Abstract
The 2017 guidelines on the diagnosis and treatment of high blood pressure in adults were published by the American College of Cardiology and the American Heart Association. The impact on clinical outcomes and costs needs to be estimated prior to adopting these guidelines in China. Data from a nationally representative sample in China were analyzed. The prevalence and treatment were calculated based on the criteria of the 2017 guidelines and 2018 Chinese guidelines among participants aged ≥35 years old. Direct medical costs, as well as the averted disability adjusted of life years and cost saving from cardiovascular disease events prevented by controlling hypertension, were also estimated. The prevalence and treatment rate of hypertension were 32.0% and 43.4% according to the 2018 Chinese guidelines. Based on the 2017 guidelines, another 24.5% of the adult population (estimated 168.1 million) would be classified as having hypertension; of whom, about 32.1 million would need to be pharmaceutically treated to reach the current treatment rate of 43.4%. As a result, an estimated additional 42.7 billion US dollars of the direct medical cost would be required for lifetime therapy. By preventing cardiovascular events, the new guidelines would reduce lifetime costs by 3.77 billion US dollars, while preventing 1.41 million disability adjusted of life years lost. Application of the 2017 guidelines in China will substantially increase the prevalence of hypertension and produce a large increase in therapy costs, although it would prevent cardiovascular disease events and save disability adjusted of life years.
Keywords: China, cost, guidelines, hypertension, prevalence, treatment
1. INTRODUCTION
The American College of Cardiology (ACC) and the American Heart Association (AHA) recently released guidelines for the detection and management of hypertension in adults.1 Compared with previous guidelines, the 2017 ACC/AHA guidelines recommend using lower systolic and diastolic blood pressure (BP) levels to define hypertension (systolic BP ≥130 or diastolic BP ≥80 mm Hg), as well as recommending lifestyle changes or treatment for systolic BP/diastolic BP to a target <130/80 mm Hg. Also, the previous evidence indicated that intensive antihypertensive treatment with achieved blood pressure (BP) ≤140/90 mm Hg could further improve cardiovascular outcomes in Chinese hypertensive patients.2, 3
Khera et al4 examined the effect of the 2017 ACC/AHA guidelines on the prevalence as well as the eligibility for initiation and intensification of therapy using the data from the China Health and Retirement Longitudinal Study (CHARLS). However, CHARLS used the pooled cohort equations to predict cardiovascular disease (CVD) event rates, which are inaccurate in the Chinese population.5 Furthermore, the impact of the 2017 ACC/AHA guidelines on the economic burden of hypertension in China has not previously been studied.
The burden of hypertension and related diseases is increasing along with urbanization, rising incomes, and aging of the population in China.6, 7 Our recent study, using the China Hypertension Survey (CHS; 2012‐2015), suggested that there is high prevalence (23.2%), but low treatment (40.7%) and control rates (15.3%) of hypertension, based on the 2018 Chinese guidelines.8, 9 We used data from the nationally representative CHS study to estimate the impact of adopting the 2017 ACC/AHA guidelines on the prevalence and treatment of hypertension, as well as related health care costs and savings from hypertension control.
2. METHODS
2.1. Survey participants
The design and results of the CHS, conducted between October 2012 and December 2015, have been published previously.10 Briefly, a stratified, multistage random sampling method was used to obtain a nationally representative sample of 451 755 residents aged ≥18 years from 31 provinces in mainland China from October 2012 to December 2015. 10.
Meanwhile, a substudy, as previously published,11 was conducted among participants aged ≥35 years; in whom, blood samples, electrocardiograms, and echocardiograms were also collected. Two hundred sixty‐two cities and counties, selected in the first phase, were stratified into Eastern, Middle, and Western regions, representing the varying economic development status in China. Using simple random sampling, 16 cities and 17 counties were selected, including seven cities and seven counties in the Eastern region, six cities and six counties in the Middle region, and three cities and four counties in the Western region. From these sites, 56 000 participants were randomly selected and invited; of whom, 34 994 responded (62.5%). We excluded 4130 participants with missing data on variables of interest, which left 30 864 individuals eligible to estimate the 10‐year atherosclerotic cardiovascular disease (ASCVD) and the percentage of recommended antihypertensive medication use in Chinese adults according to the 2017 ACC/AHA guidelines. The excluded participants were older and more often urban residents, while there was no difference in sex and BMI compared with the included participants (Table S1). To maintain consistency, 320 409 participants aged ≥35 years selected from CHC study were used to estimate the prevalence, awareness, and control according to the 2018 Chinese guidelines and the 2017 ACC/AHA guidelines in the present study.
Informed consent was obtained from each participant before data collection. The ethics committee of Fuwai Hospital approved the study.
2.2. Training and data collection
A standardized questionnaire developed by the coordinating center at Fuwai Hospital was administered by trained staff to obtain information on demographic characteristics, socioeconomic factors, and CVD events (including stroke and coronary heart disease [CHD]). The average of three BP readings, measured with the OMRON HBP‐1300 Professional Portable Blood Pressure Monitor (OMRON), was used for analysis.
2.3. Outcome definitions
In the 2018 Chinese guidelines, hypertension was defined as systolic BP ≥140 mm Hg, and/or diastolic BP ≥90 mm Hg, and/or use of antihypertensive medicine within the preceding 2 weeks.9 According to the 2017 ACC/AHA guidelines, hypertension was defined as systolic BP ≥130 mm Hg, and/or diastolic BP ≥80 mm Hg, and/or use of antihypertensive medicine within the preceding 2 weeks; stage 1 of hypertension as systolic BP 130‐139 and/or diastolic BP 80‐89 mm Hg; stage 2 as systolic/diastolic BP ≥140 and/or 90 mm Hg; and elevated BP as systolic BP 120‐129 and diastolic BP <80 mm Hg and without antihypertensive medications. The treatment of hypertension was defined as self‐reported use of antihypertensive medication within 2 weeks at the time of the interview, and BP control was defined as systolic BP <140 mm Hg and diastolic BP <90 mm Hg according to the 2018 Chinese guidelines, or <130 and <80 mm Hg according to the 2017 ACC/AHA guidelines, respectively. The recommended treatment threshold by 2017 ACC/AHA guidelines was as follows: (a) patients with systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg; (b) patients with systolic BP of 130‐139 mm Hg or diastolic BP 80‐89 mm Hg, and with one of the following criteria: ≥75 years old, 10‐year predicted risk of developing atherosclerotic cardiovascular disease ≥10%,5 pre‐existing heart failure, coronary heart disease, stroke, chronic kidney disease, or diabetes mellitus.
2.4. Cost and DALY
The additional costs of antihypertensive medications and direct medical costs, based on the 2017 ACC/AHA guidelines, were estimated with an assumption of reaching the same treatment rate (43.4%) as for the 2018 Chinese guidelines. Direct medical costs were defined as the cost associated with outpatient visits, diagnosis/tests, procedures, hospitalizations for diagnosis or therapy, and antihypertensive medications. Based on our previous studies,12, 13 the cost of monotherapy, single‐pill combinations, two‐drug combinations, and three or more antihypertensive drugs was 27.0, 8.2, 98.7, and 118.4 US dollars per person per year, respectively; the direct medical costs were 115.7 and 109.0 US dollars per person per year in urban and rural areas.12, 13 Lifetime direct costs were calculated using the following equation: (life expectancy estimated by the World Bank14 − average age of hypertensive patients who recommended but not receive antihypertensive drugs treatment in our study) × annual estimate of direct medical costs.
The Felodipine Event Reduction (FEVER) study, a prospective, multicenter, double‐blind, randomized, placebo‐controlled, parallel group trial in the Chinese population, indicated that 4.7 stroke events and 1.7 CHD events would be prevented in 1000 patients by controlling BP to ≤140/90 mm Hg.2, 3 So, the number of prevented events was calculated as patients with drug therapy multiplied by 4.7/1000 for strokes or 1.7/1000 for CHD. The disability adjusted of life years (DALYs) of per event was defined as the total DALYs from the WHO Global Burden of Disease (GBD) study15 divided by the prevalence from the CHS (Table S2). The annual costs of each CVD event were estimated from the China Health Statistics Yearbook.16 DALY averted from CVD events prevented by controlling hypertension was calculated by multiplying the number of prevented stroke/CHD events and the DALYs associated with each stroke/CHD event, respectively. The costs saved from CVD events prevented by controlling hypertension were calculated in the same manner: multiplying the number of prevented stroke/CHD events and the cost associated with each stroke/CHD event.
2.5. Statistical analysis
Statistical analyses were conducted with SAS version 9.4 (SAS Institute Inc) and Stata 12.1 (StataCorp.). To address the multilevel stratified sampling design, rates were calculated using PROC SURVEYFREQ; differences or trends across groups, including age, sex, and region (urban vs rural), were tested using PROC SURVEYLOGISTIC in SAS. Survey weights were calculated based on the 2010 China population census data and sampling scheme and included oversampling for specific age subgroups, nonresponse, and other demographic differences between the sample and the total population.17 Adjustment for different probabilities of selection and the complex sampling design was used to enhance the representativeness of the survey sample population. Variables were summarized using means with 95% confidence intervals (CI) for continuous data and frequencies, percentages, and proportions for categorical data. 95% CI for all parameters was estimated. P < 0.05 was the threshold for statistical significance.
3. RESULTS
3.1. Prevalence, treatment, and control of hypertension
The prevalence of hypertension was 32.0% (219.5 million) according to the Chinese 2018 guidelines. Another 24.5% of the population, representing an additional 168.1 million nationally, would be classified as hypertensive if the 2017 ACC/AHA guidelines were adopted. According to the 2017 ACC/AHA guidelines, the prevalence would be higher in men and people living in eastern areas and increased with age (all P < 0.001, Table 1). Table S3 shows the number of Chinese adults with hypertension according to the two sets of guidelines. Figure 1 shows that more than half (25.6% over 42.1%) of individuals with prehypertension based on Chinese guidelines would be reclassified as patients with stage 1 hypertension according to the ACC/AHA guidelines.
Table 1.
Prevalence of hypertension by characteristics according to the 2018 Chinese/2017 ACC/AHA guideline
| Characteristics | Prevalence | Awarenessa | Pharmaceutical treatmenta | Control | Control among treated hypertensive participants | |||
|---|---|---|---|---|---|---|---|---|
| 2018 Chinese | 2017 ACC/AHA | 2018 Chinese | 2018 Chinese | 2018 Chinese | 2017 ACC/AHA | 2018 Chinese | 2017 ACC/AHA | |
| Overall | 32.0 (30.2‐33.7) | 56.5 (54.2‐58.8) | 49.7 (46.1‐53.3) | 43.4 (39.9‐47.0) | 16.3 (14.0‐18.6) | 9.2 (7.8‐10.5) | 37.6 (35.0‐40.1) | 14.9 (13.4‐16.4) |
| Age | ||||||||
| 35‐44 | 15.0 (13.5‐16.4) | 41.7 (39.4‐43.9) | 31.7 (26.5‐37.0) | 24.5 (19.9‐29.1) | 9.9 (7.0‐12.7) | 3.5 (2.4‐4.6) | 40.3 (35.4‐45.3) | 14.0 (12.2‐15.8) |
| 45‐54 | 29.6 (27.6‐31.6) | 56.1 (53.5‐58.7) | 47.0 (42.9‐51.0) | 40.3 (36.2‐44.3) | 16.1 (13.7‐18.6) | 8.4 (7.1‐9.7) | 40.1 (37.4‐42.8) | 14.2 (12.6‐15.9) |
| 55‐64 | 44.6 (42.4‐46.9) | 67.2 (64.7‐69.7) | 53.9 (50.1‐57.7) | 48.1 (44.3‐51.9) | 18.6 (15.9‐21.2) | 12.2 (10.4‐14.1) | 38.6 (35.5‐41.6) | 16.0 (13.9‐18.1) |
| 65‐74 | 55.7 (53.5‐58.0) | 74.7 (72.4‐77.0) | 58.6 (55.6‐61.7) | 52.8 (49.6‐56.1) | 18.4 (16.2‐20.7) | 13.6 (11.9‐15.4) | 34.9 (32.2‐37.6) | 15.2 (13.2‐17.2) |
| ≥75 | 60.2 (57.7‐62.8) | 78.7 (77.1‐80.2) | 57.3 (53.9‐60.6) | 52.1 (48.4‐55.7) | 17.0 (14.7‐19.4) | 13.0 (11.2‐14.8) | 32.7 (29.9‐35.6) | 13.6 (11.8‐15.3) |
| P value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.092 |
| Sex | ||||||||
| Men | 32.8 (30.9‐34.7) | 61.1 (58.7‐63.4) | 46.1 (42.5‐49.8) | 39.1 (35.7‐42.6) | 14.5 (12.4‐16.7) | 7.8 (6.6‐8.9) | 37.2 (34.6‐39.8) | 14.0 (12.5‐15.4) |
| Women | 31.1 (29.3‐32.8) | 51.9 (49.5‐54.3) | 53.4 (49.7‐57.1) | 48.0 (44.2‐51.9) | 18.2 (15.7‐20.8) | 10.8 (9.2‐12.5) | 37.9 (35.2‐40.6) | 15.7 (14.0‐17.5) |
| P value | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.357 | 0.008 |
| Region | ||||||||
| Eastern | 34.4 (32.2‐36.5) | 60.4 (57.6‐63.1) | 51.9 (46.3‐57.5) | 46.5 (40.7‐52.4) | 18.8 (15.0‐22.6) | 10.6 (8.4‐12.8) | 40.3 (36.5‐44.1) | 16.0 (13.6‐18.4) |
| Middle | 29.9 (25.7‐34.2) | 52.0 (47.9‐56.1) | 53.0 (47.5‐58.6) | 45.4 (40.3‐50.5) | 17.8 (14.8‐20.8) | 10.1 (7.9‐12.4) | 39.2 (36.2‐42.1) | 16.0 (14.1‐18.0) |
| Western | 30.7 (27.6‐33.8) | 55.8 (52.3‐59.2) | 42.1 (37.0‐47.1) | 35.9 (30.8‐41.0) | 10.4 (7.9‐12.9) | 5.7 (4.4‐6.9) | 29.1 (24.9‐33.3) | 10.8 (8.0‐13.7) |
| P value | 0.073 | 0.001 | 0.011 | 0.013 | 0.001 | 0.001 | <0.001 | 0.009 |
| Urban/rural | ||||||||
| Urban | 31.8 (29.2‐34.4) | 55.9 (52.8‐59.0) | 53.9 (48.8‐59.0) | 48.7 (43.5‐53.8) | 20.7 (17.3‐24.0) | 11.7 (9.7‐13.7) | 42.5 (39.2‐45.7) | 16.9 (14.7‐19.0) |
| Rural | 32.0 (29.7‐34.4) | 56.8 (53.6‐60.0) | 47.4 (42.3‐52.5) | 40.6 (35.6‐45.7) | 14.0 (10.8‐17.1) | 7.8 (6.0‐9.7) | 34.4 (30.6‐38.3) | 13.6 (11.5‐15.8) |
| P value | 0.899 | 0.686 | 0.070 | 0.027 | 0.005 | 0.007 | 0.002 | 0.035 |
Data are presented as % (95% CI).
Awareness and pharmaceutical treatment based on the 2017 ACC/AHA guideline cannot be estimated in this study.
Figure 1.
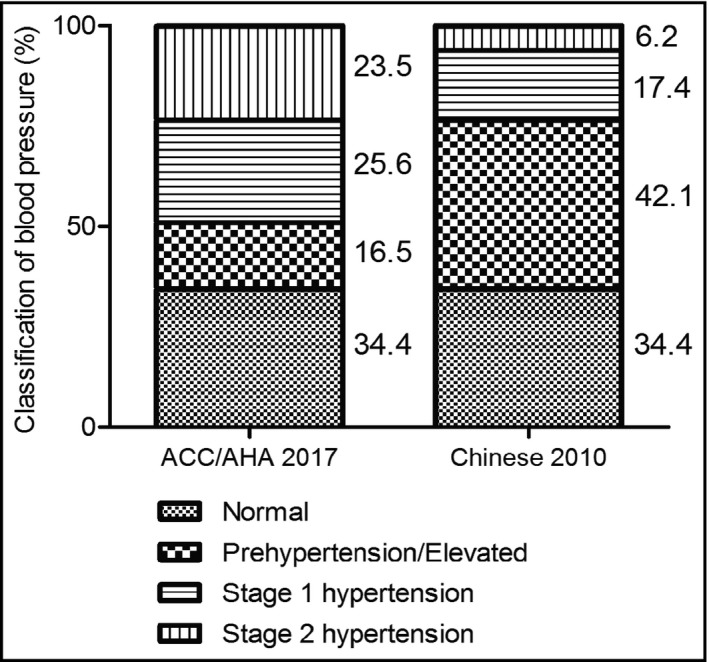
Classification of hypertension of Chinese adults according to the 2017 ACC/AHA guideline and Chinese 2018 guideline. Stage 2 and stage 3 were combined to stage 2 for the Chinese 2018 guideline
Accordingly, 22.7% (39.9 million) and 21.1% (34.0 million) patients with stage 1 and stage 2 hypertension, respectively, who did not require drug treatment according to the 2018 Chinese guideline, would be appropriate for pharmacological treatment if the 2017 ACC/AHA guidelines were applied in China. The proportions who would need to be treated were significantly higher in older and male patients (P < 0.001, Table 2). There were no significant differences among regions, or between urban and rural for patients requiring treatment who did not meet treatment goal (Table 2). The control rate would be significantly lower in the younger age group (P < 0.05), and only 14.9% (5.3 million) hypertensive patients taking antihypertensive medications had BP below 130/80 mm Hg (Table 1).
Table 2.
Hypertensive patients reclassified and recommended for treatment according to the 2017 ACC/AHA guideline
| Stage 1 hypertension | Stage 2 hypertension | Estimated number of hypertensive patients need to be pharmaceutically treated to reach the current treatment rate (43.4%) according to the 2018 Chinese guideline (mean, million) | |
|---|---|---|---|
| Untreated patients recommended for drug therapy (%) | Untreated patients recommended for drug therapy (%) | ||
| Overall | 22.7 (19.6‐25.8) | 21.1 (18.5‐23.6) | 32.1 (27.9‐36.2) |
| Age | |||
| 35‐44 | 6.0 (4.0‐7.9) | 8.8 (4.3‐13.4) | 3.2 (2.0‐4.3) |
| 45‐54 | 11.3 (9.1‐13.5) | 10.8 (8.9‐12.7) | 4.7 (4.1‐5.3) |
| 55‐64 | 40.1 (30‐50.1) | 16.3 (12.1‐20.5) | 8.9 (7.1‐10.5) |
| 65‐74 | 73.9 (60.3‐87.4) | 22.6 (16.7‐28.6) | 6.8 (5.7‐7.7) |
| ≥75a | 100.0 | 100.0 | 8.5 |
| P value | <0.001 | <0.001 | – |
| Sex | |||
| Men | 26.1 (21.5‐30.6) | 20.2 (18.0‐22.4) | 19.4 (17.8‐21.1) |
| Women | 18.4 (14.4‐22.3) | 22.2 (18.6‐25.8) | 12.7 (11.1‐14.3) |
| P value | 0.011 | 0.124 | – |
| Region | |||
| Eastern | 23.4 (16.2‐30.6) | 22.6 (19.4‐25.8) | 13.7 (11.3‐16.0) |
| Middle | 22.0 (18.6‐25.5) | 19.1 (12.7‐25.4) | 10.0 (8.3‐11.7) |
| Western | 22.5 (15.3‐29.7) | 21.2 (13.1‐29.4) | 8.3 (5.8‐10.7) |
| P value | 0.861 | 0.381 | – |
| Region | |||
| Urban | 21.0 (14.7‐27.3) | 21.5 (17.0‐25.9) | 10.1 (8.1‐12.1) |
| Rural | 23.5 (19.7‐27.3) | 20.9 (17.5‐24.3) | 21.9 (19.8‐24.1) |
| P value | 0.458 | 0.811 | – |
Data are presented as mean or percentage (95% CI). All values were weighted to represent the total population of Chinese aged 35 y or older based on the Chinese census 2010.
For those older than age 75, antihypertensive drugs are recommended for all hypertensive patients with systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥80 mm Hg.
3.2. The incremental cost of hypertension treatments, and averted DALY and cost on CVD events
Among the additional 168.1 million hypertensive patients, application of the ACC/AHA guidelines would yield approximately 32.1 million patients (19.1%) requiring pharmaceutical therapy to reach the current treatment rate of 43.4% in patients aged 35 years and older (Table 2), which would generate an additional cost of 1.7 billion US dollars for hypertensive medications in each fiscal year (Table 3). In total, if the 2017 ACC/AHA guidelines were adopted, an additional 3.6 billion US dollars direct medical costs would be required in each fiscal year, and 42.7 billion over a lifespan (Table 3).
Table 3.
The estimated increase in the cost of hypertension according to the 2017 ACC/AHA guideline (US dollar, million)
| Cost of antihypertensive drugs | Annual costsa of direct medical care of hypertensive patients | Lifetime costsb of direct medical care of hypertensive patients | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Monotherapy | SPC | Two‐drug combinations | Total | Urban | Rural | Total | Urban | Rural | Total | |
| Region | ||||||||||
| Eastern | 157.8 (130.1‐184.3) | 24.7 (20.3‐28.8) | 266.3 (219.7‐311.0) | 705.1 (581.6‐823.5) | 802.5 (726.0‐884.5) | 720.1 (651.4‐793.7) | 1522.6 (1377.4‐1678.3) | 9630.3 (8711.8‐10 614.6) | 8641.3 (7817.1‐9524.5) | 18 271.6 (16 529.0‐20 139.0) |
| Middle | 115.2 (95.6‐134.8) | 18.0 (14.9‐21.1) | 194.4 (161.3‐227.5) | 514.7 (427.2‐602.2) | 518.1 (540.1‐655.2) | 518.1 (471.6‐572.0) | 1111.4 (1011.7‐1227.2) | 6216.7 (6481.6‐7862.1) | 6216.7 (5659.1‐6864.5) | 13 336.9 (12 140.7‐14 726.7) |
| Western | 95.6 (66.8‐123.2) | 14.9 (10.4‐19.3) | 161.3 (112.8‐208.0) | 427.2 (298.5‐550.7) | 512.7 (314.1‐498.6) | 512.7 (392.9‐623.7) | 922.5 (707.0‐1122.3) | 6151.9 (3769.0‐5983.2) | 6151.9 (4714.9‐7484.7) | 11 069.7 (8483.9‐13 468.0) |
| Urban/rural | ||||||||||
| Urban | 116.3 (93.3‐139.4) | 18.2 (14.6‐21.8) | 196.3 (157.5‐235.2) | 519.8 (416.9‐622.8) | – | – | 1168.6 (937.2‐1400.0) | – | – | 14 023.3 (11 246.4‐16 800.2) |
| Rural | 252.2 (228.1‐277.6) | 39.4 (35.7‐43.4) | 425.7 (384.9‐468.5) | 1127.2 (1019.1‐1240.4) | – | – | 2387.9 (2158.9‐2627.8) | – | – | 28 654.9 (25 907.2‐31 533.5) |
| Total | 369.7 (321.3‐416.9) | 57.8 (50.2‐65.2) | 624.0 (542.4‐703.7) | 1652.1 (1436.0‐1863.2) | – | – | 3556.5 (3096.1‐4027.8) | – | – | 42 678.2 (37 153.6‐48 333.7) |
Data are presented as mean (95% CI).
Abbreviations: SPC, single‐pill combinations.
Annual costs associated with outpatient visits, diagnosis/tests, procedures, hospitalizations, and antihypertensive medications.
Lifetime costs of direct medical care = (life expectancy estimated by the World Bank [76 y] (Ref. 14) − age of hypertensive patients who recommended antihypertensive drugs but not receive drug treatment in our study [64 y]) × costs of direct medical care.
However, by adopting the 2017 ACC/AHA guidelines, the number of CVD events prevented annually is estimated to be 151 000 (95% CI: 131 130, 170 140) for stroke and 55 000 (95% CI: 47 430, 61 540) for CHD. Based on the estimated total DALYs due to CVD from the WHO Global Burden of Disease study and the prevalence of CVD in China, the total prevented DALYs is estimated to be 726 000 (95% CI: 444 531, 1 410 461) for stroke and 688 000 (95% CI: 438 253, 1 177 260) for CHD. Besides reducing disease burden in terms of DALYs, it is also estimated that the reduction in the disease burden of CVD events will result in annual saving of 313.2 (95% CI: 181.1, 575.9) million US dollars and lifetime saving of 3.76 (95% CI: 2.17, 6.91) billion US dollars by adopting the 2017 guidelines (Table 4, Table S2).
Table 4.
Averted DALY and cost on CVD events prevented by controlling hypertension according to 2017 ACC/AHA guideline
| Stroke | CHD | Totalg | |
|---|---|---|---|
| Number of prevented eventa | 151 000 (131 130, 170 140) | 55 000 (47 430, 61 540) | 206 000 (178 560, 231 680) |
| DALY per eventb | 4.82 (3.39, 8.29) | 12.60 (9.24, 19.13) | 6.72 (4.78, 11.20) |
| Averted DALYc | 726 000 (444 531, 1 410 461) | 688 000 (438 253, 1 177 260) | 1 414 000 (882 784, 2 587 721) |
| Annual cost per event (US dollar)d | 1178.1 (994.5, 1786.7) | 2485.4 (1069.0, 4418.7) | – |
| Reduced annual cost (US dollar, million)e | 177.6 (130.4, 304.0) | 135.6 (50.7, 271.9) | 313.2 (181.1, 575.9) |
| Reduced lifetime cost (US dollar, million)f | 2130.6 (1564.9, 3648.0) | 1627.5 (608.4, 3263.1) | 3758.2 (2173.3, 6911.1) |
Data are presented as mean (95% CI).
Abbreviations: CHD, coronary heart disease; DALY, disability adjusted of life year.
Suppose 4.7/1000 strokes and 1.7/1000 coronary heart disease events each year in hypertensive patients with pharmaceutical treatments could be prevented based on Felodipine Event Reduction study.2 The number of prevented event was calculated as patients with drug therapy multiplies 4.7/1000 for strokes or 1.7/1000 for CHD.
The DALYs was 44 947 064.55 for stroke, and 38 060 559.75 for CHD based on GDB (Ref. 15); the prevalence was 9 330 000 (5 420 000, 13 240 000) for stroke, and 3 020 000 (1 990 000, 4 120 000) for CHD from Table S2. So, DALY per event was 4.82 (3.39‐8.29) for stroke, 12.60 (9.24‐19.13) for CHD, and 6.72 (4.78‐11.20) for total.
Averted DALY = Number of prevented event × DALY per event.
Values were cited from China Health Statistics Yearbook, 2013 (Ref. 16).
Reduced annual cost = Annual cost per event × Number of prevented event.
Reduced lifetime cost = (life expectancy estimated by the World Bank [76 y] (Ref. 14) − age of hypertensive patients who recommended antihypertensive drugs but not receive drug treatment in our study [64 y]) × reduced annual costs.
The value of the Column of “Total” = the Column of “Stroke” + “CHD”.
The net annual cost was estimated at 3.43 billion US dollars, and 38.92 billion US dollars for a lifetime, respectively. The cost will be more than 27 500 US dollars per DALY averted.
4. DISCUSSION
The current study presents the potential impact if the 2017 ACC/AHA hypertension guidelines are adopted in China. This would lead to a substantial increase in the proportion of Chinese adults defined as having hypertension; the control rate would significantly lower with a target BP of 130/80 mm Hg. To reach currently the treatment rate, an additional lifetime direct medical care costs would be 42.7 billion US dollars for about 32.1 million hypertensive patients aged 35 years and older. However, about 206 000 CVD events (considering stroke and CHD only) would be prevented, resulting in 3.76 billion US dollars lifetime cost and 1.41 million DALYs being saved by controlling hypertension, while yielding net costs of 38.92 billion US dollars.
The lowering of the treatment target for hypertensive patients in the 2017 ACC/AHA was guided by evidence for a reduced rate of major adverse cardiovascular events,18 and the intensive systolic BP control among adults at high risk for cardiovascular disease has been shown to be cost‐effective, that is, below common US willingness‐to‐pay thresholds.19 However, even based on the current conservative guidelines,9 the appropriate management of high BP patients has been a huge challenge with high rates of non‐ and undertreatment in China.8
High BP remains a serious public health problem worldwide. A previous study has indicated a steady increase in prevalence across China over the past several decades,20 along with urbanization and aging of the population,6 suggesting that there are huge hypertension and related CVD burden. By combining the increased lifetime direct cost of treating hypertension, the reduced lifetime cost of prevented CVD events, and the averted DALY, the lower limit of cost will be more than 27 500 US dollars per DALY averted, which is more than three times GDP per capita (8 832 US dollars GDP per capita of China 2017), the maximal willingness‐to‐pay threshold recommended by the WHO. Therefore, it is likely that adoption of the 2017 guidelines would be above the current societal willingness‐to‐pay threshold. The benefit of cost reduction by preventing CVD is not likely to be judged sufficient to offset the costs incurred by antihypertensive treatments in a larger proportion of the population.21
It is necessary to be cautious that the beneficial effects of intensive systolic BP control have not been confirmed in European and Asian populations, including the Chinese population22; even in the United States, it has been suggested that intensive antihypertensive treatment in a broad population of older adults is lacking in evidence, and may result in low‐value care.23 A cohort study from China implied that participants aged 35‐59 years old with stage 1 hypertension defined by the 2017 guidelines were associated with higher CVD risk; however, the association was not shown among patients aged 60 years or older.24
In addition, the beneficial effects of intensive BP management also remain underexplored in younger populations (≤45 years).18, 25 While high BP has been shown to have significant economic consequences based on the current guidelines,26 the high initial cost will need to be accounted for when considering the adoption of the 2017 ACC/AHA guidelines in China. Thus, more evidence will be needed to identify the optimal BP cutoff, to permit the appropriate resources to be made available in developing countries, such as China.
The public health response to this challenge should drive the development of strategies suitable for developing countries. Lifestyle changes, such as increasing exercise and decreasing consumption of calorie‐dense and fat‐rich foods, salt, tobacco, and alcohol, will help prevent the development of advanced stages of hypertension.27 Therefore, population‐based interventions could be developed and implemented.28 In addition, strategies aimed at the use of less expensive antihypertensive medications and the use of combinations to improve treatment effectiveness and adherence should be pursued aggressively. Continuing hypertension education is urgently needed to ensure that physicians in general practice are aware of and adhere to national hypertension guidelines. Indeed, the feasibility and cost‐effectiveness of programs to increase adherence to antihypertensive treatment have been confirmed in developing countries.29 Such programs could also be applied in some specific geographical regions in China.
The current study has several strengths. The CHS provides nationally representative estimates for the general Chinese population aged ≥35 years, and the results of this analysis have broad generalizability. BP was measured three times following a standardized protocol. However, some limitations should be noted. BP was measured at a single visit in this study. First, due to lack of patient‐level data, instead of a formal cost‐effectiveness model, the cost‐effectiveness of adopting of the 2017 AHA/ACC was simulated based on the number of cardiovascular events avoided, and the unit cost and DALYs per event. Second, about 10% participants with missing data were excluded for analysis. From Table S1, we can see that excluded patients were older, and more often urban, although there was no difference in sex or BMI compared with the included participants. Third, due to no data on the number of CVD events prevented by controlling BP to ≤130/80 mm Hg among the Chinese population, we used the data from FEVER study (controlling BP to ≤140/90mm Hg),2, 3 so the averted DALY may be underestimated in the study.
5. CONCLUSIONS
We found that application of the 2017 AHA/ACC guidelines would substantially increase the prevalence of hypertension compared with the 2018 Chinese guidelines. To reach even the current treatment rate, considerable additional costs of therapy for hypertensive patients aged 35 years and older would be required, although this would be mitigated by the beneficial effects of events prevented and associated costs avoided. Thus, the challenges of bringing more intensive control of BP to the Chinese population are considerable. Additional studies and less expensive therapies for hypertension may make adoption of the new, intensive 2017 ACC/AHA guidelines feasible in the future.
CONFLICT OF INTEREST
None of the authors had any conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Zengwu Wang, Runlin Gao, Zuo Chen, Linfeng Zhang, and Xin Wang were involved in study design; Zengwu Wang, Zuo Chen, Linfeng Zhang, Xin Wang, and Guang Hao were involved in data collection. Guang Hao, Zengwu Wang, Zugui Zhang, and Hao Hu interpreted the analysis and wrote the manuscript. William S. Weintraub and Runlin Gao supervised the project. All authors contributed to revision and approved the final version of the submitted manuscript.
Supporting information
ACKNOWLEDGMENTS
We thank for all the colleagues involving in the survey (Appendix S2), and gratefully acknowledge Tianming Zhao, Guohui Fan, Jingyu Nie, and Linlin Jiang for help in maintaining the data. We are grateful to OMRON Corporation, Kyoto, Japan, for supporting the Blood Pressure Monitor (HBP‐1300) and body fat and weight measurement device (V‐body HBF‐371); Henan Huanan Medical Science & Technology Co., Ltd, China, for Digital ECG device (GY‐5000); and Microlife, Taipei, Taiwan, for Automated ABI device (Watch BP Office device). Finally, we are thankful to Buchang Pharma, Xian, China; Kinglian Technology, Guangzhou, China; Merck Serono; Pfizer China; and Essen Technology (Beijing) Company Limited for their support to fund the project.
Wang Z, Hao G, Wang X, et al; for the China hypertension survey investigators . Clinical outcomes and economic impact of the 2017 ACC/AHA guidelines on hypertension in China. J Clin Hypertens. 2019;21:1212–1220. 10.1111/jch.13609
Funding information
This work was supported by the Projects in the Chinese National Science & Technology Pillar Program during the Twelfth Five‐year Plan Period (No.: 2011BAI11B01), and the Chinese National Special Fund for Health‐Scientific Research in the Public Interest (No.: 201402002).
REFERENCES
- 1. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:2199‐2269.29146533 [Google Scholar]
- 2. Liu L, Zhang Y, Liu G, et al. The felodipine event reduction (fever) study: a randomized long‐term placebo‐controlled trial in chinese hypertensive patients. J Hypertens. 2005;23:2157‐2172. [DOI] [PubMed] [Google Scholar]
- 3. Zhang Y, Zhang X, Liu L, Zanchetti A, FEVER Study Group . Is a systolic blood pressure target <140 mmhg indicated in all hypertensives? Subgroup analyses of findings from the randomized fever trial. Eur Heart J. 2011;32:1500‐1508. [DOI] [PubMed] [Google Scholar]
- 4. Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in united states and china: Nationally representative cross sectional study. BMJ. 2018;362:k2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang X, Li J, Hu D, et al. Predicting the 10‐year risks of atherosclerotic cardiovascular disease in Chinese population: the China‐par project (prediction for ASCVD risk in china). Circulation. 2016;134:1430‐1440. [DOI] [PubMed] [Google Scholar]
- 6. Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987‐2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. GBD Mortality Collaborators . Global, regional, and national under‐5 mortality, adult mortality, age‐specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1084‐1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344‐2356. [DOI] [PubMed] [Google Scholar]
- 9. Writing Group of Chinese Guidelines for the Management of Hypertension . [2018 Chinese guidelines for the management of hypertension]. Prev Treat Cardio Cereb Vasc Dis. 2019;19:579‐615. [Google Scholar]
- 10. O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612‐623. [DOI] [PubMed] [Google Scholar]
- 11. Dong Y, Wang Z, Chen Z, et al. Comparison of visceral, body fat indices and anthropometric measures in relation to chronic kidney disease among Chinese adults from a large scale cross‐sectional study. BMC Nephrol. 2018;19:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feng R, Wang Z, Wang X. [Study on the economic affordability of common antihypertensive monolithic preparations in community]. J Health Econ Res. 2014; 330:91‐93. [Google Scholar]
- 13. Luo A, Feng R, Wang Z. [Economic affordability of antihypertensive drugs in community standardized management]. J Hosp Pharm. 2014;34:1951‐1954. [Google Scholar]
- 14. The World Bank . Health expenditure. https://data.Worldbank.Org/indicator/sp.Dyn.Le00.In. Accessed Augusta 16, 2018.
- 15. GBD Disease Injury Incidence Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211‐1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Health and Family Planning Commission of the People's Republic of China . China Health Statistics Yearbook, 2013. Beijing, China: Peking Union Medical College Press; 2014. [Google Scholar]
- 17. Census Office of the State Council of China , Division of Population and Employment Statistics , National Bureau of Statistics of China . Tabulation on the 2010 Population Census on the People's Republic of China. Beijing, China: China Statistics Press; 2012. [Google Scholar]
- 18. Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta‐analysis. JAMA Cardiol. 2017;2:775‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Richman IB, Fairley M, Jorgensen ME, Schuler A, Owens DK, Goldhaber‐Fiebert JD. Cost‐effectiveness of intensive blood pressure management. JAMA Cardiol. 2016;1:872‐879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bundy JD, He J. Hypertension and related cardiovascular disease burden in china. Ann Glob Health. 2016;82:227‐233. [DOI] [PubMed] [Google Scholar]
- 21. Vaucher J, Marques‐Vidal P, Waeber G, Vollenweider P. Population impact of the 2017 ACC/AHA guidelines compared with the 2013 ESH/ESC guidelines for hypertension management. Eur J Prev Cardiol. 2018;25:1111‐1113. [DOI] [PubMed] [Google Scholar]
- 22. Habib GB, Virani SS, Jneid H. Is 2015 the primetime year for prehypertension? Prehypertension: a cardiovascular risk factor or simply a risk marker? J Am Heart Assoc. 2015;4:e001792. 10.1161/JAHA.1115.001792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilt TJ, Kansagara D, Qaseem A. Clinical Guidelines Committee of the American College of Physicians. Hypertension limbo: balancing benefits, harms, and patient preferences before we lower the bar on blood pressure. Ann Intern Med. 2018;168:369‐370. [DOI] [PubMed] [Google Scholar]
- 24. Qi Y, Han X, Zhao D, et al. Long‐term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline. J Am Coll Cardiol. 2018;72:1201‐1210. [DOI] [PubMed] [Google Scholar]
- 25. Wei Y, Jin Z, Shen G, et al. Effects of intensive antihypertensive treatment on Chinese hypertensive patients older than 70 years. J Clin Hypertens (Greenwich). 2013;15:420‐427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang D, Wang G, Joo H. A systematic review of economic evidence on community hypertension interventions. Am J Prev Med. 2017;53:S121‐S130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mittal BV, Singh AK. Hypertension in the developing world: challenges and opportunities. Am J Kidney Dis. 2010;55:590‐598. [DOI] [PubMed] [Google Scholar]
- 28. Murray CJ, Lauer JA, Hutubessy RC, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular‐disease risk. Lancet. 2003;361:717‐725. [DOI] [PubMed] [Google Scholar]
- 29. Neupane D, McLachlan CS, Mishra SR, et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open‐label, cluster‐randomised trial. Lancet Glob Health. 2018;6:e66‐e73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


