Abstract
Hypertension (HT) is a prominent cardiovascular risk factor. Although there are various pharmacological treatment choices for this condition, many patients fail to adhere to them, making non‐pharmacological options attractive alternatives. Foot reflexology has been proven to decrease blood pressure (BP), but data are limited in patients with stage‐2 HT. We conducted a randomized clinical trial to examine the effectiveness of foot reflexology in reducing BP and heart rate (HR). Stage‐2 HT patients were enrolled and randomized into the intervention and the control groups (n = 47, each), the former of which underwent foot reflexology during a follow‐up visit. Office BP and HR were measured before and at 15 and 30 min after the procedure in the intervention group and after resting in the control group. In the intervention group, systolic BP (SBP), diastolic BP (DBP), and HR at 15 min were significantly lower than at baseline: −3.29 mm Hg (95%CI; −5.64 to −0.93), −1.71 mm Hg (95%CI; −3.11 to −0.32), and −1.71 beats per min (bpm; 95%CI; −2.88 to −0.54), respectively. Similar trends were also observed at 30 min. However, when compared with the control group, only the reduction in HR was significant (−4.96 bpm; 95%CI, −9.63 to −0.28). We conclude that foot reflexology was effective in reducing HR in stage‐2 HT patients and partially effective in reducing BP.
Keywords: acupressure, hypertension, non‐pharmacological therapy, pulse rate, reflexology
1. INTRODUCTION
Uncontrolled hypertension (HT) is an important risk factor for major cardiovascular events. 1 Moreover, one study in the United States found that only half of patients achieve target blood pressure (BP). 2 Based on national health survey data, the rate of uncontrolled HT (BP >140/90 mm Hg) in Thailand is approximately 80% in patients undergoing conventional treatment. 3 Recent HT guidelines recommend a lower BP target (≤130/80 mm Hg) for the prevention of cardiovascular events in adults, 4 , 5 which further increases the rate of uncontrolled HT. In addition to elevated BP, increased heart rate (HR) is also common in HT patients. Epidemiological studies found that around 40% of HT patients had HR >80 beats per minute (bpm) 6 and that HR was associated with increased risk of cardiovascular events and all‐cause mortality. 7 There have been various studies examining the effectiveness pharmacological treatments for BP and HR, 8 , 9 but there are limited data available on the impact of non‐pharmacological treatment options.
Previous studies have shown complementary therapies (eg, music therapy, acupuncture, and reflexology) to be effective adjunctive treatments for lowering BP. 10 , 11 , 12 , 13 Foot reflexology, a traditional therapy that is well‐known in many Asian countries (such as China, India, and Thailand), is one such promising treatment. 14 , 15 However, there is yet no consensus regarding the effect of foot reflexology on systolic and diastolic BP (SBP and DBP). 16 , 17 , 18 Although one trial found foot reflexology to be beneficial in terms of stress response and biofeedback, 19 there have yet been no randomized trials showing its effect on both BP and HR. In addition, while many trials have explored the benefits foot reflexology in chronic disease and cancer patients, 20 , 21 few have enrolled only HT patients. 16 , 17 , 18
Foot reflexology is a noninvasive treatment and has long been practiced in Thailand. It is recommended by the Department of Thai Traditional and Alternative Medicine under the Ministry of Public Health in order to promote health in older adults, 22 suggesting that it may be useful as an adjunctive treatment for HT patients. This was a well‐controlled, randomized trial to examine the effects of foot reflexology on office SBP, DBP, and HR in individuals with stage‐2 HT.
2. MATERIALS AND METHODS
2.1. Study design and setting
This study was a parallel‐group, randomized clinical trial (RCT) conducted from November 1, 2018 to May 31, 2019 at the Hypertensive Crisis Clinic at Srinagarind Hospital, a tertiary‐care university hospital located in northeast Thailand. The Khon Kaen University ethics committee approved the study protocol, and informed consent was obtained from all participants before enrollment. This trial was registered retrospectively on ClinicalTrials.gov (registration number: NCT04516005).
2.2. Participants
Eligible participants were adults between 40 and 80 years of age diagnosed with stage‐2 HT (defined as office SBP ≥140 mm Hg and/or DBP ≥90 mm Hg at the first hospital visit) and who had been on a stable anti‐HT drug regimen for at least 3 months before enrollment. Exclusion criteria were (a) pregnancy, (b) history of foot surgery or bone fracture, (c) skin disease of the foot, and (d) diabetic neuropathy.
2.3. Sample size calculation
The sample size for comparing mean SBP and DBP with repeated measures was calculated using the following parameters: two tails, alpha error probability of 0.05, and power of test of 0.8. The expected differences in SBP and DBP between the intervention and control group were 10 and 6 mm Hg, respectively. 16 Based on this, we determined that a total 80 participants (40 in each group) would be required.
2.4. Study protocol
2.4.1. Randomization
After giving informed consent, participants were randomized into either the intervention group (foot reflexology group) or the control group using computer‐generated block randomization (block of four [1:1]; Figure 1). Non‐team members performed the randomization, and investigators involved in enrolling participants had no access to the randomization lists. Randomization numbers were kept in opaque, sealed envelopes, which were selected and opened by the treatment investigators after history taking and physical examination of the patients. Treatment investigators and participants knew the results of the randomization, but the investigator responsible for statistical analysis was blinded.
FIGURE 1.
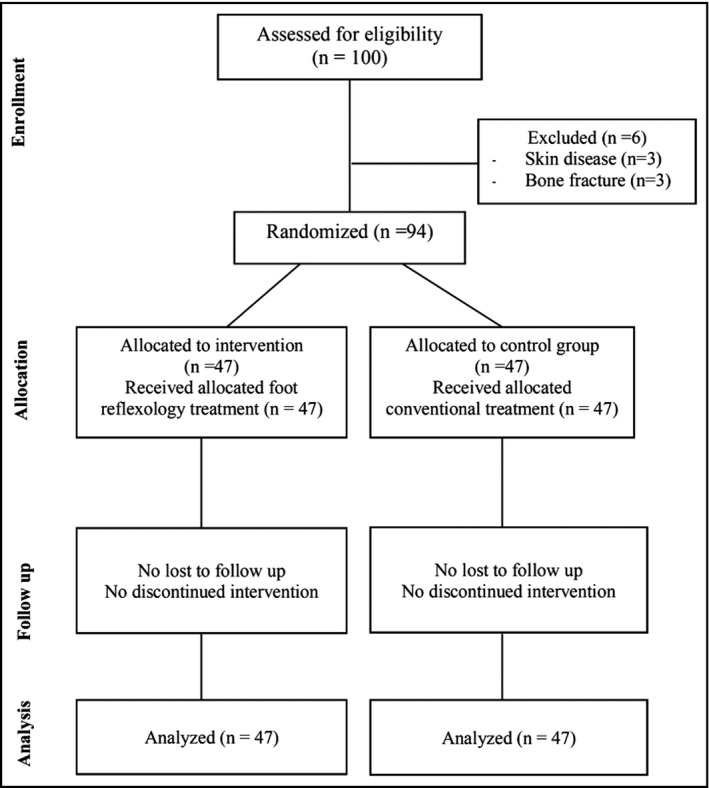
CONSORT flow diagram. Flow diagram of the progress through the phases of the parallel‐randomized trial
2.4.2. Foot reflexology
Foot reflexology was performed in all participants in the intervention group after they had rested for 5 min in a sitting position. In all cases, the procedure was performed by the same researcher, who was trained and certified by the Ministry of Public Health's Department of Thai Traditional and Alternative Medicine. Acupressure was applied at the plantar side of the right foot at the first metatarsal bone, around 1–1.5 cm proximal to the first metatarsophalangeal joint (Figure 2). Approximately 3 kg of pressure was applied using a knuckle of the right index finger (dorsal part of the proximal interphalangeal joint in a flexing position) in a perpendicular manner and held for 15 s then released for 5 s. This hold‐release cycle was performed five times over the total course of 2 min. The Department of Thai Traditional and Alternative Medicine recommends this method in accordance with zone and meridian theories. 14
FIGURE 2.
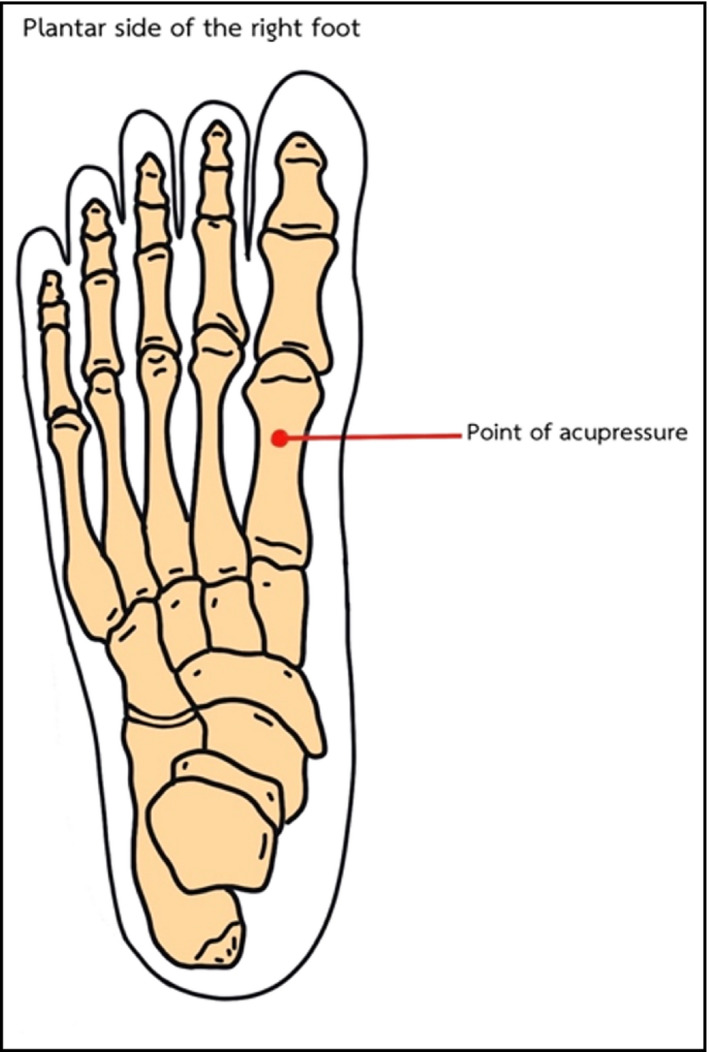
Location of foot reflexology used in the present study. Acupressure was applied at the plantar side of right foot at the first metatarsal bone, around 1–1.5 cm proximal to the first metatarsophalangeal joint
2.4.3. Conventional treatment
Participants in the intervention and the control group received the same conventional treatment, including anti‐HT drugs, according to standard HT guidelines. 4 At the end of the follow‐up visit, all participants were instructed to adhere to their drugs and encouraged to lead healthy lifestyles including salt restriction, regular exercise, and healthy diets.
2.4.4. BP and HR measurements
Each patient's BP level at first HT diagnosis was retrieved from electronic medical records (Health Object, Srinagarind Hospital) in order to assess their eligibility. After enrollment, office BP and HR were measured by a nurse at baseline (0 min) and again at 15 and 30 min after foot reflexology in the intervention group and after resting in a quiet room in the control group. A validated, FDA‐approved automatic BP device (DINAMAP Pro 300, GE healthcare) with the appropriate cuff size for the patient's arm circumference was used for all measurements. Two BP measurements were taken at 2‐min intervals, and the average BP and HR were recorded for analysis.
2.5. Adverse event monitoring
All participants were instructed to immediately report any adverse events occurring after enrollment and during the study period. Participants with life‐threatening adverse events (as determined by the treatment investigators) were withdrawn prematurely from the study for safety reasons.
2.6. Statistical analysis
All analyses were based on the intention‐to‐treat principle. Baseline characteristics were shown as mean ± standard deviation (SD) or percentage (%). A paired t test was used to compare SBP, DBP, and HR at baseline and at 15 and 30 min after acupressure in the intervention group and after resting in the control group. A general estimating equation (GEE) was used to compare SBP, DBP, and HR between the two randomized groups. A probability value of <.05 was considered statistically significant. All statistical analyses were performed using STATA version 10.1 (registered to Khon Kaen University).
3. RESULTS
A total of 100 participants were enrolled, 94 of whom were included in the final analysis (47 participants in each group). Of the six who were excluded, three had skin diseases of the feet and three had a history of metatarsal bone fractures (Figure 1). The mean age was 57.5 ± 8.5 years in the intervention group and 56.0 ± 8.5 years in the control group. In both groups, the majority of participants were women: 70.2% and 72.3% in the intervention and control group, respectively. Participants in the two groups had similar marital status, smoking and drinking habits, underlying diseases, and family history of HT (Table 1). Regarding the type of anti‐HT drugs, participants in both groups received comparable calcium channel blockers (CCB) and angiotensin‐converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB), but participants in the control group received more beta‐adrenergic blockers (12.8% vs 4.3%) and diuretics (8.5% vs 2.1%) compared with the intervention group (Table 1). Baseline office SBP and DBP in the reflexology and the control groups were comparable (SBP: 139.0 and 136.3 mm Hg, respectively, and DBP: 81.2 and 80.8 mm Hg, respectively; all p > .05). However, baseline HR in the foot reflexology group was moderately lower than in the control group (76.5 bpm vs 81.4 bpm; p = .113; Table 2).
TABLE 1.
Baseline characteristics
| Measures | Foot reflexology group (n = 47) | Control group (n = 47) |
|---|---|---|
| Age, y (mean ± SD) | 57.5 ± 8.5 | 56.0 ± 8.5 |
| Female, % | 72.3 | 70.2 |
| Body mass index, kg/m2 (mean ± SD) | 24.7 ± 3.5 | 24.3 ± 3.6 |
| Occupation, n (%) | ||
| Farmer | 3 (6.4) | 0 |
| Merchant | 6 (12.7) | 10 (21.3) |
| Homemaker | 9 (19.2) | 6 (12.7) |
| Self‐employed | 4 (8.5) | 7 (14.9) |
| Government officer | 16 (34.0) | 15 (31.9) |
| No occupation | 9 (19.2) | 9 (19.2) |
| Marital status, n (%) | ||
| Single | 6 (12.7) | 6 (12.7) |
| Married | 34 (72.3) | 34 (72.3) |
| Divorced | 7 (14.9) | 7 (14.9) |
| Current smoker, n (%) | 9 (19.1) | 8 (17.0) |
| Alcohol consumption, n (%) | 7 (14.9) | 6 (12.7) |
| Family history of hypertension, n (%) | 30 (63.8) | 27 (57.4) |
| Diabetes, n (%) | 12 (25.5) | 11 (23.4) |
| Hyperlipidemia, n (%) | 25 (53.2) | 23 (48.9) |
| Type of anti‐hypertensive drugs, n (%) | ||
| Calcium channel blockers | 30 (63.8) | 32 (68.1) |
| ACEI/ARB | 32 (68.1) | 31 (66.0) |
| Beta‐adrenergic blockers | 2 (4.3) | 6 (12.8) |
| Diuretics | 1 (2.1) | 4 (8.5) |
| No. of anti‐hypertensive drugs, n (%) | ||
| 1 | 18 (38.3) | 23 (48.9) |
| 2 | 28 (59.6) | 23 (48.9) |
| ≥3 | 1 (2.1) | 1 (2.1) |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitors; ARB, angiotensin receptor blockers; No, number.
TABLE 2.
Comparison of systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) between the foot reflexology and control groups
| Foot reflexology | Control | p | |
|---|---|---|---|
| SBP | |||
| Difference in change (95% CI) | −2.68 (−2.60 to 7.96) | .320 a | |
| Baseline, mean (95% CI) | 139.0 (135.5 to 142.6) | 136.3 (132.2 to 140.5) | .959 b |
| After 15 min, mean (95% CI) | 132.3 (128.3 to 136.3) | 136.5 (132.1 to 140.8) | .466 b |
| After 30 min, mean (95% CI) | 130.6 (126.7 to 134.5) | 138.4 (134.3 to 142.5) | .017 b |
| DBP | |||
| Difference in change (95% CI) | −0.49 (−3.27 to 4.25) | .798 a | |
| Baseline, mean (95% CI) | 81.3 (78.5 to 84.0) | 80.8 (78.0 to 83.5) | >.999 b |
| After 15 min, (95% CI) | 78.6 (75.9 to 81.4) | 80.0 (77.4 to 82.5) | >.999 b |
| After 30 min, (95% CI) | 77.9 (75.0 to 80.8) | 81.0 (78.6 to 83.4) | .295 b |
| HR | |||
| Difference in change (95% CI) | −4.96 (−9.63 to −0.28) | .038 a | |
| Baseline, mean (95% CI) | 76.5 (73.3 to 79.6) | 81.4 (77.6 to 85.2) | .113 b |
| After 15 min, mean (95% CI) | 73.9 (70.8 to 77.0) | 80.6 (76.9 to 84.3) | .015 b |
| After 30 min, mean (95% CI) | 72.4 (69.6 to 75.3) | 79.6 (75.7 to 83.5) | .008 b |
Using the generalized estimating equations (GEE) model.
Pairwise comparison of between group contrasts (Bonferroni).
In the reflexology group, SBP, DBP, and HR decreased significantly from baseline after intervention, with mean differences of −3.29 mm Hg (95% CI; −5.64 to −0.93), −1.71 mm Hg (95%CI; −3.11 to −0.32), and −1.71 bpm (95% CI; −2.88 to −0.54), respectively, at 15 min and −3.18 mm Hg (95% CI; −5.57 to −0.79), −1.55 mm Hg (95%CI; −2.97 to −0.14), and −2.94 bpm (95% CI; −3.98 to −1.90), respectively, at 30 min (Figure 3). In the control group, there were no significant differences from baseline at 15 min after resting, but SBP and HR had decreased significantly after 30 min, with mean differences of −2.04 mm Hg (95%CI; −4.07 to −0.18), and −1.83 bpm (95% CI; −3.25 to −0.41), respectively. The mean difference in DBP at 30 min was not statistically significant (−0.23 mm Hg; 95%CI; −0.88 to 2.00; Figure 3).
FIGURE 3.
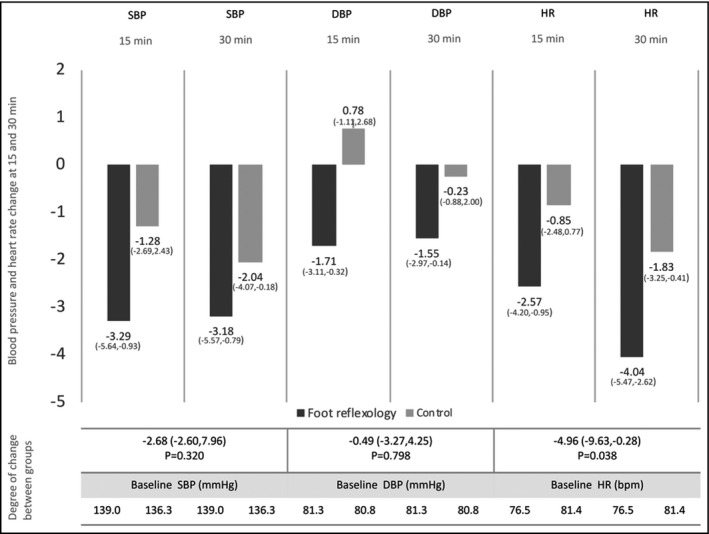
Blood pressure (BP) and heart rate (HR) change in the foot reflexology and control groups and comparison of the degree of BP and HR change between groups. At 15 and 30 min after the intervention, systolic BP (SBP), diastolic BP (DBP), and HR had significantly decreased from baseline in the foot reflexology group. In the control group, there was no significant difference in SBP, DBP, or HR at 15 min, but at 30 min, SBP and HR had decreased significantly. Overall, SBP and DBP at the end of the study in the foot reflexology group were lower than in the control group, but this difference was not statistically significant. However, HR in the foot reflexology group was significantly lower than in the control group. Abbreviations:95% CI, 95% confidence interval; bpm, beats per minute; mm Hg, millimeter of mercury
Comparison between the two groups using the GEE showed that overall SBP and DBP at the end of the study in the foot reflexology group were lower than in the control group: −2.68 mm Hg (95%CI; −2.60 to 7.96) and −0.49 mm Hg (95%CI; −3.27 to 4.25), respectively. However, these differences were not statistically significant. Interestingly, HR in the foot reflexology group was significantly lower than in the control group, with a difference of −4.96 bpm (95%CI; −9.63 to −0.28; Table 2, Figure 3).
4. DISCUSSION
Hypertension is a leading cause of major cardiovascular events and disability‐adjusted life years in many populations, 1 and early administration of anti‐HT drugs is recommended for BP control in stage‐2 HT patients. 4 However, previous trials have reported low adherence to medication in more than half of treated HT patients, partly due to the presence of intolerable side effects. 23 , 24 This suggests that integrative treatment including non‐pharmacological therapies may be beneficial. This study found that foot reflexology was effective in lowering HR in stage‐2 HT patients, as demonstrated by the significant difference in the degree of HR reduction between the intervention and control group. We also observed decreases in both SBP and DBP, but these differences were not statistically significant.
Although this and previous studies have found that foot reflexology can lower BP, results have been inconsistent. An RCT in Taiwan, for example, found that patients who received acupressure at the Taichong point (dorsum of the right foot, at the distal hallow of the junction between the first and second metatarsal bone) exhibited significant reductions in SBP and DBP at 15 and 30 min compared with controls. 16 However, another clinical study in Korean essential‐HT patients (nonequivalent control group, pretest‐posttest design) showed that foot reflexology lowered SBP but not DBP. 18 These discrepancies might be explained by slight differences in reflexology technique across studies (eg, location of the acupressure point, intensity applied, and duration of the procedure). Further clinical studies should thus be conducted compare techniques and determine the most beneficial acupressure point, intensity, and duration for BP and HR reduction.
Although the mechanism behind foot reflexology's ability to lower HR is unclear, it may be similar to that of acupuncture. Although unlike acupuncture, acupressure does not involve the subdermal insertion, pressure is applied at the same points. Meridian theory in traditional Chinese medicine describes the BP‐ and HR‐lowering mechanisms of acupuncture in terms of “Qi” which is believed to be a vital force forming part of any living entity. 14 Acupuncture targets the points of the human body that are responsible for the regulation of vital energy, 14 and puncturing or applying pressure to the Taichong point of the foot allows Qi to flow smoothly, thereby lowering BP. 14 , 25 , 26 Another possible mechanism involves the ability of these techniques to induce relaxation. Some studies conducted in elderly and cardiovascular disease patients, for example, found foot reflexivity to be effective in relieving anxiety, 27 , 28 which decreased BP and HR as observed in the present study.
Blood pressure levels and variability are important parameters for predicting a poor outcomes in cardiovascular patients, 29 and HR is an essential factor in the assessment and treatment of HT patients, especially those with co‐morbidities such as heart failure or myocardial infarction. Elevated BP and HR in these patients are associated with increased risk for cardiovascular complications but are, fortunately, correctable. 30 , 31 , 32 Foot reflexology requires only around 2 min per session and is can be easily performed by anyone who is properly trained. In addition, if performed regularly at home by the patient, it may result in long‐term improvements in BP, HR, and cardiovascular outcomes. However, further studies are required to determine the long‐term benefits of foot reflexology.
The strength of the present study was that we measured SBP, DBP, and HR, whereas most previous studies focused only on BP. Second, this was an RCT, which limited the possibility of selection bias. Third, we standardized the technique and intensity of the procedure by assigning only one certified nurse to perform the intervention. However, our study also had some limitations. Although HR after acupressure in the intervention group was significantly lower than in the control group, average baseline HR in the intervention group was 5 bpm lower than in controls. This difference was not statistically significant; however, care should be taken when interpreting our results since the different starting points might limit the comparability. Another limitation was that this study measured the short‐term effects of foot reflexology based on office BP, which made it difficult to control for the white‐coat effect. Home BP monitoring (HBPM) or ambulatory BP monitoring (ABPM) have greater correlation with future CV events than office BP, as they represent BP absent the external stress of the hospital environment. 33 , 34 We suggest that further studies should measure HBPM or ABPM rather than office BP. Furthermore, our data were obtained from Thai participants and may thus not be generalizable to patients of other ethnicities or cultural backgrounds. Finally, lifestyle‐related data, such as salt intake, exercise, anxiety, and stress, were not collected or analyzed.
5. CONCLUSION
Foot reflexology was effective in reducing HR in stage‐2 HT patients and was partially effective in reducing BP. It is noninvasive and can be performed in a short period of time as a complimentary therapy.
CONFLICT OF INTEREST
K. Kario has received research grants from Teijin Pharma Limited, Novartis Pharma KK, Takeda Pharmaceutical Co., Ltd., Omron Healthcare Co., Ltd., Fukuda Denshi, and honoraria from Mochida Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd. The other authors report no conflict of interest.
AUTHOR CONTRIBUTIONS
Praew Kotruchin: Conceived and designed the analysis; Performed the analysis; Wrote the paper. Supap Imoun: Collected the data; Contributed data. Thapanawong Mitsungnern: Collected the data. Patcharin Aountrai: Collected the data. Maneenuch Domthaisong: Collected the data. Kazuomi Kario: Helped supervise the project and manuscript.
ACKNOWLEDGMENTS
The authors would like to express our sincere gratitude to the HOPE ASIA Network for their recommendations on HT management and research opportunities, as well as to the patients and staff at the Khon Kaen University Hypertensive Crisis Clinic (Faculty of Medicine Department of Emergency Medicine) for their participation. We would also like to acknowledge Dr Dylan Southard for editing this manuscript via the KKU Publication Clinic (Thailand).
REFERENCES
- 1. Canto JG, Iskandrian AE. Major risk factors for cardiovascular disease: debunking the only 50% myth. JAMA. 2003;290:947‐949. [DOI] [PubMed] [Google Scholar]
- 2. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013;133:1‐8. [PubMed] [Google Scholar]
- 3. Aekplakorn W, Sangthong R, Kessomboon P, et al. Changes in prevalence, awareness, treatment and control of hypertension in Thai population, 2004–2009: Thai National Health Examination Survey III–IV. J Hypertens. 2012;30:1734‐1742. [DOI] [PubMed] [Google Scholar]
- 4. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;2017:24430. [DOI] [PubMed] [Google Scholar]
- 5. Kario K, Park S, Chia YC, et al. 2020 Consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:351‐362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Palatini P, Dorigatti F, Zaetta V, et al. Heart rate as a predictor of development of sustained hypertension in subjects screened for stage 1 hypertension: the HARVEST Study. J Hypertens. 2006;24:1873‐1880. [DOI] [PubMed] [Google Scholar]
- 7. Julius S, Palatini P, Kjeldsen SE, et al. Usefulness of heart rate to predict cardiac events in treated patients with high‐risk systemic hypertension. N Am J Cardiol. 2012;109:685‐692. [DOI] [PubMed] [Google Scholar]
- 8. Williams B, Lacy PS, CAFE and the ASCOT (Anglo‐Scandinavian Cardiac Outcomes Trial) Investigators . Impact of heart rate on central aortic pressures and hemodynamics: analysis from the CAFE (Conduit Artery Function Evaluation) study: CAFE‐Heart Rate. J Am Coll Cardiol. 2009;54:705‐713. [DOI] [PubMed] [Google Scholar]
- 9. Teeäär T, Serg M, Paapstel K, et al. Atenolol's inferior ability to reduce central vs peripheral blood pressure can be explained by the combination of its heart rate‐dependent and heart rate‐independent effects. Int J Hypertens. 2020;2020:4259187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization , ed. WHO Global Report on Traditional and Complementary Medicine, 2019. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 11. Im‐oun S, Kotruchin P, Thinsug P, Mitsungnern T, Techa‐atik P, Pongchaiyakul C. Effect of Thai instrumental folk music on blood pressure: a randomized controlled trial in stage‐2 hypertensive patients. Complement Ther Med. 2018;39:43‐48. [DOI] [PubMed] [Google Scholar]
- 12. Nahas R. Complementary and alternative medicine approaches to blood pressure reduction: an evidence‐based review. Can Fam Physician. 2008;54:1529‐1533. [PMC free article] [PubMed] [Google Scholar]
- 13. Fan H, Lu F, Yang A, Dong Y, Liu P, Wang Y. A Review on the nonpharmacological therapy of traditional Chinese medicine with antihypertensive effects. Evid Based Complement Alternat Med. 2019;2019:1317842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang J, Xiong X. Evidence‐based Chinese medicine for hypertension. Evid Based Complement Alternat Med. 2013;2013:978398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Embong NH, Soh YC, Ming LC, Wong TW. Revisiting reflexology: concept, evidence, current practice, and practitioner training. J Tradit Complement Med. 2015;5:197‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lin G‐H, Chang W‐C, Chen K‐J, Tsai C‐C, Hu S‐Y, Chen L‐L. Effectiveness of acupressure on the taichong acupoint in lowering blood pressure in patients with hypertension: a randomized clinical trial. Evid Based Complement Alternat Med. 2016;2016:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Elshamy K, Elsafety E. Effect of nursing intervention using foot reflexology on blood pressure and quality of life of hypertensive patients at Mansoura University: preliminary results. Med J Cairo Univ. 2011;79(2). http://erepository.cu.edu.eg/index.php/MJCU/article/view/858. Accessed August 1, 2020 [Google Scholar]
- 18. Park H‐S, Cho G‐Y. Effects of foot reflexology on essential hypertension patients. Taehan Kanho Hakhoe Chi. 2004;34:739‐750. [DOI] [PubMed] [Google Scholar]
- 19. Jirayingmongkol P, Chantein S, Phengchomjan N, Bhanggananda N. The effect of foot massage with biofeedback: a pilot study to enhance health promotion. Nurs Health Sci. 2002;4:A4. [Google Scholar]
- 20. Özdelikara A, Tan M. The effect of reflexology on chemotherapy‐induced nausea, vomiting, and fatigue in breast cancer patients. Asia Pac J Oncol Nurs. 2017;4:241‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Polat H, Ergüney S. The effect of reflexology applied to patients with chronic obstructive pulmonary disease on dyspnea and fatigue. Rehabil Nurs. 2017;42:14‐21. [DOI] [PubMed] [Google Scholar]
- 22. Department of Thai Traditional and Alternative Medicine, Ministry of Public Health . Foot Reflexology. Division of Complementary and Alternative Medicine Website. February 2, 2018. https://thaicam.go.th/foot‐reflexology/. Accessed August 1, 2020.
- 23. Michel B, Egan BM. Adherence in hypertension. Circ Res. 2019;124:1124‐1140. [DOI] [PubMed] [Google Scholar]
- 24. Devkota S, Dhungana RR, Pandey AR, et al. Barriers to treatment and control of hypertension among hypertensive participants: a community‐based cross‐sectional mixed method study in municipalities of Kathmandu, Nepal. Front Cardiovasc Med. 2016;3:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wu HL, Li XQ, Wang X. The immediate effect on blood pressure of acupuncture at Taichong (LR 3) in 65 cases of hypertension patient with hyperactivity of liver‐yang. J Tradit Chin Med. 2008;49:622‐624. [Google Scholar]
- 26. Xiong X, Yang X, Liu W, Chu F, Wang P, Wang J. Trends in the treatment of hypertension from the perspective of traditional Chinese medicine. Evid Based Complement Alternat Med. 2013;2013:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chamberlain AM, Vickers KS, Colligan RC, Weston SA, Rummans TA, Roger VL. Associations of preexisting depression and anxiety with hospitalization in patients with cardiovascular disease. Mayo Clin Proc. 2011;86:1056‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bahrami T, Rejeh N, Heravi‐Karimooi M, Tadrisi SD, Vaismoradi M. The effect of foot reflexology on hospital anxiety and depression in female older adults: a randomized controlled trial. Int J Ther Massage Bodywork. 2019;12:16‐21. [PMC free article] [PubMed] [Google Scholar]
- 29. Kario K, Chirinos JA, Townsend RR, et al. Systemic hemodynamic atherothrombotic syndrome (SHATS) ‐ coupling vascular disease and blood pressure variability: proposed concept from Pulse of Asia. Prog Cardiovasc Dis. 2020;63:22‐32. [DOI] [PubMed] [Google Scholar]
- 30. Kannel W, Kannel C, Paffenbarger R, Cupples A. Heart rate and cardiovascular mortality: the Framingham study. Am Heart J. 1987;113:1489‐1494. [DOI] [PubMed] [Google Scholar]
- 31. Gillman M, Kannel W, Belanger A, D'Agostino R. Influence of heart rate on mortality among persons with hypertension: the Framingham study. Am Heart J. 1993;125:1148‐1154. [DOI] [PubMed] [Google Scholar]
- 32. Singh B. Increased heart rate as a risk factor for cardiovascular disease. Eur Heart J Suppl. 2003;5:G3‐G9. [Google Scholar]
- 33. Stergiou GS, Bliziotis IA. Home blood pressure monitoring in the diagnosis and treatment of hypertension: a systematic review. Am J Hypertens. 2011;24:123‐134. [DOI] [PubMed] [Google Scholar]
- 34. Kario K, Hoshide S, J‐HOP Study Group . Sleep blood pressure self‐measured at home as a novel determinant of organ damage: Japan Morning Surge Home Blood Pressure (J‐HOP) study. J Clin Hypertens (Greenwich). 2015;17:340‐348. [DOI] [PMC free article] [PubMed] [Google Scholar]


