Abstract
Out‐of‐office blood pressure (BP) monitoring appears to be a very useful approach to hypertension management insofar it allows to obtain multiple measurements in the usual environment of each individual, allows the detection of hypertension phenotypes, such as white‐coat and masked hypertension, and appears to have superior prognostic value than the conventional office BP measurements. Out‐of‐office BP can be obtained through either home or ambulatory monitoring, which provide complementary and not identical information. Home BP monitoring yields BP values self‐measured in subjects' usual living environment; it is an essential method for the evaluation of almost all untreated and treated subjects with suspected or diagnosed hypertension, best if combined with telemonitoring facilities, also allowing long‐term monitoring. There is also increasing evidence that home BP monitoring improves long‐term hypertension control rates by improving patients' adherence to prescribed treatment. In Latin American Countries, it is widely available, being relatively inexpensive, and well accepted by patients. Current US, Canadian, Japanese, and European guidelines recommend out‐of‐office BP monitoring to confirm and refine the diagnosis of hypertension.
Keywords: adherence to treatment, arterial hypertension diagnosis, blood pressure measurement, home blood pressure, hypertension treatment, self‐measurement
1. INTRODUCTION
Recent US, Canadian, and European Guidelines for hypertension management1, 2, 3 have clearly emphasized the importance of out‐of‐office blood pressure (BP) monitoring (M), in daily management of hypertensive patients. In particular, evidence has been obtained that use of either self‐monitoring by patients at home (HBPM) and/or 24‐hour ambulatory BP monitoring (ABPM) should be recommended for confirmation of the diagnosis and for long‐term management of hypertension. Moreover, out‐of‐office BPM has been shown to allow the identification of specific hypertension phenotypes, such as white‐coat and masked hypertension, and strong evidence is available that it is superior to the conventional office BP measurements (OBP) in predicting development of hypertension mediated organ damage (HMOD) as well as the occurrence of cardiovascular events.1, 3, 4, 5, 6, 7
How far and how much can this evidence be translated into daily practice application in Countries with diverse resource availability and with a large diversity in health care system organization and funding, such as the Latin American Countries?
This paper is aimed at summarizing the data available on the indications and feasibility of HBPM in Latin America and at discussing a number of issues related to its application in daily practice in such settings, with the final goal to provide recommendations for implementation of these approaches in the management of Hypertension in this part of the world.
Measurement of BP in the office is the most commonly performed part of the physical examination also in Latin America (LA). However, there is growing evidence that this approach to BP assessment is no longer sufficient in the diagnosis as well as in the management of hypertension. Indeed, over the last years a number of studies have shown that out‐of‐office BP monitoring, in particular when based on HBPM, is important to confirm the existence of a high BP condition and is superior to office BP values when assessing the risk of cardiovascular morbidity and mortality in the setting of hypertension.8 Thus, it is not surprising that HBPM is increasingly being used in clinical practice also in LA. Currently, approximately 65% of Northern Americans with hypertension own a home BP monitor, while 30% of LA individuals are experienced in its application.9 In addition, use of HBPM has been associated with a greater engagement of hypertensive patients in the management of their condition and with better BP control, in particular when associated with telemonitoring facilities.10, 11 Hypertension control is even better when telemonitoring is combined with counseling and educational support.12
In this paper, we focus on a number of aspects relevant to the clinical use and interpretation of HBPM in LA Countries.
1.1. Advantages and applicability of HBPM in the management of hypertensive patients in Latin America
HBPM, by actively involving hypertensive patients in the management of their condition, is acknowledged as an approach offering a significant contribution to BP control, when compared to conventional BP monitoring..12, 13 HBP values are also more reproducible than OBP measurements, and are characterized by a better prognostic value.5 HBPM may also contribute to reduce the cost of hypertension care.3, 14
In 2008, both in the United States and in Europe strong recommendations were published to promote use of HBPM as a routine approach to BP assessment in the majority of patients with hypertension, in particular if treated, thus supporting its application even in low‐income countries.5, 9, 15 Acknowledged advantages of HBPM are summarized in Box 1.16
Box 1. Advantages of home blood pressure monitoring.
Advantages of home blood pressure monitoring
Superiority to OBP in predicting subclinical target organ damage and cardiovascular events (similar to ABPM).
Sensibility in detecting white‐coat and masked hypertension‐related phenotypes in both untreated and treated patients (in the latter case termed white‐coat resistant and masked uncontrolled hypertension phenomena, respectively).
In treated hypertensive patients improvement of long‐term adherence to antihypertensive drug treatment and hence of hypertension control rates.
These indications were then further supported by the NICE 2011 guidelines17 for the clinical management of primary hypertension in adults,3 which recommended that if clinic BP is 140/90 mm Hg or higher, out‐of‐office BP should be offered to confirm the diagnosis of hypertension. In all persons unable to tolerate ABPM, HBPM was proposed as a suitable alternative.
More recently, US guidelines have strongly recommended out‐of‐office BPM for confirming the diagnosis of hypertension1, 18 an indication which has been provided also by the 2018 ESC‐ESH hypertension guidelines.3 Evidence obtained over the last years has further supported the prognostic role of HBPM, with morning HBP in particular appearing to be a strong predictor of future cardiovascular and stroke events.19, 20
The cost‐effectiveness of HBPM vs OBP measurements was also investigated.7, 21, 22 The results suggest that reimbursement of HBPM would be cost beneficial from an insurer's perspective, when focusing on diagnosing and treating hypertension.23 However, in spite of these encouraging analyses, in low‐ and middle‐income countries one of the most important current limitations for implementation of out‐of‐office BPM in daily practice, including both HBPM and even more so ABPM, is their limited accessibility due to economic problems and lack of coverage by health care systems. Thus, to face these difficulties, adequate reimbursement for use of out‐of‐office BPM, in particular for purchase of HBPM devices, appears to be a mandatory requirement in these settings. This would allow expanding use of this approach, also in LA, favoring a more precise assessment of the different hypertension phenotypes. A stronger support by health care systems would be important also because, as suggested by the Australian guidelines, a larger use of HBPM would require physicians (or other health care providers) to spend incrementally more time in training patients to use HBPM devices, in transferring HBPM data to patient's health records, and in interpreting these additional datasets to formulate more effective management plans.24
2. METHODOLOGICAL ASPECTS
2.1. HBPM
HBPM should be preferentially performed by the patients themselves in their home and/or work environment.7, 25 Practical recommendations to be provided to patients for optimal HBPM implementation regarding device25, 26, 27 and cuff selection as well as on measurement conditions and procedures25, 28 are provided in Box 2.
Box 2. Practical recommendations to be provided to patients for optimal HBPM performance. Adapted from Peixoto et al29 by permission.
Practical recommendations to be provided to patients for optimal HBPM
Use a reliable monitor, after checking that it has been validated according to internationally accepted validation protocols.30
Periodically bring your machine to your doctor's office to make sure it is working properly when compared to calibrated machines used in the office. Do this once a year or any time you suspect the machine may not be working well.
Use only devices with arm cuffs. Wrist cuff devices are not as accurate and should not be used if not in selected cases when arm cuffs cannot be reliably applied (eg, severe obesity with very large arm size).
Make sure to rest for about 5 minutes before measuring your BP. Sit comfortably, refrain from talking during the measurements, and avoid caffeinated beverages or smoking before measuring BP.
Check your BP twice at each time—both values should be recorded, and the average of the two values will also be calculated.
Typically, a period of 1 week of monitoring before each clinic visit is enough to give your doctor a good idea of your BP control. BP should be measured twice daily: in the morning before taking medications and in the evening before dinner. The average of the 7 days (or of 6 days after excluding the first one) will be used to determine the degree of HBP control.
2.2. Data reporting
A minimum of 12 measurements (when HBPM is performed over 3 days) and a maximum of 28 measurements (when HBPM is performed over 7 days) are needed to achieve clinically relevant information on HBP levels. Current guidelines recommend measuring BP levels at home over 7 days, with at least two morning and two evening measurements, before each clinic visit.5 For clinical decision‐making, the average of all these values should be used with the exception of the first day, which should be discarded.5 Programmable HBPM devices have been recently introduced that additionally provide a few measures of nighttime BP, thus widening the clinical applications of HBPM to the assessment of sleep BP levels whenever ABPM is not available.5, 9
Brazilian Guidelines are in line with the above indications and recommend HBPM to be performed over 5 days with 3 measurements in the morning and 3 in the afternoon (discarding first day) or alternatively over 7 days.31 Similar indications have been provided by the very recent LASH guidelines on hypertension management.32
2.3. Home blood pressure monitoring and telemedicine
The imprecise reporting of self‐measured BP values by patients and the fast development of information and communication technologies have stimulated development of HBP telemonitoring facilities. Telemonitoring of HBP has been shown to help in better defining HBP cutoff values for the identification of white‐coat and masked hypertension.33 Evidence is available that HBP telemonitoring may improve patients' adherence and fight physicians' inertia, facilitating hypertension control.10, 34 As already mentioned, combination of remote telemonitoring of HBP values with patients' education and empowerment might further improve correlation of self‐measured BP with casual36 blood pressure measurement, might reduce patients' alarm reaction33 and might improve hypertension control.35
Recent evidence suggests that even better results could be obtained through use of mobile and digital health technologies, as shown by encouraging data on improved hypertension control rates obtained through use of the ESH CARE Application developed by the Italian and European Societies of Hypertension.37, 38
3. PROGNOSTIC VALUE
HBPM measurements have been shown to better predict hypertension mediated organ damage as compared to traditional OBP readings. As an example, HBP correlates better with left ventricular hypertrophy and presence of atherosclerosis than OBP.39, 40
Several studies have shown HBP to be a better prognostic indicator with respect to risk of cardiovascular mortality and cardiovascular events than OBP.23, 41
Moreover, in patients with chronic kidney disease followed over a mean of 3.5 years, HBP was a stronger predictor of end‐stage renal disease or death compared with BP values obtained in the clinic.42 The predictive value of HBPM on outcome has also been compared to that of ABPM in a systematic review summarizing available studies.43 Conclusion of this analysis was that HBPM and ABPM correlated similarly with cardiovascular events and mortality. Moreover, targeting HBP or ABP values with treatment resulted in similar outcomes.43
4. DIAGNOSTIC AND THERAPEUTIC THRESHOLDS
4.1. Diagnostic thresholds
HBP values <130/80 mm Hg may be considered normal, while a mean HBP ≥ 135/85 mm Hg is considered elevated. These values refer to the average of HBP readings performed for 3‐7 days prior to a clinic or office visit, with 2 readings taken 1‐2 minutes apart in the morning and in the evening5. Threshold values for hypertension diagnosis when using different types of BP measurement recommended by the Latin American Society of Hypertension are provided in Table 1. These values are in agreement with those indicated by the 2018 ESC/ESH Hypertension guidelines.3
Table 1.
Office, home, and ambulatory blood pressure Thresholds proposed for hypertension diagnosis by the task force of the Latin American Society of Hypertension
| SBP (mm Hg) | DBP (mm Hg) | ||
|---|---|---|---|
| Office BP | ≥140 | or | ≥90 |
| Home BP | ≥135 | or | ≥85 |
| Ambulatory BP | |||
| Daytime | ≥135 | or | ≥85 |
| Nighttime | ≥120 | or | ≥70 |
| 24 h | ≥130 | or | ≥80 |
Reproduced from32 by permission.
Abbreviation: BP, Blood Pressure.
Some additional information on possible thresholds for stratifying patients based on their different BP levels when focusing on clinic, home or ambulatory BP was provided by the 2017 US Hypertension guidelines.1 It should be noticed, however, that these values are not outcome‐based, but are rather based on statistical analysis of data provided in previous papers which compared office, ambulatory, and home BP levels. See Table 2.
Table 2.
Corresponding values of SBP/DBP for clinic, HBPM, daytime, nighttime, and 24‐h ABPM measurements
| Clinic | HBPM |
Daytime ABPM |
Nighttime ABPM |
24‐h ABPM |
|---|---|---|---|---|
| 120/80 | 120/80 | 120/80 | 100/65 | 115/75 |
| 130/80 | 130/80 | 130/80 | 110/65 | 125/75 |
| 140/90 | 135/85 | 135/85 | 120/70 | 130/80 |
| 160/100 | 145/90 | 145/90 | 140/85 | 145/90 |
Reproduced by permission from Whelton et al.1
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; DBP, diastolic blood pressure; HBPM, home blood pressure monitoring; SBP, systolic blood pressure.
4.2. Therapeutic thresholds
HBP thresholds for hypertension in high‐risk patients might be lower than 135/85 mm Hg. Although the target HBP to be achieved with treatment should logically be below the threshold used to diagnose hypertension, information on outcome‐based target HBP levels is still missing, being currently explored by ongoing studies.44, 45 Indeed, no clear indication based on outcome is yet available on what the HBPM targets for treatment might be.3
5. CLINICAL INDICATIONS
HBPM is commonly rated as better tolerated by patients than ABPM.46 HBPM has been reported to refine cardiovascular risk stratification in individuals classified as with no or mild risk of cardiovascular disease by office BP measurements (found to be in the optimal, normal or high‐normal OBP categories), by identifying subjects with masked hypertension.22
Evidence on the ability of HBP to identify WCH and MH was provided by the PAMELA‐study in which the initial diagnosis of WCH (elevated office BP with normal 24‐hour BP mean or home BP) was reassessed 10 years later. The study showed largely similar results between HBPM and ABPM for identifying WCH, sustained hypertension, true normotension, and masked hypertension, even if a substantial percentage of subjects changed from one category to another over time, including progression to sustained hypertension.27
Interestingly, HBP readings seem to correlate well with ABPM values. There is indeed evidence of a reasonable agreement between these methods, given that when average HBP values are ≥ 135/85 mm Hg, there is an 85% probability that ABP values will also be in the high BP range.28
Classification of patients in different BP categories based on the combination of office and out‐of‐office BP is shown in Figure 1.
Figure 1.
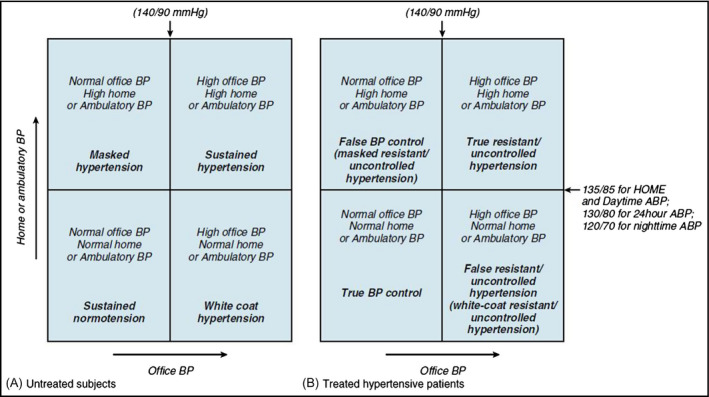
Different blood pressure phenotypes in treated and untreated hypertensives, respectively, defined by comparing office and out‐of‐office BP measurements. Reproduced from Parati et al5 by permission
6. HOME BLOOD PRESSURE MONITORING IN SPECIAL PATIENTS' GROUPS
6.1. Children: devices, diagnostic thresholds, schedule
The definition of hypertension in children is arbitrary and is based on the analysis of a normal distribution of BP values in healthy children. A child with BP values higher than the 95th percentile according to gender, age, and height compared to a reference population is defined hypertensive. Tables classifying BP in children based on such a distribution are available.47, 48
Also in LA self‐measurement of BP at home has been proposed in children and adolescents. However, available HBPM data from children are scanty. As in adults, also in children correct self‐measurement requires two BP measurements to be taken within a few minutes, both in the morning and in the evening, at least for 3 consecutive days.49 HBP correlates closely with daytime ambulatory BP values also in this age group and has superior reproducibility than office BP, similar to that of ABPM in adults. HBP is lower than daytime ambulatory BP in children and adolescents. Some evidence is available that home BP in children correlates with target organ damage (TOD) better than office BP and that it may also better reflect the effect of risk factors for high BP, such as family history or obesity.50
The criteria to define hypertension based on HBP are also based on HBP values being higher than or equal to the 95th percentile for sex and height, as long as HBP values are lower than the threshold values for hypertension accepted for adults (average 135/85 mm Hg). Several issues about the clinical application of this method in children and adolescents, including availability of validated devices, remain underinvestigated, however.48 In particular, not much information on HBPM in children has been published so far in Latin America. Some data concerning masked and white‐coat prevalence as well as normalcy values are available.51, 52 The main issues related to HBPM in children and adolescents have been addressed by Lurbe et al47 and are summarized in Box 3 and Box 4.
Box 3. Methodological aspects for Home Blood Pressure Monitoring in children and adolescents.
Adapted from Lurbe et al47 by permission
Methodological aspects for HBPM in children and adolescents
Measured daily on at least 3‐4 days, preferably on 7 consecutive days in the mornings as well as in the evenings.
Measured in a quiet room, with the patient in the seated position, back and arm supported, after 5 minutes of rest.
Two measurements per occasion taken 1‐2 minutes apart.
The HBP value to be used for clinical management is the average of these readings, with exclusion of the first monitoring day.
Box 4. Indications for clinical use of home blood pressure monitoring in children and adolescents.
Adapted from Lurbe et al47 by permission
Indications for HBPM in Children and adolescents
All young patients receiving antihypertensive medication.
Suspicion of white‐coat hypertension.
Conditions where strict blood pressure control is mandatory (high‐risk patients).
Clinical trials.
6.2. Elderly people
Both ambulatory and home BP could play also in the elderly a complementary role in guiding clinical decisions toward management of hypertension. A comparable degree of association between markers of hypertension‐modulated organ damage, such as left ventricular hypertrophy, albuminuria, or carotid intima‐medial thickness, and HBP or 24‐hour ambulatory BP has been reported.53
6.3. Obese people
HBP is important in detecting Masked Hypertension and White‐coat Hypertension in this group. Only a few studies have provided data on the prevalence and covariates of Masked Hypertension in obese cohorts, in whom nocturnal hypertension could be more frequent due to a higher prevalence of obstructive sleep apnea.54
There is considerable uncertainty as to the diagnostic accuracy of HBPM based on use of arm cuff devices in obese people, and hence on which might be the best reliable alternative approach. Use of a regular cuff in obese individuals leads to overestimating BP, thus guidelines recommend to use a cuff of appropriate size.5 However, use of an appropriate cuff in obese individuals should consider not only the arm circumference but also its shape. In particular, a conical shaped arm, common in obese individuals, introduces additional difficulties in fitting the cuff to the arm, thus being responsible for further inaccuracies.55 The use of wrist devices may help avoiding these difficulties and may be considered for HBPM in obese individuals, but additional studies and improved technology are needed.56 Also, the use of a cuff on subjects' forearm has been suggested, although this approach might lead to some overestimation of properly measured arm cuff BP.57, 58, 59
6.4. Patients with arrhythmias
Patients with atrial fibrillation (AF) or other arrhythmias may not be good candidates for home BP monitoring. This is because the oscillometric BP monitoring devices recommended for use at home may not be able to give accurate measurements in patients with uncontrolled tachyarrhythmia. Stergiou and colleagues60 assessed the diagnostic accuracy of an automated device for self‐home blood pressure monitoring, which implements an algorithm for AF detection. A modified, automated oscillometric device for self‐home BP monitoring with an AF detector was used to carry out triplicate BP measurements in subjects with sinus rhythm, AF, and non‐AF arrhythmias. These data suggest that an electronic device for self‐home BP monitoring, which implements an algorithm for AF diagnosis has a good diagnostic accuracy and might, therefore, be used as a reliable screening test for the early diagnosis of arrhythmias in hypertension.61
Several guidelines recommend opportunistic screening for AF in subjects aged ≥65 years using pulse palpation during routine BP measurement. However, this method clearly has limited diagnostic accuracy. A specific algorithm for AF detection during automated BP measurements was developed and implemented in an oscillometric device (Microlife Watch BP Home‐A (https://bihsoc.org/bp-monitors/for-specialist-use/). In 2013, the NICE recommended this device for AF screening during routine OBP measurement in primary care in subjects with 65 years or older. A systematic review and meta‐analysis of the available evidence on diagnostic accuracy of this algorithm were performed. Six studies (including a total of 2332 patients) were found, which investigated the accuracy of AF detection using the Microlife BP monitor, with an estimated pooled sensitivity of 0.98 and specify of 0.92. AF detection with routine automated BP measurement is thus a reliable screening approach, particularly in the elderly, although a precise diagnosis requires confirmation by electrocardiography. Paroxysmal AF might also be detected by routine automated home or ambulatory BP monitoring, although with lesser accuracy.62 No specific data on this issue have been published in LA.
6.5. Pregnancy
Potential advantages and limitations of HBPM in pregnant women are summarized in Box 5.
Box 5. Advantages and limitations of HBPM in pregnancy. Adapted from Hodgkinson JA, et al63 by permission.
Advantages and limitations of HBPM in pregnancy
Potential advantages
Increased accuracy.
Patient friendly.
Potential to free health care professional time or reduce clinic visits.
Potential to identify white‐coat hypertension.
Potential limitations
Few monitors have been validated for use in pregnancy.
Poor understanding of normal blood pressure levels in pregnancy.
No diagnostic thresholds from home monitoring to identify pre‐eclampsia or gestational hypertension.
False reassurance if woman with white‐coat hypertension subsequently develops true hypertension in pregnancy.
No evidence that earlier detection of high blood pressure through home monitoring will alter pregnancy outcomes.
No evidence on optimal frequency and timing of home monitoring in pregnancy.
May increase women's anxiety or risk of excessive medicalization of care.
Self‐monitoring of BP in pregnancy appears to be more effective in hypertension management in pregnant women than making more frequent clinic visits, hospital admission, or ambulatory monitoring.64
Self HBP monitoring for a minimum of 3 days and ideally for 7 days is currently recommended also in pregnant women, although the evidence supporting this indication is not particularly compelling. Moreover, only few data are available on diagnostic thresholds for HBPM in pregnancy, comparing clinic thresholds with self‐monitored BP pressure in pregnancy, and were obtained from studies affected by important methodological weaknesses.65, 66
6.6. Chronic kidney disease
An important proportion of HBP monitors used by patients seen in different nephrology units in LA are inaccurate (data unpublished). A validation of the accuracy and safety of the HBPM devices, already in use in nephrology high‐risk patients, is thus recommended, before relying on their measurements for clinical decisions.67
Out‐of‐office BP monitoring (ABPM and HBPM) is a useful tool to evaluate the efficacy of hypertension treatment in chronic kidney disease patients and has been shown to be particularly useful to explore the association between BP levels and interdialytic symptoms. HBP has been reported also to be superior to clinic BP for titration of antihypertensive therapy in these high‐risk patients.68, 69
Decisions about dialysis prescription and timing of antihypertensive drug administration can in fact be made more effectively after understanding the duration of BP control (or even by identifying low BP levels) after each dialysis session. HBPM is a valuable adjunct in this assessment and is often used in nephrology practice also in LA.42
In dialysis patients, HBPM is a very informative and inexpensive technique, which has the ability to provide comparable information on BP profile between morning and evening as well as on prognosis.
Usefulness of HBPM has also been investigated following kidney transplantation. HBP in kidney transplant recipients more closely correlated with ABPM data than did office BP measurements (72% concordance vs 54% discordance). Moreover, using ABPM as reference data, HBP was both more sensitive and specific at detecting hypertension than office‐based BP measurements in patients receiving a kidney transplantation.70
6.7. Diabetes
Data are available that out‐of‐office BP monitoring allows for an improved management of hypertension in individuals with type 2 diabetes.71, 72 In spite of this, it is not yet clear how low home BP target level should be in these patients, because of lack of evidence from intervention trials. In the latest version of LASH hypertension clinical management guidelines,73 the goal clinic BP in type 2 diabetes was raised to 140/85 mm Hg and HBPM was suggested also for confirming hypertension control. In diabetic patients, studies have shown that HBP values, particularly readings taken in the morning, are better predictors of target organ damage than OBP measurements alone.
7. ADVANTAGES AND LIMITATIONS OF HBPM
General advantages and limitations of HBPM are summarized in Box 6, while possible specific indications for HBPM and ABPM are reported in Box 7.
Box 6. Advantages and limitations of HBPM.
Adapted from Jacob et al67 by permission
Advantages and limitations of HBPM
Advantages
Can take multiple readings over an extended period of time.
Avoids White‐coat reaction to BP measurement.
Reproducible.
Predicts CV morbidity and mortality better than OBP.
Can diagnose White‐coat and masked hypertension.
Allows patients to better understand hypertension management.
Telemonitoring allows remote monitoring by health care professionals.
Detects increased BP variability.
Limitations
Some devices have been found to be inaccurate.
Cuff placement can affect accuracy.
May induce anxiety and excessive monitoring.
Risk of treatment change by patients based on causal home measurements without doctor's guidance.
Lack of nocturnal recording, so far.
Not yet reimbursed by insurance companies in many countries.
Box 7. Specific Indications for HBPM and ABPM.
Adapted, modified, from Peixoto et al29 by permission
Specific Indications for HBPM and ABPM
Home BP Monitoring
Any patient with hypertension
To rule out White‐coat hypertension
To rule out masked hypertension
Evaluation of resistant hypertension
Evaluation of medication‐related hypotensive symptoms
Evaluation of mid‐term, day by day BP variability
Improvement of patients' adherence to treatment
Ambulatory BP monitoring
To rule out white‐coat hypertension
To rule out masked hypertension
Evaluation of resistant hypertension
Evaluation of medication‐related hypotensive symptoms
Evaluation of short term and diurnal BP variability
Assessment of nocturnal blood pressure
Evaluation of autonomic dysfunction
The reproducibility of HBPM is better than that of traditional OBP measurements, and it overcomes some limitations affecting OBP readings such as digit preference and observer bias.74
7.1. HBPM and hypertensin diangosis
While performing ABPM and/or HBPM for detecting the presence of white‐coat hypertension (WCH) and to identify the presence of true hypertension and masked hypertension in all patients with uncomplicated stage 1 and 2 hypertension before starting antihypertensive drug should be encouraged, there still uncertainty on when HBPM and ABPM should be applied, respectively. ABPM is currently considered the standard method for confirming the diagnosis of hypertension in clinical practice (see below).7 However, ABPM is less easily accepted by patients than HBPM and needs trained clinic staff and specialized equipment, which are not commonly available, in particular in LA. Moreover, compared with 24‐hour ABPM, HBPM is less expensive, much more widely available also in LA, and provides information about the day‐to‐day variability of blood pressure.75
On the other hand, there is evidence supporting the superior prognostic value of ABPM vs HBPM. Although HBPM shares many of the advantages of ABPM, including a cost‐effective approach to the diagnosis of hypertension, it should not be considered as a substitute but rather as a complement to ABPM.29 Box 7 provides some indications on the use of HBPM and ABPM in hypertension management.
7.2. HBPM and blood pressure control by treatment
HBP may contribute in many ways to improve the management of hypertensive patients, improving compliance with prescribed treatment and BP control.76
It is reasonable to expect that more active participation of patients in the care of their health, as stimulated by use of HBPM, might improve therapeutic compliance, which may suggest to systematically combining HBPM with other approaches aimed at improving patients' adherence to treatment.76 Data are available that patients properly adhering to the instructions for HBPM have a better response to antihypertensive treatment.76 There is indeed evidence that HBPM is associated with improved BP control,77 being also associated with marginally lower medical cost.78 Such a benefit, as mentioned above54 is particularly evident when HBPM is accompanied with remote telemonitoring and adequate patients' education and empowerment.
HBPM proves to be an appropriate tool for assessing drug efficacy because it has the advantage of providing multiple readings over a 24‐hour period as well as over multiple days, during either a short or a long‐term follow‐up.79
HBPM appears, in particular, to be a suitable approach in low‐mid income regions of the world, even when they are characterized by a limited level of education of the population.
7.3. HBPM: research applications in clinical trials
HBPM should also be considered as one of the best approaches to BP measurement not only in daily practice but also in a clinical trial setting, because of its reproducibility, strong outcome predicting power and the possibility of monitoring BP under treatment over relative long time periods, also comparing the degree of BP control in the morning and in the evening.
8. CONCLUSIONS
HBPM is a simple, inexpensive methodology that offers significant clinical advantages over routine OBP measurements. Large evidence has indicated that HBPM is a strong predictor of cardiovascular risk with superior prognostic value over conventional OBP measurements in predicting initiation, establishment, and progression of subclinical organ damage, and development of fatal and non‐fatal CV events and all‐cause and CV mortality in hypertension.
HBPM also has a role in monitoring BP control in treated subjects during extended periods of time between office visits, especially in patients with good BP control on ABPM which would thus not need to be repeated too often. There is also the added advantage that it can improve long‐term adherence to medication and thereby hypertension control rates.
Because of all these features, HBPM should have a primary role in diagnosis, treatment adjustment, and long‐term follow‐up of most cases with hypertension in LA, although in a number of instances it may still be poorly applicable because of unavailability of HBPM devices and/or because of their unaffordable cost while facing very low resource settings. Improvement of this situation over a relatively short time appears to be an important challenge aimed at better fighting cardiovascular risk in these settings.
CONFLICT OF INTEREST
Authors declare no conflicts of interest in relation to this paper
Villar R, Sanchez RA, Boggia J, et al. Recommendations for home blood pressure monitoring in Latin American countries: A Latin American Society of Hypertension position paper. J Clin Hypertens. 2020;22:544–554. 10.1111/jch.13815
REFERENCES
- 1. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. JACC. 2018;71(19):e127‐e248. [DOI] [PubMed] [Google Scholar]
- 2. Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506‐525. [DOI] [PubMed] [Google Scholar]
- 3. Williams B, Mancia G, Spiering W, Agabiti Rosei E. 2018 ESC/ESH guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953‐2041. [DOI] [PubMed] [Google Scholar]
- 4. Stergiou GS, Parati G, McManus RJ, Head GA, Myers MG, Whelton PK. Guidelines for blood pressure measurement: development over 30 years. J Clin Hypertens. 2018;20:1089‐1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Parati G, Stergiou GS, Asmar R, et al. ESH Working Group on Blood Pressure Monitoring: European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505‐1530. [DOI] [PubMed] [Google Scholar]
- 6. Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359‐1366. [DOI] [PubMed] [Google Scholar]
- 7. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731‐1768. [DOI] [PubMed] [Google Scholar]
- 8. Sebba Barroso WK, Magalhães Feitosa AD, Costa Duarte Barbosa E, et al. Prevalence of masked and white‐coat hypertension in pre‐hypertensive and stage 1 hypertensive patients with the use of TeleMRPA. Arq Bras Cardiol. 2019;113(5):970‐975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. American Heart Association/American Society of Hypertension; Preventive Cardiovascular Nurses Association Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52(1):1‐9. [DOI] [PubMed] [Google Scholar]
- 10. Parati G, Omboni S, Albini F, et al. TeleBPCare Study Group: home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. J Hypertens. 2009;27(1):198‐203. [DOI] [PubMed] [Google Scholar]
- 11. Sebba Barroso de Souza WK, Brandão Veiga Jardim, et al. Comparison and correlation between self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167‐174. [DOI] [PubMed] [Google Scholar]
- 12. Draws PE, Abdala M, Rahman M. Blood pressure measurement: clinic, home, ambulatory, and beyond. Am J Kidney Dis. 2012;60:449‐462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharman JE, Howes FS, Head GA. Home blood pressure monitoring: Australian Expert Consensus Statement. J Hypertens. 2015;33:1721‐1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kindman LA, Turner JR, Lee J. Blood pressure measurement modalities: a primer for busy practitioners. J Clin Hypertens. 2016;18(4):262‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24(12):779‐785. [DOI] [PubMed] [Google Scholar]
- 16. Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta‐analysis of randomized trials. BMJ. 2004;329(7458):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hypertension in adults: diagnosis and management clinical guideline. 24 August 2011. nice.org.uk/guidance/cg127.
- 18. Feitosa ADM, Mota‐Gomes MA, Miranda RD, et al. ACC/AHA hypertension guidelines on the prevalence of white‐coat and masked hypertension: a home blood pressure monitoring study. J Clin Hypertens. 2018;20(12):1745‐1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy primary results of HONEST, a large‐scale prospective, real world observational study. Hypertension. 2014;64:989‐996. [DOI] [PubMed] [Google Scholar]
- 20. Saito I, Kario K, Kushiro T, et al. Rationale, study design, baseline characteristics and blood pressure at16 weeks in the HONEST study. Hypertens Res. 2013;36:177‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Benetos A, Gautier S, Labat C, et al. Mortality and cardiovascular events are best predicted by low central/peripheral pulse pressure amplification but not by high blood pressure levels in elderly nursing home subjects: the PARTAGE (Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Population) study. J Am Coll Cardiol. 2012;60:1503‐1511. [DOI] [PubMed] [Google Scholar]
- 22. Asayama K, Thijs L, Brguljan‐Hitij J, et al. Risk stratification by self‐measured home blood pressure across categories of conventional blood pressure: a participant‐level meta‐analysis. PLoS Medicine. 2014;11(1):e1001591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Asayama K, Ohkubo T, Kikuya M, et al. Prediction of stroke by self‐measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the Joint National Committee 7 classification : the Ohasama study. Stroke. 2004;35:2356‐2361. [DOI] [PubMed] [Google Scholar]
- 24. National Heart Foundation of Australia . Guidelines for the Diagnosis and Management of Hypertension in Adults – 2016. Melbourne National Heart Foundation of Australia; 2016. https://www.mja.com.au/system/files/issues/10.5694mja16.00526.pdf. Accessed January 28, 2020 [Google Scholar]
- 25. Thijs L, Staessen JA, Celis H, et al. The international database of self‐recorded blood pressures in normotensive and untreated hypertensive subjects. Blood Press Monit. 1999;4(2):77‐86. [PubMed] [Google Scholar]
- 26. Caulfield M. Home blood pressure monitoring: new evidence for an expanded role. PLoS Medicine. 2014;11(1):e1001592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population. Follow‐up results from the Pressioni Arteriose Monitorate e Loro Associazione (PAMELA) Study. Circulation. 2005;111:1777‐1783. [DOI] [PubMed] [Google Scholar]
- 28. Stergiou GS, Kollias A, Zeniodi M, Karpettas N, Ntineri A. HBPM: primary role in hypertension management. Curr Hypertens Rep. 2014;16(8):462. [DOI] [PubMed] [Google Scholar]
- 29. Peixoto A. Practical aspects of home and ambulatory blood pressure monitoring. Methodist Debakey Cardiovasc J. 2015;11(4):214‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stergiou GS, Alpert B, Mieke S, et al. A universal standard for the validation of blood pressuremeasuring devices: association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO). Collaboration Statement J Hypertens. 2018;36:472‐478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nobre F, Mion D Jr, Gomes MAM, et al. 6a Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4a Diretrizes de Monitorização Residencial da Pressão Arterial. 2018;110(5, Suppl. 1):1‐29. [Google Scholar]
- 32. Task Force of the Latin American Society of Hypertension: guidelines on the management of arterial hypertension and related comorbidities in Latin America. J Hypertens. 2017;35:1529‐1545. [DOI] [PubMed] [Google Scholar]
- 33. Feitosa ADM, Mota‐Gomes MA, Barroso WS, et al. Blood pressure cutoffs for white‐coat and masked effects in a large population undergoing home blood pressure monitoring. Hypertens Res. 2019;42:1816‐1823. [DOI] [PubMed] [Google Scholar]
- 34. Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta‐analysis of randomized controlled studies. J Hypertens. 2013;31:455‐467. [DOI] [PubMed] [Google Scholar]
- 35. Tucker KL, Sheppard JP, Stevens R, et al. Self monitoring of blood pressure in hypertension: a systematic review and individual patient data meta‐analysis. PLoS Medicine. 14(9):e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Feitosa ADM, Mota‐Gomes MA, Barroso WS, et al. Correlation between office and home blood pressure in clinical practice: a comparison With 2017 ACC/AHA hypertension guidelines recommendations. J Hypertens. 2020;38(1):179‐181. [DOI] [PubMed] [Google Scholar]
- 37. Albini F, Liu X, Torlasco C, et al. ICT and mobilehealth integratedapproach to optimize patients' education on hypertension and its management byphysicians: the Patients Optimal Strategy of Treatment (POST) pilot study. Conf Proc IEEE Eng Med Biol Soc. 2016;2016:517‐520. [DOI] [PubMed] [Google Scholar]
- 38. Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone applications for hypertension management: a potential game‐changer that needs more control. Curr Hypertens Rep. 2017;19(6):48. [DOI] [PubMed] [Google Scholar]
- 39. Shimbo D, Pickering TG, Spruill TM, et al. Relative utility of home, ambulatory, and office blood pressures in the prediction of end‐organ damage. Am J Hypertens. 2007;20:476‐482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19(10):801‐807. Niiranen TJ, Jula AM, Kantola IM, et al. Home‐measured blood pressure is more strongly associated with electrocardiographic left ventricular hypertrophy than is clinic blood pressure: the Finn‐HOME study. J Hum Hypertens. 2007;21(10):788‐794. [DOI] [PubMed] [Google Scholar]
- 41. Niiranen TJ, Asayama K, Thijs L, et al. International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators: outcome‐driven thresholds for home blood pressure measurement: International Database for HOme blood pressure in relation to Cardiovascular Outcome. Hypertension. 2013;61(1):27‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Da Silva GV, de Barros S, Abensur H, Ortega KC, Mion D Jr. Home blood pressure monitoring in blood pressure control among hemodialysis patients: an open randomized clinical trial. Nephrol Dial Transplant. 2009;24(12):3805‐3811. [DOI] [PubMed] [Google Scholar]
- 43. Breaux‐Shropshire TL, Judd E, Vucovich LA, Shropshire TS, Singh S. Does home blood pressure monitoring improve patients' outcomes? A systematic review comparing home and ambulatory blood pressure monitoring on blood pressure control and patient outcomes. Integrated Blood Pressure Control. 2015;8:43‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Parati G, Ochoa J. Home (self) monitoring of blood pressure. In: White WB, ed. Blood Pressure Monitoring in Cardiovascular Medicine and Therapeutics, 3rd ed. Chapter 2. Humana Press; 2016:15‐43. [Google Scholar]
- 45. Thijs L, Staessen JA, Celis H,, et al. Reference values for self‐recorded blood pressure. A meta‐analysis of summary data. Arch Intern Med. 1998;158:481‐488. [DOI] [PubMed] [Google Scholar]
- 46. Sebba Barroso de Souza WK, Brandão Veiga Jardim, et al. Comparison and correlation between self‐measured blood pressure, casual blood pressure measurement and ambulatory blood pressure monitoring. Arq Bras Cardiol. 2011;97(2):148‐155. [DOI] [PubMed] [Google Scholar]
- 47. Lurbe E, Agabiti‐Rosei E, Cruickshank JK, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2009;27(9):1719‐1742. [DOI] [PubMed] [Google Scholar]
- 48. Corrado C. Meeting Abstract. Blood pressure measurement in children. Ital J Pediatr. 2015;41(S2):A19. [Google Scholar]
- 49. Jardim TV, de Souza CC, Morais P, et al. Home blood pressure normalcy in non‐European adolescents. J Hypertens. 2018;36(1):61‐68. [DOI] [PubMed] [Google Scholar]
- 50. Karatzi K, Protogerou A, Rarra V, Stergiou GS. Home and office blood pressure in children and adolescents: the role of obesity. The Arsakeion School Study. J Hum Hypertens. 2009;23:512‐520. [DOI] [PubMed] [Google Scholar]
- 51. Rolim Póvoa TI, Jardim TV, de Souza CC, et al. Home blood pressure monitoring as an alternative to confirm diagnoses of hypertension in adolescents with elevated office blood pressure from a Brazilian State Capital. Arq Bras Cardiol. 2017;109(3):241‐247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jardim TV, de Souza CC, Morais P, et al. White coat, masked and sustained hypertension detected by home blood pressure monitoring in adolescents: prevalence and associated factors. Blood Press. 2018;27(3):151‐157. [DOI] [PubMed] [Google Scholar]
- 53. Gulati V, White W. Ambulatory blood pressure monitoring in older persons. In: White WB, ed. Blood Pressure Monitoring in Cardiovascular Medicine and Therapeutics, 3rd ed. Chapter 11. Humana Press; 2016:209‐225. [Google Scholar]
- 54. Parati G, Lombardi C, Hedner J, et al. Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (COoperation in Scientific and Technological research) ACTION B26 on Obstructive Sleep Apnea. J Hypertens. 2012;30(4):633‐646. [DOI] [PubMed] [Google Scholar]
- 55. Palatini P. Blood pressure measurement in the obese: still a challenging problem. e‐J Cardiol Pract. 2018;16:21. [Google Scholar]
- 56. Kenny IE, Saeed S, Gerdts E, Midtbø H, Halland H, Lønnebakken MT. Masked hypertension in obesity: potential predictors and arterial damage. Blood Pressure Monit. 2017;22:12‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pierin AMG, Alavarce DC, Gusmão JL, Halpern A, Mion D Jr. Blood pressure measurement in obese patients: comparison between upper arm and forearm measurements. Blood Pressure Monit. 2004;9(3):101‐105. [DOI] [PubMed] [Google Scholar]
- 58. Palatini P, Parati G. Blood pressure measurement in very obese patients: a challenging problem. J Hypertens. 2011;29(3):425‐429. [DOI] [PubMed] [Google Scholar]
- 59. O'Brien E. What to do when faced with an unmeasurable ambulatory blood pressure? J Hypertens. 2011;29(3):451‐453. [DOI] [PubMed] [Google Scholar]
- 60. Stergiou GS, Kyriakoulis KG, Stambolliu E, et al. Blood pressure measurement in atrial fibrillation. J Hypertens. 2019;37(12):2430‐2441. [DOI] [PubMed] [Google Scholar]
- 61. Stergiou GS, Karpettas N, Protogerou A, Nasothimiou EG, Kyriakidis M. Diagnostic accuracy of home blood pressure monitor to detect atrial fibrillation. J Hum Hypertens. 2009;23(10):654-658. [DOI] [PubMed] [Google Scholar]
- 62. Verberk WJ, Omboni S, Kollias A, Stergiou GS. Review: screening for atrial fibrillation with automated blood pressure measurement: research evidence and practice recommendations. Int J Cardiol. 2016;203:465‐473. [DOI] [PubMed] [Google Scholar]
- 63. Hodgkinson JA, Tucker KL, Crawford C, et al. Is self monitoring of blood pressure in pregnancy safe and effective? BMJ. 2014;349:g6616. [DOI] [PubMed] [Google Scholar]
- 64. Taylor RS, Freeman L, North RA. Evaluation of ambulatory and self‐initiated blood pressure monitors by pregnant and postpartum women. Hypertens Pregnancy. 2001;20:25‐33. [DOI] [PubMed] [Google Scholar]
- 65. Magee LA, von Dadelszen P, Chan S, et al. Women's views of their experiences in the CHIPS (Control of Hypertension in Pregnancy Study) pilot trial. Hypertens Pregnancy. 2007;26:371‐387. [DOI] [PubMed] [Google Scholar]
- 66. Golara M, Benedict A, Jones C, Randhawa M, Poston L, Shennan AH. Inflationary oscillometry provides accurate measurement of blood pressure in pre‐eclampsia. Br J Obstet Gynaecol. 2002;109(10):1143‐1147. [DOI] [PubMed] [Google Scholar]
- 67. Jacob G, MacDonald T. Home blood pressure monitoring. Eur Cardiol Rev. 2015;10(2):95‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure measurement in patients with chronic kidney disease. Kidney Int. 2006;69(2):406‐411. [DOI] [PubMed] [Google Scholar]
- 69. Asch W, Santos SFF, Peixoto AJ. ABPM in Patients with Chronic Kidney Disease in Cardiovascular Medicine and Therapeutics, 3rd ed. Chapter 14. Humana Press; 2016:277‐298. William B. White. [Google Scholar]
- 70. Agena F, Prado EOS, Souza PS, et al. HBPM in kidney transplant recipients is more adequate to monitor BP than office BP. Nephrol Dial Transplant. 2011;26(11):3745‐3749. [DOI] [PubMed] [Google Scholar]
- 71. Kamoi K, Miyakoshi M, Soda S, Kaneko S, Nakagawa O. Usefulness of home blood pressure measurement in the morning in type 2 diabetic patients. Diabetes Care. 2002;25:2218‐2223. [DOI] [PubMed] [Google Scholar]
- 72. Eguchi K, Hoshide S, Komori T, Nagasaka S, Kario K. A new proposal for the Tatget value for home BP in type 2 diabetes patients: the J‐HOP study. Am J Hypertens. 2015;28(8):971‐979. [DOI] [PubMed] [Google Scholar]
- 73. López‐Jaramillo P, Sánchez RA, Díaz M, et al. Latin‐American consensus of hypertension in patients with type 2 diabetes and metabolic syndrome. J Hypertens. 2013;31:223‐238. [DOI] [PubMed] [Google Scholar]
- 74. Robles N. Home blood pressure monitoring, reproducibility and prognostic aspects‐third in series. e‐J ESC Council Cardiol Pract. 2015;13(14). [Google Scholar]
- 75. Review . A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol. 2015;31:620‐630. [DOI] [PubMed] [Google Scholar]
- 76. Gerin W, Tobin JN, Schwartz JE, et al. The medication Adherence and Blood Pressure Control (ABC) trial: a multi‐site randomized controlled trial in a hypertensive, multi‐cultural, economically disadvantaged population. Contemp Clin Trials. 2007;28:459‐471. [DOI] [PubMed] [Google Scholar]
- 77. Stessen JA, Den Hond E, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955‐964. [DOI] [PubMed] [Google Scholar]
- 78. McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in hypertension: randomized controlled trial and cost effectiveness analysis. BMJ. 2005;331(7515):493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ewald S, vordem Esche J, et al. Relationship the frequency of blood pressure self‐measurement and blood pressure reduction with antihypertensive therapy: results of the OLMETEL (OLMEsartanTELemonitoring blood pressure) study. Clin Drug Investig. 2006;26:439‐446. [DOI] [PubMed] [Google Scholar]


