Abstract
Epidemiologic studies have consistently demonstrated an increased risk of cardiovascular disease during colder temperatures. Hemodynamic changes associated with cold temperature and an increase in thrombogenicity may both account for the increase in cardiovascular risk and mortality. Studies using both in‐office and out‐of‐office BP measurements have consistently shown an elevation in BP during the colder seasons. The large difference in BP between cold and warm months may increase the incidence of hypertension and reduce the hypertension control rate, potentially resulting in increased cardiovascular risk, especially among those at risk of cardiovascular disease. The current trends in global warming and climate change may have a profound impact on the epidemiology of hypertension and cardiovascular disease, as changes in the climate may significantly affect both BP variability and cardiovascular disease, especially in those with high cardiovascular risk and the elderly. Furthermore, climate change could have a significant influence on hypertension in Asia, considering the unique characteristics of hypertensive patients in Asia. As an increase in ambient temperature decreases the mean daytime average and morning surge in BP, but increases the nocturnal BP, it is difficult to predict how environmental changes will affect the epidemiology and prognosis of hypertension in the Asian‐Pacific region. However, these seasonal variations in BP could be minimized by adjusting the housing conditions and using anticipation medicine. In this review, we discuss the impact of seasonal variation in the ambient temperature on hypertension and cardiovascular disease and discuss how this may impact the epidemiology of hypertension and cardiovascular disease.
Keywords: ambient temperature, Asia, environment, home blood pressure, HOPE Asia Network, hypertension
1. INTRODUCTION
Seasonal variation in the ambient temperature is associated with significant differences in the risks of mortality and cardiovascular disease. Epidemiologic studies have consistently demonstrated higher risks of cardiovascular disease and mortality during the winter months than during the summer months.1, 2 Although multiple factors may contribute to the increased risk of cardiovascular disease during colder months, one important factor is the increase in blood pressure (BP) associated with colder temperatures. Recent changes in the global climate are also affecting the Asian‐Pacific region, which is a diverse region, with climates ranging from temperate to tropical. Regional climate changes will not only impact the epidemiology of hypertension, but also the epidemiology of cardiovascular disease.
In this review, we discuss the impact of seasonal variation in the ambient temperature on hypertension and cardiovascular disease and discuss how this may impact the epidemiology of hypertension and cardiovascular disease.
2. THE INFLUENCE OF AMBIENT TEMPERATURE ON CARDIOVASCULAR DISEASE
Epidemiologic studies have consistently demonstrated an increased risk of cardiovascular disease during colder temperatures. For example, in England and Wales, the peak of winter and summer accounted for 20 000 additional deaths per year.3 In the United States, an analysis of 259 891 cases of acute myocardial infarction (AMI) from the second national myocardial infarction registry demonstrated that there were 53% more cases of myocardial infarction (MI) in winter than in summer.4, 5 In a time‐series analysis of 1 826 186 non‐accidental deaths in 272 major cities in China, relative to that for the temperature with the minimum mortality (22.8°C), 14.33% of non‐accidental mortality was attributed to non‐optimal temperatures, with moderate cold temperatures (−1.4°C to 22.8°C) accounting for an attributable fraction of 10.49%, while moderate heat temperatures (22.8 to 29.0°C) accounted for an attributable fraction of only 2.08%.1 In an analysis of 74 225 200 deaths in 384 locations in Australia, Brazil, Canada, China, Italy, Japan, South Korea, Spain, Sweden, Taiwan, Thailand, UK, and the USA, attributable deaths at non‐optimal temperatures, defined as temperatures above or below the point of minimal mortality, and at extreme temperatures, defined using cutoffs at the 2.5th and 97.5th percentiles, were calculated. The results showed that the attributable risk of death by cold temperatures (7.29%, 7.02‐7.49) was higher than that by hot temperatures (0.42%, 0.39‐0.44). Interestingly, extreme cold and hot temperatures only accounted for 0.86% (0.84‐0.87) of the total mortality.2
Hemodynamic changes associated with cold temperature and increased thrombogenicity may both account for the seasonally increased cardiovascular risk and mortality.5 Exposure to cold induces endothelial dysfunction and increased BP, which may be the main contributing factors of the increased risk of mortality. Seasonal variation in the ambient temperature influences both the mean BP and the BP circadian rhythm, which may have significant influence on the seasonal variation in cardiovascular disease risk. However, other factors have also been reported, such as increases in plasma fibrinogen, LDL cholesterol, vasoconstriction, and blood viscosity, which may increase blood thrombogenicity and the risk of cardiovascular events.2, 6, 7
3. THE INFLUENCE OF AMBIENT TEMPERATURE ON BLOOD PRESSURE AND BLOOD PRESSURE VARIABILITY
Exposure to cold temperatures may increase sympathetic nervous system activation and vasoconstriction, and reduce endothelial function, which may contribute to an increase in BP. In a study of the Framingham offspring cohort, brachial flow‐mediated dilation (FMD) and its independent association with seasonal temperature were analyzed. The results showed that the highest FMD occurred in the warmest temperature quartiles and the lowest FMD occurred in the coldest outdoor temperature quartiles.8 Furthermore, studies using both in‐office and out‐of‐office BP measurements have consistently shown an elevation in BP during the colder season. For example, a study by Lewington et al cross‐sectionally assessed the seasonal variation in BP and its relationship to the outdoor temperature in 506 673 individuals from 10 regions in China, using data from the China Kadoorie Biobank. The results showed that the mean difference in systolic blood pressure (SBP) between the summer and winter months was 10 mm Hg. Additionally, for outdoor temperatures over 5°C, there was a 5.7 mm Hg increase in SBP per 10°C decrease in the outdoor temperature.9 The lack of an association between the outdoor temperature and BP at temperatures below 5°C may have been due to the confounding effect of indoor heating. In a study by Saeki et al,10 ambulatory BP monitoring (ABPM) parameters were more strongly associated with the indoor temperature than with the outdoor temperature during the colder months.
The large difference in BP between cold and warm months may increase the incidence of hypertension and reduce the hypertension control rate, potentially resulting in increased cardiovascular risk,11 especially in those at risk of cardiovascular disease. In an analysis of Kadoorie Biobank data from 23 000 individuals, at temperatures above 5°C, there was a 6.2 mm Hg increase in SBP per 10°C decrease in the outdoor temperature, and a 10 mm Hg increase in SBP was associated with a 21% increase in the risk of cardiovascular mortality, with a 41% higher risk of cardiovascular mortality in the winter than in the summer.12
In addition to the influence of seasonal variation in the ambient temperature on BP, as demonstrated above, BP can be influenced by changing weather conditions, regardless of seasonal changes. A study by Aubinière‐Robb et al mapped the data from the clinical visits of 16 010 hypertensive patients to the monthly weather data. The percent change in BP between visits was calculated according to the stability in weather; extreme alternations were defined as a change from one extreme quartile to another (Q1‐Q4 or Q4‐Q1), and stability was defined as remaining in the same quartile (Qn‐Qn). Stable temperature (Qn‐Qn) was associated with a 2% drop in BP at the subsequent clinical visit, whereas a drop in temperature (Q4‐Q1) was associated with 2.1% and 1.6% rises in SBP and diastolic BP (DBP), respectively, at the subsequent visit.13 Therefore, rapid day‐to‐day or week‐to‐week changes in temperature can also influence BP variability and, potentially, cardiovascular outcomes.
Numerous studies have examined how seasonal changes in the ambient temperature affect both the mean and variability of out‐of‐office BP. In an analysis of 2051 individuals from the Pressione Arteriose Monitorate E Loro Associazioni (PAMELA) registry, summer was associated with the lowest values and winter the highest values, for both the average home and 24‐hours BP; furthermore, normotensives, untreated hypertensives, and treated hypertensives showed similar trends.14 Additionally, a study by Modesti et al analyzed the ambulatory BP data of 6404 individuals and found that the 24‐hours BP and daytime SBP was inversely related to the ambient temperature. Interestingly, nocturnal SBP was positively related to the ambient temperature.15 Higher nocturnal BP and non‐dipping patterns of BP during the summer months have been confirmed in other studies.16, 17 In an analysis of ABPM recordings of untreated individuals, the night‐to‐day ratio of BP (n = 897) was 2.4% higher in the summer and 1.8% lower in the winter. In contrast, the morning surge in BP (n = 637) was 1.7 mm Hg lower in the summer and 1.1 mm Hg higher in the winter.16
In the Nagahama study, seasonal variation in nocturnal BP was assessed in a cohort of 4780 individuals using a fully automatic oscillometric BP measurement device (HEM 7080 IC). BP was measured at home, and the sleeping period defined by actigraphy. The results showed that the fall in nocturnal SBP was significantly lower in the summer than in the winter, and there were significantly higher frequencies of riser and non‐dipper patterns of BP during the summer months as well.17 Although clinicians tend to reduce the dosage and number of antihypertensive medications during the summer months due to the decrease in the in‐office BP and fear of hypotensive episodes, the higher nocturnal BP and prevalence of risers and non‐dippers during the summer months may have clinical significance, suggesting the need for more active use of out‐of‐office BP monitoring during the summer months to optimize the control of BP variability, especially in high‐risk hypertensive patients.18
The abovementioned studies are limited in that BP measurements were either captured at a single point, or at a few points, during each season, or were not consecutive measurements from a single person. In contrast, the Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED‐BP) study measured home BP daily during the follow‐up period in a cohort of patients. As such, they were able to analyze the weekly home BP average over multiple years and correlate the data with seasonal changes. The results showed that the highest home BP occurred mid to late January, and the differences between the maximum and minimum home SBP and DBP were 6.7 mm Hg and 2.9 mm Hg, respectively. Furthermore, a lower body mass index, older age, and male sex were independently associated with seasonal variation in the home BP.19
4. INFORMATION AND COMMUNICATION TECHNOLOGY (ICT)–BASED HOME BP MONITORING TO DETECT SEASONAL VARIATION
Home BP monitoring (HBPM) may be the best approach for detecting seasonal variation in BP. By using HBPM, one can detect BP levels and variability according to various time phases, such as morning‐evening, day‐by‐day, and seasonal variations.20 Morning home BP is more closely associated with the indoor room temperature than with the outdoor temperature, and the average home BP monitoring, especially in the morning, is significantly associated with cardiovascular risk in community‐dwelling individuals and hypertensive patients.21, 22, 23, 24, 25, 26, 27, 28, 29, 30 The current era of exponential progress in the ICT field allows home BP values to be self‐measured by patients daily and remotely sent to electronic health records; thus, the accuracy of the diagnosis of hypertension and the efficacy of its management may be increased, particularly when HBPM is accompanied by co‐interventions.31 As the first activity of the HOPE Asia Network, we have first focused on implantation of home BP use to clinical practice in Asian countries.32, 33, 34, 35, 36, 37
Seasonal variation in BP could be minimized to around 120 mm Hg in the summer and 125 mm Hg in the winter via anticipation medicine, with the up‐titration of antihypertensive drugs in the autumn months, before the onset of winter (Figure 1).38 At the time of the Great East Japan earthquake and tsunami (March 2011), the authors developed a web‐based, ICT‐based BP monitoring system (the Disaster CArdiovascular Prevention [DCAP] Network) and introduced it in an area that was catastrophically damaged (Minamisanriku town), in an effort to help control the survivors' BP. Using this system, home BP was monitored, and the data were automatically transmitted to a central computer database and the attending physicians of the survivors. The study participants, 341 hypertensive patients, continued to use this system for 4 years after the disaster. The DCAP home BP‐guided approach helped achieve a decrease in home BP over a 4‐year period (initial average: 151/87 mm Hg; final average: 120 ± 12/71 mm Hg) (Figure 1). Disaster hypertension that developed after the earthquake initially concealed the seasonal variation in home BP.39 However, after 1 year, the seasonal variation in home BP reappeared. Anticipatory antihypertensive drug titration targeting the seasonal variation in BP minimized its amplitude, and the duration from the lowest summer home BP values to the peak winter home BP values was gradually prolonged. Thus, the ICT‐based approach was useful in achieving strict home BP control and even minimized the seasonal variation in BP in a catastrophically damaged area during a 4‐year period after the disaster, suggesting that this approach could be a routine way to monitor BP in the community (Figure 1).
Figure 1.
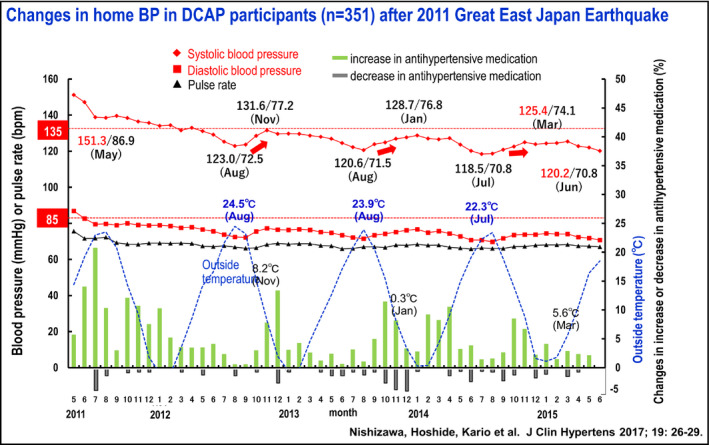
Seasonal variation in the home blood pressure of hypertensive patients living in the area damaged by the East Japan Earthquake
Another factor that needs to be considered is the housing conditions, which are especially important for elderly hypertensive patients. A study by Nishizawa et al analyzed the winter morning surge according to the housing conditions after the Great East Japanese earthquake and found that hypertensive patients aged ≥75 years who lived in self‐owned older homes showed a significantly higher risk for being in the highest quintile (≥20 mm Hg) of the morning BP surge (odds ratio 5.21; 95% confidence interval, 1.49‐18.22; P = .010) compared to that for individuals who lived in better insulated temporary housing provided by the government.40 The results from this study show the importance of adequate indoor insulation and heating to minimize the winter morning BP surge, especially in elderly individuals.
Finally, we have developed a multi‐sensor home and ambulatory BP monitoring system to monitor the 24‐hours central and brachial BP variability concurrent with physical activity, temperature, and atmospheric pressure. The new BP monitoring system utilizes our recently developed biological and environmental signal monitoring ICT, which can simultaneously monitor the environment (temperature, illumination, etc) of various rooms in a house (entryway, bedroom, living room, bathing room, and toilet), and a wrist‐type high‐sensitivity actigraph for identifying the location of the patient. By collecting data on both BP and environmental parameters, the system can assess the brachial and central hemodynamic BP reactivity profiles of patients, such as actisensitivity (BP changes with physical activity), thermosensitivity (BP changes with temperature changes), and atmospheric sensitivity (BP changes with atmospheric pressure changes).41, 42 We used this new system to monitor ambulatory BP variability in outpatients with one or more cardiovascular disease risk factors in both the summer and winter.42 Actisensitivity (the slope of the regression line of ambulatory BP against the log‐physical activity) was higher in winter than in summer. By a multi‐level analysis using the parameters monitored by this system, we estimated the ambulatory BP under different conditions. The individual time‐series big data collected by this system will contribute to further developing anticipation medicine for cardiovascular disease.
5. HOW WILL THE CURRENT CLIMATE CHANGE INFLUENCE THE EPIDEMIOLOGY OF HYPERTENSION AND CARDIOVASCULAR DISEASE IN THE ASIAN‐PACIFIC REGION?
The current trends in global warming and climate change may have a profound impact on the epidemiology of hypertension and cardiovascular disease. Extreme hot and cold temperatures have been linked to acute cardiovascular events.43 Additionally, variability in temperatures may increase the risk of cardiovascular events, especially in elderly individuals, in whom physiologic adaptations to extreme changes in temperature are slower.43 Seasonal variability in BP has been shown to be higher in elderly individuals, especially those aged >80 years.44 Therefore, changes in the climate may result in significant changes in both BP variability and cardiovascular disease, especially in those who are elderly and at high cardiovascular risk. The elderly are especially vulnerable to increased risk of cardiovascular mortality from temperature extremes, primarily due to poor thermoregulation.45 Furthermore, climate change could have a significant influence on hypertension in Asia, considering the unique characteristics of hypertensive patients in Asia. Asians tend to be more salt‐sensitive, have higher morning BP surge with morning hypertension, and have a higher incidence of isolated nocturnal hypertension.46 As an increase in the ambient temperature decreases the mean daytime average and morning surge in BP, but increases nocturnal BP, it is difficult to predict how changes in the environment will affect the epidemiology and prognosis of hypertension in the Asian‐Pacific region. The HOPE Asia Network comprises hypertension specialists from 11 Asian countries and regions who are working to (a) understand the current evidence, (b) achieve consensus, and (c) conduct clinical studies with the objective of “zero” cardiovascular events in Asia. This network is in a unique position to conduct multinational prospective cohort studies to understand the changes in the epidemiology of hypertension and BP variability that are associated with climate changes in the Asian‐Pacific region and will continue to collaborate in the future to achieve this goal.
CONFLICT OF INTEREST
S Park has received honoraria from Pfizer, Daiichi Sankyo, Takeda, Daewon pharmaceutical company, Boryung pharmaceutical company and Servier. K Kario received research grants from Omron Healthcare, Fukuda Denshi, A&D, Pfizer Japan, and honoraria from Omron Healthcare. S Siddique has received honoraria from Bayer, Novartis, Pfizer, ICI, and Servier; and travel, accommodation and conference registration support from Atco Pharmaceutical, Highnoon Laboratories, Horizon Pharma, ICI, Pfizer and CCL. YC Chia has received honoraria and sponsorship to attend conferences and CME seminars from Abbott, Bayer, Boehringer Ingelheim, GlaxoSmithKline, Menarini, Merck Sharp & Dohme, Novartis, Orient Europharma, Pfizer, and Sanofi; and a research grant from Pfizer. J Nailes has received research grants from Pfizer. J Shin has received honoraria and sponsorship to attend seminars from Daiichi Sankyo, Takeda, Menarini, MSD, Bristol‐Myers Squibb, and Sanofi. CH Chen has served as an advisor or consultant for Novartis Pharmaceuticals Corporation; has served as a speaker or a member of a speakers bureau for AstraZeneca; Pfizer Inc; Bayer AG; Bristol‐Myers Squibb Company; Boehringer Ingelheim Pharmaceuticals, Inc; Daiichi Sankyo, Inc; Novartis Pharmaceuticals Corporation; SERVIER; Merck & Co., Inc; Sanofi; TAKEDA Pharmaceuticals International; and has received grants for clinical research from Microlife Co., Ltd. J Sison has received honoraria from Pfizer, AstraZeneca, AmGen, Boehringer Ingelheim, and Novartis. GP Sogunuru has received a research grant related to hypertension monitoring and treatment from Pfizer. JG Wang has received research grants from Bayer, Merck Sharp & Dohme, Pfizer, and Phillips; and lecture and consulting fees from Bayer, Daiichi‐Sankyo, Merck Sharp & Dohme, Pfizer, Servier and Takeda. TD Wang has received honoraria from Abbott, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, Medtronic, Menarini, Novartis, Omron, Pfizer, Sanofi, and Servier. YQ Zhang has received research grants from Bayer, Novartis, and Shuanghe; and lecture fees from Bayer, Daiichi Sankyo, Novartis, Pfizer, Sanofi, Servier, and Takeda. All other authors report no potential conflicts of interest in relation to this article.
AUTHOR CONTRIBUTION
Sungha Park, MD, PhD conceived and drafted the manuscript. Sungha Park, MD, PhD, Kazuomi Kario, MD, PhD, Yook‐Chin Chia, MBBS, FRCP, Yuda Turana, MD, PhD, Chen‐Huan Chen, MD, Peera Buranakitjaroen, MD, MSc, DPhil, Jennifer Nailes, MD, MSPH, Satoshi Hoshide, MD, PhD, Saulat Siddique, MBBS, MRCP (UK), FRCP (Lon), Jorge Sison, MD, Arieska Ann Soenarta, MD, Guru Prasad Sogunuru, MD, DM, Jam Chin Tay, MBBS, FAMS, Boon Wee Teo, MB BCh (Ireland), Yu‐Qing Zhang, MD, Jinho Shin, MD, Huynh Van Minh, MD, PhD, Naoko Tomitani, BSc, Tomoyuki Kabutoya, MD, PhD, Apichard Sukonthasarn, MD, Narsingh Verma, MD, Tzung‐Dau Wang, MD, PhD, and Ji‐Guang Wang, MD, PhD contributed to critical revision for important intellectual content. Sungha Park, MD, PhD, Kazuomi Kario, MD, PhD, Yook‐Chin Chia, MBBS, FRCP, Yuda Turana, MD, PhD, Chen‐Huan Chen, MD, Peera Buranakitjaroen, MD, MSc, DPhil, Jennifer Nailes, MD, MSPH, Satoshi Hoshide, MD, PhD, Saulat Siddique, MBBS, MRCP (UK), FRCP (Lon), Jorge Sison, MD, Arieska Ann Soenarta, MD, Guru Prasad Sogunuru, MD, DM, Jam Chin Tay, MBBS, FAMS, Boon Wee Teo, MB BCh (Ireland), Yu‐Qing Zhang, MD, Jinho Shin, MD, Huynh Van Minh, MD, PhD, Naoko Tomitani, BSc, Tomoyuki Kabutoya, MD, PhD, Apichard Sukonthasarn, MD, Narsingh Verma, MD, Tzung‐Dau Wang, MD, PhD, and Ji‐Guang Wang, MD, PhD contributed to final approval of the submitted manuscript.
Park S, Kario K, Chia Y‐C, et al. on behalf of the HOPE Asia Network. The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens. 2020;22:438–444. 10.1111/jch.13762
Funding information
This research was supported by a research grant from the Fire Fighting Safety & 119 Rescue Technology Research and Development Program funded by National Fire Agency (grant number: MPSS‐FireSafety‐2015‐80) and a research grant from the Korea Centers for Disease Control & Prevention (grant number: 2018ER630200).
REFERENCES
- 1. Chen R, Yin P, Wang L, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ. 2018;363:k4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369‐375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pell JP, Cobbe SM. Seasonal variations in coronary heart disease. QJM. 1999;92:689‐696. [DOI] [PubMed] [Google Scholar]
- 4. Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31:1226‐1233. [DOI] [PubMed] [Google Scholar]
- 5. Bhatnagar A. Environmental Determinants of Cardiovascular Disease. Circ Res. 2017;121:162‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Woodhouse PR, Khaw KT, Plummer M, Foley A, Meade TW. Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet. 1994;343:435‐439. [DOI] [PubMed] [Google Scholar]
- 7. Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J (Clin Res Ed). 1984;289:1405‐1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Widlansky ME, Vita JA, Keyes MJ, et al. Relation of season and temperature to endothelium‐dependent flow‐mediated vasodilation in subjects without clinical evidence of cardiovascular disease (from the Framingham Heart Study). Am J Cardiol. 2007;100:518‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lewington S, Li L, Sherliker P, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30:1383‐1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saeki K, Obayashi K, Iwamoto J, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32:1582‐1589. [DOI] [PubMed] [Google Scholar]
- 11. Su D, Du H, Zhang X, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural Chinese population. Int J Epidemiol. 2014;43:1835‐1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang L, Li L, Lewington S, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J. 2015;36:1178‐1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Aubiniere‐Robb L, Jeemon P, Hastie CE, et al. Blood pressure response to patterns of weather fluctuations and effect on mortality. Hypertension. 2013;62:190‐196. [DOI] [PubMed] [Google Scholar]
- 14. Sega R, Cesana G, Bombelli M, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens. 1998;16:1585‐1592. [DOI] [PubMed] [Google Scholar]
- 15. Modesti PA, Morabito M, Bertolozzi I, et al. Weather‐related changes in 24‐hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155‐161. [DOI] [PubMed] [Google Scholar]
- 16. Sheng CS, Cheng YB, Wei FF, et al. Diurnal Blood Pressure Rhythmicity in Relation to Environmental and Genetic Cues in Untreated Referred Patients. Hypertension. 2017;69:128‐135. [DOI] [PubMed] [Google Scholar]
- 17. Tabara Y, Matsumoto T, Murase K, et al. Seasonal variation in nocturnal home blood pressure fall: the Nagahama study. Hypertens Res. 2018;41:198‐208. [DOI] [PubMed] [Google Scholar]
- 18. Salles GF, Reboldi G, Fagard RH, et al. Prognostic Effect of the Nocturnal Blood Pressure Fall in Hypertensive Patients: The Ambulatory Blood Pressure Collaboration in Patients With Hypertension (ABC‐H) Meta‐Analysis. Hypertension. 2016;67:693‐700. [DOI] [PubMed] [Google Scholar]
- 19. Hanazawa T, Asayama K, Watabe D, et al. Seasonal variation in self‐measured home blood pressure among patients on antihypertensive medications: HOMED‐BP study. Hypertens Res. 2017;40:284‐290. [DOI] [PubMed] [Google Scholar]
- 20. Fujiwara T, Hoshide S, Kanegae H, Nishizawa M, Kario K. Reliability of morning, before‐dinner, and at‐bedtime home blood pressure measurements in patients with hypertension. J Clin Hypertens (Greenwich). 2018;20:315‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kario K, Kanegae H, Tomitani N, et al. Nighttime Blood Pressure Measured by Home Blood Pressure Monitoring as an Independent Predictor of Cardiovascular Events in General Practice. Hypertension. 2019;73:1240‐1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kario K, Iwashita M, Okuda Y, et al. Morning Home Blood Pressure and Cardiovascular Events in Japanese Hypertensive Patients. Hypertension. 2018;72:854‐861. [DOI] [PubMed] [Google Scholar]
- 23. Kario K. Global Impact of 2017 American Heart Association/American College of Cardiology Hypertension Guidelines: A Perspective From Japan. Circulation. 2018;137:543‐545. [DOI] [PubMed] [Google Scholar]
- 24. Hoshide S, Yano Y, Mizuno H, Kanegae H, Kario K. Day‐by‐Day Variability of Home Blood Pressure and Incident Cardiovascular Disease in Clinical Practice: The J‐HOP Study (Japan Morning Surge‐Home Blood Pressure). Hypertension. 2018;71:177‐184. [DOI] [PubMed] [Google Scholar]
- 25. Fujiwara T, Yano Y, Hoshide S, Kanegae H, Kario K. Association of Cardiovascular Outcomes With Masked Hypertension Defined by Home Blood Pressure Monitoring in a Japanese General Practice Population. JAMA Cardiol. 2018;3:583‐590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kario K, Saito I, Kushiro T, et al. Morning Home Blood Pressure Is a Strong Predictor of Coronary Artery Disease: The HONEST Study. J Am Coll Cardiol. 2016;67:1519‐1527. [DOI] [PubMed] [Google Scholar]
- 27. Hoshide S, Yano Y, Haimoto H, et al. Morning and Evening Home Blood Pressure and Risks of Incident Stroke and Coronary Artery Disease in the Japanese General Practice Population: The Japan Morning Surge‐Home Blood Pressure Study. Hypertension. 2016;68:54‐61. [DOI] [PubMed] [Google Scholar]
- 28. Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large‐scale prospective, real‐world observational study. Hypertension. 2014;64:989‐996. [DOI] [PubMed] [Google Scholar]
- 29. Asayama K, Ohkubo T, Metoki H, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self‐measured home blood pressure. Hypertens Res. 2012;35:1102‐1110. [DOI] [PubMed] [Google Scholar]
- 30. Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population‐based observation in Ohasama. Japan. J Hypertens. 1998;16:971‐975. [DOI] [PubMed] [Google Scholar]
- 31. Kario K, Shimbo D, Hoshide S, et al. Emergence of Home Blood Pressure‐Guided Management of Hypertension Based on Global Evidence. Hypertension. 2019;74:229‐236. 10.1161/hypertensionaha.119.12630.Hypertensionaha11912630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Park S, Buranakitjaroen P, Chen CH, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249‐258. [DOI] [PubMed] [Google Scholar]
- 33. Kario K, Tomitani N, Buranakitjaroen P, et al. Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: Results of the Asia BP@Home study. J Clin Hypertens (Greenwich). 2018;20:1686‐1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kario K, Tomitani N, Buranakitjaroen P, et al. Rationale and design for the Asia BP@Home study on home blood pressure control status in 12 Asian countries and regions. J Clin Hypertens (Greenwich). 2018;20:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kario K, Park S, Buranakitjaroen P, et al. Guidance on home blood pressure monitoring: A statement of the HOPE Asia Network. J Clin Hypertens (Greenwich). 2018;20:456‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kario K. The HOPE Asia Network for "zero" cardiovascular events in Asia. J Clin Hypertens (Greenwich). 2018;20:212‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chia YC, Buranakitjaroen P, Chen CH, et al. Current status of home blood pressure monitoring in Asia: Statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2017;19:1192‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nishizawa M, Hoshide S, Okawara Y, Matsuo T, Kario K. Strict Blood Pressure Control Achieved Using an ICT‐Based Home Blood Pressure Monitoring System in a Catastrophically Damaged Area After a Disaster. J Clin Hypertens (Greenwich). 2017;19:26‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hoshide S, Nishizawa M, Okawara Y, et al. Salt Intake and Risk of Disaster Hypertension Among Evacuees in a Shelter After the Great East Japan Earthquake. Hypertension. 2019;74:564‐571. [DOI] [PubMed] [Google Scholar]
- 40. Nishizawa M, Fujiwara T, Hoshide S, et al. Winter morning surge in blood pressure after the Great East Japan Earthquake. J Clin Hypertens (Greenwich). 2019;21:208‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kario K, Tomitani N, Kanegae H, Yasui N, Nagai R, Harada H. The further development of out‐of‐office BP monitoring: Japan's ImPACT Program Project's achievements, impact, and direction. J Clin Hypertens (Greenwich). 2019;21:344‐349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kario K, Tomitani N, Kanegae H, et al. Development of a New ICT‐Based Multisensor Blood Pressure Monitoring System for Use in Hemodynamic Biomarker‐Initiated Anticipation Medicine for Cardiovascular Disease: The National IMPACT Program Project. Prog Cardiovasc Dis. 2017;60:435‐449. [DOI] [PubMed] [Google Scholar]
- 43. Gold DR, Mittleman MA. New insights into pollution and the cardiovascular system: 2010 to 2012. Circulation. 2013;127:1903‐1913. [DOI] [PubMed] [Google Scholar]
- 44. Alperovitch A, Lacombe JM, Hanon O, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three‐City study. Arch Intern Med. 2009;169:75‐80. [DOI] [PubMed] [Google Scholar]
- 45. Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995;345:353‐355. [DOI] [PubMed] [Google Scholar]
- 46. Kario K, Chen CH, Park S, et al. Consensus Document on Improving Hypertension Management in Asian Patients. Taking Into Account Asian Characteristics. Hypertension. 2018;71:375‐382. [DOI] [PubMed] [Google Scholar]


