Abstract
We investigated the prevalence, awareness, treatment, and control of hypertension in a large opportunistic screening study in China. Our study participants had to be ≥18 years of age and had ideally not taken blood pressure (BP) for ≥1 year. BP was measured three times consecutively in the sitting position with a 1‐minute interval, using a validated electronic BP monitor or mercury sphygmomanometer. Trained volunteer investigators administered a questionnaire to collect information on medical history, lifestyle, and use of medications. The 364 000 participants (52.6% women, and mean age 53.4 years) had a mean systolic/diastolic BP of 124.2/76.4 mm Hg. The proportion of hypertension was 24.7%. In all hypertensive subjects (n = 89 925), the awareness, treatment, and control rates of hypertension were 60.1%, 42.5%, and 25.4%, respectively. In multiple stepwise logistic regression analyses, the odds for unawareness vs awareness of hypertension was higher in men and lower with age advancing, current smoking, and the presence of diabetes mellitus, coronary heart disease, and stroke or transient ischemic attack (P < .0001). The odds for uncontrolled vs controlled hypertension was higher with age advancing and current smoking, and lower with the presence of diabetes mellitus and coronary heart disease (P ≤ .03) in 38 207 treated hypertensive patients, and it was also higher with the use of antihypertensive monotherapy (odds ratio 1.13, P = .0003) in 19 523 treated hypertensive patients with specific antihypertensive drugs. Our study identified several factors as barriers to BP control in China, such as male gender, younger age, current smoking, and the under‐use of combination therapy.
Keywords: awareness, blood pressure, China, control, hypertension, treatment
1. INTRODUCTION
According to the most recent China nationwide hypertension survey in 2012‐2015, the crude prevalence of hypertension was 27.9%, and the awareness, treatment and control rates of hypertension were 46.9%, 40.7%, and 15.3%, respectively. 1 If this survey would be compared with the previous one in 2002, 2 the prevalence was substantially increased by an absolute percentage of 9.1% from 18.8%, while the awareness, treatment, and control rate increased by an absolute percentage of 16.7%, 16.0%, and 9.2%, respectively. However, the awareness and control rate remains at low level. Untreated and uncontrolled hypertension remains a major cause of cardiovascular events and mortality in China. 3 , 4 , 5 It is, therefore, extremely important to make all efforts to raise awareness and control of hypertension in China.
As one of the China nationwide initiatives for improving the management of hypertension, we actively participated in the May Measurement Month (MMM) project, 6 , 7 , 8 organized by the International Society of Hypertension in collaboration with the World Hypertension League and the Lancet Commission on Hypertension. 9 The earlier collected data in 2017 in 125 236 participants were included in the pooled analysis of the worldwide project. 6 , 7 However, in the whole measurement period in 2017, a total of 364 000 study participants had their blood pressure measured and had sufficient quality of data. In the present study, we investigated the prevalence, awareness, treatment, and control of hypertension in this opportunistic screening in China.
2. METHODS
2.1. Study design and participants
The MMM China project strictly followed the international MMM 2017 protocol, which had been previously described in detail elsewhere. 6 , 7 The China project was conducted from May to September 2017 in 394 measurement sites across 22 of the 31 China mainland provinces. Measurement sites were mostly inside hospitals or community health centres, but usually located in a public area instead of doctors’ offices for routine clinical service. The Ethics Committee of Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China approved the study protocol. All participants provided written informed consent.
Eligible participants were volunteer adults aged ≥18 years, who had ideally not taken blood pressure for at least 1 year.
2.2. Blood pressure measurement
Blood pressure was measured three times consecutively in the sitting position after at least 5 minutes rest with an 1‐minute interval, using a validated automatic blood pressure monitor (Omron HEM‐9200T Omron Healthcare or A&D TM2656) or a mercury sphygmomanometer. These three blood pressure readings were averaged for analysis. Hypertension was defined as a blood pressure of at least 140 mm Hg systolic or 90 mm Hg diastolic, or the use of antihypertensive medication. In treated hypertensive patients, control of hypertension was defined as a blood pressure below 140 mm Hg systolic and 90 mm Hg diastolic.
2.3. Questionnaire and anthropometric measurements
Trained volunteer investigators administered a questionnaire to collect information on medical history, lifestyle, and use of medications. The trained investigators also measured body height, body weight, and waist and hip circumferences. Body mass index was calculated as the body weight in kilograms divided by the body height in meters squared. Overweight and obesity were defined as a body mass index of 24.0‐27.9 and ≥28.0 kg/m2, respectively.
2.4. Statistical methods
Database management and statistical analyses were performed using the SAS software (SAS 9.2, SAS Institute). Means and proportions were compared using the student t test and chi‐square test, respectively. We performed multiple stepwise logistic regression analyses with a P value for entry and stay in the model set at .10. We considered sex, age, body mass index, current smoking, and alcohol intake, the presence of diabetes mellitus, coronary heart disease, and stroke or transient ischemic attack (TIA), and the use of statins. For control of hypertension, we additionally considered the use of combination antihypertensive therapy vs monotherapy.
3. RESULTS
3.1. Characteristics of the study participants
The 364 000 participants included 191 605 women (52.6%) and had a mean age of 53.4 (±17.7) years, and a mean body mass index of 23.4 (±3.3) kg/m2. Men, compared with women, had a significantly (P < .0001) higher prevalence of overweight and obesity (45.0% vs 36.7%) and higher proportions of current smoking (20.3% vs 1.9%) and alcohol intake (15.0% vs 1.5%). However, they had similar (P ≥ .05) prevalence of diabetes mellitus (4.1%), coronary heart disease (1.5%), and stroke or TIA (1.1%), and similar use of statins (3.0%, Table 1).
Table 1.
Characteristics of the study participants
| Characteristic |
Men (n = 172 395) |
Women (n = 191 605) |
P value |
|---|---|---|---|
| Age, years | 53.6 ± 17.7 | 53.2 ± 17.7 | <.0001 |
| Body height, cm | 168.6 ± 6.7 | 159.1 ± 6.3 | <.0001 |
| Body weight, kg | 67.4 ± 10.0 | 58.6 ± 9.0 | <.0001 |
| Body mass index, kg/m2 | 23.7 ± 3.2 | 23.2 ± 3.4 | <.0001 |
| Waist circumference, cm | 84.1 ± 9.1 | 79.3 ± 9.4 | <.0001 |
| Hip circumference, cm | 94.6 ± 9.5 | 90.8 ± 9.1 | <.0001 |
| Waist‐to‐hip ratio | 0.89 ± 0.08 | 0.88 ± 0.08 | <.0001 |
| Systolic blood pressure, mm Hg | 125.9 ± 15.5 | 122.4 ± 16.7 | <.0001 |
| Diastolic blood pressure, mm Hg | 77.8 ± 9.9 | 75.0 ± 9.4 | <.0001 |
| Use of antihypertensive drugs, % | 10.5 | 10.5 | .80 |
| Current smoking, % | 20.3 | 1.9 | <.0001 |
| Alcohol intake, % | 15.0 | 1.5 | <.0001 |
| Diabetes mellitus, % | 4.1 | 4.1 | .83 |
| Coronary heart disease, % | 1.5 | 1.4 | .21 |
| Stroke or transient ischemic attack, % | 1.1 | 1.1 | .07 |
| Use of lipid lowering drugs, % | 3.0 | 3.0 | .86 |
Values are mean ± SD or percentage of the column total.
Men, compared with women, had higher systolic/diastolic blood pressure (125.9/77.8 vs 122.4/75.0 mm Hg, P < .0001), especially in the younger age range (Figure 1). Overall, automatic electronic blood pressure monitors were used in 89.7% of the participants, and a mercury sphygmomanometer in 11.3% of the participants.
Figure 1.
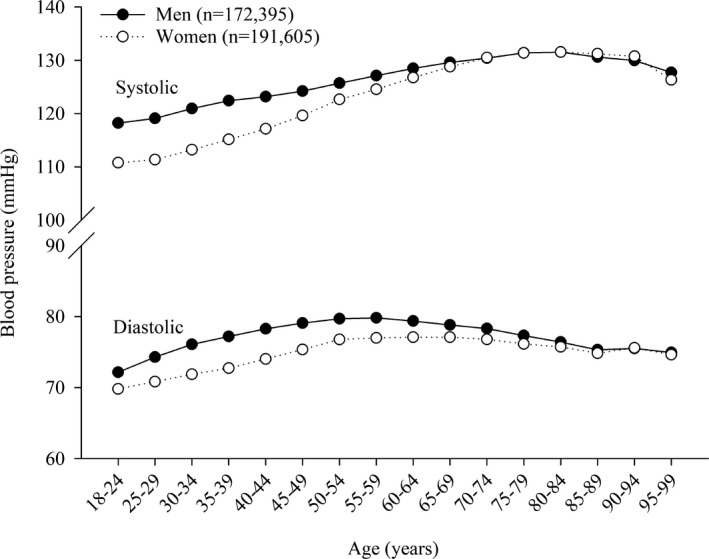
Systolic and diastolic blood pressure by age and gender. Values in dots or circles are mean in each group
3.2. Prevalence of hypertension
The prevalence of hypertension was 24.7%, being higher in men than in women (27.2% vs 22.5%, Table 2). The gender‐based difference was prominent in people less than 65 years of age (18.3% vs 39.0%, P < .0001) and became insignificant in people of 65 years or older (Figure 2).
Table 2.
Prevalence, awareness, treatment, and control of hypertension
| All | Men | Women | P value | |
|---|---|---|---|---|
| All participants | n = 364 000 | n = 172 395 | n = 191 605 | |
| Prevalence, % | 24.7 | 27.2 | 22.5 | <.0001 |
| Hypertensive patients | n = 89 925 | n = 46 819 | n = 43 106 | |
| Awareness, % | 60.1 | 57.3 | 63.5 | <.0001 |
| Treatment, % | 42.5 | 38.6 | 46.7 | <.0001 |
| Control, % | 25.4 | 22.9 | 28.1 | <.0001 |
| Treated hypertensive patients | n = 38 207 | n = 18 075 | n = 20 132 | |
| Treated and controlled, % | 59.8 | 59.3 | 60.3 | .049 |
Values are percentage of patients.
Figure 2.
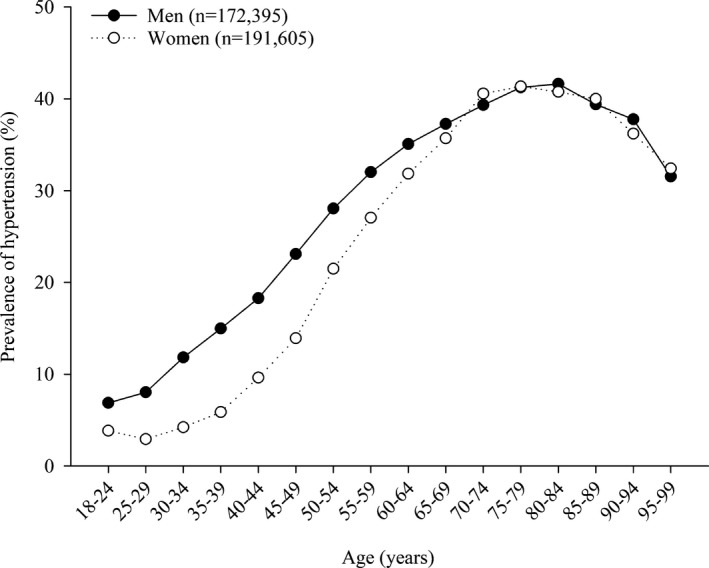
Prevalence of hypertension by age and gender. The number of men and women is given
In multiple stepwise logistic regression analyses, the prevalence of hypertension was significantly (P < .0001) higher in men (odds ratio [OR] 1.08, 95% confidence interval [CI] 1.06‐1.10) and with age advancing (for each 10‐year increase, OR 1.51, 95% CI 1.49‐1.51), current smoking (OR 1.25, 95% CI 1.22‐1.29), the presence of diabetes mellitus (OR 1.76, 95% CI 1.70‐1.83), coronary heart disease (OR 1.38, 95% CI 1.30‐1.47), and stroke or TIA (OR 1.43, 95% CI 1.33‐1.54) and the use of statins (OR 1.55, 95% CI 1.49‐1.62).
3.3. Awareness and treatment of hypertension
In all hypertensive patients (n = 89 925), the awareness and treatment of hypertension was 60.1% and 42.5%, respectively (Table 2), being significantly (P < .0001) higher in women than in men (awareness: 63.5% vs 57.3%; treatment: 46.7% vs 38.6%).
In multiple stepwise logistic regression, the odds for unawareness vs awareness of hypertension was significantly (P < .0001) higher in men (OR 1.41, 95% CI 1.37‐1.46) and lower with age advancing (for each 10‐year increase, OR 0.71, 95% CI 0.70‐0.71), current smoking (OR 0.53, 95% CI 0.48‐0.59), the presence of diabetes mellitus (OR 0.39, 95% CI 0.36‐0.42), coronary heart disease (OR 0.36, 95% CI 0.31‐0.41), and stroke or TIA (OR 0.38, 95% CI 0.33‐0.45), and the use of statins (OR 0.19, 95% CI 0.17‐0.21, Figure 3).
Figure 3.
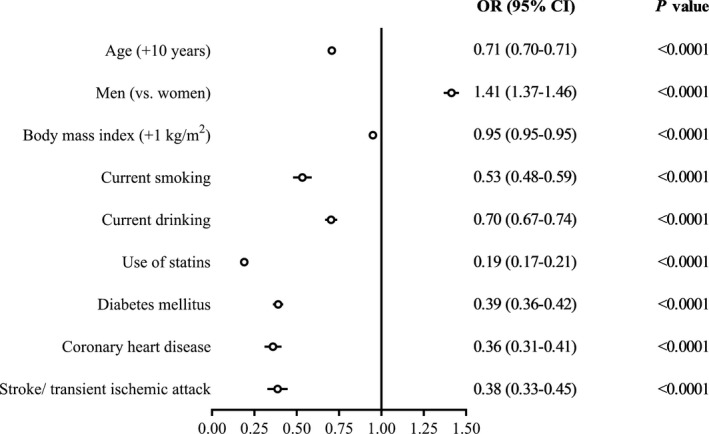
Odds (95% confidence intervals) for unawareness vs awareness of hypertension in hypertensive patients (n = 89 925). Symbols on the right side of the vertical unity (1) line indicate increased odds of unawareness
In similar multiple stepwise logistic regression analyses, the odds for untreated vs treated hypertension was significantly (P ≤ .04) higher in men (OR 1.41, 95% CI 1.35‐1.47) and current smokers (OR 1.07, 95% CI 1.01‐1.14), and lower with age advancing (for each 10‐year increase, OR 0.89, 95% CI 0.88‐0.90), the presence of coronary heart disease (OR 0.58, 95% CI 0.51‐0.65), and stroke or TIA (OR 0.88, 95% CI 0.78‐0.99), and the use of statins (OR 0.83, 95% CI 0.77‐0.90, Figure 4).
Figure 4.
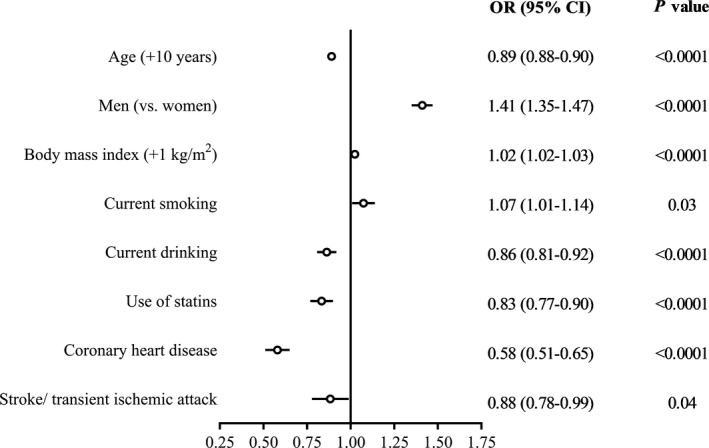
Odds (95% confidence intervals) for untreated vs treated hypertension in all hypertensive patients (n = 89 925). Symbols on the right side of the vertical unity (1) line indicate increased odds of untreated hypertension
3.4. Control of hypertension in treated hypertensive patients
The control rate of hypertension was 25.4% in all hypertensive patients (n = 89 925) and 59.8% in treated hypertensive patients (n = 38 207, Table 2), being significantly (P ≤ .049) higher in women than in men (control: 28.1% vs 22.9%; treated and controlled: 60.3% vs 59.3%).
In multiple logistic regression analyses in treated hypertensive patients, the odds for uncontrolled vs controlled hypertension was (P ≤ .03) higher with age advancing (for each 10‐year increase, OR 1.02, 95% CI 1.00‐1.04) and current smoking (OR 1.18, 95% CI 1.11‐1.26), and lower with the presence of diabetes mellitus (OR 0.93, 95% CI 0.87‐1.00) and coronary heart disease (OR 0.87, 95% CI 0.79‐0.96), and the use of statins (OR 0.87, 95% CI 0.81‐0.94, Figure 5).
Figure 5.
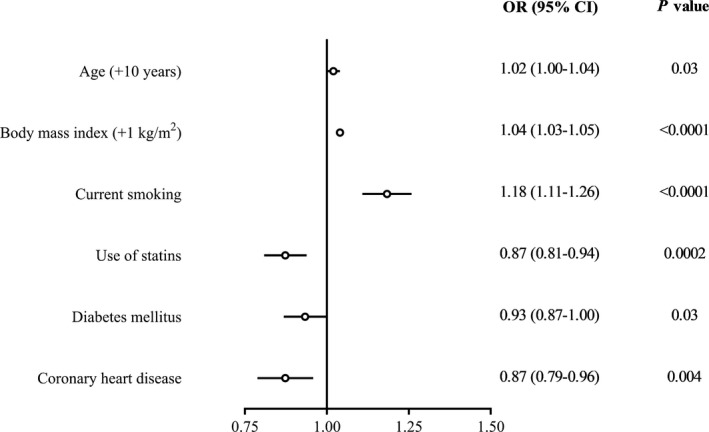
Odds (95% confidence intervals) for uncontrolled vs controlled hypertension in treated hypertensive patients (n = 38 207). Symbols on the right side of the vertical unity (1) line indicate increased odds of uncontrolled hypertension
In further analyses in treated hypertensive patients with specific antihypertensive drug information (n = 19 523, Table 3), the odds for uncontrolled vs controlled hypertension was additionally higher with the use of monotherapy (vs combination therapy, OR 1.13, 95% CI 1.06‐1.21, P = .0003).
Table 3.
Use of antihypertensive drugs in 19 523 treated hypertensive patients who volunteered detailed information on the use of antihypertensive drugs
| Antihypertensive treatment | Percentage of patients, % | Control rate, % |
|---|---|---|
| Monotherapy (n = 14 305) | 73.3 | 60.6 |
| Angiotensin‐converting enzyme inhibitors | 4.9 | 50.0 |
| Angiotensin receptor blockers | 17.1 | 68.2 |
| Long‐acting calcium channel blockers | 37.2 | 60.9 |
| Short‐acting calcium channel blockers | 7.2 | 51.1 |
| Diuretics | 2.7 | 49.4 |
| β‐blockers | 2.7 | 68.2 |
| Other a | 1.4 | 51.6 |
| Combination therapy (n = 5218) | 26.7 | 63.1 |
| Fixed‐dose combination | 8.5 | 58.1 |
| An angiotensin‐converting enzyme inhibitor or an angiotensin receptor blocker plus hydrochlorothiazide | 4.5 | 71.6 |
| Hydrochlorothiazide plus reserpine or clonidine | 4.0 | 42.9 |
| Free combination | 18.2 | 65.4 |
Values are percentage of patients.
Including α‐blockers, reserpine, clonidine, isosorbide mononitrate, and Chinese herbs.
4. DISCUSSION
Our study showed that the awareness, treatment, and control rates of hypertension were consistently lower in men than women and higher in patients with comorbid diseases, such as diabetes mellitus, coronary heart disease, stroke or TIA, or the use of statins, than those without. Advancing age was positive for the awareness and treatment, but negative for the control of hypertension. Cigarette smoking was positive for the awareness, but negative for the treatment and control of hypertension. In addition, the use of monotherapy was also negative for the control of hypertension.
Our study identified current cigarette smoking as an important negative factor for the management of hypertension. Although cigarette smokers had higher awareness of hypertension than non‐smokers, they had lower treatment and control rate of hypertension. The prevalence of cigarette smoking is high in men and increases substantially in women recently. 10 Cigarette smokers have a higher prevalence of hypertension, 11 including masked hypertension. 12 , 13 Smokers apparently are one of the major target populations for the management of hypertension.
Our study also identified the inadequate use of antihypertensive treatment as another modifiable risk factor for the management of hypertension. Indeed, combination antihypertensive therapy was under‐used in the present study, in spite of the low control rate of hypertension. Recent hypertension guidelines consistently recommended initial combination antihypertensive therapy for the management of hypertension. 14 , 15 , 16 , 17 With the increasing availability of single‐pill combination antihypertensive drugs in China, 18 combination antihypertensive therapy would be a choice of approaches for improving control of hypertension.
Our study identified several non‐modifiable factors for the worse management of hypertension, such as male gender and younger age. These observations are in keeping with the results of numerous previous studies. 19 , 20 We might have to build technological platforms to tackle the problems in these special populations. We are currently building a Web‐based and WeChat‐linked blood pressure measuring system in China mainly in public areas such as office buildings, shopping malls, airports, railway stations and so on, where younger people often walk around. 21 Hopefully, with these approaches, the awareness of hypertension will be improved in these populations.
We found that several comorbid diseases were significantly associated with a better management of hypertension. These observations are in line with the results of many previous studies. 22 When a patient sees a doctor for another disease, blood pressure may be measured, and hypertension may be diagnosed and treated. In addition, because of the comorbid diseases, the risk is high, and the patient may be more careful and mindful in the management of the diseases.
A major limitation of our study was the non‐random sampling approach for the recruitment of the study participants. Nonetheless, the estimations on the awareness, treatment and control were similar to the results of the recent China nationwide hypertension survey. 1 In addition, we did not succeed in collecting detailed information on the use of antihypertensive drugs in all participants. Our analysis for this topic had to be restricted to a much smaller number of study participants.
In conclusion, our study identified several factors as barriers to blood pressure control in China, such as male gender, younger age, current smoking, and the under‐use of combination therapy. A major implication of our study is that future initiatives in China might have to target these major barriers for the management of hypertension.
CONFLICT OF INTEREST
None.
ACKNOWLEDGMENT
The authors gratefully acknowledge the voluntary participation of the study participants and investigators from all measurement sites. Omron Healthcare (Kyoto, Japan) donated blood pressure measuring devices and provided logistics support via Shanghai ZhiZhong Technology (Shanghai, China). Shanghai Hesi Technology also provided blood pressure measuring devices.
Chen X, Xu S‐K, Guo Q‐H, et al. Barriers to blood pressure control in China in a large opportunistic screening. J Clin Hypertens. 2020;22:835–841. 10.1111/jch.13850
REFERENCES
- 1. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137:2344‐2356. [DOI] [PubMed] [Google Scholar]
- 2. Li LM, Rao KQ, Kong LZ, et al. A description on the Chinese National Nutrition and Health Survey in 2002. Chin J Epidemiol. 2005;26:478‐484. (In Chinese). [PubMed] [Google Scholar]
- 3. Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524‐532. [DOI] [PubMed] [Google Scholar]
- 4. Bundy JD, He J. Hypertension and related cardiovascular disease burden in China. Ann Glob Health. 2016;82:227‐233. [DOI] [PubMed] [Google Scholar]
- 5. Stefler D, Roever L. Hypertension and consequent mortality risk in China. J Epidemiol Community Health. 2018;72:1071‐1072. [DOI] [PubMed] [Google Scholar]
- 6. Beaney T, Schutte AE, Tomaszewski M, et al. May Measurement Month 2017: an analysis of blood pressure screening results worldwide. Lancet Glob Health. 2018;6:e736‐e743. [DOI] [PubMed] [Google Scholar]
- 7. Chen X, Xu SK, Li Y, et al. May Measurement Month 2017: an analysis of blood pressure screening results in China‐East Asia. Eur Heart J Suppl. 2019;21(Suppl D):D37‐D39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Beaney T, Burrell LM, Castillo RR, et al. May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of hypertension. Eur Heart J. 2019;40:2006‐2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on Hypertension. Lancet. 2016;388:2665‐2712. [DOI] [PubMed] [Google Scholar]
- 10. Wang M, Luo X, Xu S, et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross‐sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7:35‐45. [DOI] [PubMed] [Google Scholar]
- 11. Halperin RO, Gaziano JM, Sesso HD. Smoking and the risk of incident hypertension in middle‐aged and older men. Am J Hypertens. 2008;21:148‐152. [DOI] [PubMed] [Google Scholar]
- 12. Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941‐948. [DOI] [PubMed] [Google Scholar]
- 13. Kang YY, Li Y, Huang QF, et al. Accuracy of home versus ambulatory blood pressure monitoring in the diagnosis of white‐coat and masked hypertension. J Hypertens. 2015;33:1580‐1587. [DOI] [PubMed] [Google Scholar]
- 14. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269‐1324. [DOI] [PubMed] [Google Scholar]
- 15. Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953‐2041. [DOI] [PubMed] [Google Scholar]
- 16. Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235‐1481. [DOI] [PubMed] [Google Scholar]
- 17. Writing Group of the 2018 Chinese Guidelines for the Management of Hypertension . Chinese guidelines for prevention and treatment of hypertension ‐ a report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16:182‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang JG, Zeng WF, He YS, et al. Valsartan/amlodipine compared with nifedipine GITS in patients with hypertension inadequately controlled by monotherapy. Adv Ther. 2013; 30:771‐783. [DOI] [PubMed] [Google Scholar]
- 19. Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736‐742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moon JY, Park KJ, Hwangbo Y, et al. A trend analysis of the prevalence, awareness, treatment, and control of hypertension by age group. J Prev Med Public Health. 2013;46:353‐359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang JG. Unique approaches to hypertension control in China. Ann Transl Med. 2018;6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sheng CS, Liu M, Kang YY, et al. Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Hypertens Res. 2013;36:824‐848. [DOI] [PubMed] [Google Scholar]


