1. INTRODUCTION
Increased blood pressure is the leading single reversible risk for death in the world according to the Global Burden of Disease study. 1 As a result, there is an increased global effort to prevent and control hypertension. The World Health Organization (WHO)‐led HEARTS initiative and programs by Resolve to Save Lives are two global efforts that have a focus on hypertension control to reduce the burden of non‐communicable diseases. 2 , 3 Recently, the WHO, with support of Resolve to Save Lives, has published “WHO technical specifications for automated non‐invasive blood pressure measuring devices with cuff” in recognition of widespread inaccuracies in clinical blood pressure assessment and advances in automated blood pressure devices that could improve the accuracy of clinical blood pressure assessments. 4 Key messages to health care professionals and institutions included that accurate validated electronic blood pressure monitors with appropriately sized upper‐arm cuffs should be used in routine clinical and community screening, and that certification courses and annual training and re‐training of health care professionals should be required to ensure accurate blood pressure measurement. Training should include proper patient preparation, cuff selection, and blood pressure measurement technique. In order to minimize additional training needed for accurate manual blood pressure measurements, only automated non‐invasive blood pressure measuring devices should be used.
This commentary has been written for the Accuracy in Measurement of BP (AIM‐BP) Collaborative that promotes the identification, dissemination, and implementation of best measurement practices globally. 5 The commentary highlights the potential impact of common levels of inaccuracy in blood pressure assessment (either over‐ or under‐estimation of the true blood pressure) on the perceived population prevalence and control of hypertension.
Inherent in all hypertension management guidelines are specific recommendations to use standardized procedures, appropriate cuff size, and employ validated devices to ensure that measurement is accurate and reproducible. 6 , 7 , 8 , 9 , 10 The recommendations specify a comfortable, non‐stimulating environment, and standardized patient preparation to reduce variation in blood pressure caused by external and internal factors so as to approximate the true basal blood pressure. Standardized techniques in measuring blood pressure are recommended to reduce variation in systemic blood pressure (eg, an unsupported arm or increasing blood pressure because of hydrostatic pressure changes related to the height of the brachial artery relative to the heart).
Deviations from recommendations for proper blood pressure measurement can cause significant changes in assessed blood pressure (Table 1). 11 Inaccuracies in blood pressure assessment can be systematic if there is a consistent deviation in recommended procedure, such as use of an inaccurate blood pressure device or leaving the arm at a fixed height that differs from heart level. Variation in blood pressure can also be more random when some recommendations for blood pressure assessment are not followed (eg, a variable rest period before blood pressure measurement). Most deviations from proper blood pressure measurement result in a higher than a standardized blood pressure reading, and generally with bigger effects on systolic blood pressure than diastolic blood pressure (Table 1). Systematic variation will affect all those assessed in a similar fashion and can change the perceived prevalence, and rates of diagnosis, treatment, and control. Random variation in the procedure will result in more variable blood pressure and difficulty in assessing the true basal blood pressure.
Table 1.
Approximate changes in blood pressure with variations in blood pressure measurement technique
| Variation in blood pressure technique | Range of change in systolic/diastolic blood pressure (mm Hg) |
|---|---|
| Cold environment | 5‐32/4‐23 |
| Insufficient rest | 4.2‐11.6/1.8‐4.3 |
| Legs crossed at knee | 2.5‐14.9/1.4‐10.8 |
| Unsupported back | 0/6.5 |
| Unsupported arm | 4.9/2.7‐4.8 |
| Talking during measurement | 4‐19/5‐14.3 |
| Fast deflation rate | −9 to −2/2.1 to 6.3 |
| Arm lower than heart level | 3.7‐23/2.8‐12 |
Adapted from Kallionen et al. 11
Audits find that, in general, the recommendations for assessing an accurate reproducible blood pressure are rarely followed in clinical practice and use of inaccurate devices, or those that have not passed accuracy validation standards are very common. 12 , 13 , 14 , 15 , 16 , 17 For example, in a clinical audit of 114 primary care physicians, McKay et al reported no physician followed all the recommended blood pressure measurement technique and 30% of aneroid devices were out of calibration by more than 10 mm Hg. 12 In another study by McKay et al of family medicine residents and interns, only recommendations for arm support, bilateral measurement, and using phase V Korotkoff sounds to define diastolic blood pressure were followed by more than 50% of those assessed. 18 Sebo et al, also found few primary care physicians followed standardized technique, and that the average difference in blood pressure vs a “gold standard” measurement with recommended technique was 23.0/15.3 mm Hg and accuracy did not improve following training. 16
Figures 1 and 2 show the impact of systematic variation in blood pressure on hypertension prevalence and control rates from a blood pressure survey conducted in rural China. 19 The study protocol used specifically trained physicians following a recommended standardized technique to measure blood pressure with a validated automatic blood pressure device. Three blood pressure measurements were taken at each of three different visits within 1 week. Analysis showed that inaccuracies in blood pressure by 10/5 mm Hg changed the perceived hypertension prevalence (22.1% vs 53.4%) and control rate (21.2% vs 3.6%), respectively. This problem was apparent irrespective of the direction of inaccuracy (lower or higher than true blood pressure). Analyses from United States, Canada, and the United Kingdom using population survey data produced similar results. In the United States, Cook et al modeled that a 2 mm Hg reduction in population diastolic blood pressure reduced the perceived diastolic hypertension prevalence by 17%. 20 In the population screened for the Hypertension Detection and Follow‐up Program (HDFP), a 5 mm Hg decrease in diastolic blood pressure reduced diastolic hypertension prevalence by 42% while an increase in diastolic blood pressure of 5 mm Hg increased diastolic hypertension prevalence by 54%. 21 In Canada, modeling a decrease in population blood pressure of 5/2.7 mm Hg reduced the hypertension prevalence by 30% and almost doubled the hypertension control rate. 12 , 22 An increase in population diastolic blood pressure of 5 mm Hg more than doubled the hypertension prevalence and a decrease of 5 mm Hg reduced the prevalence by 62%. 23 , 24 An increase in population systolic blood pressure of 5 mm Hg increased the hypertension prevalence 43% and a decrease of 5 mm Hg reduced the prevalence by 30%. 23 , 24 In the United Kingdom, an increase in population diastolic blood pressure of 5 mm Hg increased the hypertension prevalence 73% and a decrease of 5 mm Hg reduced the prevalence by 47%. 24 An increase in population systolic blood pressure of 5 mm Hg increased the hypertension prevalence 26% and a decrease of 5 mm Hg reduced the prevalence by 21%. 24
FIGURE 1.

The impact on hypertension prevalence of systematic errors in measuring blood pressure. The blood pressure data are from an adult population study in rural China based on three blood pressure readings at each of three visits in one week. 18 Blood pressure is changed at intervals of 2/1 mm Hg for each individual to calculate the change in hypertension prevalence (≥140/90 mm Hg or taking antihypertensive medications). The 0/0 change in blood pressure represents the hypertension prevalence without adjustments to the blood pressure
FIGURE 2.
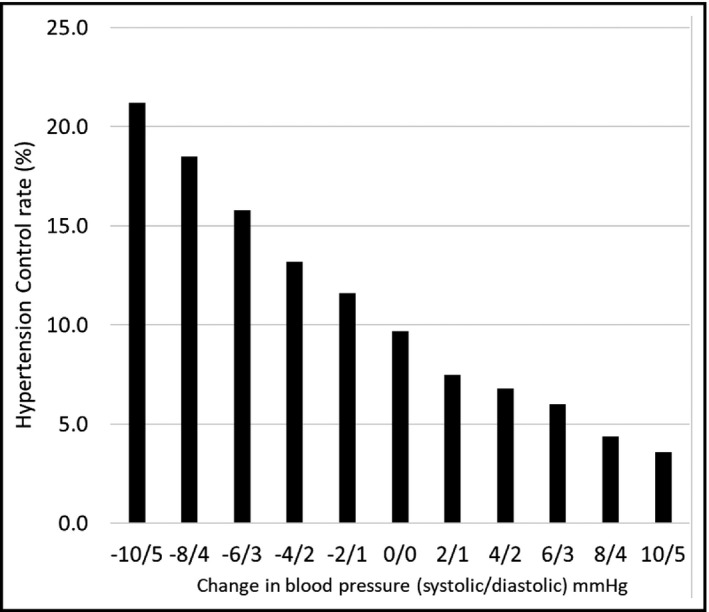
The impact on hypertension control rate (<140/90 mm Hg) of systematic errors in measuring blood pressure. The blood pressure data are from an adult population study in rural china based on three blood pressure readings at each of three visits in one week. 18 Blood pressure is changed at intervals of 2/1 mm Hg for each individual to calculate the change in hypertension control (blood pressure < 140/90 mm Hg as a percent of all adults with hypertension). The 0/0 change in blood pressure represents the control rate of all those with hypertension without adjustments to the blood pressure
A limitation of the analyses on the impact of systematic variation in blood pressure is that they were conducted using a threshold of 140/90 mm Hg with the exception of the study by Fan et al who reported both 140/90 mm Hg and 130/80 mm Hg thresholds. 19 , 25 The 130/80 mm Hg threshold results in a higher hypertension prevalence rate and lower rate of control; however, the errors still have a major impact. 19 Differences in the average population blood pressure and the shape of the population distribution of blood pressure will result in differences in the proportion of the population impacted by a fixed error in blood pressure measurement. We also note there is variation in recommendations on standardized measurement technique in different guidelines and those variations may impact blood pressure. 6 , 8 , 9 , 10 Many of the studies assessing clinical accuracy were done in practices using manual blood pressure measurement. Accuracy validated automated blood pressure measurement devices maybe subject to less error as they automate some of the measurement techniques.
These modeling studies of population surveys are consistent with clinical studies. In a study in primary care clinics, usual clinic blood pressures were on average 6.2/3.9 mm Hg higher than readings taken with standardized techniques and the hypertension normotension classification differed in 57% of those assessed. 26 Seventy‐four percent of the misclassifications related to hypertensive clinic readings while the standardized readings were normal. Similar results have been found in other studies. 16
The above data highlight that small errors in assessing blood pressure at the individual level have a substantial impact on perceived hypertension prevalence and control rates at the population level. This emphasizes a strong need to enhance the accuracy of hypertension measurement in clinical practice and in clinical research. National hypertension surveys have been enhanced by the standardization of blood pressure assessment through the WHO STEPs methodology as well as by several national governments. 27 , 28 , 29 , 30 There have been several efforts to standardize and enhance the clinical measurement of hypertension. For example, in Cuba, a program to improve hypertension control included a mandatory certification course in accurate blood pressure measurement. 31 Several organizations including the World Hypertension League, Lancet Commission on Hypertension Group, AIM‐BP, and STRIDE‐BP have advocated for use of accurate validated automated blood pressure devices in clinical practice and included calls to regulate the blood pressure device industry. 5 , 32 , 33 , 34 A consensus on a universal standard for validating the accuracy of automated electronic blood pressure measuring devices has been established. 35 More recently, the WHO has provided recommendations for policies and regulations relating to accurate blood pressure assessment. 4
It is now time for organizations focused on cardiovascular risk reduction and health care professionals to join the effort to promote the routine use of accurate, validated electronic blood pressure monitors with appropriately sized upper‐arm cuffs in clinical and community practice. Certification courses and annual training and re‐training of health care professionals should be required to ensure accurate blood pressure measurement. In this way, these entities can add their voice to the ongoing efforts to ensure accurate diagnosis and management for patients affected by this highly prevalent and deadly condition.
Campbell NRC, Padwal R, Picone DS, Su H, Sharman JE; for the Accuracy in Measurement of BP (AIM‐BP) Collaborative . The impact of small to moderate inaccuracies in assessing blood pressure on hypertension prevalence and control rates. J Clin Hypertens. 2020;22:939–942. 10.1111/jch.13915
REFERENCES
- 1. Institute for Health Metrics and Evaluation ; 2020. https://vizhub.healthdata.org/gbd‐compare/. Accessed March 25, 2020.
- 2. World Health Organization . HEARTS: Technical package for cardiovascular disease management in primary health care. Geneva, Switzerland: World Health Organization; 2016:1‐73. https://apps.who.int/iris/bitstream/handle/10665/252661/9789241511377‐eng.pdf;jsessionid=D0929959E42B9A51B2C1D9BBD9CC3722?sequence=1. [Google Scholar]
- 3. Frieden TR, Jaffe MG. Saving 100 million lives by improving global treatment of hypertension and reducing cardiovascular disease risk factors. J Clin Hypertens. 2018;20:208‐211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . WHO technical specifications for automated non‐invasive blood pressure measuring devices with cuff. Geneva, Switzerland. World Health Organization; 2020:1–72. https://www.who.int/docs/default‐source/searo/indonesia/who‐tech‐spec‐for‐automated‐non‐invasive‐blood‐pressure‐measuring‐devices‐with‐cuff.pdf?sfvrsn=b112be47_2. [Google Scholar]
- 5. Padwal R, Campbell NRC, Weber MA, et al. The Accuracy in Measurement of Blood Pressure (AIM‐BP) collaborative: background and rationale. J Clin Hypertens. 2019;21(12):1780‐1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71:e13‐e115. [DOI] [PubMed] [Google Scholar]
- 7. Cloutier L, Daskalopoulou SS, Padwal RS, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol. 2015;31(5):620‐630. [DOI] [PubMed] [Google Scholar]
- 8. Daskalopoulou SS, Rabi DM, Zarnke KB, et al. The 2015 Canadian hypertension education program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2015;31(5):549‐568. [DOI] [PubMed] [Google Scholar]
- 9. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021‐3104. [DOI] [PubMed] [Google Scholar]
- 10. TRUE Consortium (inTernational consoRtium for qUality resEarch on dietary sodium/salt) . Recommended standards for assessing blood pressure in human research where blood pressure or hypertension is a major focus. J Clin Hypertens. 2017;19(2):108‐113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients' resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35(3):421‐441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McKay DW, Campbell NRC, Parab LS, Chockalingam A, Fodor JG. Clinical assessment of blood pressure. J Hum Hypertens. 1990;4(6):639‐645. [PubMed] [Google Scholar]
- 13. Ray GM, Nawarskas JJ, Anderson JR. Blood pressure monitoring technique impacts hypertension treatment. J Gen Intern Med. 2012;27(6):623‐629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim JW, Bosworth HB, Voils CI, et al. Brief report: How well do clinic‐based blood pressure measurements agree with the mercury standard? J Gen Intern Med. 2005;20(7):647‐649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Campbell NRC, Culleton BW, McKay DW. Misclassification of blood pressure by usual measurement in ambulatory physician practices. Amer J Hypertens. 2005;18:1522‐1527. [DOI] [PubMed] [Google Scholar]
- 16. Sebo P, Pechère‐Bertschi A, Herrmann FR, Haller DM, Bovier P. Blood pressure measurements are unreliable to diagnose hypertension in primary care. J Hypertens. 2014;32(3):509‐517. [DOI] [PubMed] [Google Scholar]
- 17. Picone DS, Deshpande RA, Schultz MG, et al. Non‐validated home blood pressure devices dominate the online marketplace in Australia: major implications for cardiovascular risk management. Hypertension. 2020;75(6):1593‐1599. [DOI] [PubMed] [Google Scholar]
- 18. McKay DW, Raju MK, Campbell NRC. Assessment of blood pressure measuring techniques. Med Educ. 1992;26(3):208‐212. [DOI] [PubMed] [Google Scholar]
- 19. Fan WG, Xie F, Wan YR, Campbell NRC, Su H. The impact of changes in population blood pressure on hypertension prevalence and control in China. J Clin Hypertens. 2020;22(2):150‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cook NR, Cohen J, Hebert P, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch of Internal Med. 1995;155(7):701‐709. [PubMed] [Google Scholar]
- 21. Daugherty SA. Hypertension detection and follow‐up program. Description of the enumerated and screened population. Hypertension. 1983;5:IV1‐IV43. [DOI] [PubMed] [Google Scholar]
- 22. Joffres M, Campbell NR, Manns B, Tu K. Estimate of the benefits of a population‐based reduction in dietary sodium additives on hypertension and its related health care costs in Canada. Can J Cardiol. 2007;23(6):437‐443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Campbell NRC, McKay DW. Accurate blood pressure measurement. Why does it matter? Can Med Assoc J. 1999;161(3):277‐278. [PMC free article] [PubMed] [Google Scholar]
- 24. Turner MJ, Baker AB, Kam PC. Effect of systematic errors in blood pressure measurements on the diagnosis of hypertension. Blood Press Monit. 2004;9(5):249‐253. [DOI] [PubMed] [Google Scholar]
- 25. Campbell NRC, Myers MG, McKay DW. Is usual measurement of blood pressure meaningful? Blood Press Monit. 1999;4(2):71‐76. [PubMed] [Google Scholar]
- 26. Lackland DT, Beilin LJ, Campbell NRC, et al. Global implications of blood pressure thresholds and targets. Hypertension. 2018;71(6):985‐987. [DOI] [PubMed] [Google Scholar]
- 27. Riley L, Guthold R, Cowan M, et al. The World Health Organization STEPwise approach to noncommunicable disease risk‐factor surveillance: methods, challenges, and opportunities. Am J Publ Health. 2016;106(1):74‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ostchega Y, Prineas RJ, Paulose‐Ram R, Grim CM, Willard G, Collins D. National Health and Nutrition Examination Survey 1999‐2000: effect of observer training and protocol standardization on reducing blood pressure measurement error. J Clin Epidemiol. 2003;56(8):768‐774. [DOI] [PubMed] [Google Scholar]
- 29. Tolonen H, Koponen P, Naska A, et al. Challenges in standardization of blood pressure measurement at the population level. BMC Med Res Methodol. 2015;15:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bryan SLM, Campbell N, Clarke J, Tremblay MS. Resting blood pressure and heart rate measurement in the Canadian Health Measures Survey, cycle 1. Health Rep. 2010;21:1‐8. [PubMed] [Google Scholar]
- 31. Valdés González Y, Campbell NRC, Pons Barrera E, et al. Implementation of a community‐based hypertension control program in Matanzas, Cuba. J Clin Hypertens. 2020;22(2):142‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stergiou GS, O'Brien E, Myers M, et al. STRIDE BP international initiative for accurate blood pressure measurement: systematic review of published validation studies of blood pressure measuring devices. J Clin Hypertens. 2019;21(11):1616‐1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388(10060):2665‐2712. [DOI] [PubMed] [Google Scholar]
- 34. Campbell NR, Berbari AE, Cloutier L, et al. Policy Statement of the World Hypertension League on noninvasive blood pressure measurement devices and blood pressure measurement in the clinical or community setting. J Clin Hypertens. 2014;16(5):320‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stergiou GS, Alpert B, Mieke S, et al. A Universal Standard for the Validation of Blood Pressure Measuring Devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. J Hypertension. 2018;37(3):459‐466. [Google Scholar]


