1. INTRODUCTION
Menopause in women is associated with significant cardiometabolic changes, which increase the risk for cardiovascular diseases and premature death. Most of these cardiometabolic changes are attributed to the decrease in the estrogen levels, which confer cardiovascular protection during their younger reproductive age. 1 Among the main cardiometabolic changes are increases in body weight, insulin resistance, T2DM, cholesterol, and glucose levels, and obesity‐related hypertension. 2 In addition, menopause and physical inactivity lead to dyslipidemia (increased total cholesterol, LDL‐C, triglycerides, and low HDL‐C), atherosclerosis and consequent cardiovascular disease (CVD), and coronary heart disease (CHD), and cardiovascular (CV) death. 3 Another serious non‐cardiovascular complication of menopause especially in sedentary postmenopausal women is bone and muscle mass loss leading to osteoporosis and sarcopenia. 4 All these cardiometabolic changes are the result of a significant decrease in estrogen levels associated with menopause, but treatment with hormone replacement therapy (HRT), although beneficial, is associated with an increase in breast cancer. 5 Therefore, alternative means of treatment have been sought and one of them is physical exercise. In this issue of the journal, Stamatelopoulos et al 6 present interesting data from a large cohort study of 625 Greek postmenopausal women defined by low estradiol levels (<50 pg/mL) and increased follicle‐stimulating hormone levels (>25 mIU/mL) on the effects of physical activity in decreasing atherosclerosis and reducing arterial stiffness. They found that physical activity dose‐responsively was associated with weight and body fat loss (by BMI and waist circumference), as well as decreases in blood pressure (BP), pulse wave velocity (PWV), insulin resistance, lipid levels (cholesterol, LDL‐C, Triglycerides), and increase in HDL‐C. In this study, the physical exercise was associated with improved functional vascular changes (decrease in BP and PWV), but not organic changes (IMT, atherosclerotic plaque). It appears that physical exercise improved the arterial elasticity as a first stage, because organic changes like IMT and carotid plaque regression require longer duration of physical exercise and in a retrospective study is difficult to assess the level and duration of exercise due to memory recall problems. Overall this is an important study enhancing the knowledge on the beneficial cardiometabolic effects of exercise in postmenopausal women.
2. BENEFICIAL CARDIOMETABOLIC EFFECTS OF EXERCISE IN POSTMENOPAUSAL WOMEN: MECHANISM OF ACTION
Many studies have demonstrated the cardiometabolic benefits of regular exercise in both men and women, and it is recommended by the American College of Cardiology/American Heart Association (ACC/AHA) guideline for the primary prevention of cardiovascular disease. Postmenopausal women are at an increase risk of CVD and other important clinical maladies that can significantly be prevented or improved with regular physical exercise. These adverse effects of menopause are summarized in Table 1 and they will, briefly, discussed here.
Table 1.
Cardiometabolic benefits of physical exercise in postmenopausal women
| Risk factor | Benefit |
|---|---|
| Hypertension | Reduces BP through vasodilation from release of NO, improves endothelial dysfunction, vagal nervous system stimulation |
| Obesity | Improves obesity through weight and body fat loss |
| Dyslipidemia | Improves dyslipidemia through decrease in total cholesterol, LDL‐C, TGs, and increase in HDL‐C |
| CVD, HF | Prevents primary and secondary CVD and atherosclerosis through favorable lipid changes, weight loss insulin resistance, T2DM, and hypertension |
| Osteoporosis‐sarcopenia | Prevents or improves these conditions by preventing or improving bone and muscle loss, prevents fractures and increases mobility |
2.1. Hypertension
Regular physical exercise can either, prevent or improve preexisting hypertension through weight reduction and peripheral vasodilatation through improvement in endothelial dysfunction, release of nitric oxide (NO), and cyclic guanosine monophosphate (cGMP), as well as improvement of oxidative stress. In addition, the exercise‐induced cardiac output and blood flow and the shear stress are additional factors for NO release and improvement in autonomic system function through an increase in parasympathetic nerve function and increase in peripheral vasodilation. 8 The antihypertensive benefits of exercise can be better improved with a combination of dynamic and isometric exercise. 8 , 9
2.2. Obesity
Most menopausal women gain weight after menopause, which is accompanied by several changes in their body composition. Increased body weight is associated with an increased in total body fat content that includes visceral as well as epicardial fat resulting in myocardial dysfunction, metabolic syndrome, insulin resistance, T2DM, and dyslipidemia. 10 In such cases, moderate physical exercise at 60%‐70% of maximum heart rate has been shown to produce significant beneficial effects on body mass index (BMI), fat mass, lean body mass, visceral fat, adiponectin levels, serum lipids, and the metabolic status of postmenopausal women. 11 , 12
2.3. Lipid levels
Menopause is also associated with adverse changes in the lipid profile with increases in total cholesterol, LDL‐C, TGs, and decrease in HDL‐C in postmenopausal women, and physical exercise can lead to beneficial lipid changes. A recent study in a small number of postmenopausal women showed that a 3‐month aerobic treadmill training of moderate intensity, of 30 minutes, three times/week was associated with an increase in HDL‐C by approximately 30% and a decrease in LDL‐C and TGs by approximately 27% and 18%, respectively, in addition to cholesterol treatment. 13
2.4. Cardiovascular disease
The decrease in estrogen levels in postmenopausal women in combination with the various risk factors such as inflammation, hypertension, dyslipidemia, obesity, and T2DM, lead to atherosclerotic cardiovascular disease (ASCVD), CHD, myocardial infarction (MI), and eventually to CV death. 14 It is hypothesized that all these adverse cardiometabolic changes in postmenopausal women are due to the loss of the atheroprotective effects estrogen through their E2 receptors and are sex specific. 15 In addition to their atheroprotective effects, estrogen also mediates the protection against the ischemia reperfusion injury following a period of vascular ischemia from MI, and postmenopausal women lose this protection. 16 Another cardiovascular adverse effect of estrogen decrease in postmenopausal women is the oxidative mediated fibrous tissue accumulation, which together with the obesity and hypertension could lead left ventricular hypertrophy, left ventricular dysfunction, and the development of heart failure with preserved ejection fraction. 17 , 18
2.5. Osteporosis and sarcopenia
This is another serious adverse effect in sedentary postmenopausal women. The lack of estrogen protection and exercise lead to bone and muscle bulk loss and the development of osteoporosis and sarcopenia. These adverse effects lead to bone fractures, muscle weakness and decreased mobility and quality of life. 4 , 19 These changes can be either prevented or reversed with a combination of dynamic and isometric exercise, which has been shown to increase bone density and muscle mass and improve mobility and quality of life. 20
3. COMMENT
From the data presented, it is clearly demonstrated that the lack of estrogen support and inactivity in postmenopausal women is associated with several cardiovascular risk factors, such obesity, the metabolic syndrome. T2DM, hypertension, and dyslipidemia which predispose the postmenopausal women to increased incidence of C VD and HF. In addition, the combination of decrease of estrogen levels and sedentary existence predispose the postmenopausal women to bone and muscle loss and the development of osteoporosis and sarcopenia leading to bone fractures, weakness, decreased mobility, and quality of life. All these adverse effects can be prevented or reversed with exercise as has been demonstrated from the study by Stamatelopoulos et al 6 as well as by several other studies. However, the sad part is that although physical activity is so important for the maintenance of healthy life and cardiorespiratory fitness (CRF), people do not exercise enough or not at all today. As is shown from Figure 1 by the 2019 ACC/AHA guidelines for the primary prevention of cardiovascular disease, Americans today spent only 0.2 hours/d for either moderate or vigorous physical activity. 7 Part of this problem is the increased technology and the time spent in front of the computer either for work or recreation, watching TV, or playing video games, or driving to work. 21 In order to maintain good health and good CRF, the ACC/AHA guidelines recommend about 150 minutes/wk of moderate physical activity or 75 minutes/wk of vigorous physical activity. It is very critical that physicians caring for postmenopausal women to stress the importance of physical activity of any kind (walking, running, bicycling, or gardening) in combination with some weight bearing, together with healthy eating for the maintenance of quality of life. All these recommendations will go a long way in the prevention and reversal of the adverse cardiometabolic risk factors associated with menopause and inactivity.
Figure 1.
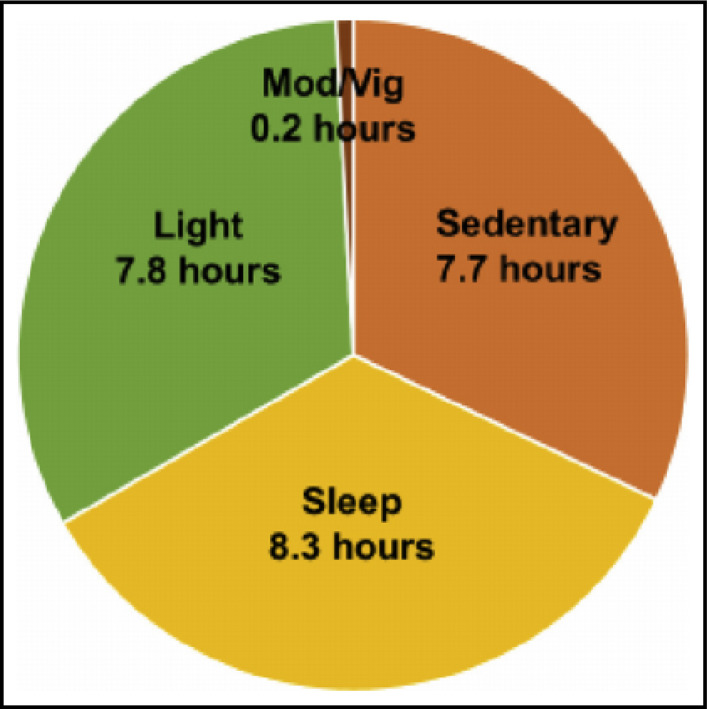
Daily hours spent by Americans on various states of physical activity. Figure demonstrates that Americans spent the majority of their time (≥7 h) in sedentary activities and only 0.2 h on moderate or vigorous activity. Adapted from Arnett et al 7
CONFLICT OF INTEREST
The author declares no conflict of interest and that no funds were received for the preparation of the manuscript.
Chrysant SG. The cardiometabolic benefits of exercise in postmenopausal women. J Clin Hypertens. 2020;22:1691–1693. 10.1111/jch.13968
REFERENCES
- 1. Zmijewski P, Mazurek K, Kozdrn E, et al. Cardiovascular risk reduction in sedentary postmenopausal women during organized physical activity. Kardiol Pol. 2017;75:476‐485. [DOI] [PubMed] [Google Scholar]
- 2. Chrysant SG. Pathophysiology and treatment of obesity‐related hypertension. J Clin Hypertens. 2019;21:555‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Paschou SA, Marina LV, Spartalis E, et al. Therapeutic strategies for type 2 diabetes mellitus after menopause. Maturitas. 2019;126:69‐72. [DOI] [PubMed] [Google Scholar]
- 4. Agostini D, Zeppa SD, Lucertini F, et al. Muscle and bone health in postmenopausal women: role of protein and vitamin D supplementation combined with exercise training. Nutrients. 2018;10:1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yoo TK, Han KD, Kim DH, et al. Hormone replacement therapy, breast cancer risk factors, and breast cancer risk: a nationwide population‐based cohort. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1341‐1347. [DOI] [PubMed] [Google Scholar]
- 6. Stamatelopoulos K, Tsoltos N, Armeni E, et al. Physical activity is associated with lower arterial stiffness in normal‐weight post menopausal women. J Clin Hypertens. 2020. 10.1111/jch.13954. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary. J Am Coll Cardiol. 2019;74:1376‐1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fagard RH. Exercise therapy in hypertensive cardiovascular disease. Prog Cardiovasc Dis. 2011;53:404‐411. [DOI] [PubMed] [Google Scholar]
- 9. Cornelissen VA, Fagard RH, Coeckelberghs E, et al. Impact of resistance training on blood pressure and other cardiovascular risk factors. Hypertension. 2011;58:950‐958. [DOI] [PubMed] [Google Scholar]
- 10. González N, Moreno‐Villegas Z, González‐Bris A, et al. Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol. 2017;16:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jarrete AP, Novais IP, Nunes HA, et al. Influence of aerobic exercise training on cardiovascular and endocrine‐inflammatory biomarkers in hypertensive postmenopausal women. J Clin Transl Endocrinol. 2014;1:108‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee JA, Kim JW, Kim DY. Effects of yoga exercise on serum adiponectin and metabolic syndrome factors in obese postmenopausal women. Menopause. 2012;19:296‐301. [DOI] [PubMed] [Google Scholar]
- 13. Ammar T. Effects of aerobic exercise on blood pressure and lipids in overweight hypertensive postmenopausal women. J Exerc Rehabbil. 2015;11:145‐150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Insull W Jr. The pathology of atherosclerosis: plaque development and plaque responses to medical treatment. Am J Med. 2009;122:S3‐S14. [DOI] [PubMed] [Google Scholar]
- 15. Aryan L, Younessi D, Zargari M, et al. The role of estrogen receptors in cardiovascular disease. Int J Mol Sci. 2020;21:4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kalogeris T, Baines CP, Krenz M, et al. Cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol. 2012;298:229‐317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bernardo BC, Weeks KL, Pretorius L, et al. Molecular distinction between physiological and pathological cardiac hypertrophy: experimental findings and therapeutic strategies. Pharmacol Ther. 2010;128:191‐227. [DOI] [PubMed] [Google Scholar]
- 18. Chrysant SG, Chrysant GS. Obesity‐related heart failure with preserved ejection fraction: new treatment strategies. Hosp Pract. 2019;47:67‐72. [DOI] [PubMed] [Google Scholar]
- 19. Dennison EM, Sayer AA, Cooper C. Epidemiology of sarcopenia and insight into possible therapeutic targets. Nat Rev Rheumatol. 2017;13:340‐347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liguori I, Russo G, Aran L, et al. Sarcopenia: assessment of disease burden and strategies to improve outcomes. Clin Interv Aging. 2018;13:913‐927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chrysant SG, Chrysant GS. The cardiovascular consequences of excess sitting time. J Clin Hypertens. 2015;17:528‐531. [DOI] [PMC free article] [PubMed] [Google Scholar]


