Abstract
The purposes of this study were to describe the hypertensive population and therapeutic management of hypertension in adults between 18 and 74 years of age in France in 2015. Esteban survey is a cross‐sectional survey with a clinical examination conducted in a representative sample of French adults aged 18‐74 years between 2014 and 2016. Esteban was entirely public‐funded. Blood pressure (BP) was measured during clinical examination with a standardized protocol, and pharmacological treatment was collected through the exhaustive Système National des Données de Santé (SNDS) database. Hypertension was defined by systolic BP (SBP)> 140 mm Hg, diastolic BP (DBP)> 90 mm Hg or treatment with BP‐lowering drugs. The therapeutic control of treated hypertensive patients was defined by SBP < 140 mm Hg and DBP < 90 mm Hg. Adherence to drug treatment was defined as more than 80% of days covered by BP‐lowering drug per year. The prevalence of hypertension was 31.3%. 74.7% of aware hypertensive participants taking an antihypertensive drug, and 57.7% of them were treated with a single antihypertensive pharmacological class. Overall, among hypertensives, 24.3% had a satisfactory BP control. Only 49.7% of treated hypertensives participants were controlled, and 33.6% of them were adherent to their drug treatment. The prevalence of hypertension in France remains high, with only 74.7% of the aware hypertensive participants receiving pharmacological therapy and only 48.9% of aware hypertensives with a BP at goal. More effective measures are needed to improve clinical management of hypertension in France.
Keywords: adherence, awareness, control, hypertension, therapy
1. INTRODUCTION
Hypertension is the main prevalent chronic disease, affecting more than 30% of adults aged >25 years worldwide.1 Because of projected changes in the age distribution of the population, this proportion could increase in the future.2 Moreover, according to a worldwide survey, approximately 54% of stroke and 47% of ischemic heart disease are estimated to be attributed to high blood pressure (BP).3
Studies with BP measurements are necessary to determine the prevalence and control of hypertension. In France, few previous studies involving BP measurements have been conducted over the past few years.4, 5, 6 The latest previous article on the description of hypertension in France was published in 2010.5 The Esteban survey is the main survey using BP readings taken in a representative national sample of French adults aged 18‐74 years.
The purposes of the study were to describe the hypertensive population and the management of the disease (pharmacological treatment, therapeutic control, awareness of hypertension and adherence to drug treatment), and to examine factors associated with drug treatment and control of hypertension in a representative sample of French adults.
1.1. Study design
The Esteban survey is cross‐sectional, in a representative population of French adults (Figure S1). The protocol of the Esteban survey has been previously published.7 The study was registered in the French National Agency for Medicines and Health Products Safety (No. 2012‐A00456‐34) and was approved by the Advisory Committee for Protection of Persons in Biomedical Research.
One of the objectives of the Esteban survey is to describe food consumption, physical activity and to estimate the prevalence of certain chronic diseases and vascular risk factors. The design of the Esteban survey was multistage stratified random sample at three degrees. The first stage of sampling involved random selection of 190 geographic zones (municipalities or groups of municipalities). This was stratified on eight large regions and on the degree of urbanization (four groups, from “rural” to “towns of more than 100 000 inhabitants” and in addition Paris). The number of individuals included in each stratum was defined proportionally to the population size, with a minimum of twenty‐four dwellings to be investigated. At the second level, households were randomly selected by telephone sampling. In each stratified sample, two household samples were randomly drawn independently. The concerned households composed of at least one adult aged 18‐74 years. Households were sampled by random generation of telephone numbers. The main sample consisted of households reachable by landline telephones (numbers 01‐05). To enable the recruitment of households without a geographic wireline telephone line, a complementary sample has been created. This “exclusive mobile” sample consisted of households that could be contacted exclusively by mobile phone with a number starting with 06 or 07 (these households could possibly have a telephone line with a number in 09). At the third level, a single individual (an adult or a child, depending on the sample of households concerned) was selected by lot from among the eligible household members according to Kish's method.8
1.2. Study population
A total of 3021 adults were included between April 2014 and March 2016. Valid BP measurement and hypertensive treatment were available for 2105 participants who were included in analyses (Figure 1).
Figure 1.
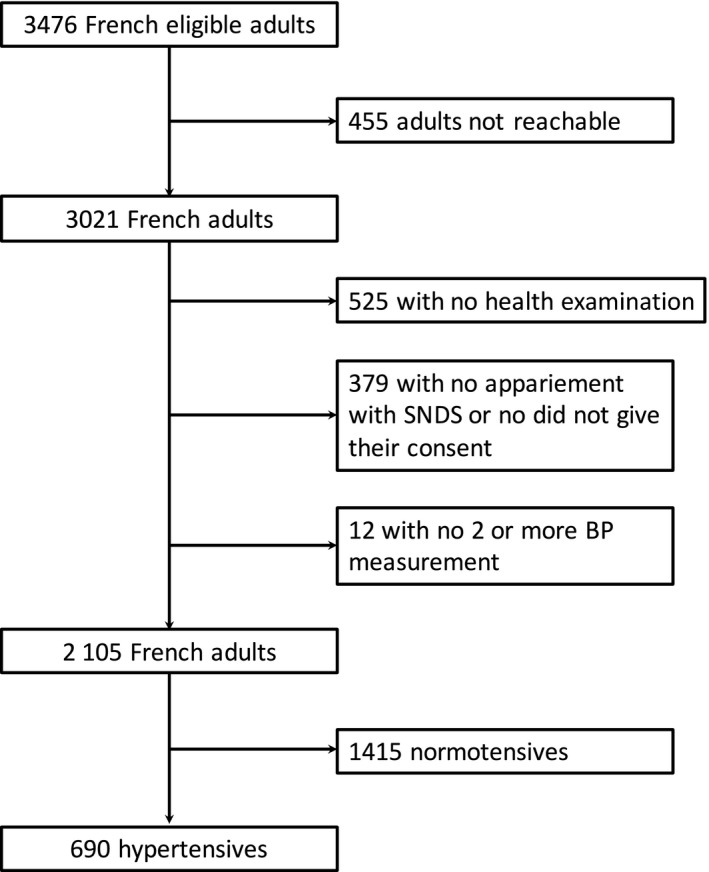
Flowchart
1.3. Data collected
Data were collected (a) by face‐to‐face questionnaires (socioeconomic variables, smoking, dietary intake, physical activity, familial history of cardiovascular diseases, personal history of cardiovascular diseases (stroke, heart failure, peripheral artery disease, myocardial infarction or angina pectoris, or revascularization procedure); (b) during clinical health examination (height, weight, BP, fasting glucose, cholesterol measurement). BP was measured sitting, at home or in health examination center by a medical staff, with an Omron 705‐IT BP monitor on the right arm using a cuff adapted to the circumference of the arm, and using a standardized protocol.9 Measurements were taken at 30 minutes from the blood test and after 5 minutes of rest, without change in position. Three measurements were made, 1 minute apart. The systolic BP (SBP) and diastolic BP (DBP) for each person are the average of the last two measurements. People who did not have at least two BP measurements were excluded from the analysis.
Data of the participants (health examination and questionnaires) were linked to the Système National des données de santé database (SNDS; or National Health Insurance Information System) by a deterministic process. This database provides exhaustive reimbursements for health care expenditure such as drugs, outpatient medical care prescribed or done by health care professionals, number and primary health care utilization of GP or specialist consultations.10
Primary health care utilization and number of consultations were collected from the SNDS in the year preceding the clinical examination and the date of examination itself for GP and cardiologist. Primary health care utilization was defined as at least one visit with a practitioner. These data were compiled in the SNDS by being reimbursed by the French health insurance. Taking into account the French care system, the exhaustiveness of the dates of consultations was compiled in the SNDS.
The names of the drug treatments and the delivery date in the year preceding the health examination were collected. Drugs were collected according to the Anatomical Therapeutic Chemical (ATC) classification of the World Health Organization (C02, C03, C07, C08, and C09 classes for antihypertensive drugs). The search for an indication of the drug treatments was carried out on a case‐by‐case basis by a medical doctor. Each drug treatment compatible with the hypertension was verified when the participants did not declare themselves hypertensive regarding their cardiovascular‐associated diseases.
1.4. Definitions
Hypertension was defined as SBP ≥ 140 mm Hg and/or mean DBP ≥ 90 mm Hg and/or antihypertensive treatment delivery in the 6 months preceding clinical examination.11, 12
Adults were considered aware of their hypertension if they responded positively to the question “have you ever been told by a doctor that you had high BP” or if adults self‐reported hypertension in the questionnaire.
Hypertensive patients were considered treated if they had at least one delivery of hypertensive drug in the 6 months preceding the study. Treated hypertensive adults were considered as being controlled when SBP was <140 mm Hg and DBP < 90 mm Hg.
Proxy for drug adherence was defined as a proportion of day covered by an antihypertensive drug >80% in the year preceding clinical examination, based on the number of drug boxes purchased during the year and reported by the SNDS database.13
Awareness of hypertension was based on self‐report: Two questions in the Esteban survey were used to determine the awareness of hypertension: as “a doctor ever told you that your blood pressure is too high?” and as “have you ever had hypertension?”.
Control of hypertension was defined as SBP < 140 mm Hg and DBP < 90 mm Hg.
1.5. Statistical analysis
For the participants who underwent a health examination, probabilities of inclusion were calculated to consider the complex survey design. The complex, stratified, and multistage sampling design was considered in the calculation of the initial weighting applied to everyone who participated in the first visit. This weighting corresponded to the number of eligible persons in the household, multiplied by the reciprocal of the probability of drawing the household and by the inverse of the probability of draw of the primary units. The method used to calculate household draw probabilities distinguished, on the one hand, households recruited by landline telephone, and on the other hand, households in the “exclusive mobile” sample, the number of telephone lines that had been estimated by primary units for landlines and nationally for mobiles.
To account for individuals who dropped the study between first visit and the health examination, a first adjustment was made using the scores method to correct nonresponse. A set of weightings was thus calculated and applied to the individuals having participated in the health examination. Finally, the adjustment was completed by the application of the margin calibration method for the health examination weighting. The margins used in the calibration were taken from the last population census (in 2012) and concerned the following data: age, sex, diploma, marital status, household, and seasons. Calibration was carried out using the SAS macro program CALMAR (CALibration on MARgins), and census data came from the National Institute for Statistics and Economic Studies (Insee). Because of the small number of hypertensive participants under 45, all age groups between 18 and 54 were grouped together. Statistical analyses were performed with SAS version 9.4 (SAS Institute). For all analyses, P‐values were two‐tailed and differences considered significant at P < .05. Kruskal‐Wallis test was used to study quantitative variables, while Pearson's chi‐squared test and logistic regression analysis were used for qualitative variables.
2. RESULTS
The prevalence of hypertension was 31.3%. Among adults with hypertension, 56.3% were aware, 48.9% were treated (74.7% among aware hypertensives), and 24.3% were controlled (49.7% among treated hypertensives) (Figure 2, Table S1).
Figure 2.
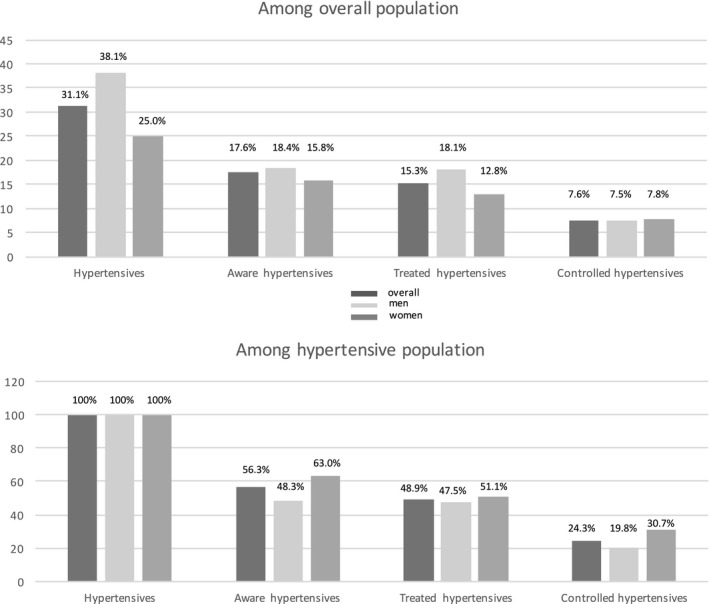
Descriptive situation of hypertension in France according to sex
2.1. Prevalence of hypertension
The prevalence of hypertension was 31.3% (Table 1) and was significantly higher among men than among women (38.6% vs 25.8%, P < .0001), and this difference remained significant after adjustment for age and BMI (P < .0001). The prevalence increased with age, reaching 68.8% of the population age 65‐74 (P < .0001). 56.3% of the hypertensive participants reported being aware of their hypertension. Women were more often aware of their condition than men (P = .009). The rate of awareness increased with age for both sexes (for men, P = .001 and for women, P = .002; Table S2).
Table 1.
Hypertension: prevalence, awareness, treatment, control and adherence in men and women
|
All (n = 2015) (%) |
Men (n = 945) (%) |
Women (n = 1160) (%) |
|
|---|---|---|---|
| Prevalence | |||
| 18‐54 | 15.5 | 21.9 | 9.7 |
| 55‐64 | 53.6 | 59.8 | 47.8 |
| 65‐74 | 68.8 | 75.0 | 62.4 |
| All | 31.3 | 38.1 | 25.0 |
| Awarness a | |||
| 18‐54 | 40.7 | 37.3 | 47.6 |
| 55‐64 | 64.6 | 60.9 | 68.8 |
| 65‐74 | 62.5 | 58.6 | 67.3 |
| All | 56.3 | 48.3 | 63.0 |
| Treatment b | |||
| 18‐54 | 61.2 | 60.1 | 63.1 |
| 55‐64 | 76.6 | 76.9 | 74.3 |
| 65‐74 | 82.5 | 87.0 | 77.6 |
| All | 74.7 | 75.8 | 73.3 |
| Control a | |||
| 18‐54 | 15.4 | 12.4 | 21.5 |
| 55‐64 | 30.2 | 26.1 | 35.0 |
| 65‐74 | 26.4 | 21.7 | 32.3 |
| All | 24.3 | 19.8 | 30.7 |
| Adherence c | |||
| 18‐54 | 43.3 | 43.1 | 43.5 |
| 55‐64 | 36.4 | 37.4 | 35.3 |
| 65‐74 | 25.7 | 28.7 | 21.1 |
| All | 33.6 | 34.9 | 31.8 |
Values are weighted percentage.
Among hypertensive participants.
Among aware hypertensive participants.
Among treated hypertensive participants.
2.2. Treatment of hypertension
Among all hypertensive adults, less than one in two were treated. When the hypertensive adults were restricted to those who were aware of their hypertension, the proportion of hypertensive adults treated rose to 74.7%. (Table 1). There is no difference between sexes for therapy (P = .293). Treated hypertensive adults had more often other vascular risk factors (diabetes treated, hypercholesterolemia treated and obesity and previous CV events) (Table 2). Tobacco was the only risk factors which was more frequent in non‐treated hypertensives compared to treated hypertensives (P < .0001). Treated hypertensive participants have more often primary health care utilization to a general practitioner (P < .0001) and a cardiologist (P = .032) compared to non‐treated hypertensives. In addition, the number of consultations (GP and cardiologist) was higher in treated hypertensives than in non‐treated (P < .0001) (Table 2). Finally, treated hypertensives declare that they had more often a self‐monitoring (P = .0005). Information by sex was shown in Table S3.
Table 2.
Comparison of treated and untreated aware hypertensive participants
| All hypertensives (n = 690) | Aware treated hypertensives (n = 300) | Aware non‐treated hypertensives (n = 96) | P value* | |
|---|---|---|---|---|
| SBP (mm Hg) | 145.6 (17.1) | 141.9 (19.6) | 151.8 (13.4) | <.0001 |
| DBP (mm Hg) | 85.8 (10.4) | 82.9 (10.7) | 90.9 (7.3) | <.0001 |
| Mean age (y) | 57.8 (11.0) | 61.2 (8.4) | 55.7 (10.3) | <.0001 |
| Current smokers | 17.9% | 8.9% | 23.4% | <.0001 |
| Obesity | 30.1% | 40.8 % | 21.9% | .0007 |
| Treated diabetes | 12.4% | 19.0% | 5.4% | .0001 |
| Treated hypercholesterolemia | 51.9% | 62.8% | 38.3% | <.0001 |
| Previous CV events | 9.1% | 12.5% | 4.1% | .017 |
| GP recourse | 92.9% | 97.8% | 82.4% | <.0001 |
| Cardiologist recourse | 11.4% | 16.2% | 7.6% | .032 |
| Number of GP consultations/y | 10.2 (9.3) | 13.5 (9.5) | 7.6 (8.0) | <.0001 |
| Number of Cardiologist consultations/y | 0.16 (0.52) | 0.21 (0.6) | 0.09 (0.3) | <.0001 |
| Self‐monitoring | 42.1% | 59.2% | 39.3% | .0005 |
Values are weighted percentage.
Abbreviations: CV, cardiovascular; DBP, diastolic blood pressure; GP, general practitioner; HBPM, home blood pressure monitoring; SBP, systolic blood pressure.
P value for comparison between aware treated hypertensives and aware non‐treated hypertensives.
2.3. Pharmacological treatment of hypertension
62.1% of treated hypertensives received a single antihypertensive class and 37.9% two or more. There is no significant difference between men and women in treatment by polytherapy (40.4% vs 34.6%, P = .197). Number of drugs per age and sex are shown in Table S4.
Among treated hypertensives, angiotensin II receptor blockers (ARB) were prescribed in 38.4%, diuretics in 32.9%, angiotensin converting enzyme inhibitors (ACEI) in 25.2%, beta‐blockers (BB) in 25.2%, calcium‐channel blockers (CCB) in 19.3%, and others antihypertensive drugs in 2.2%. Figure 3 represents the different drugs prescribed according to sex.
Figure 3.
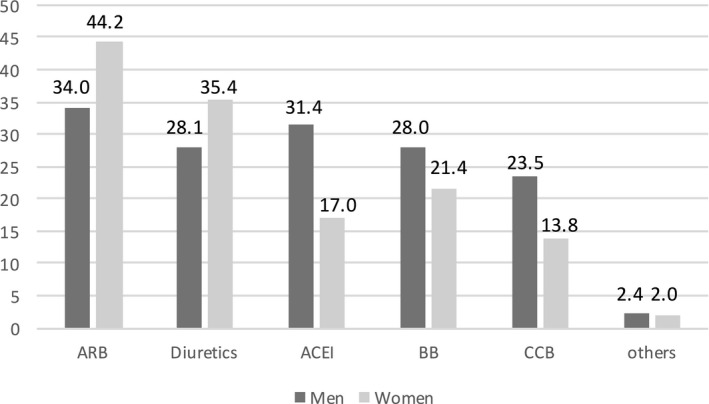
The different classes of drugs prescribed according to sex (in percentage)
The difference by age was significant in both sexes, in men: 36.5% of 18‐ to 54‐year‐olds treated received polytherapy vs 46.3% of 65‐ to 74‐year‐olds (P = .0008) and in women: 27.8% of 18‐ to 54‐year‐olds treated received polytherapy vs 37.1% of 65‐ to 74‐year‐olds (P = .0001).
Among treated hypertensives with monotherapy, ARBs were prescribed in 30.5%, BB in 26.2%, ACEI in 19.3%, diuretics in 11.4%, CCB in 11.1%, and others in 1.5% (Figure 4).
Figure 4.
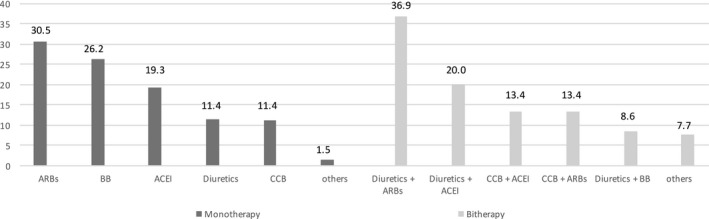
Pharmacological treatment of hypertensives among monotherapies and bi‐therapies (in percentage)
In bi‐therapies, the main combinations were “diuretic + ARB” with 36.9%, “diuretic + ACEI” with 20.0%, “CCB + ARB” with 13.4%, “CCB + ACEI” with 13.4%, and “diuretic + BB” with 8.6%, other with 7.7% (Figure 4).
2.4. Therapeutic control of treated hypertension
Among treated hypertensive adults, 49.7% were not controlled. Uncontrol of treated hypertensives was significantly more frequent in men than in women (respectively, 58.2% vs 39.8%, P = .001; Figure 5). Polytherapy was not more frequent in uncontrolled hypertensives (P = .723; Table 3). No significant difference was observed for hypertension control regarding the number of drugs (bitherapy vs monotherapy OR = 0.91 [0.70‐1.12], P = .698; tritherapy vs bitherapy OR = 1.22 [0.54‐1.90], P = .851; and tritherapy vs monotherapy OR = 1.11 [0.41‐1.81], P = .957). Uncontrolled treated hypertensives have a lower number of GP consultations than controlled treated hypertensives (12.3 vs 14.2, P = .012), but no difference in the number of cardiologist consultations was observed (0.29 vs 0.25, P = .622; Table 3). There is no significant difference in controlled and uncontrolled hypertensive for the possession of self‐monitoring (P = .393). Information by sex was shown in Table S3.
Figure 5.
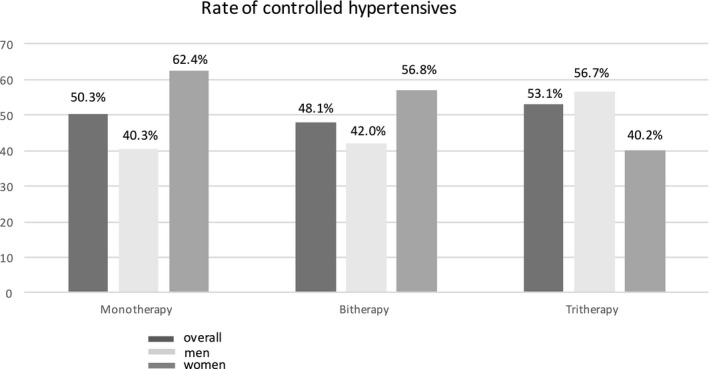
Rate of controlled hypertensives by number of drugs
Table 3.
Comparison of control vs uncontrol and adherent vs non‐adherent in treated hypertensive participants
| Control hypertensives (n = 182) | Uncontrol hypertensives (n = 168) | P value | Adherent (n = 123) | Non‐adherent (n = 230) | P value | |
|---|---|---|---|---|---|---|
| Monotherapy antihypertensivea | 50.3% | 49.7% | 35.3% | 64.7% | ||
| Bitherapy antihypertensivea | 48.1% | 51.9% | .288 | 28.6% | 71.4% | .297 |
| Tritherapy antihypertensivea | 53.1% | 46.9% | 51.5% | 48.5% | ||
| GP care utilization | 99.5% | 96.7% | .074 | 97.6% | 98.3% | .923 |
| Cardiologist care utilization | 15.6% | 22.0% | .404 | 9.67% | 23.5% | .013 |
| Number of GP consultations/y | 14.2 (10.9) | 12.3 (7.81) | .012 | 11.2 (7.46) | 14.3 (10.2) | .034 |
| Number of cardiologist consultations/y | 0.25 (0.69) | 0.29 (0.62) | .622 | 0.11 (0.39) | 0.35 (0.75) | .017 |
| Self‐monitoring | 53.9% | 58.5% | .393 | 59.3% | 54.6% | .732 |
Abbreviations: GP, general practitioner; HBPM, home blood pressure monitoring.
Per rows, P value for comparison between control and uncontrol and between adherent and non‐adherent.
2.5. Adherence of treatment
Only 33.6% of treated hypertensive adults were adherent with their therapeutic drugs and with a proportion of days per year covered of 64.1%. There is no significant difference for the adherence of treatment between men and women (P = .537). However, the adherence of treatment decreases with age (P = .054) (Table 2). There is no significant association between adherence and the number of class (P = .254; bitherapy vs monotherapy OR = 0.73 [0.44‐1.02], P = .106; tritherapy vs bitherapy OR = 2.65 [0.28‐5.02], P = .846; and tritherapy vs monotherapy OR = 1.94 [0.37‐3.51], P = .520). Non‐adherent‐treated hypertensives have more often primary health care utilization to high number of cardiologist and GP consultations (respectively, P = .017 and P = .034; Tables 3 and S3).
3. DISCUSSION
The Esteban survey is the main recent survey measuring BP carried out on a national and representative sample of French adults (aged 18‐74 years). Salient findings of this survey are the following: The hypertension prevalence was 31.3% in the 18‐ to 74‐year‐old population; 48.9% of hypertensive adults taking an antihypertensive drug. Among treated hypertensive adults, 24.3% had satisfactory control of their hypertension, 62.1% were treated with a single antihypertensive pharmacological class, and 33.6% were adherent to their treatment.
In France, the prevalence of hypertension and its management appear to be constant from 2006. The prevalence of the hypertension was 31.3% for Esteban compared to 31.0% for ENNS (Etude Nationale Nutrition Santé—national study nutrition health study) in 2006. The ENNS survey was conducted in 2006 with the same survey design than Esteban.5 Nevertheless, the control tends to decrease over the time (respectively, 24.3% vs 25.6%) as drugs treatment rate (respectively, 48.9% vs 50.3%), whereas the awareness of hypertension increases (respectively 56.3% vs 52.2%).5 Moreover, recent controversies, in particular relating to statins, may have an impact on cardiovascular drug therapies and especially on hypertension.14
However, some sex differences can be highlighted between Esteban and ENNS. The prevalence rate of hypertension in men is increased (respectively 38.1% vs 34.1%), while for women, the rate is decreased (respectively, 25.0% vs 27.8%). Similarly, the control rate of hypertension increased in men (respectively, 19.8% vs 17.1%) and decreased in women (respectively, 30.7% vs 36.2%). Drug treatment rate tends to decrease over time, but sex differences should be observed (with an increased rate for men, respectively, 47.5% vs 41.0% and a decrease rate for women, respectively, 51.1% vs 62.0%). Previous studies have shown that women were more likely to use antihypertensive drugs than men, but this behavior seems to be convergent with time.5, 15
3.1. Prevalence of hypertension
Esteban survey is a cross‐sectional study which involves several BP reading on a single occasion. In clinical practice, the diagnosis of hypertension is based on observation of high values on several occasions. Studies on hypertension prevalence using a single run of measurements are useful for geographic and temporal comparisons. But for the more recent years, comparisons are difficult because of a lack of common protocol and disparities in the age groups studied.
In central and eastern Europe, hypertensive adults were in 2015 over 150 million.16, 17 The worldwide prevalence of hypertension in adults is around 30%‐45%,18 with 30.0% in England,19 31.6% in Germany,20 or 42.2% in Portugal.21 Recent studies carried out in North America reported a prevalence at 32% with 140/90 mm Hg,22, 23 but the prevalence increased to 46% with new recommendations (SBP/DBP ≥130/80 mm Hg).24
3.2. Awareness of hypertension
The proportion of awareness in France is higher than the mean observed in the United States and in Europe with 51%,18 but lower than England with 71.0%,19 Portugal with 76.6%,21 and Germany with 82.3%.20 Some sex differences have been observed for the awareness of hypertension. According to previous studies, women present a higher rate of awareness compared to men.25 This could be explained by the fact that women interact more regularly than men with health care system (gynecological health, maternal programs, etc).26
3.3. Drug treatment of hypertension
The proportion of treated hypertensives in our study is lower than the proportion observed in Germany with 71.8% of hypertensives treated,20 and in England with 58.0% of hypertensives treated.19 In France, the proportion of treated hypertensive adults have decreased in women since 2006 but remained stable in men.5 Every person in France is covered by health insurance regardless of their economic status. Lack of hypertension management may be rather a problem of awareness than an insufficient access to health care system.
Among aware hypertensive adults, the proportion of treated adults is similar to those observed in Portugal with 74.5%21 and in the United States with 74.5%,27, 28 but lower than those observed in Canada with 78.1%,29 and Germany with 87.7%.20
European recommendations in 2013, effective at the time of data collection, mentioned that a large proportion of hypertensives require numerous therapeutic classes to control their hypertension.12 In Esteban, 42.3% of aware treated hypertensives received drug treatment including more than one pharmacological class.
3.4. Pharmacological treatment of hypertension
The high proportion of BB in patients treated by monotherapy was in variance with the 2013‐French guidelines which recommended that initiation should be preferable with thiazide diuretics, CCB, ARB, or ACEI; those two latter classes being mainly associated with higher persistence and tolerance compared to BB and diuretics.11, 30 Moreover, the same French guidelines ruled that the combination of “BB + diuretics” increases risk of diabetes,11, 30 while this combination represented 9.0% of bi‐therapies prescribed in the Esteban survey.
3.5. Control of treated hypertension
The control of hypertension in France remains insufficient. However, hypertension was more frequently controlled in France than in other countries of North America and Europe, with a control rate at 18.4% of hypertensive adults and 38.5% of treated hypertensive adults.18 But this situation is less efficient than other countries, such as England with 37.0% of controlled among hypertensive adults (63.0% of controlled among treated hypertensive adults),19 Portugal with 42.5% of controlled among hypertensives (55.7% of controlled among treated hypertensives)21 and Germany with 51.2% of controlled among hypertensives (71.5% of controlled among treated hypertensives).20
Several barriers have been highlighted to hypertension control at the health care system. Poor access to health care, poor insurance coverage, and medication costs were the main barriers to hypertension control.31 Nevertheless, due to the French insurance coverage, these barriers could be not the explanation. Other barriers could be responsible, as physician time and lack of preventing counseling.32 Poor adherence to guidelines and the absence of prioritizing hypertension management among numerous chronic diseases provide some barriers.31 The representation of hypertensions as a non‐prior management disease could impact the adherence of medications and care visit.33
3.6. Adherence of drug treatment
The rate of adherence of antihypertensive drugs was low in our study. There is a growing evidence that poor adherence to drug treatments appears as the main cause of poor BP control.34 Non‐adherence to antihypertensive therapy was associated with higher risk of CV events.35
Barriers to hypertension control are highly correlated with poor adherence, the perception of low‐risk level of high BP, a lack of motivation, and side effects of drugs.31, 36 Antihypertensive drug adherence is complex due to some side effects and a non‐benefit immediately observed.37 A combination of different factors could explain the low rate of hypertension control, and adherence to drug treatment should be one of the main objectives to reach.38 The adherence could be improved by numerous interventions. The main useful interventions are those linking drug intake with habits or using pillboxes and other special packaging and motivational interviewing.39
3.7. Limitations
The main strength of our study is that participants of the ESTEBAN survey are representative of the general French population. The data were collected regarding standardized protocols which add validity to our study's results. Pharmacological treatments were collected by using delivery of drugs in the SNDS database which is exhaustive and avoid memory bias. Medical history and comorbidities have been collected self‐reporting and physician assertion during medical examination in health centers. They are less participant to misinterpretation, under or over‐reporting.
However, some limitations are present in our study. The study population was limited to adults aged 18‐74. The sample size was rather small limiting the statistical power of the analyses. The prevalence of hypertension was overestimated due to the protocol used: 3 measures during a single visit and affected by white coat phenomenon. However, methodology of BP measurement and hypertension prevalence definition were coherent with previous studies carried in France and in other epidemiologic worldwide studies estimating the prevalence of hypertension.
Hypertension was considered as being controlled for values of SBP and DBP strictly <140 and 90 mm Hg, respectively, without adapting it to targets defined for populations at high vascular risk, diabetics, and patients with renal dysfunction. Three measurements were made, nevertheless, in clinical practice hypertension was diagnosed based on several measurements at several visits at the physician's office and ideally using home‐based or ambulatory‐based BP.
The prevalence of white coat hypertension (WCH) ranged from 10% to 29% in untreated patients, around 30% in treated hypertensive patients and ranged from 18% to 40% in population‐based studies.40 Nevertheless, the prevalence of WCH is depending on the use of ambulatory or office BP and the definition of BP cutoff for hypertension.41 Masked hypertension (MH) is the opposed of WCH and ranged around 20%‐30% in untreated patients and population‐based studies.40 Gorostidi et al concluded that patients presenting WCH were mainly women, older, and obese but with low CV risk profile, whereas patients with MH were mostly men, younger, obese, and smokers and presented high CV risk profile.40 Thus, even if the population profiles were different, the proportion of WCH and MH are almost equal, and therefore, the overall prevalence of hypertension would not change even if out of office BP measurement was available.
Adherence of antihypertensive drugs was assessed by the number of drug boxes purchased during the year. Thus, adherence was overestimated, since patients may buy the medication without taking it. However, drugs delivery remains a better proxy of adherence than the simple drug prescription.
4. CONCLUSIONS
According to the Esteban study, the prevalence of hypertension was 31.3% in the 18‐ to 74‐year‐old population in France in 2015. Overall, among hypertensives, 56.3% were aware of their status, less than one in two were treated with antihypertensive drugs, and one in four had satisfactory control of their hypertension. Improve hypertension awareness should be a major way to improve the proportion of drug treatment among hypertensive adults, and, by consequences, adherence and control of hypertension.
IRB APPROVAL
The study was registered in the French National Agency for Medicines and Health Products Safety (No. 2012‐A00456‐34) and was approved by the Advisory Committee for Protection of Persons in Biomedical Research.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Alexandre Vallée made the conception, design, statistical analysis, and interpretation of data. Jacques Blacher and Valérie Olié made substantial contribution to conception and interpretation of data. Alexandre Vallée, Amélie Gabet, Clémence Grave, Emmanuel Sorbets, Jacques Blacher, and Valérie Olié have been involved in drafting the manuscript or revisiting it critically for intellectual content. All the authors have given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supporting information
ACKNOWLEDGEMENTS
The authors thank the Centers for Health Examinations, the Cetaf and the laboratories involved in the collection, and the entire Esteban team and study participants. The Esteban study, from the National Biosafety launches, is financed by the Ministry of Solidarities and Health and the Ministry of Ecological and Solidarity Transition.
Vallée A, Gabet A, Grave C, Sorbets E, Blacher J, Olié V. Patterns of hypertension management in France in 2015: The ESTEBAN survey. J Clin Hypertens. 2020;22:663–672. 10.1111/jch.13834
REFERENCES
- 1. WHO . A global brief on hypertension; 2013. http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf
- 2. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet Lond Engl. 2005;365:217‐223. [DOI] [PubMed] [Google Scholar]
- 3. Lawes CMM, Vander Hoorn S, Rodgers A, International Society of Hypertension . Global burden of blood‐pressure‐related disease, 2001. Lancet Lond Engl 2008;371:1513‐1518. [DOI] [PubMed] [Google Scholar]
- 4. Wagner A, Dallongeville J, Ferrières J, Amouyel P, Haas B. État des lieux sur l’hypertension artérielle en France en 2007 : l’étude Mona Lisa. BEH. 2008; 49‐50.
- 5. Godet‐Mardirossian H, Girerd X, Vernay M, Chamontin B, Castetbon K, de Peretti C. Patterns of hypertension management in France (ENNS 2006–2007). Eur J Prev Cardiol. 2012;19:213‐220. [DOI] [PubMed] [Google Scholar]
- 6. Marques‐Vidal P, Ruidavets JB, Amouyel P, et al. Change in cardiovascular risk factors in France, 1985–1997. Eur J Epidemiol. 2004;19:25‐32. [DOI] [PubMed] [Google Scholar]
- 7. Balicco A, Oleko A, Boschat L, et al. Esteban design: a cross‐sectional health survey about environment, biomonitoring, physical activity and nutrition (2014–2016). Toxicol Analyt Clin. 2017;29:517‐537. [Google Scholar]
- 8. Kish L. A Procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44:380‐387. [Google Scholar]
- 9. Tolonen H. EHES Manual. Part B. Fieldwork procedures. National Institute for health and welfare ; 2013. Directions 2013 002. http://urn.fi/URN:ISBN:978-952-245-843-8
- 10. Tuppin P, Rudant J, Constantinou P, et al. Value of a national administrative database to guide public decisions: from the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017;65(Suppl 4):S149‐S167. [DOI] [PubMed] [Google Scholar]
- 11. Blacher J, Halimi J‐M, Hanon O, et al. Management of hypertension in adults: the 2013 French Society of Hypertension guidelines. Fundam Clin Pharmacol. 2014;28:1‐9. [DOI] [PubMed] [Google Scholar]
- 12. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281‐1357. [DOI] [PubMed] [Google Scholar]
- 13. Baumgartner PC, Haynes RB, Hersberger KE, Arnet I. A systematic review of medication adherence thresholds dependent of clinical outcomes. Front Pharmacol. 2018;9:1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nielsen SF, Nordestgaard BG. Negative statin‐related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37:908‐916. [DOI] [PubMed] [Google Scholar]
- 15. Gu Q, Burt VL, Paulose‐Ram R, Dillon CF. Gender differences in hypertension treatment, drug utilization patterns, and blood pressure control among US adults with hypertension: data from the National Health and Nutrition Examination Survey 1999–2004. Am J Hypertens. 2008;21:789‐798. [DOI] [PubMed] [Google Scholar]
- 16. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population‐based measurement studies with 19·1 million participants. Lancet. 1975;2017(389):37‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. NCD Risk Factor Collaboration (NCD‐RisC) . Long‐term and recent trends in hypertension awareness, treatment, and control in 12 high‐income countries: an analysis of 123 nationally representative surveys. Lancet Lond Engl 2019;394:639‐651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high‐, middle‐, and low‐income countries. JAMA. 2013;310:959‐968. [DOI] [PubMed] [Google Scholar]
- 19. Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross‐sectional study from 1994 to 2011. Lancet Lond Engl. 2014;383:1912‐1919. [DOI] [PubMed] [Google Scholar]
- 20. Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–11. J Hum Hypertens. 2015;29:247‐253. [DOI] [PubMed] [Google Scholar]
- 21. Polonia J, Martins L, Pinto F, Nazare J. Prevalence, awareness, treatment and control of hypertension and salt intake in Portugal: changes over a decade. The PHYSA study. J Hypertens. 2014;32:1211‐1221. [DOI] [PubMed] [Google Scholar]
- 22. Whelton PK. The elusiveness of population‐wide high blood pressure control. Annu Rev Public Health. 2015;36:109‐130. [DOI] [PubMed] [Google Scholar]
- 23. Crim MT, Yoon SSS, Ortiz E, et al. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes. 2012;5:343‐351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive Summary: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertens Dallas Tex. 1979;2018(71):1269‐1324. [DOI] [PubMed] [Google Scholar]
- 25. Courtenay WH. Constructions of masculinity and their influence on men’s well‐being: a theory of gender and health. Soc Sci Med. 1982;2000(50):1385‐1401. [DOI] [PubMed] [Google Scholar]
- 26. Brett KM, Burt CW. Utilization of ambulatory medical care by women: United States, 1997–98. Vital Health Stat. 2001;13:1‐46. [DOI] [PubMed] [Google Scholar]
- 27. Fang J. Prevalence of self‐reported hypertension and antihypertensive medication use among adults aged ≥18 years — United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2018;67:219‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yoon SSS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief. 2015;1‐8. [PubMed] [Google Scholar]
- 29. DeGuire J, Clarke J, Rouleau K, Roy J, Bushnik T. Blood pressure and hypertension. Health Rep. 2019;30:14‐21. [PubMed] [Google Scholar]
- 30. Blacher J, Halimi J‐M, Hanon O, et al. Management of arterial hypertension in adults: 2013 guidelines of the French Society of Arterial Hypertension. Ann Cardiol Angeiol. 2013;62:132‐138. [DOI] [PubMed] [Google Scholar]
- 31. Walsh JME, Sundaram V, McDonald K, Owens DK, Goldstein MK. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens. 2008;10:311‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jaén CR, Stange KC, Nutting PA. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract. 1994;38:166‐171. [PubMed] [Google Scholar]
- 33. Lin ND, Martins SB, Chan AS, et al. Identifying barriers to hypertension guideline adherence using clinician feedback at the point of care. AMIA Annu Symp Proc. 2006;494‐498. [PMC free article] [PubMed] [Google Scholar]
- 34. Krousel‐Wood M, Joyce C, Holt E, et al. Predictors of decline in medication adherence: results from the cohort study of medication adherence among older adults. Hypertens. 1979;2011(58):804‐810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Corrao G, Parodi A, Nicotra F, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29:610‐618. [DOI] [PubMed] [Google Scholar]
- 36. Ogedegbe G. Barriers to optimal hypertension control. J Clin Hypertens. 2008;10:644‐646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785‐794. [DOI] [PubMed] [Google Scholar]
- 38. Mills KT, Rubinstein A, Irazola V, et al. Comprehensive approach for hypertension control in low‐income populations: rationale and study design for the hypertension control program in Argentina. Am J Med Sci. 2014;348:139‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Conn VS, Ruppar TM, Chase J‐AD, Enriquez M, Cooper PS. Interventions to improve medication adherence in hypertensive patients: systematic review and meta‐analysis. Curr Hypertens Rep. 2015;17:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white‐coat and masked hypertension in national and international registries. Hypertens Res. 2015;38:1‐7. [DOI] [PubMed] [Google Scholar]
- 41. Mancia G, Bombelli M, Seravalle G, Grassi G. Diagnosis and management of patients with white‐coat and masked hypertension. Nat Rev Cardiol. 2011;8:686‐693. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


