Abstract
Facial injuries remain a significant source of morbidity in trauma. Due to the variety and unpredictable patterns of injuries associated with either blunt or ballistic mechanisms, advanced diagnostic imaging and complex management options are necessary. Multidisciplinary collaboration is essential to optimize the care of craniomaxillofacial trauma.
Introduction
Facial trauma can encompass skin, muscles, nerves, blood vessels, and bones. There can be a combination of those structures and range from simple to complex. About one-third of facial fractures have concomitant soft tissue trauma. The precise incidence and epidemiology of facial trauma is dependent on demographic factors such as socioeconomic status, age, gender, and mechanism of injury. Furthermore, it can be confounded by underreporting and treatment of these injuries. Facial fractures alone presenting to the emergency room is around half-a-million per year in the United States.1 We know that these types of injuries occur more in young males than females, and are most frequently the result of accidents, assaults, falls, and motor vehicle collisions (MVC).2 Despite mandatory implementation of airbags and seatbelts, MVCs remain the most significant cause of facial trauma all over the world. Facial trauma needs to be performed in a holistic and multidisciplinary setting as there can be multiple associated injuries. Fractures of the skull, intracranial injuries (10%), cervical spine injury, and upper extremity injuries are not uncommon.1,3 A collaboration between plastic surgery and the multiple surgical, medical and radiologic subspecialties is critical to patient care and recovery.
Mechanisms of Facial Injury
Two broad categories of facial injury mechanisms include blunt versus ballistic. Two case examples are presented to compare and contrast what may be required to manage these types of trauma.
Case 1
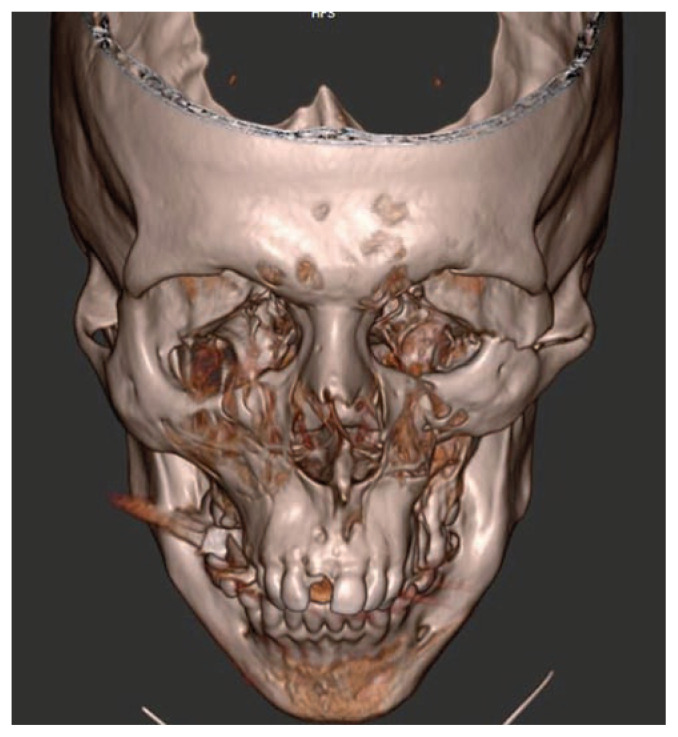
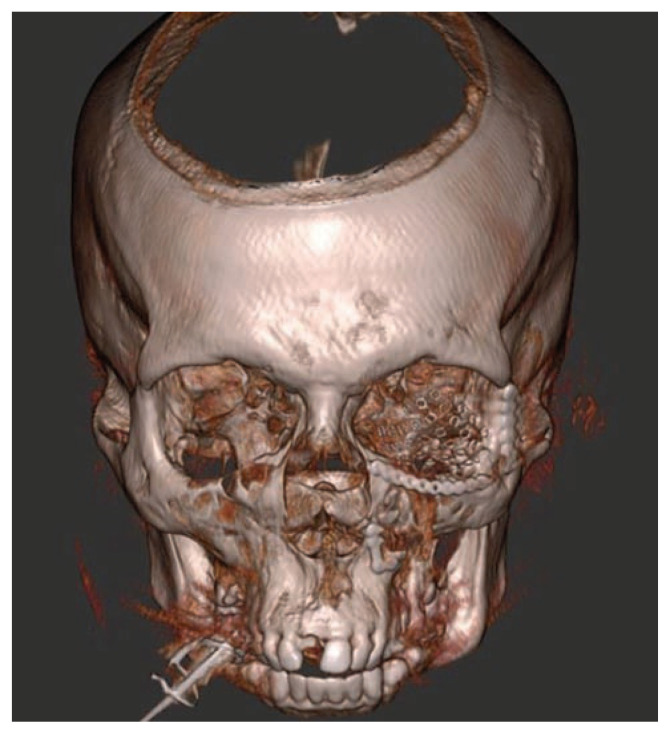
A young male was assaulted with a fist resulting in cheek depression. Additionally, he felt that his teeth did not fit together appropriately. After a thorough evaluation by emergency medicine, trauma surgery, plastic surgery, and ophthalmology, the patient underwent a craniomaxillofacial CT scan. The facial bones are organized into units that can break in relatively predictable patterns when subjected to blunt forces (e.g., falls, assault, MVC). The images were 3D reconstructed revealing displaced fractures to his left orbital floor and a depressed zygomatico-maxillary-complex (ZMC) fracture (Figure 1). His injuries required surgery, but he had no other injuries and was discharged home safely on a soft diet and did not require any antibiotics.4 Several days later, the patient underwent operative reduction and internal fixation with plates and screws of his orbit and ZMC fractures. Optimal reduction of these fractures is essential to vision, facial function, and form. To aid with this three-dimensional process, we utilize an intra-operative O-arm (Medtronic. Minneapolis, MN). CT scan is used to obtain images after the surgery but before the patient is woken up from surgery (Figure 2). It allows us to confirm the places of the implants, plates, and screws and the opportunity to re-adjust as necessary during a single operation. Figure 3 shows the 3D reconstructed picture of the intra-operative CT scan after fracture reduction and fixation with orbital floor implant, plates and screws (Stryker. Kalamazoo, MI).
Figure 1.
A three-dimensional reconstructed image of the craniomaxillofacial CT scan showing left orbital floor fracture zygomatico-maxillary-complex fracture.
Figure 2.
Intraoperative use of the O-arm CT scanner (Medtronic. Minneapolis, MN). A craniomaxillofacial CT scan takes about two minutes and allows for immediate feedback of fracture reduction and hardware placement.
Figure 3.
A three-dimensional reconstructed image of the intra-operative CT scan showing adequate fracture reduction and placement of left orbital floor implant and hardware fixation.
The use of imaging technology in evaluating, planning, and management of complex facial injuries is evolving into the standard. Pre-operative CT scan are the gold standard for diagnosing facial fractures and are widely used in the post-operative setting to confirm repair.5–7 With advancements in equipment, CT scanners are now more portable and less costly and produce high-quality images. Intraoperative CT is a powerful tool to evaluating bony anatomy and has been used by surgeons to assess the skull, skull base, and spine, and is becoming increasingly accessible.8 The literature supports the routine use of intraoperative CT for orbital, pan-facial, and complex ZMC, LeFort, and naso-orbital-ethmoidal fractures.9
Case 2
A young woman suffered a gunshot wound to the mandible that resulted in a severely displaced and comminuted fracture. The pre-operative 3D CT reconstruction showed multiple fragments of her anterior mandible (Figure 4). After being deemed safe for surgery by multiple surgical specialists, the patient was taken to the operating room for initial debridement of devitalized tissue and repair of as many disrupted structures as possible. At the end of this surgery, it was apparent that standard bony fracture reduction and fixation with plates and screws would not be feasible or optimal for patient recovery.
Figure 4.
A three-dimensional reconstructed image of the pre-operative CT scan showing displace and comminuted fracture of the anterior mandible after a ballistic injury.
A team consisting of industry (Stryker. Kalamazoo, MI), engineers (3D Systems. Rock Hill, SC) and plastic surgeons with training in craniofacial surgery and microsurgical reconstructive surgery was assembled to tackle this problem. Through virtual surgical planning (VSP) using pre-operative CT scans of the face and lower extremities, a segment of the patient’s fibula was shaped into a new mandible to reconstruct what she was missing (Figure 5). In a subsequent operation, this bone from her leg was brought with its blood supply and connected to her facial blood vessels as a vascularized free-fibular flap (Figure 6). Once this was accomplished, the patient had a complete mandible with which she could resume eating and speaking normally again without any significant impact to her ability to walk.
Figure 5.
Virtual surgical planning rendering by 3D Systems (Rock Hill, SC) showing vascularized free fibular bone flap in reconstruction of missing mandible.
Figure 6.
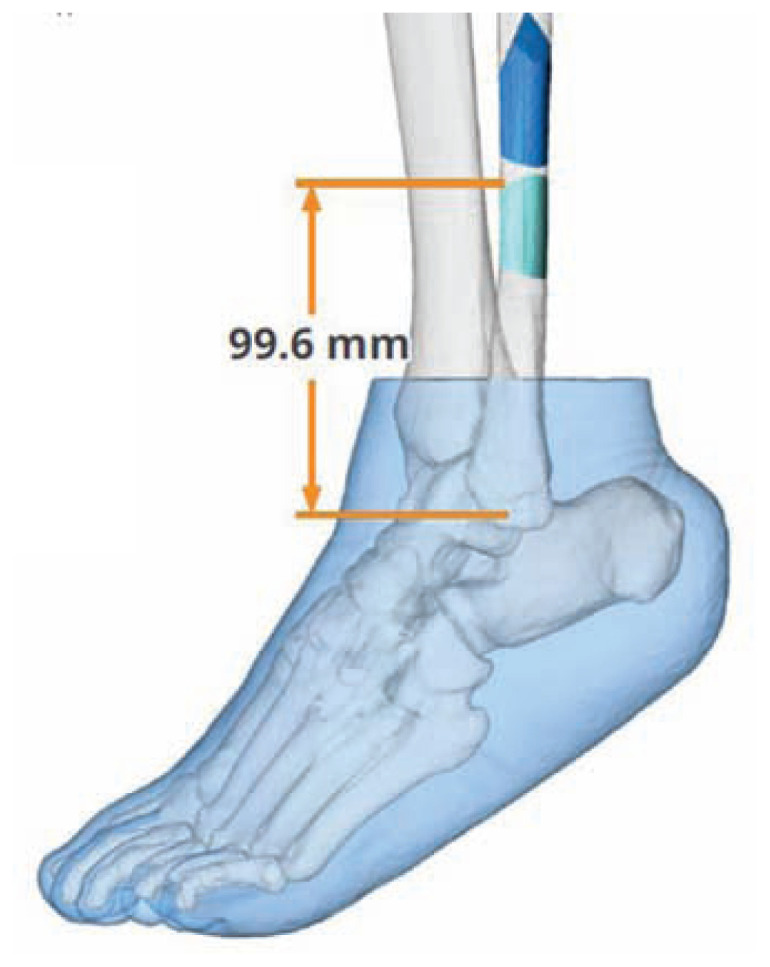
Virtual surgical planning rendering by 3D Systems (Rock Hill, SC) showing precise harvest and bony cuts in the fibula.
Ballistic injury to the face presents a unique and challenging dilemma for the surgeon. There can be significant and unpredictable disruption of normal anatomy planes of soft tissue and bone. Much of what we know about management of ballistic and blast injuries come from military combat. Identifying the problem and restoring form and function with good support structures and healthy soft tissue coverage as close to the time of injury are the core principles.
Sequencing and execution of the different operations by a multidisciplinary team in craniofacial microsurgical reconstruction following trauma is complex. These cases test the surgeon’s technical and creativity abilities to optimize functional and aesthetic outcomes. A wide variety of free flap options exist for reconstructing facial defects, each with their own unique strengths and limitations. This patient with a large mandibular defect was reconstructed with a free fibular flap. Hidalgo first described this flap in mandibular reconstruction over three decades ago and it still remains one of the most commonly used for its reliability and versatility.10 The free fibular flap provides quality bone stock and can be harvested with different tissues (e.g. muscle, fascia, skin). It is limited by the patient’s own bone length, pedicle length, and potential for leg weakness and ankle instability.11
Computer-assisted surgery started in the 1980s and has since become increasingly integrated into complex craniomaxillofacial reconstruction.12,13 Virtual surgical 3D simulation and planning has many advantages (i.e. analysis, planning, virtual surgery, printout of guides or implants, verification of actual to planned results).14 Despite these, it should be stressed that technology cannot replace a surgeon’s clinical judgement or technique.
Conclusion
Future directions for technology and craniofacial surgery entail achieving greater precision and accuracy in the actual surgical procedure. Collaboration between experts within plastic surgery provides greater breadth of experience and better care and outcomes for patients.
Footnotes
Dennis C. Nguyen, MD, MS, is in the Division of Plastic and Reconstructive Surgery, Washington University, St. Louis, Missouri.
Disclosure
None reported.
References
- 1.Allareddy V, Allareddy V, Nalliah RP. Epidemiology of facial fracture injuries. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2011;69(10):2613–2618. doi: 10.1016/j.joms.2011.02.057. [DOI] [PubMed] [Google Scholar]
- 2.VandeGriend ZP, Hashemi A, Shkoukani M. Changing trends in adult facial trauma epidemiology. The Journal of craniofacial surgery. 2015;26(1):108–112. doi: 10.1097/SCS.0000000000001299. [DOI] [PubMed] [Google Scholar]
- 3.Mithani SK, St-Hilaire H, Brooke BS, Smith IM, Bluebond-Langner R, Rodriguez ED. Predictable patterns of intracranial and cervical spine injury in craniomaxillofacial trauma: analysis of 4786 patients. Plastic and reconstructive surgery. 2009;123(4):1293–1301. doi: 10.1097/PRS.0b013e31819e26f2. [DOI] [PubMed] [Google Scholar]
- 4.Linkugel AD, Odom EB, Bavolek RA, Snyder-Warwick AK, Patel KB. Systemic Preoperative Antibiotics with Mandible Fractures: Are They Indicated at the Time of Injury? Craniomaxillofac Trauma Reconstr. 2018;11(1):35–40. doi: 10.1055/s-0037-1603458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyette JR, Pemberton JD, Bonilla-Velez J. Management of orbital fractures: challenges and solutions. Clin Ophthalmol. 2015;9:2127–2137. doi: 10.2147/OPTH.S80463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marinho RO, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral and maxillofacial surgery clinics of North America. 2013;25(4):617–636. doi: 10.1016/j.coms.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Manson PN, Markowitz B, Mirvis S, Dunham M, Yaremchuk M. Toward CT-based facial fracture treatment. Plastic and reconstructive surgery. 1990;85(2):202–212. discussion 213–204. [PubMed] [Google Scholar]
- 8.Schichor C, Terpolilli N, Thorsteinsdottir J, Tonn JC. Intraoperative Computed Tomography in Cranial Neurosurgery. Neurosurgery clinics of North America. 2017;28(4):595–602. doi: 10.1016/j.nec.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Cuddy K, Khatib B, Bell RB, et al. Use of Intraoperative Computed Tomography in Craniomaxillofacial Trauma Surgery. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2018;76(5):1016–1025. doi: 10.1016/j.joms.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plastic and reconstructive surgery. 1989;84(1):71–79. [PubMed] [Google Scholar]
- 11.Momoh AO, Yu P, Skoracki RJ, Liu S, Feng L, Hanasono MM. A prospective cohort study of fibula free flap donor-site morbidity in 157 consecutive patients. Plastic and reconstructive surgery. 2011;128(3):714–720. doi: 10.1097/PRS.0b013e318221dc2a. [DOI] [PubMed] [Google Scholar]
- 12.Vannier MW, Marsh JL, Warren JO. Three dimensional CT reconstruction images for craniofacial surgical planning and evaluation. Radiology. 1984;150(1):179–184. doi: 10.1148/radiology.150.1.6689758. [DOI] [PubMed] [Google Scholar]
- 13.Toth BA, Ellis DS, Stewart WB. Computer-designed prostheses for orbitocranial reconstruction. Plastic and reconstructive surgery. 1988;81(3):315–324. doi: 10.1097/00006534-198803000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Steinbacher DM. Three-Dimensional Analysis and Surgical Planning in Craniomaxillofacial Surgery. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2015;73(12 Suppl):S40–56. doi: 10.1016/j.joms.2015.04.038. [DOI] [PubMed] [Google Scholar]