To the Editor,
Resting pulse wave velocity (PWV), central blood pressure (BP), and central augmentation index (cAIx) are established arterial health parameters, and add to the traditional brachial BP measurement predictive value for cardiovascular risk estimation.1, 2, 3 In this sense, new devices jointly evaluate the 24‐hour central BP, PWV, and cAix, and available data suggest improvement of this combined approach in the estimation of cardiovascular remodeling in several clinical scenarios.4, 5, 6, 7 However, little is known regarding the correlation between office and out‐of‐office measures of central BP, PWV, and cAIx. We compared the values of office and 24‐hour ambulatory central BP, PWV, cAIx, and brachial BP measures and assessed the correlation between office and respective ambulatory measures in individuals untreated or treated with BP‐lowering medications.
This cross‐sectional study prospectively evaluated 697 individuals (450 untreated and 247 treated with BP‐lowering medications) aged >18 years from the Clinical Research Center of the Cesmac University Center from 2014 to 2016. All office and ambulatory measures of brachial BP, central BP, PWV, and cAIx were performed with the Mobil‐O‐Graph PWA monitor (IEM Healthcare, Stolberg, Germany), as previously reported.5, 7 Office measures comprised one reading taken in the office after 5 minutes of rest in the sitting position. Ambulatory measures comprised 24‐hour readings taken at 30‐minutes intervals. Only individuals with at least 16 valid daytime and eight valid nighttime readings were included in the analysis. The Ethics committee of the Pedro Ernesto University Hospital approved the study protocol, which conforms to the principles of the declaration of Helsinki. Written informed consent was obtained from all participants. Descriptive data are presented as mean ± SD. Comparisons between office and respective ambulatory (24‐hour, daytime and nighttime) measures were performed using 1‐way ANOVA followed by Dunnett's test. Bivariate correlations between office measures and respective ambulatory measures were assessed using Pearson's correlation coefficient. P‐values < 0.05 were considered significant.
Participants not using BP‐lowering medications were 51% males and had average age = 44.7 ± 15.5 years and body mass index = 27.4 ± 4.1 kg/m2, while participants treated with BP‐lowering medications were 45% males and had average age = 51.5 ± 14.3 years and body mass index = 27.9 ± 4.5 kg/m2. Compared to office measures, all 24‐hour, daytime and nighttime central BP, PWV, cAIx, and brachial BP measures were significantly lower in both treated and untreated participants, except for daytime PWV and cAIx measures (Table 1).
Table 1.
Office and ambulatory values of studied measures and correlation coefficients between office and respective ambulatory measures in individuals treated and untreated with BP‐lowering medications
| Variable | Untreated with BP‐lowering medications (n = 457) | Treated with BP‐lowering medications (n = 240) | ||||||
|---|---|---|---|---|---|---|---|---|
| Office | 24 h | Daytime | Nighttime | Office | 24 h | Daytime | Nighttime | |
| Mean ± SD | ||||||||
| Brachial SBP, mm Hg | 132.1 ± 17.2 | 120.8 ± 11.1c | 123.8 ± 11.2c | 115.6 ± 12.5c | 136.9 ± 18.4 | 123.7 ± 12.2c | 126.2 ± 12.6c | 119.6 ± 13.6c |
| Brachial DBP, mm Hg | 86.6 ± 12.8 | 77.0 ± 9.2c | 80.1 ± 9.8c | 71.8 ± 9.8c | 90.5 ± 14.4 | 78.9 ± 10.5c | 81.5 ± 11.0c | 74.5 ± 11.1c |
| Central SBP, mm Hg | 122.1 ± 16.1 | 112.6 ± 10.4c | 114.7 ± 10.6c | 109.0 ± 11.9c | 127.5 ± 17.4 | 115.6 ± 11.5c | 117.2 ± 12.0c | 113.1 ± 13.2c |
| Central DBP, mm Hg | 88.0 ± 13.4 | 78.4 ± 9.6c | 81.9 ± 10.4c | 72.9 ± 10.2c | 92.2 ± 14.5 | 80.5 ± 10.9c | 83.4 ± 11.4c | 75.6 ± 12.1c |
| cAIx, % | 25.8 ± 11.6 | 23.4 ± 8.7b | 24.7 ± 8.5 | 21.3 ± 11.1c | 28.5 ± 11.2 | 25.9 ± 8.6a | 26.4 ± 8.0 | 25.0 ± 11.4c |
| PWV, m/s | 7.20 ± 1.90 | 6.86 ± 1.79a | 6.94 ± 1.77 | 6.72 ± 1.84c | 8.01 ± 1.91 | 7.60 ± 1.76a | 7.66 ± 1.74 | 7.49 ± 1.80b |
| Correlation coefficients | ||||||||
| Brachial SBP, mm Hg | — | 0.61c | 0.59c | 0.55c | — | 0.62c | 0.63c | 0.51c |
| Brachial DBP, mm Hg | — | 0.71c | 0.71c | 0.60c | — | 0.73c | 0.73c | 0.63c |
| Central SBP, mm Hg | — | 0.61c | 0.61c | 0.53c | — | 0.60c | 0.63c | 0.45c |
| Central DBP, mm Hg | — | 0.64c | 0.65c | 0.54c | — | 0.75c | 0.76c | 0.63c |
| cAIx, % | — | 0.53c | 0.57c | 0.37c | — | 0.56c | 0.62c | 0.40c |
| PWV, m/s | — | 0.97c | 0.97c | 0.96c | — | 0.97c | 0.97c | 0.95c |
BP, blood pressure; cAIx, central augmentation index; DBP, diastolic blood pressure; PWV, pulse wave velocity; SBP, systolic blood pressure; SD, standard deviation.
P < 0.05;
P < 0.01;
P < 0.001 compared with respective office measures in untreated or treated individuals.
Office and ambulatory central systolic BP measures showed correlation coefficients ranging from 0.45 to 0.63, while stronger correlations (r = 0.54‐0.76) were observed between office and ambulatory central diastolic BP measures in the two studied populations. Analogous results were obtained for brachial BP measures (Table 1). Correlation coefficients between office and ambulatory cAIx ranged from 0.37 to 0.62, while office and ambulatory PWV measures showed correlation coefficients ranging from 0.95 to 0.97 (Table 1 and Figure 1).
Figure 1.
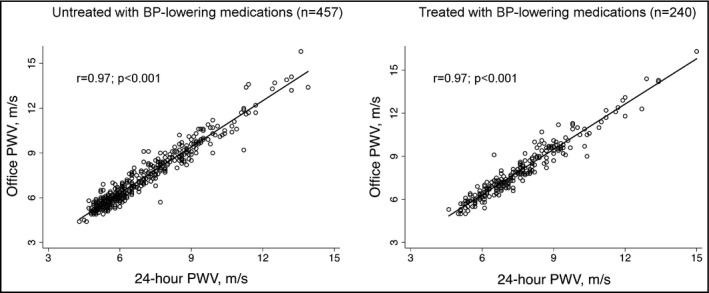
Correlation between office and 24‐h PWV in individuals treated and untreated with BP‐lowering medications. BP, blood pressure; PWV, pulse wave velocity
The present results show that ambulatory measures of PWV and cAIx are lower than respective office measures, independently of anti‐hypertensive medications use. Similar results were found for central and brachial BP, which are in agreement with previous data.4, 8 We also found a moderate correlation between office and ambulatory central BP measures, even though diastolic BP measures tended to have stronger relationship than systolic BP ones. In addition, while office and ambulatory cAIx measures had only weak to moderate correlation, office and ambulatory PWV measures had a very strong relationship. These findings suggest that office and ambulatory measures of PWV, but not of central BP and cAIx, might have similar clinical meaning regardless of BP‐lowering medication use.
CONFLICT OF INTEREST
None.
REFERENCES
- 1. Vlachopoulos C, Aznaouridis K, O'Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all‐cause mortality with arterial stiffness: a systematic review and meta‐analysis. Eur Heart J. 2010;31:1865‐1871. [DOI] [PubMed] [Google Scholar]
- 2. McEniery CM, Cockcroft JR, Roman MJ, Franklin SS, Wilkinson IB. Central blood pressure: current evidence and clinical importance. Eur Heart J. 2014;35:1719‐1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ben‐Shlomo Y, Spears M, Boustred C, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta‐analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63:636‐646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Omboni S, Posokhov IN, Kotovskaya YV, Protogerou AD, Blacher J. Twenty‐four‐hour ambulatory pulse wave analysis in hypertension management: current evidence and perspectives. Curr Hypertens Rep. 2016;18:72. [DOI] [PubMed] [Google Scholar]
- 5. Protogerou AD, Argyris AA, Papaioannou TG, et al. Left‐ventricular hypertrophy is associated better with 24‐h aortic pressure than 24‐h brachial pressure in hypertensive patients: the SAFAR study. J Hypertens. 2014;32:1805‐1814. [DOI] [PubMed] [Google Scholar]
- 6. Aissopou EK, Argyris AA, Nasothimiou EG, et al. Ambulatory aortic stiffness is associated with narrow retinal arteriolar caliber in hypertensives: the SAFAR study. Am J Hypertens. 2016;29:626‐633. [DOI] [PubMed] [Google Scholar]
- 7. Scheppach JB, Raff U, Toncar S, et al. Blood pressure pattern and target organ damage in patients with chronic kidney disease. Hypertension. 2018;72:929‐936. [DOI] [PubMed] [Google Scholar]
- 8. Jankowski P, Bednarek A, Olszanecka A, Windak A, Kawecka‐Jaszcz K, Czarnecka D. Twenty‐four‐hour profile of central blood pressure and central‐to‐peripheral systolic pressure amplification. Am J Hypertens. 2013;26:27‐33. [DOI] [PubMed] [Google Scholar]


