Abstract
Increasing life expectancy in the population means that the prevalence of hypertension in China will increase over the coming decades. Although awareness and control rates have improved, the absolute rates remain unacceptably low. Cardiovascular disease (CVD) is the biggest killer in China, and sharp increases in the prevalence of CVD risk factors associated with rapid lifestyle changes will contribute to ongoing morbidity and mortality. This highlights the importance of effectively diagnosing and managing hypertension, where home blood pressure monitoring (HBPM) has an important role. Use of HBPM in China is increasing, particularly now that Asia‐specific guidance is available, and this out‐of‐office BP monitoring tool will become increasingly important over time. To implement these recommendations and guidelines, a Web‐based and WeChat‐linked nationwide BP measurement system is being established in China. Local guidelines state that both HBPM and ambulatory blood pressure monitoring should be implemented where available. In China, hypertension is managed most often using calcium channel blockers, followed by angiotensin receptor blockers or angiotensin‐converting enzyme inhibitors. Key barriers to hypertension control in China are low awareness and control rates.
Keywords: Asia, China, home blood pressure, hypertension, management
1. CARDIOVASCULAR DISEASE INCIDENCE AND HYPERTENSION MANAGEMENT IN CHINA
Hypertension control in China has significantly improved over the past decade because of increasing health insurance coverage. According to the most recent China nationwide hypertension survey of 451 755 adults in 2012‐2015, the prevalence of hypertension was 27.9%, and hypertension awareness, treatment, and control rates were 46.9%, 40.7%, and 15.3%, respectively.1 The estimated total number of hypertensive patients among Chinese adults was 244.5 million. Compared with the preceding survey conducted in 2002 (n = 141 892), rates of hypertension prevalence, treatment, and control had increased by 48.4%, 64.8%, and 150.8%, respectively.2, 3 Despite relative increases of 55.3% and 50.4%, respectively, in awareness and control rates in treated hypertensive patients, absolute rates remained unacceptably low.3
Although there have been improvements in the prevention and control of hypertension in China, the overall cardiovascular disease (CVD) prevalence and mortality rates remain high. According to 2017 statistics, the estimated total number of patients with CVD in China was 290 million, including 13 million prevalent strokes and 11 million prevalent coronary heart disease.4 CVD was the most common cause of death. A systematic analysis of the Global Burden of Disease Study 2013 showed that the age‐standardized CVD mortality rate in China decreased slightly (by 21%) from 389/100 000 in 1990 to 307/100 000 in 2013.5 This decrease in CVD mortality was to a large extent attributable to decreases in mortality from hemorrhagic stroke (−37.7%) and hypertensive heart disease (−41.3%), whereas ischemic stroke and ischemic heart disease mortality rates increased by 28.8% and 2.6%, respectively.5 These changes likely reflect an improvement in hypertension control and worsening of several other major cardiovascular risk factors, such as diabetes mellitus, dyslipidemia, and obesity.
Due to increasing life expectancy, the prevalence of hypertension will inevitably increase over the next few decades. In addition, rapid changes in lifestyle in China, characterized by a high‐salt, high‐fat, high‐sugar, and high‐calorie diet and low physical activity, have resulted in a sharp increase in the prevalence of diabetes mellitus, dyslipidemia, and obesity over the past decade.6 This will undoubtedly increase the prevalence of hypertension and the challenges of managing hypertension.
2. CURRENT STATUS OF HBPM IN THE MANAGEMENT OF HYPERTENSION IN CHINA
Home blood pressure monitoring (HBPM) is an effective approach to improve awareness and control of hypertension. It may help identify white‐coat (uncontrolled) hypertension and masked (uncontrolled) hypertension and evaluate long‐term blood pressure (BP) variability (BPV).7, 8 Due to the tighter relationship of BP with cardiovascular events, higher prevalence of masked uncontrolled hypertension, higher morning BP levels, and greater BPV, home BP monitoring is likely to be of greater importance in Asian than in Western populations.9 HBPM is also recommended to monitor the effectiveness of antihypertensive therapy, support dose adjustment, and provide information about treatment adherence.7, 8 Several studies have reported that even when clinic BP is well controlled, masked uncontrolled morning hypertension with residual cardiovascular risk should still be a target for the management of hypertension.10
Home blood pressure monitoring use in China has increased over the last decade, especially after publication of the China expert consensus document in 2012.7 With the publication of the HOPE Asia Network recommendations and guidelines,8, 9 and the Chinese Hypertension League guidelines on HBPM (personal communication), this out‐of‐clinic BP measurement will play a more important role in the management of hypertension in China over time. To implement these recommendations and guidelines, a Web‐based and WeChat‐linked nationwide BP measurement system is being established in China.3 Hopefully, patients will be able to measure their BP at home regularly in a standardized manner, with careful clinical input from the system.
3. CHINA SUB‐ANALYSIS OF THE ASIABP@HOME STUDY
The control status of both clinic and home BP has recently been investigated in 1437 treated hypertensive patients from 12 Asian countries/regions in the AsiaBP@Home study.11, 12 The same validated BP monitor and the same standardized measurement procedure were used for clinic and home BP monitoring in all study participants. According to the conventional diagnostic criteria of 140/90 mm Hg for clinic BP and 135/85 mm Hg for home BP, the prevalence of controlled hypertension was 46% and the prevalence of white‐coat, masked and sustained uncontrolled hypertension was 23%, 9%, and 22%, respectively.12 Applying the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) classification thresholds,13 the prevalence of controlled hypertension and masked uncontrolled hypertension decreased to 26% and 6%, respectively.12 The prevalence of sustained uncontrolled hypertension and white‐coat uncontrolled hypertension increased to 40% and 28%, respectively.12 Looking only at study participants from China (n = 197), the corresponding proportions of patients were 35%, 24%, 12%, and 29%, respectively, using conventional thresholds, and 19%, 22%, 9%, and 50%, respectively, using the new ACC/AHA criteria (Figure 1). These results showed that, regardless of the BP threshold, using only clinic BP as a target will miss almost 10% of patients with masked uncontrolled hypertension and result in over‐treatment of more than 20% of patients with white‐coat uncontrolled hypertension. Therefore, HBPM is essential for the precise titration and evaluation of antihypertensive therapy.
Figure 1.
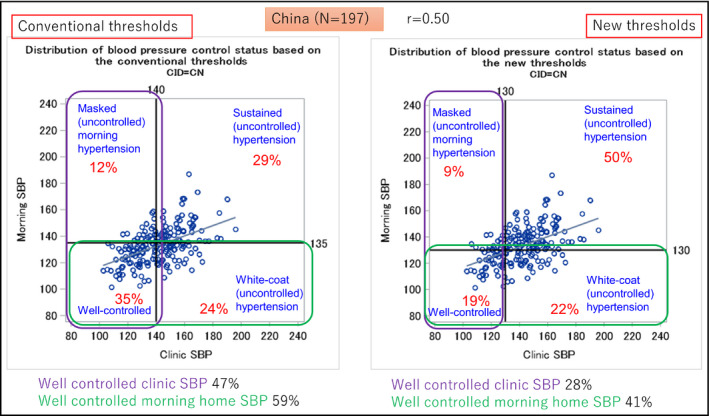
Distributions of blood pressure (BP) control status based on different clinic and morning home BP thresholds in the China sub‐analysis from the AsiaBP@Home study. Left panel represents the results based on cutoff values of 140 mm Hg for clinic systolic BP (SBP) and 135 mm Hg for home SBP. Right panel represents the results based on cutoff values of 130 mm Hg for both clinic SBP and home SBP
4. POSITIONING OF HBPM IN THE 2018 CHINESE HYPERTENSION GUIDELINES
In the recently published 2018 Chinese guidelines for the management of hypertension,14 clinic BP is recommended for the diagnosis and classification of hypertension and therapeutic monitoring, with a threshold of 140/90 mm Hg. The 2018 Chinese guidelines also recommend the use of 24‐hour ambulatory BP monitoring (ABPM) and HBPM in the management of hypertension. Out‐of‐office BP, if available, should be measured in all patients for the identification of white‐coat hypertension and masked hypertension in untreated individuals and white‐coat and masked uncontrolled hypertension in treated hypertensive patients, especially those with resistant hypertension.
Home blood pressure monitoring may play a crucial role in patients with a clinic BP in the range of 130‐139/85‐89 mm Hg or 140‐159/90‐99 mm Hg. In the former case, HBPM may help identify those with masked hypertension, which confers high cardiovascular risk.15 In the latter case, HBPM may help identify those with white‐coat hypertension, which has a high prevalence and is often treated, but there is little evidence of benefit from antihypertensive therapy in low‐risk patients.16
To improve the use of HBPM in the management of hypertension, a specific guideline was recently presented in the Fifth Scientific Meeting on China Blood Pressure Monitoring. HBPM was recommended at three levels according to BP. If BP without treatment remains normal from the most recent measurement, BP can be measured at home at least once a year. If BP is controlled with antihypertensive therapy, BP can be measured at home at least once a week. For the initial diagnosis of hypertension or in newly diagnosed or uncontrolled hypertension, BP should be measured 2‐3 times in the morning and evening for 5‐7 consecutive days.
5. TRADITIONAL ANTIHYPERTENSIVE THERAPY AND POPULAR ANTIHYPERTENSIVE DRUGS IN CHINA
The 2018 Chinese hypertension guidelines recommend the use of calcium channel blockers (CCBs), angiotensin‐converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), β‐blockers and diuretics as the main antihypertensive therapies.14 In primary care clinical practice, the most commonly used antihypertensive medications in China have been reported to be CCBs (55.2%), followed by ACE inhibitors or ARBs (28.5%) and diuretics (9.4%).17 The most commonly used two‐drug combination was CCB + ACE inhibitor or ARB (34.7%), followed by ACE inhibitor or ARB + diuretic (14.4%) and CCB + β‐blocker (11.5%).17 In the 2017 May Measurement Month project,18 information on the use of antihypertensive medication was collected in 19 523 hypertensive patients in China.19 In those receiving antihypertensive monotherapy, 44.4% were taking CCBs, 22.0% ACE inhibitors or ARBs, 2.7% diuretics, and 2.7% β‐blockers.19
Compared with more than a decade ago, there are several major changes in the use of antihypertensive medication. One is the substantial decrease in the use of traditional single‐pill combination of central sympatholytics, such as reserpine or clonidine, with hydrochlorothiazide.20 Another is the substantial increase in the use of CCBs and ACE inhibitors or ARBs. These newer agents are often long acting and have better tolerability, and therefore, patient compliance is better.
6. SPECIFIC CONCERNS AND PERSPECTIVES FOR HYPERTENSION MANAGEMENT IN CHINA
Low awareness in hypertensive patients and the low control rate in treated hypertensive patients are the two major barriers to hypertension control. To tackle these, the Chinese Hypertension League recently started several initiatives in China.3 First, a Web‐based and WeChat‐linked home BP measurement system is being established nationwide. This system will support both HBPM and BP measurement in public places, such as shopping malls, office buildings, and factories. It is hoped that this system will allow individuals to measure their BP regularly and receive feedback about whether it is normal or not. Secondly, Web‐based and WeChat‐linked intelligent excellence centers for hypertension are being established in various hospitals in China. The system will include four platforms: clinic automated BP measurement, Web‐based and WeChat‐linked ABPM and HBPM, comprehensive risk assessment for the identification of organ damage and high‐risk patients, and measurement of plasma aldosterone concentration for the identification of primary and secondary aldosteronism. After establishment of these two systems over the next few years, it is hoped that awareness and control rates will both increase to 70%. Subsequently, the hypertension control rate may reach 50%. It is then probably time to consider 130/80 mm Hg as the therapeutic target for antihypertensive treatment, and perhaps even as the diagnostic threshold for hypertension, in China.
CONFLICT OF INTEREST
Dr Wang reports receiving lecture and consulting fees from Bayer, Omron, Pfizer, Servier, and Takeda. The other authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Ji‐Guang Wang contributed to the conception and design of the work. Qian‐Hui Guo prepared the first draft of the manuscript together with Ji‐Guang Wang. Ji‐Guang Wang and Yu‐Qing Zhang contributed to the data acquisition, analysis, and interpretation for the work. All authors critically revised the manuscript and gave the final approval.
ACKNOWLEDGMENTS
English language editing assistance was provided by Nicola Ryan, independent medical writer, funded by the HOPE Asia Network.
Guo Q‐H, Zhang Y‐Q, Wang J‐G. Asian management of hypertension: Current status, home blood pressure, and specific concerns in China. J Clin Hypertens. 2020;22:475–478. 10.1111/jch.13687
REFERENCES
- 1. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137:2344‐2356. [DOI] [PubMed] [Google Scholar]
- 2. Li LM, Rao KQ, Kong LZ, et al. A description on the Chinese national nutrition and health survey in 2002. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:478‐484. [PubMed] [Google Scholar]
- 3. Wang JG. Unique approaches to hypertension control in China. Ann Transl Med. 2018;6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen WW, Gao RL, Liu LS, et al. Report of cardiovascular disease in China: 2017 summary. Chin Circ J. 2018;33:1‐8 (in Chinese). [Google Scholar]
- 5. Zhou M, Wang H, Zhu J, et al. Cause‐specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251‐272. [DOI] [PubMed] [Google Scholar]
- 6. Rosengren A, Teo K, Rangarajan S, et al. Psychosocial factors and obesity in 17 high‐, middle‐ and low‐income countries: the Prospective Urban Rural Epidemiologic study. Int J Obes (Lond). 2015;39:1217‐1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chinese Hypertension Committee of the Chinese Medical Doctors Association , Chinese Hypertension League , Chinese Society of Cardiology of the Chinese Medical Association . Home blood pressure monitoring: a consensus document of China. Chin J Hypertens. 2012;2012:525‐529. [Google Scholar]
- 8. Kario K, Park S, Buranakitjaroen P, et al. Guidance on home blood pressure monitoring: a statement of the HOPE Asia Network. J Clin Hypertens (Greenwich). 2018;20:456‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Park S, Buranakitjaroen P, Chen CH, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249‐258. [DOI] [PubMed] [Google Scholar]
- 10. Wang JG, Kario K, Park JB, Chen CH. Morning blood pressure monitoring in the management of hypertension. J Hypertens. 2017;35:1554‐1563. [DOI] [PubMed] [Google Scholar]
- 11. Kario K, Tomitani N, Buranakitjaroen P, et al. Rationale and design for the Asia BP@Home study on home blood pressure control status in 12 Asian countries and regions. J Clin Hypertens (Greenwich). 2018;20:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kario K, Tomitani N, Buranakitjaroen P, et al. Home blood pressure control status in 2017–2018 for hypertension specialist centers in Asia: results of the Asia BP@Home study. J Clin Hypertens (Greenwich). 2018;20:1686‐1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199‐2269.29146533 [Google Scholar]
- 14. Writing Group of 2018 Chinese Guidelines for the Management of Hypertension , Chinese Hypertension League , Chinese Society of Cardiology , Chinese Medical Doctor Association Hypertension Committee , Hypertension Branch of China International Exchange and Promotive Association for Medical and Health Care , Hypertension Branch of Chinese Geriatric Medical Assocation . Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2018;2019(24):1‐46. [Google Scholar]
- 15. Zhang DY, Guo QH, An DW, Li Y, Wang JG. A comparative meta‐analysis of prospective observational studies on masked hypertension and masked uncontrolled hypertension defined by ambulatory and home blood pressure. J Hypertens. 2019;37(9):1775‐1785. [DOI] [PubMed] [Google Scholar]
- 16. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white‐coat, masked and sustained hypertension versus true normotension: a meta‐analysis. J Hypertens. 2007;25:2193‐2198. [DOI] [PubMed] [Google Scholar]
- 17. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population‐based screening study (China PEACE Million Persons Project). Lancet. 2017;390:2549‐2558. [DOI] [PubMed] [Google Scholar]
- 18. Beaney T, Schutte AE, Tomaszewski M, et al. May Measurement Month 2017: an analysis of blood pressure screening results worldwide. Lancet Glob Health. 2018;6:e736‐e743. [DOI] [PubMed] [Google Scholar]
- 19. Chen X, Xu SK, Li Y, et al. May Measurement Month 2017: an analysis of blood pressure screening results in China‐East Asia. Eur Heart J Suppl. 2019;21:D37‐d39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sheng CS, Liu M, Kang YY, et al. Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Hypertens Res. 2013;36:824‐828. [DOI] [PubMed] [Google Scholar]


