Abstract
Because conducting population-based oral health screening is resource intensive, oral health data at small-area levels (e.g., county-level) are not commonly available. We applied the multilevel logistic regression and poststratification method to estimate county-level prevalence of untreated dental caries among children aged 6–9 years in the United States using data from the National Health and Nutrition Examination Survey (NHANES) 2005–2010 linked with various area-level data at census tract, county and state levels. We validated model-based national estimates against direct estimates from NHANES. We also compared model-based estimates with direct estimates from select State Oral Health Surveys (SOHS) at state and county levels. The model with individual-level covariates only and the model with individual-, census tract- and county-level covariates explained 7.2% and 96.3% respectively of overall county-level variation in untreated caries. Model-based county-level prevalence estimates ranged from 4.9% to 65.2% with median of 22.1%. The model-based national estimate (19.9%) matched the NHANES direct estimate (19.8%). We found significantly positive correlations between model-based estimates for 8-year-olds and direct estimates from the third-grade State Oral Health Surveys (SOHS) at state level for 34 states (Pearson coefficient: 0.54, P = 0.001) and SOHS estimates at county level for 53 New York counties (Pearson coefficient: 0.38, P = 0.006). This methodology could be a useful tool to characterize county-level disparities in untreated dental caries among children aged 6–9 years and complement oral health surveillance to inform public health programs especially when local-level data are not available although the lack of external validation due to data unavailability should be acknowledged.
Keywords: untreated dental caries, small area estimation, dental health surveys, dental public health surveillance, children
1. Introduction
Dental caries, if untreated, can lead to pain, infection, and problems in eating, speaking and learning (Griffin et al., 2014; US Department of Health and Human Services, 2000). Although the prevalence of untreated dental caries among US children has declined in the past decade, data from 2011–2012 indicate that 21.5% of children aged 6–9 years have untreated caries in primary or permanent teeth (US Department of Health and Human Services, 2010). Reducing the prevalence of untreated dental caries in the primary and permanent teeth among these children is a Healthy People (HP) 2020 objective (US Department of Health and Human Services, 2010).
As there is strong evidence for the effectiveness of dental sealants (Ahovuo-Saloranta et al., 2013) and topical fluoride in preventing caries (Marinho et al., 2013), increasing access to these interventions could reduce untreated caries. To effectively target these interventions, caries-prevention programs require information on children’s caries risk and access to dental care at the local level (e.g., county or school). Local data on children’s oral health are rarely available because conducting population-based oral health screening is resource intensive, requiring clinical examination by highly skilled and calibrated examiners and significant material and program support (Centers for Disease Control and Prevention, 2005).
Neither of the two data sources used to monitor caries – the National Health and Nutrition Examination Survey (NHANES) (Centers for Disease Control and Prevention) tracking national progress in reaching HP objectives (US Department of Health and Human Services, 2010) and the State Oral Health Surveys (SOHS) used to monitor state-level caries status (Centers for Disease Control and Prevention, 2015) – provides county level estimates of caries status across the United States.
Two studies have generated small-area estimates of oral health measures – one estimating county-level caries prevalence among third-grade children using the 1994 Washington SOHS (Leroux et al., 1996), and another estimating census block-level periodontitis prevalence among adults using 2009–2012 NHANES (Eke et al., 2016). These studies were limited by lack of either individual-level data (Leroux et al., 1996) or area-level covariates for their small area estimation (SAE) models (Eke et al., 2016). Recent publications highlight the importance of including individual-level and area-level factors (e.g., dental care use among low-income children and dentist shortage at state and county levels) to assess the complex multilevel influence on oral health measures (Fisher-Owens et al., 2007; Lin et al., 2012).
Recent studies applied a novel methodology known as multilevel regression and poststratification (MRP) to national health survey data to generate SAE of select health indicators (e.g., obesity, smoking) at state, county and census block levels (Zhang et al., 2015; Zhang et al., 2013). MRP has the advantage of allowing use of information from both individual-level data within the survey sample and from various area-level covariates external to the original sample. Therefore, MRP estimates reflect the multilevel influence of various factors on the health outcomes. The poststratification to Census population allows flexibility of SAE generated nationwide at different geographic levels and better accounts for demographic distribution at local levels (Gelman and Little, 1997; Zhang et al., 2014).
The aim of this study to apply the MRP approach to NHANES 2005–2010 linked with various area-level factors to estimate county-level prevalence of untreated dental caries among US children aged 6–9 years, nationwide.
2. Materials and methods
Our MRP approach followed three steps: model construction, model prediction and poststratification, and evaluation of model-based estimates.
Step 1: We used individual-level data from NHANES 2005–2010 linked with census tract-, county- and state-level data to construct and fit multilevel logistic regression models to estimate associations between untreated dental caries and factors at different levels.
Step 2: We applied the estimated model parameters to the Census population at census tract level by age, sex and race/ethnicity as well as their poverty and health insurance status via bootstrapping to estimate individual-level probability of untreated caries. This was then weighted using the population counts at census tract, county, state, or national level to estimate prevalence of untreated dental caries at the corresponding level.
Step 3: We performed internal validation at the national level between direct estimates from NHANES and model-based estimates for 6–9 year olds. We also conducted external comparisons between state- and county-level SAE for 8 year old children and direct estimates from select third-grade SOHS.
2.1. Primary data source
We used geocoded NHANES data 2005–2010 at the Research Data Center (RDC) of the National Center for Health Statistics (NCHS), which allows area-level data to be linked to individual-level NHANES data by census tract, county and state. Details about NHANES are described in Appendix A.
2.2. Study population
We included 2304 children aged 6–9 years with data for untreated caries lesions. The mean age was 7.5 years. The study population was almost equally distributed by sex and single year of age.
2.3. Outcome variable
Untreated dental caries was defined as a dichotomous variable, presence of at least one primary or permanent tooth with cavitated caries lesions (yes/no). NHANES 2005–2010 used the Basic Screening Examination (BSE), a simplified caries examination conducted by health technologists in 2005–2008 and dental hygienists in 2009–2010 (Centers for Disease Control and Prevention, 2005).
2.4. Individual-level covariates
We considered select socio-demographic variables (sex, age, race/ethnicity, poverty status, health insurance status, and survey cycles) from NHANES based on self-report by parents or guardians. Details of these covariates are described in Appendix B.
2.5. Census tract-, county- and state-level variables
We selected characteristics at various area levels based on the factors reported to have potential influence on children’s oral health and data availability (Fisher-Owens et al., 2007; Lin et al., 2012). Tract-level percentage of population in poverty was obtained from the 2006–2010 5-year American Community Survey (ACS) (US Census Bureau).
We obtained the following data at both the county and state levels from the Area Health Resources Files (Health Resources and Services Administration): percentage of population in poverty, 2006, 2007–2008, 2009–2010; percentage of population aged 25 + years with high school graduate or higher education, 2005–2010; percentage of children without health insurance, 2008, 2009–2010; percentages of children in individual race/ethnicity groups (Non-Hispanic white, Non-Hispanic black, Hispanic), 2005–2006, 2007–2008, 2009–2010; and dentist population ratio per 10,000 population, 2007, 2009–2010.
We also considered two state-level factors: percentage of children enrolled in Medicaid/Children’s Health Insurance Program (CHIP) receiving dental services in the past year (2005–2006, 2007–2008, 2009) from the Centers for Medicare & Medicaid Services’ CMS-416 reports (Centers for Medicare & Medicaid Services); percentage of population served by Community Water System receiving fluoridated water (2006, 2008, 2010) from biennial reports of the Centers for Disease Control and Prevention (CDC)’s Water Fluoridation Reporting System (Centers for Disease Control and Prevention, 2015). We categorized these area-level variables by quartiles. We used the 2006 NCHS 6-level urban-rural classification scheme for counties: large central metro, large fringe metro, medium metro, small metro, micropolitan, and non-core (Ingram and Franco, 2012).
2.6. Statistical analyses
First, we used NHANES 2005–2010 data linked with tract-, county- and state-level data to construct and fit multilevel logistic regression models to quantify associations between untreated caries and individual and area-level covariates. Details about the model building are described in Appendix C. The final model included sex, age, race/ethnicity, and insurance status at the individual level; poverty rate at the tract level; poverty rate, percentage of 25 + year olds with education level ≥ high school graduate, percentage of Hispanic children, dentist population ratio, and urban-rural classification at the county level; and percentage of Medicaid/CHIP enrolled children receiving dental services at the state level. We included county-level random effects to allow county-variation in the outcome and control unobserved heterogeneity. The multilevel regression models were fitted using SAS 9.3 (SAS Institute, NC) GLIMMIX procedure.
Second, we applied the estimated model parameters to census population data to predict individual-level probability of untreated dental caries given their sex, age, race/ethnicity, health insurance status, and area-level covariates. Child population counts at census tract-level by sex, single-year age and race/ethnicity were available from US Census 2010, but their corresponding health insurance status was unknown. Thus, we further applied a parametric bootstrapping approach to generate individual health insurance status using census tract-level percentages of children by health insurance status, 2008–2012 American Community Survey (ACS) (Zhang et al., 2016). Finally, population-weighted average of the estimated probability of untreated dental caries was generated at census tract level, which was further aggregated to county, state and national levels. We used the Monte Carlo simulation approach (Robert and Casela, 2004) to generate 1000 sets of model parameters and produce 1000 SAEs, which were used to generate final means, 2.5 and 97.5 percentiles (equivalent to 95% confidence intervals [CIs]) for the estimated county-level prevalence of untreated dental caries.
Finally, we compared model-based estimated prevalence of untreated caries at the national level with the direct estimate from NHANES. Although NHANES could not provide direct estimates below the national level that allow internal evaluation of the model-based estimates at state and county levels, we conducted exploratory external comparisons between model-based estimates at state and county levels limited to 8-year-olds and direct estimates from the third-grade SOHS. The Basic Screening Survey was the most common oral health examination protocol referred to by the third-grade SOHS (Centers for Disease Control and Prevention, 2015) and was similar to the BSE protocol used by NHANES 2005–2010. We used publicly available direct estimates and 95% CIs from the third-grade SOHS obtained from the websites of CDC and state health departments. We obtained state-level direct estimates for 34 states with SOHS conducted between 2005 and 2010 from the CDC website (Centers for Disease Control and Prevention, 2015). We obtained county-level direct estimates for 53 counties from the 2009–2011 New York SOHS, available on the New York state health department website (New York State Department of Health, 2016).
3. Results
3.1. Variation in model-based county-level estimates
The overall county-level variation in the estimated prevalence was significant (P = 0.004) (Table 1). The individual-level variables including age, sex, race/ethnicity and insurance status explained 7.2% of the overall county-level variation. Adding tract and county-level covariates explained the majority of the county-level variance (96.3%) and accordingly the county-level variance in untreated caries was no longer significant (P = 0.43). Fig. 1 depicts model-based county-level estimates of prevalence of untreated caries among children aged 6–9 years nationwide, using the final model. The map illustrates variation in the estimated prevalence across counties, ranging from 4.9% to 65.2% with a median of 22.1% and interquartile range of 14.7%.
Table 1.
Proportion (%) of county-level variance in prevalence of untreated caries explained by regression models at individual, tract, county, and state levels among US children aged 6–9 years, NHANES 2005–2010.
| Models | County-level variance | SE | P-value | % county-level variance explained |
|---|---|---|---|---|
| Null model | 0.173 | 0.065 | 0.004 | |
| Model 1 with individual-level variablesa | 0.160 | 0.062 | 0.005 | 7.2% |
| Model 2 with individual- and tract-level variablesb | 0.133 | 0.056 | 0.009 | 23.2% |
| Model 3 with individual-, tract- and county-level variablesc | 0.006 | 0.036 | 0.430 | 96.3% |
| Model 4 with individual-, tract-, county, and state-level variablesd | < 0.001 | < 0.001 | > 0.50 | > 99.9% |
Abbreviations: NHANES, National Health and Nutrition Examination Survey; SE, standard error.
Model 1 included age, sex, race/ethnicity, and health insurance status at individual level.
Model 2 included tract-level poverty rate to Model 1.
Model 3 included poverty rate, dentist-population ratio, proportion of Hispanic children, proportion of population aged 25+ years with education level of high school graduate or higher, and rural-urban classification at county level to Model 2.
Model 4 included state-level proportion of children enrolled in Medicaid/CHIP receiving dental services in the past year to Model 3.
Fig. 1.
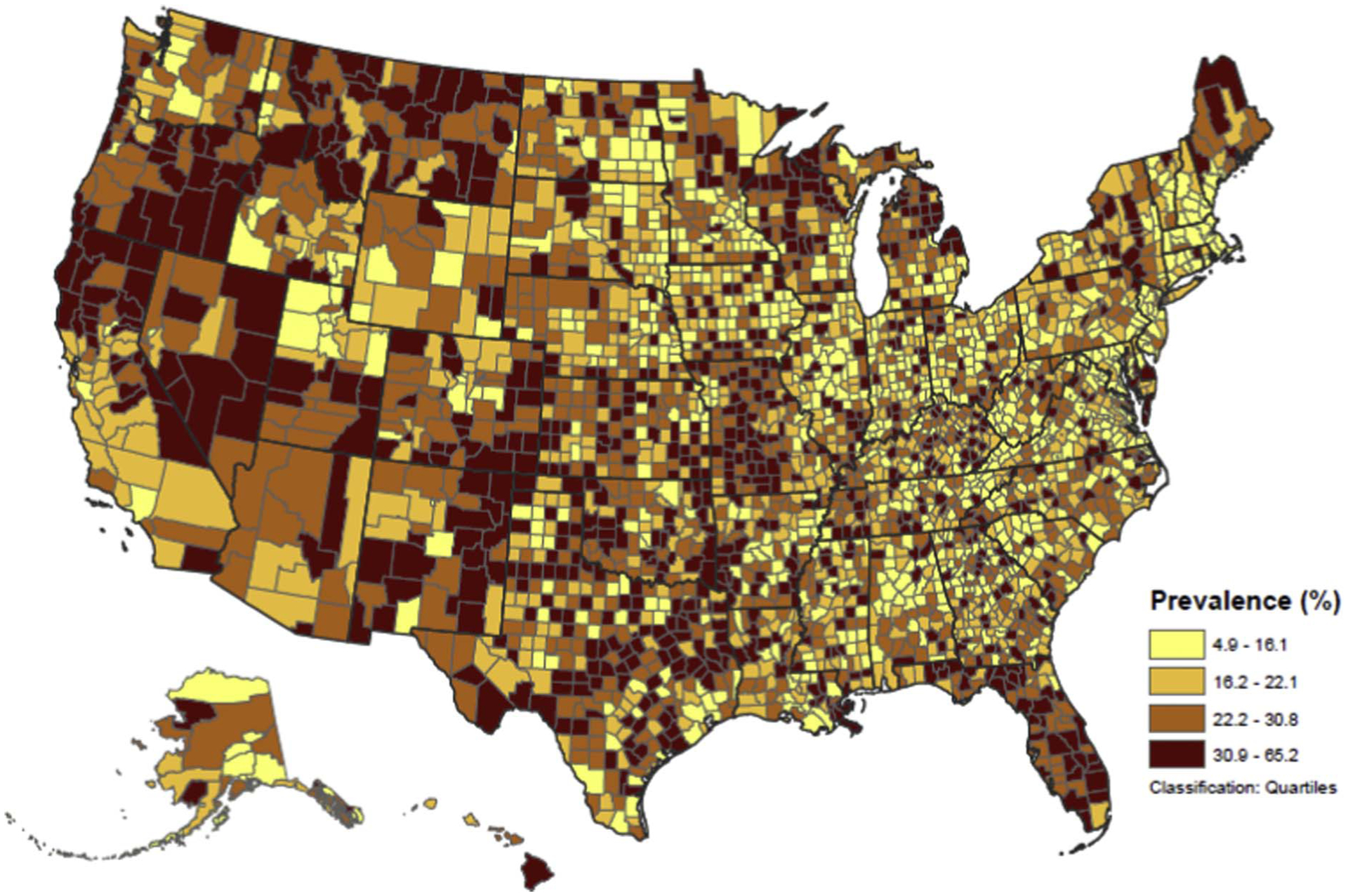
Model-based county-level estimated prevalence of untreated dental caries among children aged 6–9 years in the United States, 2005–2010.a
aModel-based county-level estimated prevalence of untreated dental caries produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficients.
3.2. Internal validation with direct national estimates from NHANES
The model-based national estimate of prevalence of untreated dental caries (19.9%) among children aged 6–9 years matched the direct estimate from NHANES (19.8%) (Table 2). When stratified by age, sex and race/ethnicity, the model-based estimates were generally similar to the direct estimates and all were contained in the 95% CI of the corresponding direct estimate. The model-based and direct estimates showed similar patterns of variation by the demographic characteristics where the prevalence estimate was higher among eight-year-olds, males, NHB, and Hispanic children than their counterparts.
Table 2.
Comparison of direct estimates from NHANES 2005–2010 and model-based estimatesa of prevalence of untreated cariesb among US children aged 6–9 years, by age, sex and race/ethnicity.
| NHANES direct estimates | Model-based estimates | |||
|---|---|---|---|---|
| Prevalence (%) | 95% CI | Prevalence (%) | 95% CI | |
| Total | 19.84 | 17.60, 22.28 | 19.89 | 19.87, 19.91 |
| Age (years) | ||||
| 6 | 18.08 | 14.71, 22.03 | 17.28 | 17.24, 17.32 |
| 7 | 18.13 | 14.60, 22.29 | 19.17 | 19.13, 19.22 |
| 8 | 23.40 | 18.75, 28.79 | 23.84 | 23.79, 23.89 |
| 9 | 19.51 | 15.68, 24.00 | 19.30 | 19.24, 19.35 |
| Sex | ||||
| Male | 21.80 | 18.49, 25.51 | 20.91 | 20.87, 20.95 |
| Female | 17.84 | 15.31, 20.69 | 18.83 | 18.79, 18.86 |
| Race/ethnicity | ||||
| Non-Hispanic White | 16.48 | 13.55, 19.90 | 17.73 | 17.70, 17.76 |
| Non-Hispanic Black | 26.52 | 22.67, 30.75 | 24.35 | 24.28, 24.41 |
| Hispanic | 25.05 | 21.87, 28.51 | 22.09 | 22.04, 22.15 |
| Other | 18.03 | 10.85, 28.44 | 20.29 | 20.24, 20.34 |
Abbreviations: CI, confidence interval; NHANES, National Health and Nutrition Examination Survey.
Model-based estimates produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficients.
Untreated caries in primary or permanent teeth.
3.3. External comparison with direct state estimates from third-grade SOHS
For 34 states with third-grade SOHS available in 2005–2010, moderate positive correlations (Pearson correlation = 0.54, P = 0.001; Spearman rank correlation = 0.58, P < 0.001) (Table 3 and Fig. 2) were found between model-based state estimates of prevalence of untreated caries for 8-year-olds and the SOHS direct estimates. A paired t-test showed no significant difference between the direct and model-based estimates (P = 0.23). The quartile distribution of the direct estimates roughly mirrored the distribution of the model-based estimates although the interquartile range for model-based estimates (7.4%) was smaller than that for direct estimates (11.5%).
Table 3.
Comparisons of direct state estimates of prevalence of untreated dental caries from third-grade SOHS 2005–2010 among 34 statesa and direct county estimates from New York third-grade SOHS 2009–2011 among 53 countiesb with model-based estimates 2005–2010 among children aged eight yearsc.
| Pearson correlation | Spearman Rank correlation | Paired t-test | Prevalence (%) | IQR (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Quartile 1 | Median | Quartile 3 | Max | |||||
| Direct state estimates from third-grade SOHS among 34 states, 2005–2010 vs. model-based state estimates among 8 year olds, 2005–2010 | |||||||||
| Direct estimates | 12.0 | 17.5 | 22.3 | 29.0 | 42.7 | 11.5 | |||
| Model-based estimates | 0.54 (P = 0.001) | 0.58 (P < 0.001) | P = 0.23 | 13.2 | 18.8 | 22.5 | 26.2 | 33.0 | 7.4 |
| Direct county estimates from the New York third-grade SOHS among 53 counties, 2009–2011 vs. model-based county estimates among 8 year olds, 2005–2010 | |||||||||
| Direct estimates | 10.1 | 19.8 | 24.5 | 30.0 | 52.8 | 10.2 | |||
| Model-based estimates | 0.38 (P = 0.006) | 0.29 (P = 0.03) | P = 0.42 | 14.1 | 20.9 | 23.0 | 29.3 | 66.0 | 8.4 |
Abbreviation: IQR, interquartile range; SOHS, State Oral Health Survey.
The comparison included 34 states, for which SOHS were available within 2005–2006 to 2010–2011.
The comparison included 53 counties of the New York state, for which the county-level direct estimates were available from the 2009–2011 New York SOHS.
Model-based estimates produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficient.
Fig. 2.
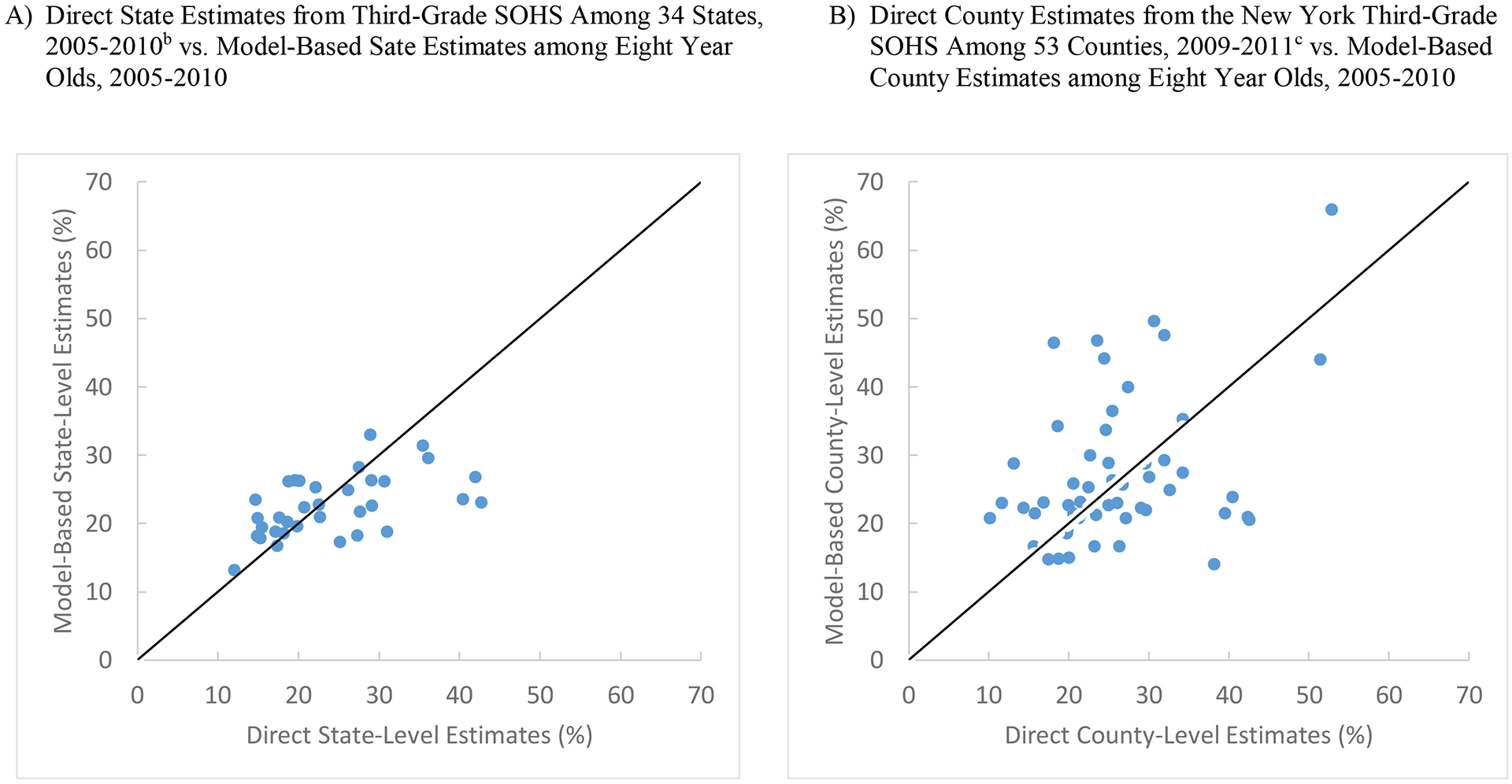
Scatter plots of direct state- and county-level estimates of prevalence of untreated dental caries (%) from select third-grade SOHS versus model-based estimates among children aged eight years, 2005–2010.a
Abbreviation: SOHS, State Oral Health Survey.
aModel-based estimates produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficients.
bPlot A included 34 states, for which SOHS were available within 2005–2006 to 2010–2011.
cPlot B included 53 counties of the New York state, for which the county-level direct estimates were available from the 2009–2011 New York SOHS.
3.4. External comparison with direct county estimates from New York third-grade SOHS
Similar results were found when the direct county-level estimates of prevalence of untreated dental caries for 53 counties from the New York third-grade SOHS 2009–2011 were compared with model-based estimates for these counties. Moderate positive correlation between direct and model-based estimates was observed (Pearson correlation = 0.38, P = 0.006; Spearman rank correlation = 0.29, P = 0.03) (Table 3 and Fig. 2). For example, the model-based estimates and direct estimates both identified Sullivan County with the highest prevalence although its model-based estimate (66.0%) was higher than its direct estimate (52.8%).
Figs. 3 and 4 show generally similar patterns of geographic clustering of the higher and lower prevalence of untreated caries when the model-based estimates for 8-year-olds were compared with direct estimates from the third-grade SOHS at state level for 34 states and at county level for 53 New York counties. About two-thirds of these states (70.6%, 12 out of 17 states) or counties (63%, 17 out of 27 counties) with direct estimates higher than the median were also in the higher than median group when ranked using model-based estimates.
Fig. 3.
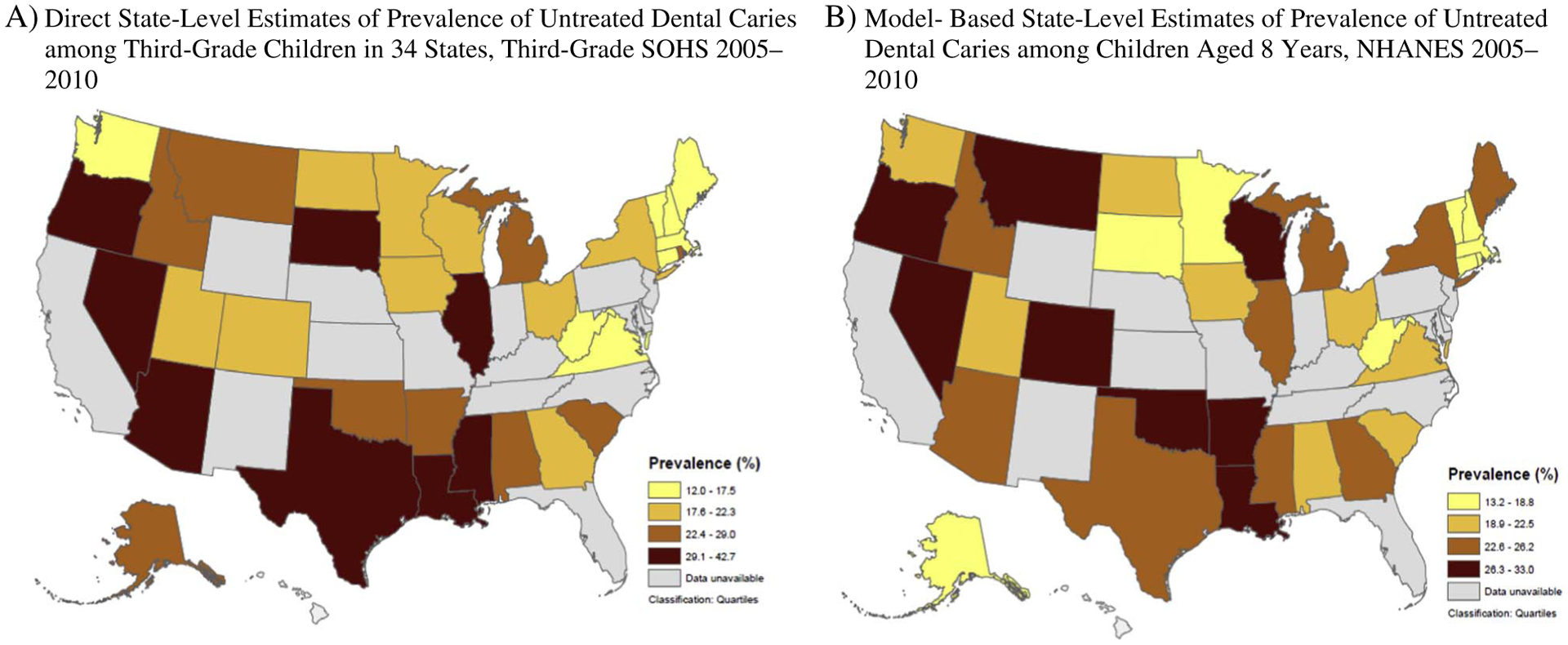
Comparison of state-level geographic variations in direct estimates of prevalence of untreated dental caries among third-grade children in 34 statesa, third-grade SOHS 2005–2010b vs. model-based estimatesc among children aged 8 years, 2005–2010.
Abbreviations: SOHS, State Oral Health Survey.
aThe comparison included 34 states, for which SOHS were available within 2005–2006 to 2010–2011. All other states that did not have SOHS available within this time period are included in the “Data unavailable” category.
bSurvey years of SOHS varied by state, ranging from 2005–2006 to 2010–2011.
cModel-based estimates produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficients.
Fig. 4.
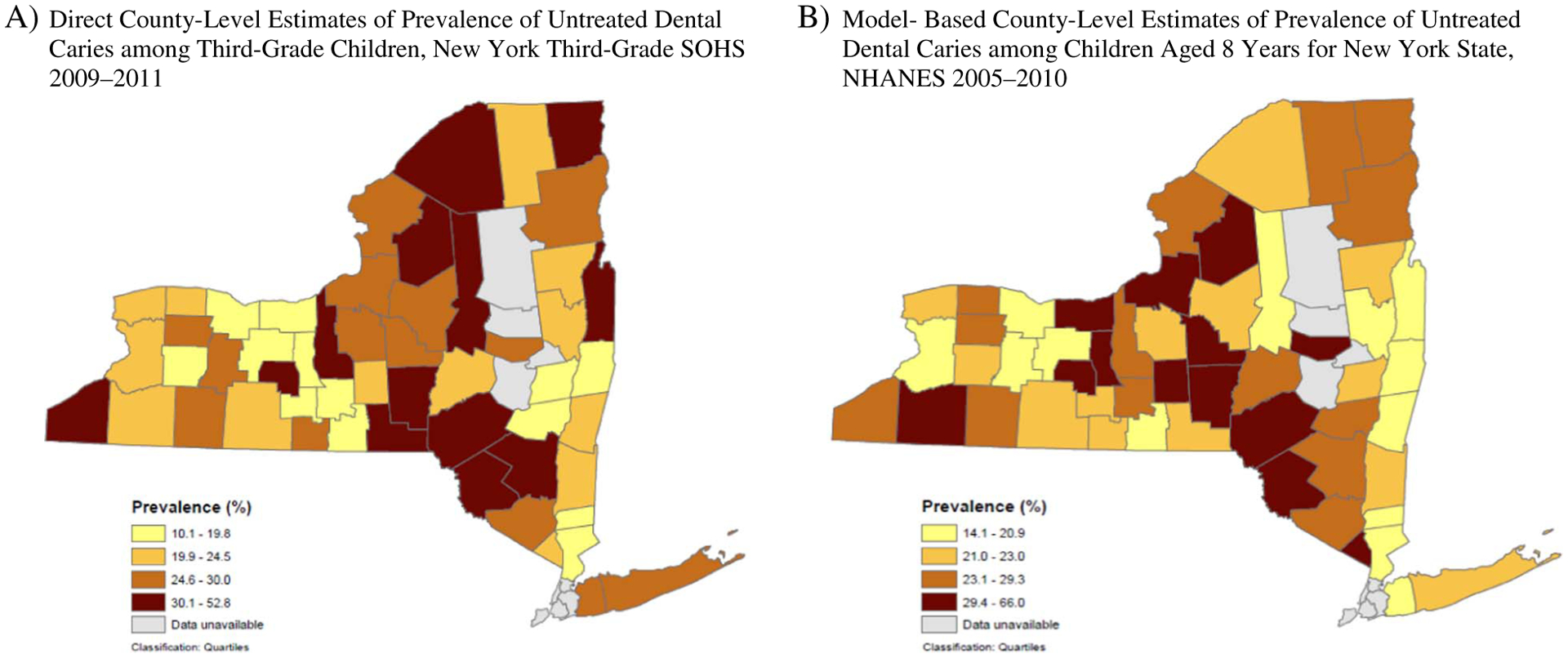
Comparison of county-level geographic variations in direct estimates of prevalence of untreated dental caries among third-grade children for 53 countiesa, New York third-grade SOHS 2009–2011 vs. model-based estimatesb among children aged 8 years, 2005–2010.
Abbreviations: SOHS, State Oral Health Survey.
aThe comparison included 53 counties of the New York state, for which the county-level direct estimates were available from the 2009–2011 New York SOHS. All other New York counties are included in the “Data unavailable” category.
bModel-based estimates produced using census data and National Health and Nutrition Examination Survey (NHANES) 2005–2010 model coefficients.
4. Discussion
We generated model-based estimates of prevalence of untreated caries among US children aged 6–9 years at the county level nationwide through application of MRP to NHANES linked with various area-level data. The estimated prevalence varied significantly across counties, with a large portion of the variation explained by area-level factors. The model-based estimates showed high internal validation performance at the national level and moderate correlations with select state- and county-level direct estimates from SOHS.
To our knowledge, our study is the first to demonstrate application of the MRP approach to NHANES linked with various area-level data to estimate county-level prevalence of untreated dental caries among children nationwide in the United States. Leroux et al. applied the mixed-effects regression model to estimate county-level caries prevalence among third-grade children using the 1994 Washington SOHS (Leroux et al., 1996). Although this study considered various characteristics associated with caries in the model, the model outcome was the school-level caries prevalence rather than caries status at the individual level and thus only covariates at aggregated levels were included in the model. Eke et al. used the 2009–2012 NHANES to estimate census block-level periodontitis prevalence among adults in the United States and demonstrated high consistency between direct and model-based estimates at the national level (Eke et al., 2016). However, their use of NHANES public-use dataset, which does not include geo-codes, does not allow including area-level covariates in the model to capture the multilevel influence and examining the extent of area-level variation explained by the prediction model.
We used restricted variables on geocoding from NHANES through access via the NCHS RDC that allowed us to overcome the limitations in the two referred studies (Eke et al., 2016; Leroux et al., 1996) and to take advantage of the MRP strengths. We applied the multilevel model with individual-level rather than area-level outcome and considered individual-level covariates from NHANES as well as various area-level covariates at tract, county and state levels to capture both individual- and contextual-level influences on the oral health outcome. In addition, our model used individual-level caries outcome. Recent SAE research suggests that compared with multilevel models using area-level aggregated outcomes, multilevel models with individual-level outcomes usually provide better model flexibility and avoid the ecological fallacy (Marhuenda et al., 2013; Zhang et al., 2014).
Multilevel modeling enabled us to incorporate both individual- and area-level factors and to examine the extent of the area-level variation in caries explained by covariates at different levels. We found that various area-level characteristics ranging from sociodemographic characteristics to factors reflecting dental care access and rural-urban designation were not only significant factors associated with untreated caries among children but also explained the majority of the county-level variation in untreated dental caries. Our findings support the multilevel conceptual framework proposed by Fisher-Owens et al. to assess children’s oral health (Fisher-Owens et al., 2007) and highlight the need and importance of incorporating area-level factors in SAE of caries among children.
In our study, the MRP approach demonstrated high internal consistency between model-based national estimates of untreated caries among children aged 6–9 years with estimates directly from NHANES overall and by age, sex and race/ethnicity. MRP has shown high internal consistency for various indicators such as Chronic Obstructive Pulmonary Disease (COPD), smoking, diabetes, obesity, and uninsured status among adults using Behavioral Risk Factor Surveillance System (BRFSS) (Zhang et al., 2015), obesity among children using the National Survey of Children’s Health (Zhang et al., 2013), and periodontal disease among adults using NHANES (Eke et al., 2016).
There is no “gold standard” data source available for external validation with model-based estimates of untreated caries from NHANES. However, we performed exploratory comparisons between model-based estimates among 8-year-olds and direct estimates among third-grade children at the state level from SOHS among 34 states and at the county level for 53 counties from the New York SOHS. We found significant positive correlations (Pearson and Spearman Rank correlations of 0.54 and 0.58 respectively at the state level and 0.38 and 0.29 respectively at the county level), comparable quartile distributions, and generally similar patterns of geographic clustering of the higher and lower prevalence estimates (Table 2, Figs. 2 and 3). The performance of our external comparisons, though not a validation, was comparable with the average level of performance from a recent MRP study that conducted external validation between BRFSS model-based estimates and direct estimates of COPD, smoking, obesity, diabetes, and uninsured adults from the Missouri County-Level Study based on BRFSS protocol (Zhang et al., 2015). The Pearson correlation and Spearman Rank correlation ranged from 0.28 and 0.17 for obesity to 0.69 and 0.63 for COPD. Of note, our relatively comparable performance was based on NHANES, which had a much smaller sample size than BRFSS.
4.1. Limitations
Several limitations of this study should be noted. First, although our internal validation indicated high consistency between model-based and direct estimates at the national level, we were not able to perform internal validation at the state or county level because NHANES is not designed to provide direct estimates at those levels.
Second, although we conducted exploratory external comparisons with direct estimates at state and county levels from select SOHS, they were not external validations per se because several limitations may impact the comparability. For example, the survey design, sampling frames, and oral health examination protocols may not be comparable between SOHS and NHANES. Considering intensive resources required, states conducted independent SOHS. Different states may field SOHS in different years, depending on availability of resources. Survey years of the 34 states ranged from 2005 to 2010. Although we used SAE limited to age 8 years, assuming it to be the most prevalent age for third graders, 8-year-olds and third graders may not be completely comparable.
Third, considering the complex and multifactorial nature of untreated dental caries (Fisher-Owens et al., 2007) our multilevel model may not capture the impact of all factors associated with the outcome. In addition, although we considered various factors at different area levels, the impact of intervention programs or policies or cultural differences specifically at local levels may not be captured by our study. These limitations may explain the moderate correlations from the external comparisons versus the high internal validation performance.
4.2. Strengths
Our study had notable strengths: 1) Our SAE was based on NHANES, which has a long history to provide ongoing and valid population surveillance data on dental caries for the nation based on standardized clinical examination and quality assurance. 2) Our study appears to be the first to demonstrate SAE of county-level untreated caries among children nationwide in the United States. 3) We considered a broad range of characteristics associated with untreated dental caries, ranging from socio-demographics to factors reflecting dental care access, rather than socio-demographics only. 4) We took advantage of MRP and considered factors at both individual and different area levels to capture multilevel influence on untreated dental caries. We reported the extent of county-level variation in untreated caries explained by factors at different levels. 5) Our external comparison performance was relatively comparable with recent SAE studies with MRP for chronic disease indicators using BRFSS, which had a much larger sample size than NHANES.
In addition, caries is the most reported unmet health care need (Vujicic et al., 2016). Strategies to reduce unmet need are typically implemented at local level. Model findings could help identify areas with high unmet dental care needs to inform targeted intervention programs (e.g., dental workforce expansion, school-based dental sealant programs).
5. Conclusions
In conclusion, our NHANES model-based estimates of prevalence of untreated caries among children aged 6–9 years demonstrated high internal validation performance at the national level and good correlations of external comparisons with select state- and county-level direct estimates from the third-grade SOHS. The estimated prevalence of untreated dental caries presented significant variation across counties, with a large portion explained by area-level factors. Both individual-level and area-level factors should be considered in the multilevel model for SAE of untreated caries among children. Given resource constraints, conducting county-level oral health surveys to generate direct estimates may not be feasible for most states. SAE of untreated caries among children using MRP with NHANES could be a useful and efficient tool to complement oral health surveillance data at local level to inform programs when direct local-level data are not available although the lack of external validation due to data unavailability should be acknowledged.
Supplementary Material
Acknowledgments
Data were analyzed at the secure CDC’s National Center for Health Statistics (NCHS) Research Data Center (RDC) at Atlanta. We gratefully acknowledge RDC staff, Dr. Frances A. McCarty, Dr. Carolyn S. Neal, Karon Lewis, and Jaylan Richardson, for their assistance with access to the geocoded NHANES. Special thanks go to Dr. Eugenio Beltran with the DB Consulting Group, Inc., Dr. Frances A. McCarty with RDC, and Dr. Lorena Espinoza with the CDC’s Division of Oral Health for their thoughtful review and suggestions on the manuscript.
Abbreviations:
- MRP
multilevel regression and poststratification
- BRFSS
Behavioral Risk Factor Surveillance System
- BSE
Basic Screening Examination
- CDC
Centers for Disease Control and Prevention
- CHIP
Children’s Health Insurance Program
- CI
confidence interval
- COPD
Chronic Obstructive Pulmonary Disease
- HP
Healthy People
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- SAE
small area estimation
- SOHS
State Oral Health Surveys
- RDC
Research Data Center
Footnotes
Publisher's Disclaimer: Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the US Department of Agriculture, the Research Data Center, the National Center for Health Statistics, or the Centers for Disease Control and Prevention.
Conflict of interest statement
The authors declare no conflict of interest relevant to this study.
Appendix. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2017.11.015.
References
- Ahovuo-Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Makela M, Worthington HV, 2013. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst. Rev (3), 1–129 CD001830. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2005. National Health and Nutrition Examination Survey (NHANES): oral health examiners manual. https://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/OH_E.pdf, Accessed date: 31 August 2016.
- Centers for Disease Control and Prevention, 2015. Oral Health Data. http://www.cdc.gov/oralhealthdata/, Accessed date: 7 June 2016.
- Centers for Disease Control and Prevention National Health and Nutrition Examination Survey - questionnaires, datasets, and related documentation. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm, Accessed date: 8 June 2016.
- Centers for Medicare & Medicaid Services Early and Periodic Screening, Diagnostic, and Treatment. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Early-and-Periodic-Screening-Diagnostic-and-Treatment.html, Accessed date: October 2015.
- Eke PI, Zhang X, Lu H, Wei L, Thornton-Evans G, Greenlund KJ, Holt JB, Croft JB, 2016. Predicting periodontitis at state and local levels in the United States. J. Dent. Res 95, 515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, Newacheck PW, 2007. Influences on children’s oral health: a conceptual model. Pediatrics 120, e510–20. [DOI] [PubMed] [Google Scholar]
- Gelman A, Little TC, 1997. Poststratification into many categories using hierarchical logistic regression. Surv. Methodol 32, 127–135. [Google Scholar]
- Griffin SO, Barker LK, Wei L, Li CH, Albuquerque MS, Gooch BF, Centers for Disease Control and Prevention, 2014. Use of dental care and effective preventive services in preventing tooth decay among U.S. Children and adolescents—Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010. MMWR Surveill. Summ 63 (Suppl. 2), 54–60. [PubMed] [Google Scholar]
- Health Resources and Services Administration, Area Health Resources Files (AHRF) 2013–2014. Accessed: August, 2015.
- Ingram DD, Franco SJ, 2012. NCHS urban-rural classification scheme for counties. Vital Health Stat. 2. [PubMed] [Google Scholar]
- Leroux BG, Maynard RJ, Domoto P, Zhu C, Milgrom P, 1996. The estimation of caries prevalence in small areas. J. Dent. Res 75, 1947–1956. [DOI] [PubMed] [Google Scholar]
- Lin M, Sappenfield W, Hernandez L, Clark C, Liu J, Collins J, Carle AC, 2012. Child- and state-level characteristics associated with preventive dental care access among U.S. children 5–17 years of age. Matern. Child Health J 16 (Suppl. 2), 320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marhuenda Y, Molina I, Morales D, 2013. Small area estimation with spatio-temporal Fay-Herriot models. Comput. Stat. Data Anal 58, 308–325. [Google Scholar]
- Marinho VC, Worthington HV, Walsh T, Clarkson JE, 2013. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev (7), 1–95 CD002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York State Department of Health, 2016. New York State Community Health Indicator Reports - oral health indicators. https://www.health.ny.gov/statistics/chac/indicators/ora.htm, Accessed date: 8 June 2016.
- Robert CP, Casela G, 2004. Monte Carlo statistical methods. In: Springer Texts in Statistics, 2nd edition. (New York, NY: ). [Google Scholar]
- US Census Bureau American Community Survey (ACS): Summary File Data. https://www.census.gov/programs-surveys/acs/data/summary-file.html, Accessed date: 18 July 2016.
- US Department of Health and Human Services, 2000. Oral health in America: a report of the Surgeon General. http://silk.nih.gov/public/hck1ocv.@www.surgeon.fullrpt.pdf, Accessed date: 8 July 2016.
- US Department of Health and Human Services, 2010. Healthy People 2020. http://www.healthypeople.gov/2020/default.aspx, Accessed date: 6 March 2017.
- Vujicic M, Buchmueller T, Klein R, 2016. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff. (Millwood) 35, 2176–2182. [DOI] [PubMed] [Google Scholar]
- Zhang X, Onufrak S, Holt JB, Croft JB, 2013. A multilevel approach to estimating small area childhood obesity prevalence at the census block-group level. Prev. Chronic Dis 10, E68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Holt JB, Lu H, Wheaton AG, Ford ES, Greenlund KJ, Croft JB, 2014. Multilevel regression and poststratification for small-area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the Behavioral Risk Factor Surveillance System. Am. J. Epidemiol 179, 1025–1033. [DOI] [PubMed] [Google Scholar]
- Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB, 2015. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the Behavioral Risk Factor Surveillance System. Am. J. Epidemiol 182, 127–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Yun S, Lu H, Wang Y, Eke PI, Holt JB, Greenlund K, Croft JB, 2016. Multilevel small-area estimation of health behaviors: an extension of multilevel regression and poststratification (MRP) approach via bootstrapping. Joint Statistical Meetings, Chicago. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


