Abstract
High blood pressure (BP) is the major cardiovascular‐risk factor for coronary artery disease (CAD), principally in young patients who have an important and increasing socioeconomic burden. Despite the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC‐7), recommended BP target <140/90 mm Hg for patients with stable CAD, in 2017 the American College of Cardiology and the American Heart Association (ACC/AHA) updated BP target to <130/80 mm Hg. We aimed to analyze the prevalence of BP control in patients with premature CAD using both criteria. In addition, antihypertensive therapy, lifestyle, clinical, and sociodemographic characteristics of the patients were evaluated in order to identify factors associated with the achievement of BP targets. The present study included 1206 patients with CAD diagnosed before 55 and 65 years old in men and women, respectively. Sociodemographic, clinical, and biochemical data were collected. The results indicate that 85.6% and 77.5% of subjects with premature CAD achieved JNC‐7 non‐strict and ACC/AHA strict BP target, respectively. Consistently, number of antihypertensive drugs and hypertension duration >10 years were inversely associated with BP targets, whereas total physical activity and smoking were directly associated with BP targets, regardless of BP criteria. Considering that age, gender, and hypertension duration are non‐modifiable cardiovascular‐risk factors, our results highlight the need for more effective strategies focused on increase physical activity and smoking cessation in young patients with CAD. These healthier lifestyles changes should favor the BP target achievement and reduce the socioeconomic and clinical burden of premature CAD.
Keywords: antihypertensive drugs, blood pressure, cardiovascular‐risk factors, hypertension, premature coronary artery disease
1. INTRODUCTION
High blood pressure (BP) is the major cardiovascular‐risk factor involved in death and years of life lost due to disability by coronary artery disease (CAD). 1 , 2 , 3 , 4 Moreover, hypertension have showed to confer 60% higher risk for premature CAD 5 and its prevalence in stable premature CAD reaches up to 50%; being greater than the prevalence of other independent cardiovascular‐risk factors, such as diabetes and dyslipidemia. 6 On the other hand, poor control of environmental risk factors, such as diet and physical activity, has been strongly related to uncontrolled BP levels in patients with primary or secondary cardiovascular prevention. 4 Although lowering BP reduces the recurrence of cardiovascular events, as well as the socioeconomic and clinical impact of premature CAD, 5 , 7 optimal BP target for secondary prevention has been uncertain and had led to inconsistent recommendations in clinical practice guidelines. 8 , 9 , 10 As noted, despite the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC‐7) recommended BP target to <140/90 mm Hg for patients with stable CAD, in 2017 the American College of Cardiology and the American Heart Association (ACC/AHA) reduced that BP target to <130/80 mm Hg. 8 , 10
Nowadays, the routine use of cardioselective beta‐blockers combined with any renin‐angiotensin‐aldosterone system (RAAS) inhibitor, either angiotensin‐converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) are considered as the first line of therapy for patients with established CAD. 8 , 11 However, patients with CAD may require other antihypertensive class of drugs, if the BP goal is not met. 8 , 12 Previous data indicate that nearly 70% of patients with cardiovascular disease had hypertension and <40% had BP values <130/80 mm Hg with the former JNC‐7 classification. 12 , 13 Nevertheless, with the recent ACC/AHA update, the current rates and degree of BP control in patients with stable CAD remain uncertain. Moreover, there are no updated reports of the treatment and control of BP in patients who have survived an acute coronary syndrome at early ages. Therefore, the aim of the present study was to analyze the prevalence of BP control in patients with premature CAD, using the previous JNC‐7 non‐strict and the current 2017 ACC/AHA strict criteria. Additionally, antihypertensive therapy, lifestyle, and sociodemographic characteristics of the patients were evaluated in order to identify the factors associated with the achievement of BP targets for secondary prevention.
2. MATERIALS AND METHODS
2.1. Patients
The population studied was selected from the Genetics of Atherosclerotic Disease (GEA) study database. This is a cross‐sectional study design to examine the genomic basis of CAD and to determine the association of traditional and emerging cardiovascular‐risk factors with clinical and subclinical CAD, in a sample of Mexican‐mestizo subjects. 14 The GEA study was approved by the Instituto Nacional de Cardiología Ignacio Chávez (INCICh) ethics committee on human research and was conducted according to the Declaration of Helsinki. All patients voluntarily signed an informed consent before participating in the study. The study included 1206 patients with a previous diagnosis of premature CAD, who were 35‐74 years old and were treated and enrolled between 2008 and 2013 at the INCICh. Premature CAD was defined as documented history of stable or unstable angina pectoris or acute myocardial infarction for more than 3 months before enrollment, history of percutaneous coronary intervention, coronary artery by‐pass grafting surgery, or angiographic demonstration of coronary stenosis >50%, diagnosed before 55 and 65 years of age in men and women, respectively. 15 Patients with current use of corticosteroids, established chronic kidney disease, hepatic, thyroid, or malignant disease before enrollment were excluded from the study.
All participants completed a medical examination in which previously trained staff interviewed and applied them standardized questionnaires to collect sociodemographic information, history of CAD, current drug therapy, and alcohol or tobacco consumption. All major classes of antihypertensive agents were recorded and included beta‐blockers, ACEIs, ARBs, thiazides, loop diuretics, spironolactone, calcium‐channel blockers (CCBs), and nitrates. Optimal pharmacological adherence was considered when the patient self‐reported treatment compliance by at least six days per week (>85%). 16 Current smoking status was defined when subjects self‐reported ≥1 cigarette consumption in the previous 12 months and included those who had quit within the past year. Former smokers were defined as those who had quit more than a year earlier. 17 The physical activity index was calculated using the Baecke questionnaire, 18 and the total physical activity was obtained from the sum of the physical activity during work, sports and recreational time. The questionnaire and physical activity indexes have been previously validated in an adult population. 19 The body mass index (BMI) was calculated as the weight in kilograms divided by the square of body height in meters; overweight was defined as BMI between 25‐29.9 kg/m2 and obesity as BMI ≥ 30 kg/m2. Systolic and diastolic blood pressures were measured after the patients remained seated for at least 10 minutes, and the average of the second and third measurements were used for the analysis. Hypertension was defined as BP values ≥140/90 mm Hg or prior documented diagnosis. 10 According to the non‐strict JNC‐7 guideline, systolic/diastolic BP values were categorized as normal (<120/80 mm Hg), pre‐hypertension (120‐139/80‐89 mm Hg), hypertension stage I (140 to 159/90 to 99 mm Hg), and hypertension stage II (≥160/100 mm Hg). 10 On the other hand, based on the strict 2017 ACC/AHA BP guideline, systolic/diastolic BP values were categorized as normal (<120/80 mm Hg), elevated BP (120‐129/<80 mm Hg), hypertension stage I (130‐139/80‐89 mm Hg), and hypertension stage II (≥140/90 mm Hg). 8 Considering BP targets for secondary prevention, non‐strict BP cutoff points were <140/90 mm Hg, whereas strict cut‐off points were <130/80 mm Hg. 8 , 10 Type 2 diabetes mellitus was defined when fasting plasma glucose were ≥126 mg/dL or when the patient self‐reported a previous diagnosis or current hypoglycemic drug use. 20
2.2. Biochemical analysis
Blood samples from the patients were collected after at least 10 hours of fasting. The glucose blood concentration, total cholesterol, high‐density lipoprotein cholesterol, and triglycerides, were evaluated in fresh samples, using standardized enzymatic procedures in a Hitachi autoanalyzer 902 (Hitachi LTD, Tokyo, Japan). The precision and accuracy of lipid measurements are evaluated regularly by the Center for Disease Control and Prevention (Atlanta, GA, USA). Low‐density lipoprotein cholesterol was calculated using the De Long et al's formula. 21
2.3. Statistical analysis
Descriptive statistical values of patients who achieved non‐strict or strict BP targets are expressed as mean ± standard deviation, median (interquartile range), or number of subjects (%). Statistical differences among these variables were tested using Student t, Mann‐Whitney U or chi‐squared test, respectively. In order to evaluate the independently associated factors with the achievement of BP control, inferences were made with multiple logistic regression analysis and they were expressed as odds ratio (95% confidence interval). Variables with biological plausibility or with scientific evidence that were different when comparing patients who achieved BP target or not, were used as covariates. Analyzes were performed using the SPSS v. 15.0 statistical package (SPSS Chicago, II.). P‐values < .05 were considered significant.
3. RESULTS
The study included 1206 patients with premature CAD from the GEA study database. The mean age of the study sample was 54 ± 8 years and 19.7% were women. Most of the subjects (87.6%) had an incident myocardial infarction and 12.4% had angina pectoris, with a median disease evolution of 2.4 years. Almost half of the patients (45%) underwent percutaneous coronary intervention with stenting and 9.9% a coronary artery by‐pass grafting surgery. Despite CAD diagnosis, 11.4% subjects were current smokers. Dietary‐healthy habits show that median total physical activity index was 7.50, median energy consumption was 2046 kcal per day and median alcohol intake was 1.3 g/d. Overall, the mean BMI of the patients was 29 ± 4 and only 17.0% had a BMI < 25 kg/m2.
The prevalence of hypertension previously diagnosed in the population studied was 69.3%, the mean systolic BP was 119 ± 19 mm Hg and diastolic BP was 72 ± 10 mm Hg. Using the former non‐strict JNC‐7 BP guideline, 85.6% of patients achieved the target BP, 28.9% of the population had pre‐hypertension and only 10.5% and 3.9% had stage I and II of hypertension, respectively (Figure 1A). Likewise, using the strict ACC/AHA BP guideline, 77.5% of patients achieved the ACC/AHA strict BP target, 20.7% of patients had elevated BP and although stage I of hypertension was similar to the observed with the JNC‐7 criteria, the prevalence of stage II was 13.0% (Figure 1B). Antihypertensive treatment was prescribed in 97.8% of the patients, and almost 95% of them referred treatment adherence >85%. Overall, 85.4% of the patients were taking beta‐blockers (from them, 95.4% were cardioselective beta‐blockers and 4.2% were combined alpha‐ and beta‐receptor beta‐blocker), 74.9% ACEIs, 13.8% ARBs, 8.8% thiazide diuretics, 5.8% loop diuretics, 6.8% spironolactone, 11.0% dihydropyridine‐CCBs, 5.1% non‐dihydropyridine‐CCBs, and 29.8% used nitrates. Moreover, 88.0% of the total population was under two or more different blood pressure‐lowering drugs; <5.0% were using beta‐blocker or any RAAS inhibitor alone, 38.3% were taking a beta‐blocker plus any RAAS inhibitor (two drugs), 28.3% a beta‐blocker plus any RAAS inhibitor plus other antihypertensive drug (three drugs), and 9.3% were using beta‐blocker plus any RAAS inhibitor plus two or more other drugs. Significant statistical differences were not detected in prevalence of drug treatment between JNC‐7 and ACC/AHA guidelines when analyzing BP target, normal BP, pre‐hypertension/elevated BP, and stage I or II of hypertension (Figure 2).
Figure 1.
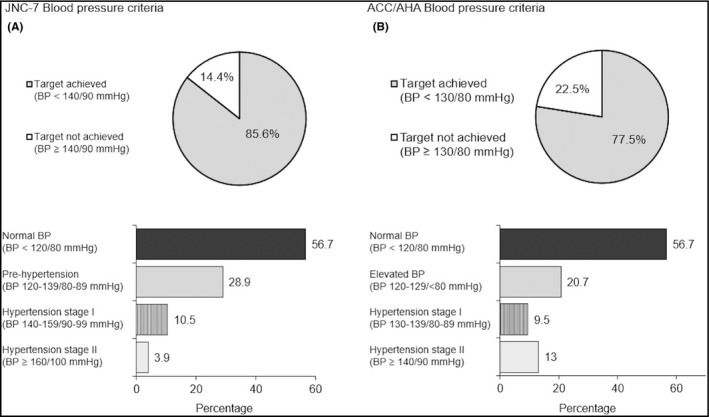
Prevalence of target blood pressure (BP) and classification in patients with premature coronary artery disease using JNC‐7 and ACC/AHA criteria. (A) JNC‐7 BP criteria: Normal BP: <120/80 mm Hg; pre‐hypertension: 120‐139/80‐89 mm Hg; hypertension stage I: 140‐159/90‐99 mm Hg; hypertension stage II: ≥160/ ≥100 mm Hg. (B) ACC/AHA 2017 BP criteria: normal BP: <120/80 mm Hg; elevated BP: 120‐129/<80 mm Hg; hypertension stage I: 130‐139/80‐89 mm Hg; hypertension stage II: ≥140/≥90 mm Hg
Figure 2.
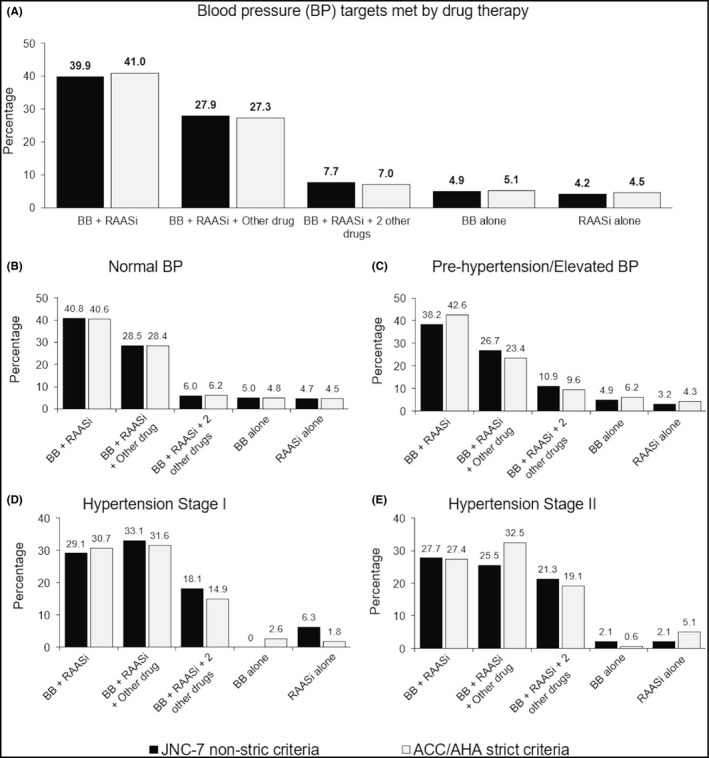
Prevalence of antihypertensive treatment in patients with premature coronary artery disease (CAD) categorized by JNC‐7 or ACC/AHA blood pressure (BP) target achievement for secondary prevention. (A) JNC‐7 BP <140/90 mm Hg or ACC/AHA BP < 130/80 mm Hg; (B) JNC‐7 and ACC/AHA BP < 120/80 mm Hg; (C) JNC‐7 BP 120‐139/80‐89 mm Hg or ACC/AHA BP 120‐129/<80 mm Hg; (D) JNC‐7 BP 140‐159/90‐99 mm Hg, ACC/AHA BP 130‐139/80‐89 mm Hg; (E) JNC‐7 BP ≥ 160/100 mm Hg or ACC/AHA BP ≥ 140/90 mm Hg. Beta‐blocker (BB): any beta‐blocker class used; renin‐angiotensin‐aldosterone system inhibitor (RAASi): angiotensin‐converting enzyme inhibitors or angiotensin II receptor blockers use; Other drug: Any other antihypertensive pharmacologic class (Thiazide or loop diuretics, calcium‐channel blockers or nitrates)
The clinical, sociodemographic, and biochemical characteristics of patients with premature CAD according to the JNC‐7 and ACC/AHA BP targets for secondary prevention are shown in Table 1. Patients who achieved non‐strict JNC‐7 BP target were younger, more likely to be men, to have higher percutaneous coronary interventions with stenting, education level, and smoking history. In addition, these patients were also characterized by lower serum creatinine levels, heart rate, and number of antihypertensive drugs, as well as lower prevalence of peripheral artery disease, diagnosis of hypertension and diabetes, unemployment, obesity, use of ARBs, diuretics, CCBs, and shorter duration of hypertension. Stratification of patients according to ACC/AHA guideline showed similar differences.
Table 1.
Clinical, sociodemographic and biochemical characteristics of patients with premature coronary artery disease (CAD), according to the achievement or not in systolic/diastolic blood pressure (BP) targets for secondary prevention
| JNC‐7 BP non‐strict cutoff points | ACC/AHA BP strict cut‐off points | |||||
|---|---|---|---|---|---|---|
| <140/90 mm Hg (n = 1032) | ≥140/90 mm Hg (n = 174) | P value | <130/80 mm Hg (n = 934) | ≥130/80 mm Hg (n = 272) | P value | |
| Age (y) | 54 ± 8 | 57 ± 8 | <.001 | 54 ± 8 | 56 ± 8 | <.001 |
| Female sex (%) | 17.2 | 35.4 | <.001 | 17.2 | 26.4 | <.001 |
| CAD evolution (y) | 2.4 (0.7‐6.5) | 2.4 (0.9‐5.8) | .566 | 2.2 (0.7‐6.4) | 2.8 (0.8‐6.5) | .115 |
| CAD diagnosis | ||||||
| Angina pectoris (%) | 12.1 | 14.0 | .485 | 12.0 | 13.4 | .525 |
| Myocardial infarction (%) | 87.9 | 86.0 | 88.0 | 86.6 | ||
| Time since last event (y) | 1.6 (0.6‐5.2) | 2.1 (0.7‐5.6) | .086 | 1.5 (0.6‐5.0) | 2.4 (0.7‐5.8) | .004 |
| PCI with stenting (%) | 46.1 | 37.8 | .046 | 46.4 | 41.3 | .119 |
| CABG surgery (%) | 9.6 | 11.6 | .427 | 9.7 | 10.2 | .789 |
| Stroke (%) | 1.2 | 1.2 | .940 | 1.0 | 1.6 | .443 |
| Peripheral artery disease (%) | 1.0 | 4.3 | .001 | 0.9 | 2.8 | .014 |
| Left ventricular ejection fraction (%) | 51 (44‐60) | 51 (43‐60) | .910 | 52 (44‐60) | 50 (43‐59) | .404 |
| Creatinine (mg/dL) | 0.96 ± 0.21 | 1.01 ± 0.25 | .010 | 0.96 ± 0.21 | 0.99 ± 0.23 | .013 |
| Type 2 diabetes (%) | 33.5 | 53.7 | <.001 | 33.4 | 44.1 | .001 |
| Married (%) | 78.9 | 80.5 | .639 | 79.4 | 78.3 | .664 |
| Education | ||||||
| Less than high school (%) | 42.1 | 55.5 | .005 | 42.4 | 48.1 | .208 |
| High school or college (%) | 57.9 | 44.5 | 57.6 | 41.9 | ||
| Unemployed (%) | 27.2 | 39.6 | .001 | 28.1 | 31.1 | .309 |
| Monthly income ≤60.0 USD$ (%) | 21.4 | 24.8 | .318 | 21.6 | 22.3 | .799 |
| Smoking status | ||||||
| Current (%) | 12.4 | 5.5 | 12.4 | 8.7 | ||
| Former (%) | 64.3 | 53.0 | <.001 | 65.4 | 55.6 | <.001 |
| Never (%) | 23.3 | 41.5 | 22.2 | 35.7 | ||
| Total physical activity index | 7.6 (6.8‐8.5) | 7.1 (6.4‐8.2) | .001 | 7.6 (6.7‐8.5) | 7.4 (6.4‐8.4) | .003 |
| Total kilocalories per day | 2062 (1672‐2572) | 1975 (1551‐2376) | .032 | 2062 (1662‐2567) | 2008 (1642‐2457) | .202 |
| Alcohol intake (g/d) | 1.34 (0.58‐4.80) | 1.15 (0.38‐4.80) | .430 | 1.34 (0.38‐4.80) | 1.34 (0.58‐4.80) | .639 |
| BMI (kg/m2) | 28.7 ± 4.2 | 30.0 ± 5.1 | .001 | 28.6 ± 4.2 | 29.6 ± 4.7 | .001 |
| <25 kg/m2 (%) | 17.4 | 13.4 | 18.0 | 13.7 | ||
| 25‐29.9 kg/m2 (%) | 47.9 | 42.1 | .048 | 47.9 | 45.0 | .042 |
| ≥30.0 kg/m2 (%) | 34.7 | 44.5 | 34.1 | 41.3 | ||
| Diagnosed hypertension (%) | 64.4 | 100 | <.001 | 61.2 | 92.2 | <.001 |
| Antihypertensive treatment (%) | 97.6 | 99.4 | .142 | 97.6 | 98.4 | .388 |
| Number of drugs (n) | 2.3 ± 0.9 | 2.7 ± 1.0 | <.001 | 2.3 ± 0.9 | 2.6 ± 1.0 | <.001 |
| Treatment adherence >85% (%) a | 94.1 | 93.5 | .762 | 94.8 | 92.4 | .176 |
| Duration of hypertension | ||||||
| <6 y (%) | 56.6 | 40.5 | 58.3 | 44.6 | ||
| 6‐10 y (%) | 23.3 | 19.6 | <.001 | 23.0 | 21.9 | <.001 |
| >10 y (%) | 20.0 | 39.9 | 18.7 | 33.4 | ||
| Systolic blood pressure (mm Hg) | 113 ± 12 | 153 ± 16 | <.001 | 110 ± 10 | 142 ± 17 | <.001 |
| Diastolic blood pressure (mm Hg) | 70 ± 8 | 85 ± 11 | <.001 | 68 ± 7 | 83 ± 9 | <.001 |
| Heart rate (bpm) | 65 ± 11 | 68 ± 11 | .001 | 64 ± 11 | 68 ± 11 | <.001 |
| Beta‐blockers (%) | 85.8 | 82.9 | .388 | 86.1 | 83.5 | .262 |
| Cardioselective (%) | 95.2 | 97.1 | 95.1 | 96.3 | ||
| Non‐cardioselective (%) | 0.4 | 0.0 | .540 | 0.4 | 0.4 | .734 |
| Combined α‐ and β‐receptor (%) | 4.4 | 2.9 | 4.5 | 3.4 | ||
| ACE Inhibitors (%) | 75.0 | 73.8 | .733 | 75.9 | 72.0 | .163 |
| ARBs (%) | 12.6 | 20.7 | .018 | 12.0 | 18.4 | .016 |
| Diuretics (%) | 17.6 | 30.5 | <.001 | 17.5 | 24.6 | .006 |
| Thiazide or thiazide‐type (%) | 7.4 | 18.3 | <.001 | 7.1 | 13.7 | .002 |
| Loop diuretics (%) | 5.4 | 8.5 | .230 | 5.5 | 6.5 | .228 |
| Aldosterone antagonist (%) | 6.8 | 6.1 | .733 | 6.9 | 6.2 | .672 |
| Calcium‐channel blockers (%) | 14.3 | 28.0 | <.001 | 13.1 | 24.6 | <.001 |
| Dihydropyridines (%) | 9.1 | 23.2 | 8.4 | 18.3 | ||
| Non‐dihydropyridines (%) | 5.2 | 4.9 | <.001 | 4.8 | 6.2 | <.001 |
| Nitrates (%) | 28.8 | 35.4 | .221 | 28.2 | 34.0 | .132 |
| Cholesterol (mg/dL) | ||||||
| Total | 163 ± 45 | 174 ± 47 | .003 | 162 ± 44 | 171 ± 48 | .004 |
| Low‐Density Lipoprotein | 95 ± 39 | 103 ± 39 | .010 | 94 ± 38 | 100 ± 40 | .033 |
| High‐Density Lipoprotein | 39 ± 10 | 40 ± 12 | .042 | 39 ± 10 | 40 ± 12 | .053 |
| Triglycerides (mg/dL) | 158 (115‐212) | 177 (130‐230) | .012 | 157 (114‐211) | 171 (128‐227) | .002 |
Abbreviations: ARBs, Angiotensin receptor blockers. BMI, body mass index; CABG, coronary artery by‐pass grafting; PCI, percutaneous coronary intervention.
Treatment adherence was defined as self‐reported consumption of lipid‐lowering treatment. Variables are shown as mean ± SD or median (interquartile range) or percentages. P value: Student t test or Mann‐Whitney U or chi‐square.
Multivariable analysis using variables with biological plausibility (total of kilocalories intake, and antihypertensive treatment adherence), or with scientific evidence of difference among patients who achieved BP target or not (age, sex, education level, employed status, diabetes presence, smoking status, physical activity, BMI, number of antihypertensive drugs, and duration of hypertension), shows that compared with patients who did not achieved the JNC‐7 non‐strict BP target (reference), those with controlled BP were significantly associated with lower BMI, number of antihypertensive drugs, prevalence of longer hypertension duration (>10 years), diabetes, and female sex. On the other hand, total physical activity index and smoking were positively associated with the achievement of BP target (Figure 3A). In order to know the effect of gender on these associations, an additional analysis indicates that non‐strict BP target achievement was principally associated with HT duration >10 years [0.264 (0.109‐0.641)], TPA index [1.421 (1.002‐2.015]), and diabetes [0.371 (0.164‐0.843)] in women (Figure S1 (A)); whereas BMI [0.943 (0.891‐0.997)] and number of drugs [0.615 (0.454‐0.832]) were associated with BP target achievement in men (Figure S1 (B)). Using patients with BP ≥ 130/80 mm Hg as reference, lower number of drugs, duration of hypertension, and age were associated with the achievement of the 2017 ACC/AHA BP target. As noted with the non‐strict BP control, total physical activity index and smoking were directly associated with ACC/AHA strict BP control (Figure 3B). The specific gender analysis shows that in addition to HT duration >10 years [0.317 (0.137‐0.733)] and TPA index [1.525 (1.106‐2.103)], current smoking [(9.539 (1.032‐88.131)] was associated with strict BP target achievement in women (Figure S1 (C)), while number of drugs [0.666 (0.518‐857)], current [2.403 (1.059‐5.455)] and former [1.665 (1.007‐2.752)] smoking, and age (0.968 (0.939‐0.999)] were independently associated with BP target achievement in men (Figure S1 (D)).
Figure 3.
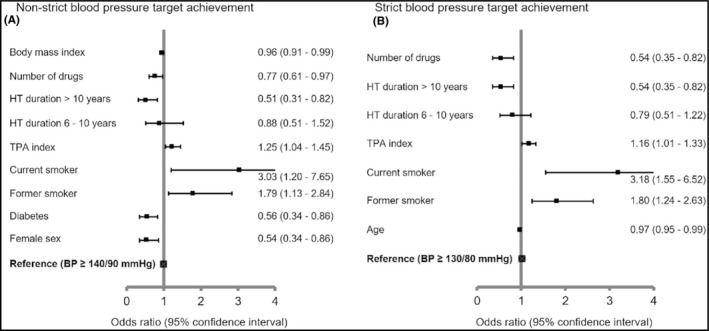
Variables associated with the achievement of blood pressure (BP) target for secondary prevention using the JNC‐7 non‐strict and the ACC/AHA strict criteria. Variables associated with the achievement of JNC‐7 non‐strict BP target (panel A) and variables associated with the achievement of ACC/AHA strict BP target (panel B). Logistic regression analysis included age, sex, diabetes, education, unemployment, smoking status, total physical activity (TPA) index, total kilocalories intake per day, body mass index (BMI), number of antihypertensive drugs, hypertension evolution, antihypertensive treatment adherence >85%, and heart rate as covariates
4. DISCUSSION
Despite the increase in life expectancy, recent data indicate that global burden of CAD at young ages has gradually increased and it is mainly attributable to increased BP levels. 2 , 3 , 4 The current study documents that control of BP was achieved in 85.6% and 77.5% of patients with premature CAD, using the JNC‐7 or ACC/AHA guidelines, respectively. Given the clinical characteristics of CAD, the most common antihypertensive drugs used in our studied population were beta‐blockers (85.4%) and ACEIs (74.9%). In addition, 75.9% of patients were using the combined prescription of beta‐blocker plus any RAAS inhibitor, as the suggested first line of antihypertensive therapy for cardiovascular secondary prevention. 8 Besides the pharmacological therapy, factors inversely associated with BP control were age, female sex, diabetes, number of antihypertensive drugs, BMI, and hypertension duration >10 years. Moreover, total physical activity index and smoking were directly associated with BP target achievement.
Over the last decades, several studies have focused to determine the optimal BP target for patients with stable CAD. 7 , 22 , 23 , 24 Overall, every 10 mm Hg reduction in systolic BP has shown to reduce the risk of major cardiovascular events by 20%, recurrent coronary events by 17% and all‐cause mortality by 13%. 22 However, in patients with established CAD under antihypertensive treatment, BP levels <120/70 mm Hg have been found to be associated with higher rates of cardiovascular events, acute renal failure and electrolyte disturbances. 7 , 24 , 25 Thus, BP values used to define control for patients with CAD in the 2017 ACC/AHA guideline, whatever their age and comorbidities, seems to be an adequate goal for the management of hypertension but whether it is ideal is still debatable. 8 As a matter of fact, results from the NHANES in the United States showed that prevalence of hypertension in patients with cardiovascular disease increased from 72.1% using JNC‐7 criteria to 79.3% using the ACC/AHA criteria. In addition, these results reported that, among adults taking antihypertensive treatment, 39.0% did not meet the JNC‐7 BP target compared with 53.4% that were above the ACC/AHA BP target. 13 Similarly, the present analysis shows that compared with the JNC‐7 guideline, the implementation of the 2017 ACC/AHA guideline exposed lower prevalence of controlled BP. However, our data highlight higher prevalence of BP targets achievement among patients with premature CAD, using both criteria. Noteworthy, 97.8% of patients included in the present study were taking antihypertensive drugs and nearly 95% referred good compliance to treatment, which could partially explain the higher rates of BP control in these patients. In addition, it is important to point out that, by design of the GEA study, patients had an acute coronary event at a premature age, which could also contribute to the higher rates of BP target attainment. This hypothesis could be supported by finding the inverse independent association of BP targets achievement with age and duration of the disease, and its direct association with higher total physical activity (Figure 3).
Beta‐blockers and RAAS blockade with ACEIs or ARBs remain the standard of care for patients with CAD, since these drugs have shown cardioprotective, anti‐arrhythmogenic, and anti‐remodeling properties beyond their antihypertensive effects. 8 , 26 , 27 , 28 Moreover, the 2017 ACC/AHA BP guideline states that concurrent use of 3 antihypertensive drugs of different classes with uncontrolled BP or controlled BP with 4 or more drugs is defined as treatment‐resistant hypertension. 8 Compared with other cohorts of patients with CAD, the present analysis shows higher rates of beta‐blockers (85.4% vs ~76.2%) and ACEIs (74.9% vs ~58.8%), but lower ARBs (13.8% vs ~22.6%), CCBs (13% vs ~14.9%), and diuretics (23% vs ~28.55%) prescription. 12 , 29 , 30 In addition, our results underline that mean number of combined antihypertensive drugs was 2.7 ± 1 and it was inversely associated with controlled BP, regardless the BP target criteria. This finding suggests that prevalence of apparent treatment‐resistant hypertension in these patients might be high, and it could supported by the prevalence of subjects with premature CAD and uncontrolled BP using 3 or more antihypertensive drugs (Figure 2). 8 , 31 Due to selection criteria of the GEA study, which excluded the most common causes of treatment‐resistant hypertension, further analyses are needed to evaluate the reasons of this condition in premature CAD. On the other hand, Bangalore et al reported that, in a sample of patients with CAD, 88.9% had BP < 140/90 mm Hg and those with controlled BP were more likely to be men, younger, to have lower BMI and prevalence of diabetes. 12 Despite patients of the present analysis were 6 years younger and had higher BMI and prevalence of current smoking, diabetes, previous myocardial infarction, and antihypertensive therapy, we found similar univariate associations. Nevertheless, in a multivariable analysis using the JNC‐7 guideline, BP target achievement was associated with lower BMI, number of drugs, prevalence of hypertension duration >10 years, diabetes, and female sex. Likewise, the use of the ACC/AHA guideline shows that number of drugs, hypertension duration >10 years, total physical activity, and smoking were consistently associated with the achievement of BP goal, and age was the only variable associated with ACC/AHA BP target achievement. Interestingly, in an additional multivariable analysis stratifying patient by decade of life (Table S1), we found that number of antihypertensive drugs was associated with the non‐strict BP target, whereas HT duration >10 years and former smoking were associated with the strict BP target achievement during the fifth decade of life. On the other hand, HT duration >10 years and diabetes were associated with non‐strict BP target and TPA index with strict BP target achievement in patients within the sixth decade of life. Finally, among patients in their seventh decade of life, TPA index, former smoking, and female sex were associated with non‐strict BP target achievement, whereas TPA index and female sex were independently associated with strict BP target achievement. These results suggest that a well drug therapy management could improve the BP control in the youngest patients with CAD, even in those with long hypertension duration. Although this improvement could not be maintained in older patients, adequate physical activity and quit smoking could bring higher benefits in them. These later results are supported by multivariable gender analyses (Figure S1), where BP target achievement was found to be associated with physical activity in women, BMI in men, and smoking habits in both genders. Moreover, the analyses also showed that in women, diabetes itself was strongly associated with BP target achievement, which could partially explain the BP control and female sex association in older patients.
Physical activity and weight loss have been widely associated with reduction in BP levels and lower incidence of recurrent cardiovascular events and all‐cause mortality in patients with CAD. 7 , 8 , 9 , 10 , 17 Our results indicate that lower BMI was independently associated with the achievement of JNC‐7 BP target and highlights that higher total physical activity is consistently associated with the achievement of BP target using both criteria. On the other hand, smoking triggers an acute increase in BP and has been thought to be associated with higher risk for hypertension. 32 , 33 Nonetheless, some studies have reported that patients at high‐cardiovascular risk have lower BP values in current smokers. 32 , 34 Consistent with this, our analysis shows that current and former smoking was associated with higher probability to achieve BP targets (Figure 3). It seems plausible that patients with history of smoking and premature CAD have quit smoking since the occurrence of the incident cardiovascular event and, therefore, it might explain the lower BP values attainment. 32 , 33 Further studies are needed in order to analyze the pattern of smoking and BP in very high‐risk patients. Despite our findings suggest that current and former smokers have increased odds for BP control, smoking should be strictly avoided because it is unequivocally a leading cause of preventable cardiovascular mortality. 17 , 32
An important strength of our analysis is that the population with premature CAD selected had an ample characterization, which allowed us analyzing the composite impact of sociodemographic, clinical, and biochemical data related to the achievement of former and recent BP guideline‐based recommendations.
A limitation of the present study is that our population was extracted from a single tertiary center of cardiology in Mexico, and this may interfere with the interpretation of the results with the whole premature CAD population due to the possible bias of the same medical inertia of our center. Furthermore, it is important to point out that selected sample was from mestizo‐Mexican origin and the results may not apply for other ethnic groups. Another limitation is the cross‐sectional design of our study, which does not allow knowing whether reducing BP target in patients with premature CAD is related to higher adverse events or cardiovascular event‐free rates. Finally, we did not evaluate the frequencies of full antihypertensive drug dosing; neither rates of their side effects such as acute renal failure, electrolyte disturbances, or angioedema. Moreover, it was not possible to know the patient drugs intake through direct evaluation; however, we applied standardized questionnaires to collect information about pharmacological prescription to properly analyze the association of therapies with BP target achievement.
In summary, the present study indicates that 85.6% and 77.5% of subjects with premature CAD achieved JNC‐7 non‐strict and ACC/AHA strict BP target, respectively. Consistently, number of antihypertensive drugs and hypertension duration >10 years were inversely associated with BP targets, whereas total physical activity and smoking were directly associated with BP targets, regardless BP criteria. Considering that age, gender, and disease duration are non‐modifiable risk factors, our results highlight that more effective preventive strategies should be implemented to address healthier lifestyles in order to reduce the socioeconomic and clinical burden of premature CAD.
CONFLICT OF INTEREST
The authors have nothing to disclose.
AUTHORS CONTRIBUTIONS
Jorge‐Galarza Esteban and Juárez‐Rojas Juan Gabriel conceived the project, researched and analyzed data, contributed to discussion, and wrote the manuscript. Martínez‐Sánchez Froylan David wrote the manuscript, researched and analyzed data, and contributed to discussion. Javier‐Montiel Ceasr Iridiani, Medina‐Urrutia Aida, Posadas‐Romero Carlos, González‐Salazar Maria Del Carmen. Osorio‐Alonso Horacio, and Arellano‐Buendía Abraham Said researched data and contributed to discussion. Juárez‐Rojas Juan Gabriel is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supporting information
Fig S1
Table S1
ACKNOWLEDGMENTS
The authors of the present paper thank the personal of Department of Endocrinology, as well as the will of the patients to participate in the study.
Jorge‐Galarza E, Martínez‐Sánchez FD, Javier‐Montiel CI, et al. Control of blood pressure levels in patients with premature coronary artery disease: Results from the Genetics of Atherosclerotic Disease study. J Clin Hypertens. 2020;22:1253–1262. 10.1111/jch.13942
REFERENCES
- 1. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2019 update: a report from the American Heart Association. Circulation. 2020;141(2):e33‐e528. [DOI] [PubMed] [Google Scholar]
- 2. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all‐cause mortality, and cause‐specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659‐1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murray CJL, Vos T, Lozano R, et al. Disability‐adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197‐2223. [DOI] [PubMed] [Google Scholar]
- 4. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217‐223. [DOI] [PubMed] [Google Scholar]
- 5. Poorzand H, Tsarouhas K, Hozhabrossadati SA, et al. Risk factors of premature coronary artery disease in Iran: a systematic review and meta‐analysis. Eur J Clin Invest. 2019;49(7):e13124. [DOI] [PubMed] [Google Scholar]
- 6. Mohammad AM, Jehangeer HI, Shaikhow SK. Prevalence and risk factors of premature coronary artery disease in patients undergoing coronary angiography in Kurdistan, Iraq. BMC Cardiovasc Disord. 2015;15:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vidal‐Petiot E, Ford I, Greenlaw N, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016;388(10056):2142‐2152. [DOI] [PubMed] [Google Scholar]
- 8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2275‐2279. [DOI] [PubMed] [Google Scholar]
- 9. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507‐520. [DOI] [PubMed] [Google Scholar]
- 10. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206‐1252. [DOI] [PubMed] [Google Scholar]
- 11. American Diabetes Association . 10. Cardiovascular Disease and risk management: standards of medical care in diabetes‐2019. Diabetes Care. 2019;42(Suppl 1):S103‐S123. [DOI] [PubMed] [Google Scholar]
- 12. Bangalore S, Fayyad R, Laskey R, et al. Prevalence, predictors, and outcomes in treatment‐resistant hypertension in patients with coronary disease. Am J Med. 2014;127(1):71‐81.e1. [DOI] [PubMed] [Google Scholar]
- 13. Muntner P, Carey RM, Gidding S, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137(2):109‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Villarreal‐Molina T, Posadas‐Romero C, Romero‐Hidalgo S, et al. The ABCA1 gene R230C variant is associated with decreased risk of premature coronary artery disease: the genetics of atherosclerotic disease (GEA) study. PLoS One. 2012;7(11):e49285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1‐87. [DOI] [PubMed] [Google Scholar]
- 16. Vonbank A, Drexel H, Agewall S, et al. Reasons for disparity in statin adherence rates between clinical trials and real‐world observations: a review. Eur Heart J Cardiovasc Pharmacother. 2018;4(4):230‐236. [DOI] [PubMed] [Google Scholar]
- 17. Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364(9438):937‐952. [DOI] [PubMed] [Google Scholar]
- 18. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936‐942. [DOI] [PubMed] [Google Scholar]
- 19. Hertogh EM, Monninkhof EM, Schouten EG, Peeters PH, Schuit AJ. Validity of the modified Baecke questionnaire: comparison with energy expenditure according to the doubly labeled water method. Int J Behav Nutr Phys Act. 2008;5:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. American Diabetes Association . 2. Classification and diagnosis of diabetes: standards of medical care in diabetes‐2019. Diabetes Care. 2019;42(Suppl 1):S13‐S28. [DOI] [PubMed] [Google Scholar]
- 21. DeLong DM, DeLong ER, Wood PD, Lippel K, Rifkind BM. A comparison of methods for the estimation of plasma low‐ and very low‐density lipoprotein cholesterol. The lipid research clinics prevalence study. JAMA. 1986;256(17):2372‐2377. [PubMed] [Google Scholar]
- 22. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta‐analysis. Lancet. 2016;387(10022):957‐967. [DOI] [PubMed] [Google Scholar]
- 23. ACCORD Study Group . Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575‐1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. SPRINT Research Group . A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373(22):2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Burnier M, Oparil S, Narkiewicz K, Kjeldsen SE. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden? Blood Press. 2018;27(2):62‐65. [DOI] [PubMed] [Google Scholar]
- 26. Chrysant SG, Chrysant GS. Dual renin‐angiotensin‐aldosterone blockade: promises and pitfalls. Curr Hypertens Rep. 2015;17(1):511. [DOI] [PubMed] [Google Scholar]
- 27. Dézsi CA, Szentes V. The real role of β‐blockers in daily cardiovascular therapy. Am J Cardiovasc Drugs. 2017;17(5):361‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ripley TL, Saseen JJ. β‐blockers: a review of their pharmacological and physiological diversity in hypertension. Ann Pharmacother. 2014;48(6):723‐733. [DOI] [PubMed] [Google Scholar]
- 29. Gandhi S, Dorian P, Greenlaw N, et al. Characteristics and evidence‐based management of stable coronary artery disease patients in Canada compared with the rest of the world: insights from the CLARIFY registry. Can J Cardiol. 2014;30(1):132‐137. [DOI] [PubMed] [Google Scholar]
- 30. Ferrari R, Ford I, Greenlaw N, et al. Geographical variations in the prevalence and management of cardiovascular risk factors in outpatients with CAD: data from the contemporary CLARIFY registry. Eur J Prev Cardiol. 2015;22(8):1056‐1065. [DOI] [PubMed] [Google Scholar]
- 31. Hannah‐Shmouni F, Gubbi S, Spence JD, Stratakis CA, Koch CA. Resistant hypertension: a clinical perspective. Endocrinol Metab Clin North Am. 2019;48(4):811‐828. [DOI] [PubMed] [Google Scholar]
- 32. Liu X, Byrd JB. Cigarette smoking and subtypes of uncontrolled blood pressure among diagnosed hypertensive patients: paradoxical associations and implications. Am J Hypertens. 2017;30(6):602‐609. [DOI] [PubMed] [Google Scholar]
- 33. Li G, Wang H, Wang K, et al. The association between smoking and blood pressure in men: a cross‐sectional study. BMC Public Health. 2017;17(1):797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vidal‐Petiot E, Sorbets E, Bhatt DL, et al. Potential impact of the 2017 ACC/AHA guideline on high blood pressure in normotensive patients with stable coronary artery disease: insights from the CLARIFY registry. Eur Heart J. 2018;39(43):3855‐3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Table S1


