S, Hall BJ. Barriers to Professional Mental Health Help‐Seeking Among Chinese Adults: A Systematic Review. Front Psychiatry [Internet]. 2020;11. https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00442/full. Accessed June 16, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Huang D, Yang LH, Pescosolido BA. Understanding the public’s profile of mental health literacy in China: a nationwide study. BMC Psychiatry. 2019;19(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Mohd TAMT, Yunus RM, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ Open. 2019;9(7):e026667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Kua EH, Rathi M. Mental health care in Singapore: Current and future challenges. Taiwan J Psychiatry. 2019;33(1):6. [Google Scholar]


