The current high salt intake is a leading dietary risk factor, accounting for over 3 million deaths and 70 million disability‐adjusted life‐years (DALYs) in 2017 worldwide.1 The World Health Organization (WHO) has recommended a reduction in population salt intake from the current level of ≈10 g/d to less than 5 g/d for all countries around the world. Member States of the WHO have committed to a 30% reduction by 2025.2 Salt reduction is an important part of the WHO’s 13th General Program of Work3 and is aligned with Sustainable Development Goal 3—by 2030, to reduce premature mortality from Non‐Communicable Diseases (NCDs) by one‐third. However, several recent studies4, 5, 6, 7 with flawed methodologies have caused controversy, challenging WHO’s recommendations and efforts in reducing salt intake worldwide. In this article, we provide a brief update on the latest evidence, with a focus on the effects of salt on blood pressure (BP) and cardiovascular disease (CVD). We will also provide a short summary of current salt reduction activities in various countries.
1. EVIDENCE ON SALT, BP AND CVD
Consuming too much salt is associated with multiple health conditions, for example, kidney disease, stomach cancer, osteoporosis, and evidence is strongest for its effect on raising BP which in turn increases the risk of CVD, including strokes, heart diseases, and heart failure.8 CVD is the leading cause of premature deaths in the world and is projected to remain so in the coming decades, as progress on reducing CVD mortality has stalled and, indeed, since 2007 CVD mortality has increased worldwide.9
The causal relationship between salt intake and BP is well established, as evidenced by several lines of research including animal experiments, human genetics, physiological studies, epidemiology, migration, population‐based intervention studies, and clinical trials.10 Despite this, Graudal et al11 in a series of meta‐analyses of randomized trials, including the latest updated one published in The Cochrane Library in April 2017, claimed that salt reduction had no or very little effect on BP in normotensive individuals, and as such, population salt reduction was not warranted. However, this conclusion for public health is inappropriate given the nature of the studies included in the meta‐analysis, that is, trials of very short duration and comparing acute salt loading to abrupt and severe salt restriction (eg, from 20 to less than 1 g/d for only a few days).11 Such acute and large changes in salt intake are known to cause large neural‐hormonal responses, which are minimal with longer‐term modest reduction in salt intake as currently recommended.12 Two other meta‐analyses12, 13 that excluded these very short and acute salt restriction trials have demonstrated that a modest reduction in salt intake over a longer period of time (which corresponds to the current public health recommendations) has a significant effect on BP in both normotensive and hypertensive individuals, in men and women, and in all ethnic groups, with a linear dose‐response relationship within the range from 3 to 12 g/d, that is, the lower the salt intake, the lower the BP.
Raised BP throughout its range starting from 115/75 mm Hg is a major cause of CVD.14 A reduction in salt intake lowers BP and would therefore reduce CVD risk. Indeed, various types of studies have demonstrated that a lower salt intake is associated with a lower risk of CVD and all‐cause mortality.8, 15, 16, 17, 18 However, a few recent cohort studies have suggested a J‐ or U‐shaped relationship, with both lower and higher salt intake being associated with an increased risk.4, 5, 6, 7 Based on these results, a working group from the World Heart Federation, the European Society of Hypertension and the European Public Health Association have suggested that salt intake should only be reduced in countries with an intake above 12.5 g/d,19 and for the majority of countries, there is no need to reduce salt intake.19 These cohort studies, however, have several severe methodological problems, such as reverse causality and biased estimates of an individual’s usual salt intake from a single spot urine with a formula. A recent analysis of the Trials of Hypertension Prevention (TOHP) follow‐up data has clearly illustrated that inaccurate estimation of salt intake is an important contributor to the paradoxical J‐shaped findings reported in some cohort studies.20, 21 When salt intake was measured by the most accurate method of multiple nonconsecutive 24‐hour urinary sodium excretions, there was a direct linear association between salt intake and CVD events17 and all‐cause mortality, down to a level of 3 g/d (Figure 1),18 which is consistent with the linear relationship between salt intake and BP.22 However, when accurately measured salt intake was replaced with estimated values from sodium concentration using a formula, the direct linear relationship was altered and there appeared to be a J‐ or U‐shaped association between the estimated salt intake and mortality (Figure 1).20, 21 Importantly, when sodium concentration was kept constant in the formulas, the estimated salt intake appeared to be inversely related to mortality at lower levels of salt intake, that is, the lower the salt intake, the higher the risk of death.21 These findings clearly indicate that variables used in the formulas, other than sodium, could at least partially explain the increased risk of mortality with a lower salt intake reported in some cohort studies. This is not surprising, given that other variables in the formulas (eg, age, sex, body weight, and creatinine concentration) are known to be associated with mortality.23, 24
Figure 1.
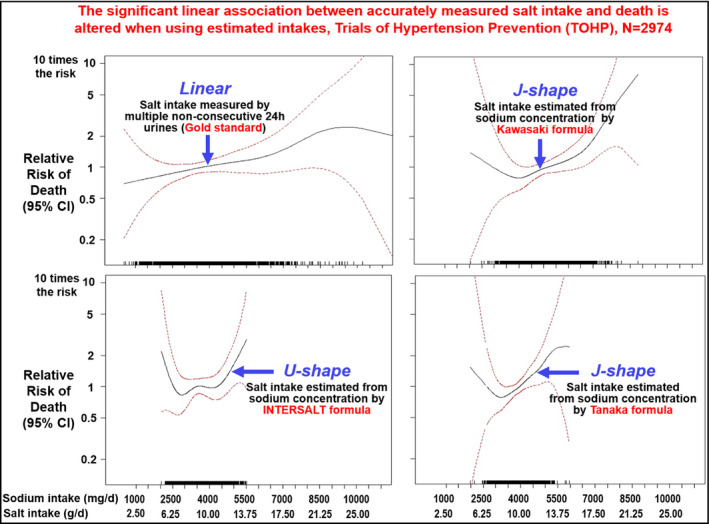
Relationship between average estimates of 24‐h urinary sodium excretion and all‐cause mortality adjusted for age, sex, race/ethnicity, clinic, treatment assignment, education status, baseline weight, alcohol use, smoking, exercise, and family history of cardiovascular disease. Rug plot indicates distribution of sodium excretion (adapted from He et al, Hypertension 2019).21
Almost all cohort studies have used salt intake estimated at baseline and then looked at its association with subsequent occurrence of CVD events or death. Such studies cannot capture the changes in salt intake during many years’ follow‐up. A recent study compared salt intake measured by a single baseline 24‐hour urine vs multiyear 24‐hour urine collections and associated CVD events and mortality.25 The results showed that the risk increased by up to 85% with the use of salt intake from 1 to 5 years’ follow‐up instead of single baseline intake. These findings clearly demonstrate the importance of accurately measuring individuals’ long‐term salt intake in association studies. The study using individuals’ long‐term salt intake showed that those with a salt intake of over 10.8 g/d had a 73%‐80% increase in CVD events and mortality compared with the individuals who had an intake of less than 7.5 g/d.25 These findings are in agreement with the observed falls in CVD mortality attributed to salt reduction in countries with robust salt reduction strategies, for example, Finland and the UK.16, 26, 27 These latest studies provide further strong support for population‐wide reduction in salt intake.
2. UPDATE ON SALT REDUCTION ACTIVITIES
2.1. United Kingdom (UK)
The UK once led the world on salt reduction by setting progressive lower salt targets for over 85 categories of foods. From 2003 to 2011, salt content in many food categories had been reduced by 20%‐50% and salt intake in the population had fallen from 9.5 to 8.1 g/d, accompanied by a decrease in population BP and cardiovascular mortality, as well as annual cost‐savings of ≈£1.5 billion for the health service.16 However, in recent years the UK’s salt reduction program has seen a loss of momentum. In 2011, responsibility for salt reduction was moved from the Food Standards Agency to the Department of Health and Social Care and their Public Health Responsibility Deal, which made the food industry responsible for improving nutrition including reducing salt in their products. Not surprisingly, progress stalled,28, 29 with evaluations highlighting the failure of the Responsibility Deal in achieving its objectives, including poor quality monitoring reports with no independent verification.30 Following the 2015 general election, the Responsibility Deal was dissolved and it was not until 2016 that responsibility for salt reduction was then passed to Public Health England (PHE). PHE’s analysis of the 2017 salt reduction targets, released in December 2018, found that half of the top 15 contributors to salt intake in the UK did not meet their average salt content targets. While 73% of retailer products met their average targets, just 37% of manufacturers met theirs, and overall, a fifth (19%) of products did not meet their maximum targets despite these targets being set in 2014.31
The UK’s Secretary of State for Health, as part of his Prevention Vision “Prevention is better than cure”, which was released in November 2018, promised new salt reduction actions by Easter 2019. These plans were released in July 2019, suggesting targets will be set in 2020 to be met by 2023.32
2.2. Other countries
South Africa was one of the first countries to introduce mandatory salt reduction targets across a range of processed foods, covering the main contributors of salt in the diet. The targets were implemented in two phases; the first phase of targets was due to be met by June 2016 and the second phase of lower targets by June 2019. An analysis in 2017 found that in the early stages of the policy implementation, two thirds (67%) of products surveyed already had a salt level equivalent to or less than the legislated limit. However, less than 30% of breads–the main source of salt in the South African diet–met their mandated limit, highlighting the level of work still to do.33 Close monitoring of salt levels in foods is required to ensure compliance with the legislation.
While South Africa is leading the way with a mandated salt reduction strategy, other countries have followed the UK’s voluntary salt‐reduction model. Voluntary actions in Australia were initially led by the Australian division of World Action on Salt and Health (WASH) and then the Food and Health Dialogue, a partnership between government, the food industry and nongovernmental organisations. In 2018, the Reformulation Working Group of the Australian Healthy Food Partnership opened a consultation on draft voluntary salt, sugar, and saturated fat reduction targets. The draft targets covered the main contributors of these risk‐associated nutrients to the Australian diet and as of February 2019, they are still under review.34
In 2018, the European Salt Action Network discussed the evidence relating to salt reduction and identified inadequacies and bias in recent studies that have alluded to a J‐shaped association between salt consumption and cardiovascular events.35 As a result, in December of that year they issued a statement in support of salt reduction to prevent CVD. Many European countries have implemented salt reduction strategies in recent years. In 2018, the Spanish Agency for Consumer Affairs, Food and Nutrition (AECOSAN) released their Collaboration Plan for the Improvement of the Composition of Food and Beverages, which committed to reducing salt levels in various food categories, such as bakery and meat products, leading to an overall 10% reduction in salt content by 2020. The Collaboration Plan has the commitment of more than 500 companies and covers restaurant, catering food, and food sold in vending machines.36 The plan builds upon AECOSAN’s work to reduce salt in crisps and savory snacks, meat products and bread.37
Bread is a key staple food but also a leading source of salt in many diets around the world. As a result, many countries have focused their salt reduction efforts on bread, including the Gulf region. By 2014, the Kuwait Flour Mills and Bakeries Company, a government‐owned bakery, had achieved a 20% reduction in the salt content of bread products including white flatbread and whole wheat toast.38 Between 2015 and 2017, Oman achieved a 10% reduction in the salt content of bread items within its main bakeries.39 Saudi Arabia’s Healthy Food Strategy, released in 2018, commits to setting a maximum level of salt in bread and bakery products, in addition to identifying food categories with high salt content and working to gradually reduce salt levels by 2030.40
Not all countries have seen success with voluntary salt reduction strategies; a key example is Canada. A 2018 analysis of the food industry’s progress toward salt reduction targets in the country–set in 2012 and due to be met in 2016—revealed that just 14% of products met their targets. Almost half (48%) of products did not achieve any meaningful reduction in salt content and of these, six product categories actually showed an increase in salt content.41
The USA has similarly seen poor progress. In 2016, the US Food and Drug Administration (FDA) proposed voluntary salt reduction targets, covering food manufacturers and the out of home sector, and sought comment from the food industry and other stakeholders. The FDA recommended reducing the salt content of foods in 150 categories to achieve an average population salt intake of less than 6 g/d.42 While these targets were met with enthusiastic support from health charities and nongovernmental organisations, claims of scientific inaccuracy and opposition from the food industry delayed their implementation. However, in March 2018, the FDA announced a renewed focus on nutrition with their Nutrition Innovation Strategy. As part of this announcement, the FDA Commissioner stated that salt reduction is an essential component of any meaningful nutrition strategy and committed to releasing updated salt reduction targets in 2019.43 In March 2019, the National Academies of Sciences, Engineering, and Medicine (NASEM) released a report confirming adult salt intake should be reduced from the current average level of 8.6 g/d to less than 6 g/d.44
Chile has pioneered a different approach, implementing front‐of‐pack warning labels on products with more than 1 g of salt per 100 g of product 36 months after implementation, in addition to marketing restrictions. These restrictions prohibit advertising of products high in salt, sugar, saturated fat, and calories on TV programs or websites targeted at children or where children make up more than 20% of the audience and the use of cartoon characters in marketing or advertisements of these products to children.45 The aim of these measures was to drive reformulation in the country. While the evaluation of these measures is ongoing, initial analysis suggests that children have had a positive response to the labeling, becoming promoters of change within their families.46 In 2019, Peru followed Chile’s lead with mandatory warning labels on products with more than 2 g of salt per 100 g of product.47
In the Asian‐Pacific region, several countries, for example, China, India, and Malaysia, have started salt reduction initiatives which included the collection of 24‐hour urine samples and dietary surveys to provide data for the development of a salt reduction program, but progress has been very slow. In these countries, most of the salt in the diet is added by the consumers during cooking or in sauces. It is extremely challenging to reduce salt intake in such settings due to the difficulty in changing dietary behavior. Various approaches have been developed with encouraging results in local/regional studies. Replacing usual salt with a potassium‐enriched salt, which is low in sodium and high in potassium, has been shown to lower BP and reduce CVD mortality.48, 49 A recent study in northern China demonstrated that children could play a key role in helping reduce salt intake in the whole families.50 The Chinese central government has included salt reduction as one of the key components of China's health development agenda, for example, “Healthy China 2030”. In 2017, the action group Action on Salt China51 was set up with the aim of developing and implementing a comprehensive, effective, and sustainable national salt reduction program to help achieve WHO’s recommended salt intake in China.
3. CONCLUSIONS
Latest evidence from good quality studies has provided further strong support for a population‐wide reduction in salt intake. Paradoxical J‐shaped findings from methodologically flawed studies should not be used to derail critical public health policy, nor divert action. Gradual stepwise reduction in population salt intake as recommended by the WHO remains an achievable, affordable, effective, and an important strategy to prevent CVD worldwide. Several countries have been successful in reducing population salt intake16, 26, 27 and many other countries have started salt reduction initiatives, but progress has been slow. Urgent action is needed to speed up salt reduction in all countries in the world. A reduction in salt intake across the whole population, even by a small amount, will have an enormous benefit on public health and result in major cost‐savings to individuals, their families, and the health service.
CONFLICT OF INTEREST
FJH is a member of Consensus Action on Salt & Health (CASH) and World Action on Salt & Health (WASH). Both CASH and WASH are nonprofit charitable organisations, and FJH does not receive any financial support from CASH or WASH. MB is an employee of CASH. GAM is Chairman of Blood Pressure UK (BPUK), Chairman of CASH, WASH, and Action on Sugar. BPUK, CASH, WASH and Action on Sugar are nonprofit charitable organisations. GAM does not receive any financial support from any of these organisations. MT has no disclosures to report.
AUTHOR CONTRIBUTION
FJH, MB, and MT drafted the manuscript. All authors contributed to revision and approved the final submitted manuscript.
ACKNOWLEDGEMENTS
FJH and GAM receive research funding from the National Institute of Health Research (NIHR) using Official Development Assistance funding (16/136/77). MT is funded by the NIHR grant. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
He FJ, Brown M, Tan M, MacGregor GA. Reducing population salt intake—An update on latest evidence and global action. J Clin Hypertens. 2019;21:1596–1601. 10.1111/jch.13664
REFERENCES
- 1. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;393:1958‐1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 3. World Health Organization . Draft thirteenth general programme of work 2019-2023. http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_4-en.pdf?ua=1. Accessed July 23, 2019.
- 4. Mente A, O'Donnell M, Rangarajan S, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465‐475. [DOI] [PubMed] [Google Scholar]
- 5. Mente A, O'Donnell M, Rangarajan S, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community‐level prospective epidemiological cohort study. Lancet. 2018;392:496‐506. [DOI] [PubMed] [Google Scholar]
- 6. O’Donnell M, Mente A, Rangarajan S, et al. Joint association of urinary sodium and potassium excretion with cardiovascular events and mortality: prospective cohort study. BMJ. 2019;364:l772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612‐623. [DOI] [PubMed] [Google Scholar]
- 8. He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15:371‐377. [DOI] [PubMed] [Google Scholar]
- 9. Institute for Health Metrics and Evaluation (IHME) . Findings from the Global Burden of Disease Study 2017. Seattle, WA: IHME; 2018. [Google Scholar]
- 10. He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52:363‐382. [DOI] [PubMed] [Google Scholar]
- 11. Graudal NA, Hubeck‐Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta‐analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 13. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta‐analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903‐1913. [DOI] [PubMed] [Google Scholar]
- 15. He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta‐analysis of outcome trials. Lancet. 2011;378:380‐382. [DOI] [PubMed] [Google Scholar]
- 16. He FJ, Pombo‐Rodrigues S, MacGregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4:e004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014;129:981‐989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cook NR, Appel LJ, Whelton PK. Sodium intake and all‐cause mortality over 20 years in the trials of hypertension prevention. J Am Coll Cardiol. 2016;68:1609‐1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mancia G, Oparil S, Whelton PK, et al. The technical report on sodium intake and cardiovascular disease in low‐ and middle‐income countries by the joint working group of the World Heart Federation, the European Society of Hypertension and the European Public Health Association. Eur Heart J. 2017;38:712‐719. [DOI] [PubMed] [Google Scholar]
- 20. He FJ, Campbell N, Ma Y, MacGregor GA, Cogswell ME, Cook NR. Errors in estimating usual sodium intake by the Kawasaki formula alter its relationship with mortality: implications for public health. Int J Epidemiol. 2018;47:1784‐1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. He FJ, Ma Y, Campbell N, MacGregor GA, Cogswell ME, Cook NR. Formulas to estimate dietary sodium intake from spot urine alter sodium‐mortality relationship. Hypertension. 2019;74(3):572‐580. [DOI] [PubMed] [Google Scholar]
- 22. He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension. 2003;42:1093‐1099. [DOI] [PubMed] [Google Scholar]
- 23. Yu E, Ley SH, Manson JE, et al. Weight history and all‐cause and cause‐specific mortality in three prospective cohort studies. Ann Intern Med. 2017;166:613‐620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Oterdoom LH, Gansevoort RT, Schouten JP, de Jong PE, Gans RO, Bakker SJ. Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis. 2009;207:534‐540. [DOI] [PubMed] [Google Scholar]
- 25. Olde Engberink R, van den Hoek TC, van Noordenne ND, van den Born BH, Peters‐Sengers H, Vogt L. Use of a single baseline versus multiyear 24‐hour urine collection for estimation of long‐term sodium intake and associated cardiovascular and renal risk. Circulation. 2017;136:917‐926. [DOI] [PubMed] [Google Scholar]
- 26. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006;49:59‐75. [DOI] [PubMed] [Google Scholar]
- 27. Laatikainen T, Critchley J, Vartiainen E, Salomaa V, Ketonen M, Capewell S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol. 2005;162:764‐773. [DOI] [PubMed] [Google Scholar]
- 28. MacGregor GA, He FJ, Pombo‐Rodrigues S. Food and the responsibility deal: how the salt reduction strategy was derailed. BMJ. 2015;350:h1936. [DOI] [PubMed] [Google Scholar]
- 29. Laverty AA, Kypridemos C, Seferidi P, et al. Quantifying the impact of the Public Health Responsibility Deal on salt intake, cardiovascular disease and gastric cancer burdens: interrupted time series and microsimulation study. J Epidemiol Commun Health. 2019;73:881‐887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Knai C, Petticrew M, Douglas N, et al. The public health responsibility deal: using a systems‐level analysis to understand the lack of impact on alcohol, food, physical activity, and workplace health sub‐systems. Int J Environ Res Public Health. 2018;15:2895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Salt targets 2017:Progress reportA report onthe foodindustry’s progress towardsmeetingthe 2017 salt target; December 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/765571/Salt_targets_2017_progress_report.pdf. Accessed July 25, 2019.
- 32. Department of Health and Social Care . Prevention is better than cure ‐ Our vision to help you live well for longer; 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/753688/Prevention_is_better_than_cure_5-11.pdf. Accessed July 25, 2019.
- 33. Peters S, Dunford E, Ware L, et al. The sodium content of processed foods in South Africa during the introduction of mandatory sodium limits. Nutrients. 2017;9:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Department of Health. Healthy Food Partnership. https://www1.health.gov.au/internet/main/publishing.nsf/Content/Healthy-Food-Partnership-Home?Open=&utm_source=health.gov.au&utm_medium=redirect&utm_campaign=digital_transformation&utm_content=healthyfoodpartnership Accessed July 25, 2019.
- 35. Cappuccio FP, Beer M, Strazzullo P. Population dietary salt reduction and the risk of cardiovascular disease. A scientific statement from the European Salt Action Network. Nutr Metab Cardiovasc Dis. 2018;29:107‐114. [DOI] [PubMed] [Google Scholar]
- 36. Collaboration PLAN for the improvement of the composition of food and beverages and other measures 2020. http://www.aecosan.msssi.gob.es/AECOSAN/docs/documentos/nutricion/EN_DOSSIER_PLAN_2020.pdf Accessed July 23, 2019.
- 37. Food reformulation . Collective agreements. http://www.aecosan.msssi.gob.es/en/AECOSAN/web/nutricion/ampliacion/reformulacion_alimentos.htm Accessed July 23, 2019.
- 38. World Health Organization . Kuwaitis lower blood pressure by reducing salt in bread. https://www.who.int/features/2014/kuwait-blood-pressure/en/. Accessed August 17, 2019.
- 39. Oman beating NCDs at the souk, the restaurant and the bakery doors. https://www.who.int/news-room/feature-stories/detail/oman-beating-ncds-at-the-souk-the-restaurant-and-the-bakery-doors Accessed July 23, 2019.
- 40. SFDA Healthy Food Strategy. https://www.sfda.gov.sa/ar/awareness/Documents/SFDA-HealthyFoodStrategy.pdf Accessed July 23, 2019.
- 41. Health Canada . Sodium Reduction in Processed Foods in Canada: An Evaluation of Progress toward Voluntary Targets from 2012 to 2016; 2018. https://www.canada.ca/en/health-canada/services/food-nutrition/legislation-guidelines/guidance-documents/guidance-food-industry-reducing-sodium-processed-foods-progress-report-2017.html Accessed July 25, 2019.
- 42. U.S. Department of Health and Human Services . Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods: Guidance for Industry ‐ Draft Guidance; 2016. https://www.fda.gov/media/98264/download Accessed July 25, 2019.
- 43. Gottlieb S. Reducing the Burden of Chronic Disease ‐ 29 March 2018. U.S. Food and Drug Administration; 2019. http://www.fda.gov/news-events/speeches-fda-officials/reducing-burden-chronic-disease-03292018 Accessed July 25, 2019.
- 44. Stallings V, Harrison M, Oria M et al. Dietary Reference Intakes for Sodium and Potassium. Washington (DC): National Academies Press; 2019. [PubMed] [Google Scholar]
- 45. Chile's Law on Food Labelling and Advertising: A Replicable Model for Latin America? https://ideas.llorenteycuenca.com/wp-content/uploads/sites/5/2016/05/160504_DI_report_food_chile_ENG.pdf Accessed July 21, 2019.
- 46. Correa T, Fierro C, Reyes M, et al. Responses to the Chilean law of food labeling and advertising: exploring knowledge, perceptions and behaviors of mothers of young children. Int J Behav Nutr Phys Act. 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gob.pe. Desde hoy el consumidor podrá elegir responsablemente qué alimentos consumer; 2019; published online June 17. https://www.gob.pe/institucion/minsa/noticias/29531-desde-hoy-el-consumidor-podra-elegir-responsablemente-que-alimentos-consumir Accessed July 29, 2019.
- 48. Chang H‐Y, Hu Y‐W, Yue C‐S, et al. Effect of potassium‐enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr. 2006;83:1289‐1296. [DOI] [PubMed] [Google Scholar]
- 49. Newberry SJ, Chung M, Anderson C, et al. Effects of dietary sodium and potassium intake on chronic disease outcomes and related risk factors: Agency for Healthcare Research and Quality (AHRQ); 2018. [PubMed]
- 50. He FJ, Wu Y, Feng X‐X, et al. School based education programme to reduce salt intake in children and their families (School‐EduSalt): cluster randomised controlled trial. BMJ. 2015;350:h770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. He FJ, Zhang P, Li Y, MacGregor GA. Action on salt China. Lancet. 2018;392:7‐9. [DOI] [PubMed] [Google Scholar]


