Abstract
Approximately 365 million people in Asia were classified as elderly in 2017. This number is rising and expected to reach approximately 520 million by 2030. The risk of hypertension and cognitive impairment/dementia increases with age. Recent data also show that the prevalence of hypertension and age‐related dementia are rising in Asian countries. Moreover, not many people in Asian countries are aware of the relationship between hypertension and cognitive impairment/dementia. Furthermore, hypertension control is poorer in Asia than in developed countries. Hypertension is known to be a major risk factor for damage to target organs, including the brain. Decreased cognitive function can indicate the presence of target organ damage in the brain. Twenty‐four‐hour blood pressure profiles and blood pressure variability have been associated with cognitive impairment and/or silent cerebral diseases, such as silent cerebral infarction or white matter lesions, which are predisposing conditions for cognitive impairment and dementia. Hypertension that occurs in midlife also affects the incidence of cognitive impairments in later life. Managing and controlling blood pressure could preserve cognitive functions, such as by reducing the risk of vascular dementia and by reducing the global burden of stroke, which also affects cognitive function.
Keywords: Asia, cognitive dysfunction, dementia, hypertension
1. INTRODUCTION
Life expectancy continues to increase globally, resulting in an increasingly elderly population.1, 2 Asia, continent that has world's biggest population (60%), is experiencing a very rapid increase in population aging, compared to Western countries.3 Approximately 365 million people were over 60 years in Asia and classified as elderly in 2017.4 This number is expected to reach approximately 520 million by 2030, with Japan having the largest percentage of elderly, estimated at around 37.3%.4, 5 And although such an increase in longevity should ideally be accompanied by improved quality of life, the incidence of dementia and other cognitive impairment also tend to increase with age.6, 7, 8 World Alzheimer Report in 2015 also showed that Asia has the highest number of people suffered from dementia, 22.9 million, compared to Europe region (10.5 million) and America region (9.4 million).6 Not surprisingly, therefore, data presented by Alzheimer's Disease International predict an increase in dementia in Asia. For example, in 2015, 1 million Indonesians are expected to be affected by dementia, and this number will increase to almost 2 million people by 2030 and nearly 4 million people by 2050. Similarly, in Japan around 3 million people had dementia in 2015, and this number will increase to 4.5 million in 2030 and 5.2 million in 2030.9 In addition, death from Alzheimer's dementia increased from 3.6 to 9.8 cases per 100 000 people between 2007 and 2017 based on the Annual Report on the Cause of Death Statistics in Korea.10
There are important ethnic differences in cardiovascular‐renal demographics around the world, and hypertension is one of the most powerful risk factors contributing to these demographic differences. For example, it has been well established that Asians display characteristics that differ markedly from those of whites and blacks.11, 12
The risk of hypertension increases with age. Data also show that the prevalence of hypertension continues to rise in Asian countries.13 Many studies have shown that hypertension increases the risk of cognitive disorders, Alzheimer's dementia, and vascular dementia.14 Data from the INTERSTROKE study show that hypertension is significantly associated with stroke incidence.15 The data show that hypertension is one of the risk factors that together account for 90.7% of the population‐attributable risk (PAR) of stroke worldwide and 97.4% of that in South‐East Asia.
The risk of dementia increases 6‐fold at 5 years after a stroke event. Moreover, the risk of dementia increases as early as 5 years before and continues more than 11 years after a stroke event, with the highest risk occurring within 1 year after the stroke event.16, 17 Stroke affects the hippocampus and white matter of the brain, thereby contributing to the pathogenesis of post‐stroke cognitive impairment.18 Reducing the incidence of stroke will thus reduce the incidence of vascular dementia.14
Age‐related dementia, which is mostly caused by Alzheimer's disease or cerebrovascular factors (vascular dementia), is a significant public health threat.19 Previous studies and current research in Asian countries show different trends, such as differences in the ratio of the incidence of Alzheimer's disease and vascular dementia, suggesting that there are trends—particularly trends related to hypertension—that will require further discussion and investigation.7, 20 In addition, not many people in Asian countries are aware of the relationship between hypertension and cognitive impairment/dementia.21, 22
2. TRENDS OF COGNITIVE IMPAIRMENT AND DEMENTIA IN ASIA
The prevalence of dementia in Asian countries varies from 2% to 13%, with the greatest risk factors being age, female sex, and low education.20, 23 The high epidemiological variation in Asian countries may be attributable to the different diagnostic criteria used. Also, differences in the level of education of respondents can also influence the results, accounting for as much as a twofold difference.6, 20, 23 Moreover, the number of dementia and cerebrovascular disease in Asia is higher than the number in Western countries.24
The differences in the trends of vascular dementia and Alzheimer's disease are especially apparent when comparing studies conducted before 1990, when the vascular ratio of dementia to Alzheimer's disease was 2:1 in Japan and China, while the reverse ratio was observed in Northern Europe and America. However, since 1990, this trend has changed as the prevalence of Alzheimer's disease has increased in East Asian countries. In Korea, for example, the ratio of Alzheimer's disease to vascular dementia increased to 4.13 in the 2010s from 1.96 in the early 1990s.25 One of the things that may underlie this trend is changes in lifestyle, such as diet, knowledge of the disease, risk management of vascular disease, and use of imaging such as CT scans.20, 21 Studies in Japan show a higher prevalence of vascular dementia compared to studies in China, which have not used CT scans.20, 26, 27
3. TRENDS AND EFFECTS OF HYPERTENSION ON COGNITIVE FUNCTION
Epidemiological data in several Asian countries reveal that hypertension is among the top three chronic diseases and contributes to both elderly morbidity and mortality.28, 29, 30, 31 Studies in India, China, and other Asian countries have also shown that smaller proportions of the population are aware of hypertension and have well‐controlled hypertension compared to the corresponding percentages in developed countries.32, 33, 34
A systematic analysis based on reports from 90 countries comparing data between 2000 and 2010 revealed that both absolute hypertension and the greatest increase in hypertension were observed in East Asia and the Pacific region. An increasing trend in systolic blood pressure for both sexes was also found in the regions of South Asia and South‐East Asia.35
In relation to race, a study conducted by Du et al36 on the prevalence of age‐adjusted hypertension among Asians living in America found that Filipinos showed the highest prevalence rate (32.7%), while Chinese showed the lowest (20%). In Indonesia, the latest data from the Basic Health Research survey show an increase in prevalence from 25.8% in 2013 to 34.1% in 2018.30, 37 Similar data were found in the May Measurement Month (MMM) study in 2017, which is the most massive screening performed in Indonesia to date; the hypertension prevalence in that survey was found to be 34.5%.38
Hypertension is known to be a major risk factor for damage to target organs, including the brain.15, 39, 40, 41, 42, 43, 44, 45 Damage to cerebral blood vessels is one of the effects of hypertension. Decreased cognitive function can indicate the presence of target organ damage in the brain, one form of which can be lesions in the white matter.46, 47 The hypertension‐induced damage can also include changes to cerebrovascular structural and function, which in turn can cause the neuropathological abnormalities responsible for cognitive deficits, such as micro‐infarcts, microbleeds, silent brain infarcts, and brain atrophy.39, 48 Other structural damages to the brain caused by arterial hypertension include remodeling of the cerebral artery, myogenic reactivity, hypertrophy, and endothelial dysfunction, which cause altered cerebral blood flow (CBF) autoregulation, blood‐brain barrier disruption, and cerebrovascular regulatory mechanism impairment.39, 49, 50, 51 In addition, clinical manifestation of reduced cognitive function can appear as learning difficulties, lack of focus, gait disorder, and depression.49, 52
Progressive decrease in BP in the early stages of dementia is likely caused directly by a neurodegenerative process that affects the brain stem and hypothalamic nucleus which regulates arterial pressure and systemic metabolism.19, 53 Godin et al conducted the 3C study in 9294 subjects with an average age of 72.4 ± 4.1 years and analyzed the association between blood pressure and anti‐hypertensive treatment in relation to white matter lesions (WML) from the Dijon MRI data. The initiation of anti‐hypertensive treatment significantly affected the course of WML evolution only in subjects with a base level of systolic blood pressure higher than 160 mm Hg (n = 113); an approximately 85% greater decrease in average WML volume was observed in subjects who started anti‐hypertensive treatment compared to those who did not.54
4. BLOOD PRESSURE VARIABILITY AND COGNITIVE IMPAIRMENT
The term blood pressure variability (BPV) encompasses a wide range of BP variations, occurring over seconds or minutes (very short term BPV), along 24 hours (short term BPV, usually assessed by ambulatory BP monitoring), and between days (midterm or day to day BPV, assessed with home BP monitoring). Long‐term BPV has also been described, including seasonal BP variations and changes between clinic visits over months or years.55
Observational studies in elderly subjects ≥60 years of age in Japan, all of whom lacked dementia at enrollment and were followed for 5 years (2007‐2012), showed that daily increase in blood pressure variability led to the development of dementia in the form of either vascular dementia or Alzheimer's disease.56 Twenty‐four‐hour blood pressure profiles and blood pressure variability have been shown to be associated with cognitive function and/or silent cerebral diseases, such as silent cerebral infarction or white matter lesions, which are predisposing conditions for cognitive dysfunction (Figure 1).54, 57, 58, 59, 60, 61 A previous study by Kario et al62 showed a relationship between diurnal blood pressure variations and silent cerebrovascular damage, marked by findings of lacunae and advanced periventricular hyperintense lesions on magnetic resonance imaging (MRI) in asymptomatic hypertensive elderly. This silent cerebrovascular damage happens not only to nondippers, but also to extreme dippers (with marked nocturnal fall of blood pressure).
Figure 1.
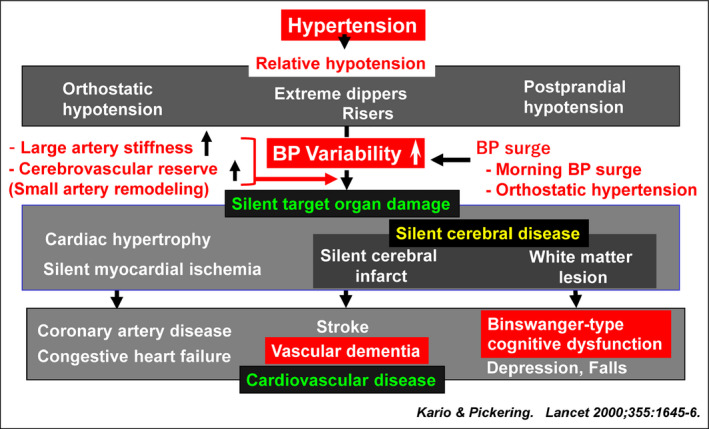
Clinical significance of blood pressure variability in elderly people with hypertension
Recently, studies on elderly with high risk of cardiovascular disease showed that exaggerated visit‐to‐visit BP fluctuations were associated with silent cerebral injury, stroke, and advanced carotid artery remodeling, which lead to cognitive impairment.60, 61 Absolute ambulatory systolic blood pressure level (particularly during sleep) and nocturnal dipping in systolic blood pressure were strong indicators of brain matter volume and cognitive function.63 In addition, an abnormal circadian blood pressure rhythm, especially the riser pattern, was shown to be clinically significant as a potential indicator of subclinical brain damage and mild cognitive impairment in heart failure patients.64 Therefore, measuring blood pressure variability by ambulatory monitoring could be considered as one way to detect patients who are at high risk of developing ischemic target organ damage.59
5. MIDLIFE HYPERTENSION AND COGNITIVE IMPAIRMENT
Studies in Asia have shown that hypertension is associated with incidence of dementia in the elderly.65, 66, 67, 68, 69 Indeed, not only is hypertension directly related to cognitive function, but hypertension that occurs in midlife (around the age of 45‐55 years) also affects the incidence of cognitive impairments in later life.46, 70, 71 An analysis conducted in conjunction with the Hisayama study, a prospective cohort study in Japan performed over 32 years (1973‐2005), was designed to compare blood pressure in midlife and late life, and to compare these data with dementia output and its subtypes. The results showed that high systolic and diastolic blood pressure in midlife increased the risk of vascular dementia (24% for each 10 mm Hg increase in systolic blood pressure and 37% for each 10 mm Hg increase in diastolic blood pressure).71 The Coronary Artery Risk Development in Young Adults study (CARDIA) showed that higher SBP from as young as 25 years of age to middle age was associated with worse cognitive functions, including verbal memory and executive function.39, 72 In addition, other studies have shown a significant association between elevated blood pressure levels in midlife and dementia in later life.73, 74
Although an increase in late‐life blood pressure increases the risk of all cases of dementia, including vascular dementia, the risk is greater for those whose blood pressure was increased in midlife, regardless of blood pressure in late life.71 Similar studies conducted in Korea show that hypertension is associated with all types of dementia, but especially with vascular dementia. Hypertension in men under 65 years is associated with Alzheimer's disease, which is distinct from the association between hypertension and vascular dementia, which is strong both before and after 65 years of age, and both for men and for women.75 As to the potential mechanism, it was suggested that chronic hypertension disrupts the blood vessels and impairs the cerebrovascular regulation, which makes the brain, especially the white matter regions that play roles in cognitive function, susceptible to ischemic injury.39
6. BLOOD PRESSURE CONTROL, ANTI‐HYPERTENSION AGENTS, AND COGNITIVE FUNCTION
The increased incidence of hypertension, especially in Asian populations, and its association with cognitive impairment in old age, suggests that managing and controlling blood pressure would be a potential means of preserving cognitive function, including by reducing the risk of vascular dementia and by reducing the global burden of stroke, which also affects cognitive function.15, 70, 75, 76 However, aggressive reductions in blood pressure must be carried out carefully in the elderly. In fact, recent findings have revealed that blood pressure‐lowering treatment in young adults might eliminate the progression of the detrimental effects related to arterial stiffness, indicating that younger adults may have more favorable outcomes in cognition than their older counterparts if early intervention is conducted at the subclinical stage.77 Although there was no impact on risk reduction of probable dementia, a recent trial (SPRINT MIND) showed that among ambulatory adults with hypertension who were treated with a goal of SBP <120 mm Hg, the risk of mild cognitive impairment was significantly reduced, compared to that in those treated with an SBP goal of <140 mm Hg (14.6 vs 18.3 cases per 1000 person‐years; HR, 0.81; 95% CI, 0.69‐0.95).78 A recent review of early morning BP surge (EMBS) showed that EMBS was one form of BP variability associated with the occurrence of strokes and other cardiovascular events. The study also concluded that 24‐hour‐long‐acting anti‐hypertensives, such as amlodipine and telmisartan, could control EMBS more effectively than valsartan.57 Moreover, strict BP control including during sleep may have a neuroprotective effect on the brain, and thereby prevent the incidence of dementia, and vice versa: As an independent marker associated with increased risk of CVD events, cognitive function should always be evaluated in elderly hypertensive patients.79, 80
A meta‐analysis comparing four randomized controlled trials—Syst‐Eur, Progress, HYVET‐COG, and SHEP—showed that anti‐hypertensive medication could significantly reduce the risk of dementia.81 Both calcium channel blockers (CCBs) and angiotensin receptor blockers (ARBs) are suggested to have a more pronounced protective effect than other anti‐hypertensives.82, 83, 84 In addition, the Syst‐Eur trial also showed that anti‐hypertensive medications can reduce stroke morbidity and mortality, and respondents may not be affected by dementia until at least 60 years of age. In that study, a calcium channel blocker (CCB) was used and had a protective effect against dementia, especially Alzheimer's.85 Another similar study in Kentucky showed that CCBs could reduce dementia progression and minimize amyloid beta peptide formation without changes to cell viability.82 And in a study conducted on the predominantly male population of the Veterans Healthcare System in the United States, angiotensin receptor blockers achieved a significant reduction in the incidence and progression of AD and dementia compared to other cardiovascular drugs, including angiotensin converting enzyme inhibitors.83
A cohort study in China showed similar results—namely although no significant difference in cognitive decline was found between hypertensive subjects who were taking anti‐hypertensive medications and subjects without hypertension, greater cognitive decline was seen in the group with untreated hypertension than the group without hypertension.86 Recent studies also support the idea that the detection of hypertension, and the reduction and control of blood pressure are protective measures against later‐life cognitive decline.87 However, other studies have reported that anti‐hypertensive therapy does not reduce the incidence of dementia.88 Given the continued uncertainty regarding the protective effects of anti‐hypertensive therapy on patients with cognitive dysfunction or dementia, further research is needed.89
7. CONCLUSIONS
The prevalence of dementia in Asia is expected to increase in the future in accordance with global aging. It has been well established that hypertension is a major risk factor for damage to various target organs, including the brain. Managing and controlling hypertension and blood pressure variability could preserve cognitive functions, such as by reducing the risk of vascular dementia and reducing the global burden of stroke, which also affects cognitive function. The detection of hypertension, and the reduction and control of blood pressure are protective measures against later‐life cognitive decline.
AUTHOR CONTRIBUTIONS
The contributions of the individual authors are summarized below: Turana Y and Tengkawan J drafted the manuscript. Chia YC, Hoshide S, Shin J, Chen CH, Buranakitjaroen P, Nailes J, Park S, Siddique S, Sison J, Soenarta AA, Tay JC, Sogunuru GP, Zhang Y, Wang JG, and Kario K involved in critical revision for important intellectual content. Turana Y, Tengkawan J, Chia YC, Hoshide S, Shin J, Chen CH, Buranakitjaroen P, Nailes J, Park S, Siddique S, Sison J, Soenarta AA, Tay JC, Sogunuru GP, Zhang Y, Wang JG, and Kario K involved in final approval of the submitted manuscript.
DISCLOSURES
K Kario received research grants from Teijin Pharma, Omron Healthcare, Fukuda Denshi, Bayer Yakuhin, A&D, Daiichi Sankyo, Mochida Pharmaceutical, EA Pharma, Boehringer Ingelheim Japan, Tanabe Mitsubishi Pharma, Shionogi & Co., MSD KK, Sanwa Kagaku Kenkyusho, Bristol‐Myers Squibb KK, Pfizer Japan, and Otsuka Holdings, and honoraria from Takeda Pharmaceutical, Daiichi Sankyo, Omron Healthcare, and Terumo Corporation. S Park has received research grants and honoraria from Pfizer. S Siddique has received honoraria from Bayer, GlaxoSmithKline, Pfizer, ICI, and Servier; and travel, accommodation and conference registration support from Atco Pharmaceutical, Highnoon Laboratories, Horizon Pharma, ICI, and Pfizer. YC Chia has received honoraria and sponsorship to attend conferences and CME seminars from Abbott, Bayer, Boehringer Ingelheim, GlaxoSmithKline, Menarini, Merck Sharp & Dohme, Novartis, Orient Europharma, Pfizer, and Sanofi; and a research grant from Pfizer. J Shin has received honoraria and sponsorship to attend seminars from Daiichi Sankyo, Takeda, Menarini, MSD, Bristol‐Myers Squibb, and Sanofi. CH Chen has received honoraria as a member of a speaker's bureau for Pfizer. R Divinagracia has received honoraria as a member of speaker's bureaus for Bayer, Novartis, and Pfizer. J Sison has received honoraria from Pfizer, AstraZeneca, Boehringer Ingelheim, and Novartis. GP Sogunuru has received a research grant related to hypertension monitoring and treatment from Pfizer. JC Tay has received advisory board and consultant honoraria from Pfizer. JG Wang has received research grants from Bayer, Pfizer, and Phillips; and lecture and consulting fees from Bayer, Daiichi Sankyo, Merck Sharp & Dohme, Pfizer, Sanofi, and Servier. L Wong has received honoraria from Bristol‐Myers Squibb and Pfizer. Y Zhang has received research grants from Bayer, Novartis, and Shuanghe; and lecture fees from Bayer, Daiichi Sankyo, Novartis, Pfizer, Sanofi, Servier, and Takeda. All other authors report no potential conflicts of interest in relation to this article.
ACKNOWLEDGMENTS
Editing assistance was provided by Pfizer Inc. The meetings held between the authors to discuss and prepare this manuscript were funded by unrestricted educational grants from Pfizer and Omron Healthcare Co., Ltd.
Turana Y, Tengkawan J, Chia YC, et al. Hypertension and Dementia: A comprehensive review from the HOPE Asia Network. J Clin Hypertens. 2019;21:1091–1098. 10.1111/jch.13558
Contributor Information
Yuda Turana, Email: kkario@jichi.ac.jp.
Kazuomi Kario, Email: yuda.turana@atmajaya.ac.id.
REFERENCES
- 1. Gulland A. Global life expectancy increases by five years. BMJ. 2016;19(353):i2883. [DOI] [PubMed] [Google Scholar]
- 2. WHO . Life expectancy [Internet]. WHO. Available from: http://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends_text/en/. Accessed November 8, 2018.
- 3. Goh VH. Aging in Asia: a cultural, socio‐economical and historical perspective. Aging Male. 2005;8(2):90‐96. [DOI] [PubMed] [Google Scholar]
- 4. Post TJ. How Asia’s population is aging, 2015–2030 scenario [Internet]. The Jakarta Post. Available from: http://www.thejakartapost.com/news/2018/02/14/how-asias-population-is-aging-2015-2030-scenario.html. Accessed November 8, 2018.
- 5. Allaudeen A. Asia is expected to be home to more than half of the elderly population worldwide by 2030 [Internet]. Business Insider. Available from: https://www.businessinsider.com/asia-will-be-home-to-more-than-half-of-the-elderly-population-2017-9. Accessed November 8, 2018.
- 6. Prince MJ. World Alzheimer Report 2015: The Global Impact of Dementia [Internet]. 2015. Available from: https://www.alz.co.uk/research/world-report-2015. Accessed November 8, 2018.
- 7. World Alzheimer Report 2018 . Alzheimer’s Disease International [Internet]. Available from: https://www.alz.co.uk/research/world-report-2018. Accessed November 8, 2018.
- 8. World Health Organization . Dementia [Internet]. Available from: http://www.who.int/news-room/fact-sheets/detail/dementia. Accessed November 8, 2018.
- 9. Alzheimer’s Disease International . Dementia in the Asia Pacific Region [Internet]. Available from: https://www.alz.co.uk/dementia-in-the-asia-pacific. Accessed December 3, 2018.
- 10. Statistics Korea . Annual report on the causes of death statistics. Daejon Stat Korea. 2017.
- 11. Kario K, HOPE Asia (Hypertension Cardiovascular Outcome Prevention and Evidence in Asia) Network . The HOPE Asia Network for “zero” cardiovascular events in Asia. J Clin Hypertens. 2018;20(2):212‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kario K. Evidence and perspectives on the 24‐hour management of hypertension: hemodynamic biomarker‐initiated “anticipation medicine” for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59(3):262‐281. [DOI] [PubMed] [Google Scholar]
- 13. Angeli F, Reboldi G, Verdecchia P. The 2014 hypertension guidelines: implications for patients and practitioners in Asia. Heart Asia. 2015;7(2):21‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aronow WS. Hypertension and cognitive impairment. Ann Transl Med. 2017;5(12):259‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O'Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case‐control study. Lancet. 2016;388(10046):761‐775. [DOI] [PubMed] [Google Scholar]
- 16. Guo X, Östling S, Kern S, Johansson L, Skoog I. Increased risk for dementia both before and after stroke: a population‐based study in women followed over 44 years. Alzheimers Dement. 2018;14(10):1253‐1260. [DOI] [PubMed] [Google Scholar]
- 17. Huang C‐Y, Li Y‐C, Wang H‐K, et al. Stroke suggests increased risk of dementia. Curr Alzheimer Res. 2015;12(3):287‐295. [DOI] [PubMed] [Google Scholar]
- 18. Sun J‐H, Tan L, Yu J‐T. Post‐stroke cognitive impairment: epidemiology, mechanisms and management. Ann Transl Med. 2014;2(8):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iadecola C, Davisson RL. Hypertension and cerebrovascular dysfunction. Cell Metab. 2008;7(6):476‐484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Catindig J‐AS, Venketasubramanian N, Ikram MK, Chen C. Epidemiology of dementia in Asia: insights on prevalence, trends and novel risk factors. J Neurol Sci. 2012;321(1):11‐16. [DOI] [PubMed] [Google Scholar]
- 21. Suriastini NW, Turana Y, Witoelar F, Sikoki B, Wicaksono T, Mulyanto ED. The prevalence, risk factors of dementia and caregiver knowledge of the early symptoms: evidence from a large‐scale survey in Yogyakarta [Internet]. IUSSP – 2017 International Population Conference. Available from: https://iussp.confex.com/iussp/ipc2017/meetingapp.cgi/Paper/4311. December 8, 2018.
- 22. Jin C‐N, Yu C‐M, Sun J‐P, et al. The healthcare burden of hypertension in Asia. Heart Asia. 2013;5(1):238‐243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen C, Homma A, Mok V, et al. Alzheimer’s disease with cerebrovascular disease: current status in the Asia‐Pacific region. J Intern Med. 2016;280(4):359‐374. [DOI] [PubMed] [Google Scholar]
- 24. Kandiah N, Chander RJ, Ng A, Wen MC, Cenina AR, Assam PN. Association between white matter hyperintensity and medial temporal atrophy at various stages of Alzheimer’s disease. Eur J Neurol. 2015;22(1):150‐155. [DOI] [PubMed] [Google Scholar]
- 25. Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in Korea: a systematic review and meta‐analysis. J Korean Med Sci. 2014;29(7):903‐912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ikejima C, Yasuno F, Mizukami K, Sasaki M, Tanimukai S, Asada T. Prevalence and causes of early‐onset dementia in Japan: a population‐based study. Stroke. 2009;40(8):2709‐2714. [DOI] [PubMed] [Google Scholar]
- 27. Honda M, Kusaka Y, Morita A, Nagasawa S, Umino K, Isaki K. A cross‐sectional population‐based study on senile dementia in a rural city. Environ Health Prev Med. 2000;5(1):31‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wu F, Guo Y, Kowal P, et al. Prevalence of major chronic conditions among older Chinese adults: the Study on Global AGEing and Adult Health (SAGE) wave 1. PLoS ONE. 2013;8(9):e74176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sherina MS, Rampal L, Mustaqim A. Factors associated with chronic illness among the elderly in a rural community in Malaysia. Asia Pac J Public Health. 2004;16(2):109‐114. [DOI] [PubMed] [Google Scholar]
- 30. Ministry of Health and National Institute of Health Research and Development . National report on basic health research, Riskesdas, 2013. Jakarta, Indonesia, 2014 (and additional analysis).
- 31. Mwangi J, Kulane A, Van Hoi L. Chronic diseases among the elderly in a rural Vietnam: prevalence, associated socio‐demographic factors and healthcare expenditures. Int J Equity Health. 2015;14(1):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118(25):2679‐2686. [DOI] [PubMed] [Google Scholar]
- 33. Anchala R, Kannuri NK, Pant H, et al. Hypertension in India: a systematic review and meta‐analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170‐1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chia Y‐C, Buranakitjaroen P, Chen C‐H, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia Network. J Clin Hypertens. 2017;19(11):1192‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population‐based studies from 90 countries. Circulation. 2016;134(6):441‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Du Y, Shih M, Lightstone AS, Baldwin S. Hypertension among Asians in Los Angeles County: findings from a multiyear survey. Prev Med Rep. 2017;24(6):302‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ministry of Health and National Institute of Health Research and Development . National report on basic health research, Riskesdas, 2018. Jakarta, Indonesia, 2018.
- 38. Widyantoro B, Situmorang TD, Turana Y, et al. Indonesian May Measurement Month 2017. Publ
- 39. Iadecola C, Yaffe K, Biller J, et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension. 1979;68(6):e67‐e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mezue K, Goyal A, Pressman GS, Matthew R, Horrow JC, Rangaswami J. Blood pressure variability predicts adverse events and cardiovascular outcomes in SPRINT. J Clin Hypertens (Greenwich). 2018;20(9):1247‐1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fujiwara T, Hoshide S, Kanegae H, Eguchi K, Kario K. Exaggerated blood pressure variability is associated with memory impairment in very elderly patients. J Clin Hypertens. 2018;20(4):637‐644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lima N. Hypertension and cognition decline: is there an ultimate link? J Clin Hypertens. 2018;20(11):1584‐1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lattanzi S, Brigo F, Vernieri F, Silvestrini M. Visit‐to‐visit variability in blood pressure and Alzheimer’s disease. J Clin Hypertens (Greenwich). 2018;20(5):918‐924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lattanzi S, Vernieri F, Silvestrini M. Blood pressure variability and neurocognitive functioning. J Clin Hypertens (Greenwich). 2018;20(4):645‐647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wei J, Yin X, Liu Q, Tan L, Jia C. Association between hypertension and cognitive function: a cross‐sectional study in people over 45 years old in China. J Clin Hypertens (Greenwich). 2018;20(11):1575‐1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. National Institute on Aging . High blood pressure is linked to cognitive decline [Internet]. Available from: https://www.nia.nih.gov/news/high-blood-pressure-linked-cognitive-decline. Accessed November 8, 2018.
- 47. van Swieten JC, Geyskes GG, Derix M, et al. Hypertension in the elderly is associated with white matter lesions and cognitive decline. Ann Neurol. 1991;30(6):825‐830. [DOI] [PubMed] [Google Scholar]
- 48. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689‐701. [DOI] [PubMed] [Google Scholar]
- 49. Meissner A. Hypertension and the brain: a risk factor for more than heart disease. Cerebrovasc Dis. 2016;42(3‐4):255‐262. [DOI] [PubMed] [Google Scholar]
- 50. Pires PW, Dams Ramos CM, Matin N, Dorrance AM. The effects of hypertension on the cerebral circulation. Am J Physiol – Heart Circ Physiol. 2013;304(12):H1598‐H1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Huisa BN, Caprihan A, Thompson J, Prestopnik J, Qualls CR, Rosenberg GA. Long‐term blood‐brain barrier permeability changes in binswanger disease. Stroke. 2015;46(9):2413‐2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rosenberg GA. Neurological diseases in relation to the blood‐brain barrier. J Cereb Blood Flow Metab. 2012;32(7):1139‐1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ishii M, Iadecola C. Metabolic and non‐cognitive manifestations of Alzheimer’s disease: the hypothalamus as both culprit and target of pathology. Cell Metab. 2015;22(5):761‐776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Godin O, Tzourio C, Maillard P, Mazoyer B, Dufouil C. Antihypertensive treatment and change in blood pressure are associated with the progression of white matter lesion volumes: the Three‐City (3C)‐Dijon Magnetic Resonance Imaging Study. Circulation. 2011;123(3):266‐273. [DOI] [PubMed] [Google Scholar]
- 55. Parati G, Stergiou GS, Dolan E, Bilo G. Blood pressure variability: clinical relevance and application. J Clin Hypertens. 2018;20(7):1133‐1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Oishi E, Ohara T, Sakata S, et al. Day‐to‐Day blood pressure variability and risk of dementia in a general Japanese elderly population: the Hisayama Study. Circulation. 2017;136(6):516‐525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sogunuru GP, Kario K, Shin J, et al. Morning surge in blood pressure and blood pressure variability in Asia: evidence and statement from the HOPE Asia Network. J Clin Hypertens. 2018;28:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cho N, Hoshide S, Nishizawa M, Fujiwara T, Kario K. Relationship between blood pressure variability and cognitive function in elderly patients with good blood pressure control. Am J Hypertens. 2018;31(3):293‐298. [DOI] [PubMed] [Google Scholar]
- 59. Kario K, Pickering TG. Blood pressure variability in elderly patients. Lancet Lond Engl. 2000;355(9215):1645‐1646. [DOI] [PubMed] [Google Scholar]
- 60. Nagai M, Hoshide S, Nishikawa M, Masahisa S, Kario K. Visit‐to‐visit blood pressure variability in the elderly: associations with cognitive impairment and carotid artery remodeling. Atherosclerosis. 2014;233(1):19‐26. [DOI] [PubMed] [Google Scholar]
- 61. Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K. Visit‐to‐visit blood pressure variations: new independent determinants for cognitive function in the elderly at high risk of cardiovascular disease. J Hypertens. 2012;30(8):1556‐1563. [DOI] [PubMed] [Google Scholar]
- 62. Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertens. 1996;27(1):130‐135. [DOI] [PubMed] [Google Scholar]
- 63. Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K. Ambulatory blood pressure as an independent determinant of brain atrophy and cognitive function in elderly hypertension. J Hypertens. 2008;26(8):1636‐1641. [DOI] [PubMed] [Google Scholar]
- 64. Komori T, Eguchi K, Saito T, Nishimura Y, Hoshide S, Kario K. Riser blood pressure pattern is associated with mild cognitive impairment in heart failure patients. Am J Hypertens. 2016;29(2):194‐201. [DOI] [PubMed] [Google Scholar]
- 65. Eshkoor SA, Hamid TA, Shahar S, Ng CK, Mun CY. Predictive factors of severe stage of dementia among the Malaysian elderly. Arch Gerontol Geriatr Res. 2016;1(1):6‐12. [Google Scholar]
- 66. Lv Y‐B, Zhu P‐F, Yin Z‐X, et al. A U‐shaped association between blood pressure and cognitive impairment in chinese elderly. J Am Med Dir Assoc. 2017;18(2):193.e7‐193.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Youngsakul J, Tohnakayor S. Predicting factors in identifying cognitive decline among Thai adults. J Med Assoc Thai. 2017;100(3):353. [PubMed] [Google Scholar]
- 68. Raina SK, Chander V, Raina S, Kumar D, Grover A, Bhardwaj A. Hypertension and diabetes as risk factors for dementia: a secondary post‐hoc analysis from north‐west India. Ann Indian Acad Neurol. 2015;18(1):63‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Turana Y, Suzy Handajani Y, Widjaja NT. Association between APOE ε4 genotype and memory impairment in elderly with normal global cognitive assessment. Diagnostics. 2015;5(4):615‐623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association between midlife blood pressure levels and late‐life cognitive function. The Honolulu‐Asia Aging Study. JAMA. 1995;274(23):1846‐1851. [PubMed] [Google Scholar]
- 71. Ninomiya T, Ohara T, Hirakawa Y, et al. Midlife and late‐life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58(1):22‐28. [DOI] [PubMed] [Google Scholar]
- 72. Yaffe K, Vittinghoff E, Pletcher MJ, et al. Early adult to midlife cardiovascular risk factors and cognitive function. Circulation. 2014;129(15):1560‐1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Launer LJ, Ross GWebster, Petrovitch H, et al. Midlife blood pressure and dementia: the Honolulu‐Asia aging study. Neurobiol Aging. 2000;21(1):49‐55. [DOI] [PubMed] [Google Scholar]
- 74. Kennelly SP, Lawlor BA, Kenny RA. Blood pressure and dementia – a comprehensive review. Ther Adv Neurol Disord. 2009;2(4):241‐260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Kimm H, Lee PH, Shin YJ, et al. Mid‐life and late‐life vascular risk factors and dementia in Korean men and women. Arch Gerontol Geriatr. 2011;52(3):e117‐e122. [DOI] [PubMed] [Google Scholar]
- 76. Liang X, Shan Y, Ding D, et al. Hypertension and high blood pressure are associated with dementia among Chinese dwelling elderly: the Shanghai Aging Study. Front Neurol. 2018;9:664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lin C‐H, Cheng H‐M, Chuang S‐Y, Chen C‐H. Vascular aging and cognitive dysfunction: silent midlife crisis in the brain. Pulse. 2017;5(1‐4):127‐132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. The SPRINT MIND Investigators for the SPRINT Research Group , Williamson JD, Pajewski NM, et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321:553‐561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nagai M, Hoshide S, Kario K. Hypertension and dementia. Am J Hypertens. 2010;23(2):116‐124. [DOI] [PubMed] [Google Scholar]
- 80. Yano Y, Bakris GL, Inokuchi T, et al. Association of cognitive dysfunction with cardiovascular disease events in elderly hypertensive patients. J Hypertens. 2014;32(2):423‐431. [DOI] [PubMed] [Google Scholar]
- 81. Igase M, Kohara K, Miki T. The association between hypertension and dementia in the elderly. Int J Hypertens. 2012;2012:320648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lovell MA, Abner E, Kryscio R, Xu L, Fister SX, Lynn BC. Calcium channel blockers, progression to dementia, and effects on amyloid beta peptide production. Oxid Med Cell Longev. 2015;2015:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Li N‐C, Lee A, Whitmer RA, et al. Use of angiotensin receptor blockers and risk of dementia in a predominantly male population: prospective cohort analysis. BMJ. 2010;340:b5465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. van Middelaar T, van Vught LA, van Charante E, et al. Lower dementia risk with different classes of antihypertensive medication in older patients. J Hypertens. 2017;35(10):2095‐2101. [DOI] [PubMed] [Google Scholar]
- 85. Forette F, Seux M‐L, Staessen JA, et al. Prevention of dementia in randomised double‐blind placebo‐controlled Systolic Hypertension in Europe (Syst‐Eur) trial. Lancet. 1998;352(9137):1347‐1351. [DOI] [PubMed] [Google Scholar]
- 86. Gao S, Jin Y, Unverzagt FW, et al. Hypertension and cognitive decline in rural elderly Chinese. J Am Geriatr Soc. 2009;57(6):1051‐1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Whelton PK, Williams B. The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: more similar than different. JAMA. 2018;320(17):1749‐1750. [DOI] [PubMed] [Google Scholar]
- 88. Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET‐COG): a double‐blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683‐689. [DOI] [PubMed] [Google Scholar]
- 89. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021‐3104. [DOI] [PubMed] [Google Scholar]


