Abstract
The present study aims to examine the cross‐sectional and longitudinal association between self‐reported nocturnal sleep duration, blood pressure, and hypertension in European children, aged 2‐9.9 years, participating in the IDEFICS project. Blood pressure (BP) and the main anthropometric indices were measured according to standardized procedures. Childhood elevated BP and hypertension were defined according to the European Society of Hypertension Guidelines for children and adolescents. Parents reported lifestyle and socio‐demographic data. Nocturnal sleep duration was assessed as part of a parental 24‐h recall and categorized as follows: (a) ≤9 hours/night; (b) >9 hours to ≤10 hours/night; (c) >10 hours to ≤11 hours/night; and (d) >11 hours/night. A complete set of variables included in the present analysis was provided by 7974 participants (boys/girls = 4049/3925) at the baseline survey (T0). Of them, 5656 were re‐examined 2 years later at follow‐up (T1). Children reporting shorter sleep duration at T0 had significantly higher BP values (P for trend < 0.001) compared to those who slept more. Prospective analyses showed that shorter sleep duration at baseline predicted, over the 2‐year follow‐up, higher increases in systolic blood pressure and diastolic blood pressure, after adjustment for age, sex, country of origin, BMI z‐score, parental education, physical activity, screen time, and T0 value of the examined outcome variables (P for trend < 0.001). Our findings reveal that shorter sleep duration is associated with higher BP in childhood, suggesting that sleep may be a potential risk factor for hypertension later in life.
Keywords: blood pressure, childhood, hypertension, sleep duration
1. INTRODUCTION
Hypertension is a global public health problem with increasing prevalence among both adults1 and children.2
Hypertension in childhood has been identified as a significant risk factor for later cardiovascular diseases3 and target‐organ damage.4 There is increasing evidence that high blood pressure (BP) tracks from childhood to adulthood,5 suggesting that children with high BP are more likely to develop hypertension later in life. Considering that no single cutoff point defines hypertension in children and adolescents, the identification of hypertension in young people is more difficult than in adults.6
Even if the major risk factors for hypertension, including obesity, ethnicity, family history of hypertension, dietary, and lifestyle habits are well established, sleep is an unusual and often overlooked factor. Sleep plays an essential role in the daily life of adults and in the growth of children and adolescents; an adequate amount of sleep is fundamental for human functioning and well‐being throughout the lifetime.7
Sleep habits are influenced by different factors (eg, biological, cultural, and socio‐demographic) whose interaction plays an important role in the establishment of behavioral rules.8 Previous studies revealed significant differences in bedtimes and total sleep times among children in diverse areas.9 These differences might reflect distinct cultural values, beliefs, and customs, which, in turn, seem to influence sleep behaviors and practices during childhood.
The National Heart, Lung and Blood Institute (NHLBI) recommend at least 10 hours of sleep a day for school‐aged children and 7 to 8 hours a day for healthy adults.10 However, according to the “2014 Sleep in America poll,” 31% of US children, aged 6‐11 years, sleep less than 9 hours per night on school days.11 Similarly, about 33% of European adolescents sleep < 8 hours per night, as reported in the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study.12
Several studies have suggested that insufficient sleep duration is associated with adverse health outcomes, including hypertension, in both children and adults.13, 14, 15, 16 In detail, more studies have shown that adults, without apparent sleep disorders and with habitual sleep time less than 6 hours per night, have an increased risk of hypertension.15, 16 Few epidemiological studies have investigated this association in younger populations, with contrasting results.14, 17, 18
A longitudinal study in younger children (aged 6 to 11 years) found that decreases in total sleep time were associated with increases in BP at follow‐up.19 In contrast, Sampei et al20 suggested that long sleep duration was significantly associated with increased systolic blood pressure (SBP) in children aged 5‐6 years. Furthermore, no significant association between sleep quantity and 24‐hour ambulatory BP was reported in healthy children by Martikainen et al.21
Collectively, these studies suggest a plausible link between sleep duration and risk of hypertension, although confirmation is needed especially in children and adolescents. Our study aims to examine both cross‐sectional and prospective associations of self‐reported sleep duration with blood pressure and prevalent and incident elevated BP/hypertension in a large sample of European pre‐school and school children participating in the IDEFICS (Identification and prevention of Dietary‐ and lifestyle-induced health EFfects In Children and infantS) study.22
2. METHODS
2.1. Study population
The IDEFICS study is a large‐scale multi‐center study, funded by the European Commission within the Sixth Framework Program, aiming to investigate the etiology of overweight and obesity in European children aged 2 to 9.9 years (registration number ISRCTN62310987). Details on the general design and objectives of the study have been described elsewhere.22 The study was conducted according to the standards of the Declaration of Helsinki. All applicable institutional and governmental regulations pertaining to the ethical use of human volunteers were followed during this research. Participants were not subjected to any study procedure before informed consent was given by, both, the children (orally) and their parents (in writing). Participants were allowed to opt out for specific examination modules. The study protocol was approved by the local ethics committee in each participating country.
Briefly, the baseline survey (T0) was conducted from September 2007 to May 2008 in a cohort of 16 228 children from eight European countries (Belgium, Cyprus, Estonia, Germany, Hungary, Italy, Spain, and Sweden), according to a standardized protocol. Comparable intervention and control regions were selected in each country. In the intervention regions, a coherent set of intervention modules were implemented, focusing on diet, physical activity, and stress‐coping capacity. All the materials for the intervention were centrally developed and culturally adapted. A detailed description of the IDEFICS intervention program has been previously published.23 A follow‐up examination (T1) was carried out from September 2009 to May 2010.
The cross‐sectional analysis included 7974 children (boys/girls = 4049/3925) after the exclusion of 8254 children from the original cohort because of missing data on sleep duration (n = 6778) and BP (n = 1476). Excluded children did not differ from the analysis group in terms of sex distribution and BP, while they were on average slightly younger (mean difference 0.20 years, P < 0.001) and slept longer (mean difference 0.25 hours/night, P < 0.001) than children included in the analysis. Of the children examined at T0, 5656 (boys/girls = 2853/2803) were re‐examined 2 years later at T1 (71% of the T0 sample). The participants flowchart is shown in Figure 1.
Figure 1.
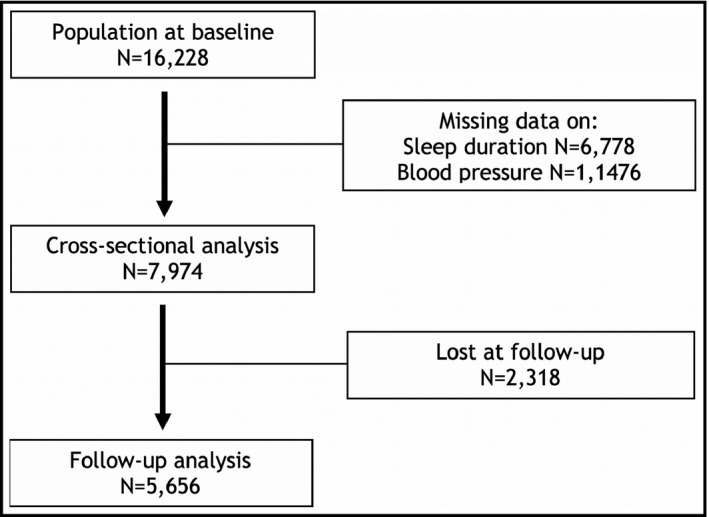
Flow chart showing how the final study population was selected
2.2. Anthropometric measurements
At both examinations, T0 and T1, children underwent a standardized physical examination. Anthropometric data included body weight and height, waist and hip circumference, and the measurement of skinfold thickness. A detailed description of the anthropometric measurements in the IDEFICS study, including intra‐ and inter‐observer reliability, has been already published.24 Body height was measured, without shoes, by a calibrated stadiometer (SECA 225; Seca, Birmingham, UK) to the nearest 0.1 cm. The children were weighed in light clothes and without shoes using an electronic scale (Tanita BC 420 SMA, Tanita Europe GmbH, Sindelfingen, Germany) with an approximation of 0.1 kilograms (kg). Body mass index (BMI) was calculated as weight in kg divided by the square of height in meters (kg/m2). Sex‐ and age‐specific BMI z‐scores 25 were used as anthropometric indices for the statistical analysis.
2.3. Blood pressure measurement
Blood pressure measurement was performed during the day of the physical examination, in a quiet and warm room. Systolic BP (SBP) and diastolic BP (DBP) were measured at the right arm while the child was in a seated position with the back supported, uncrossed legs, feet on the floor, and the upper arm at the heart level. Children were asked to sit for at least 5 minutes before the measurement, and they were advised to avoid stimulant food/drinks and physical activity within the last 30 minutes before measurement. An automated oscillometric device (Welch Allyn 4200B‐E2 Inc, Skaneateles Falls, NY, USA)26 was used according to a standardized procedure. For the choice of the appropriate cuff size, arm circumference was measured using an inelastic tape (Seca 200, Birmingham, UK). Detailed procedures have been previously described.27
Two measurements were taken with 2‐minute interval, plus a further one in case of a >5% difference in BP between the first two readings. The mean of the two values of SBP and DBP closest together were used for the analyses here described. For the definition of elevated BP and hypertension, we referred to the criteria of the update to the 2004 “The Fourth Report on the Diagnosis, Evaluation, and Treatment of High BP in Children and Adolescents”.28 According to age‐, sex‐ and height‐specific BP percentiles, calculated in the IDEFICS population,27 normal BP in children was defined as average SBP and DBP below the 90th percentile; elevated BP was identified as average SBP or DBP equal to or above the 90th percentile, but below the 95th percentile; finally, hypertension was defined as average SBP and/or DBP equal to or above the 95th percentile. In the current analysis, high values of BP included elevated BP and hypertension.
2.4. Sleep information and questionnaire
The primary exposure of interest in our study was sleep duration. On the day of the physical examination, nocturnal sleep duration was collected in the context of a standardized 24‐hour dietary recall (24HDR), based on the responses of parents or guardians of each participating child to the Self‐Administered Children and Infant Nutrition Assessment (SACINA). This computer‐based instrument, developed for the IDEFICS project, was based on a previously existing validated software used in European adolescents, called HELENA‐DIAT.29 Sleep data were collected on all days of the week but, for our analysis, we used only those referred to the nights from Monday to Thursday. We assume that weekdays sleep should be more representative of habitual sleep duration given that bedtime and wake‐up times, in the school age, more likely adhere to a regular routine on weekdays than during the weekend. Parents were thus asked about their child's get up time in the morning and bedtime on the day before the visit.
Socio‐demographic data, environmental and behavioral factors were collected using a questionnaire filled in at home by parents, both at T0 and at T1.30 The parental education level was assessed by asking parents for their highest educational attainment and categorized according to the International Standard Classification of Education (ISCED) into low (ISCED levels 1 and 2), medium (ISCED levels 3 and 4), and high (ISCED level 5) educational attainment.31 With regard to physical activity, parents were asked to report if their children were sports club members. In addition, parents reported how much time their child usually spent watching television or computer screen (screen time).
2.5. Statistical analysis
Data were analyzed using IBM SPSS Statistics (version 23.0 Armonk, NY: IBM Corp.). Statistical significance was accepted for P values < 0.05. Data are expressed as mean (95% confidence intervals, CI) for continuous variables and as percentages for categorical variables. Nocturnal sleep duration was calculated as the difference between bed and getup time in the SACINA interview, and a continuous variable, expressed as hours per night, was obtained. For our analysis, children were categorized into four groups according to sleep duration: (a) ≤9 hours/night (n = 971); (b) >9 hours to ≤10 hours /night (n = 2799); (c) >10 hours to ≤11 hours/night (n = 2907); and (d) >11 hours /night (n = 1297).
Analysis of covariance (ANCOVA) was performed to compare mean values of outcome variables across the sleep duration categories adjusting for covariates (age, sex, BMI z‐score, and country of origin). P values for linear trend were reported. Differences in categorical variables across sleep duration groups were compared using the chi‐square test.
Longitudinal analyses were performed using the 2‐year change in SBP and DBP variables (SBP/DBP at T1 minus SBP/DBP at T0). The effect of belonging to the intervention or control groups on the outcome variables was estimated by the effect size selecting the option “Estimates of effect size” in “Univariate” analysis in SPSS. Specifically, to test the “sleep duration × intervention” interaction, we used analysis of variance with sleep duration, intervention/control group, and “sleep duration × intervention” factor as the independent variables predicting the change in SBP and DBP over time. Since the effect was negligible (partial Eta squared values of SBP and DBP <0.01), intervention and control groups were pooled in the analysis. Therefore, the analysis was adjusted for country of origin, and baseline values of age, sex, BMI z‐score, physical activity, screen time, parental education, and BP.
3. RESULTS
3.1. Descriptive analysis
The present analysis includes 7974 children (boys/girls = 4049/3925) with a mean age of 6.1 ± 1.8 years (mean ± standard deviation, M ± SD) at baseline. Children slept, on average, 10.2 ± 1.0 hours per night during weekday nights (M ± SD). The mean systolic and diastolic BP values were 100.6 ± 9.3 mm Hg (M ± SD) and 63.2 ± 6.5 mm Hg (M ± SD), respectively.
3.2. Cross‐sectional analysis
Table 1 shows the characteristics of the study participants at T0 according to sleep duration categories. Overall, 12.2% (n = 971) of the children reported a sleep duration of ≤ 9 hours/night, 35.1% (n = 2799) of >9 hours to ≤10 hours/night, 36.4% (n = 2907) of >10 hours to ≤11 hours/night, and 16.3% (n = 1297) of >11 hours/night.
Table 1.
Baseline characteristics of the sample according to sleep duration categories
| Sleep duration categories | |||||
|---|---|---|---|---|---|
| ≤9 h | >9 h to ≤10 h | >10 h to ≤11 h | >11 h | P | |
| Boys/Girls (N) | 493/478 | 1410/1389 | 1509/1398 | 637/660 | |
| Age (years) | 6.3 (6.2;6.4) | 6.4 (6.3;6.5) | 6.1 (6.1;6.2) | 5.4 (5.3;5.5) | <0.001* |
| SBP (mm Hg)a | 101.2 (100.7;101.8) | 101.0 (100.7;101.3) | 100.4 (100.1;100.7) | 99.7 (99.2;100.2) | <0.001* |
| DBP (mm Hg)a | 63.9 (63.5;64.3) | 63.5 (63.2;63.7) | 62.9 (62.7;63.2) | 62.5 (62.1;62.8) | <0.001* |
| Prevalence of elevated BP/hypertension % (N) | 18.5 (180) | 17.5 (491) | 15.9 (463) | 11.6 (151) | χ2 ≤ 0.001 # |
| BMI z‐scoreb | 0.5 (0.5;0.6) | 0.4 (0.4;0.5) | 0.3 (0.3;0.4) | 0.2 (0.2;0.3) | <0.001* |
| Screen time (hours per week)a | 13.1 (12.6;13.5) | 12.3 (12.0;12.6) | 11.5 (11.3;11.8) | 11.1 (10.7;11.5) | <0.001* |
| Physical activity (%) Yes | 46.2 | 46.4 | 47.7 | 47.9 | χ2 = 0.684 # |
| Parental education (%) High | 16.3 | 29.0 | 35.9 | 33.4 | χ2 ≤ 0.001 # |
Data are expressed as mean (95% confidence interval) or as frequency (%).
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Analysis adjusted by age, sex, BMI z‐score, and country of origin.
Analysis adjusted by age, sex, and country of origin.
P value for trend.
P by Linear‐by‐linear association.
An inverse, linear and statistically significant association was found between sleep duration and BP: the higher the number of hours of sleep, the lower the SBP and DBP (P for trend < 0.001). These associations were independent of sex, age, BMI z‐score, and country of origin. Moreover, children with shorter sleep duration (≤9 hours/night) reported a higher screen time per week, and a lower level of parental education compared to those who slept more. The prevalence of elevated BP/hypertension significantly decreased along with the increase of sleep duration.
3.3. Prospective analysis
Table 2 shows the changes in SBP and DBP over the 2‐year follow‐up. Participants with shorter baseline sleep duration showed significantly higher increase in BP after adjustment for age, sex, BMI z‐score, country of origin, physical activity, screen time, and parental education, and T0 value of the examined variables (Pfor trend < 0.001). We also examined whether there was an interaction between the sleep duration and the intervention program on the change in the BP traits at 2 years. No statistically significant “sleep duration × intervention” interaction was found for changes in SBP (F = 0.63, P = 0.60) and DBP (F = 1.40, P = 0.24). At T1, 410 incident cases of elevated BP/hypertension were observed among children normotensive at baseline. The incidence of elevated BP/hypertension significantly declined along with increasing sleep duration.
Table 2.
Changes in SBP and DBP, and incidence of elevated BP/hypertension over the 2‐year follow‐up according to sleep duration categories defined at baseline
| Sleep duration | |||||
|---|---|---|---|---|---|
| ≤9h | >9 h to ≤10 h | >10 h to ≤11 h | >11 h | P | |
| Δ SBP (mm Hg) | 3.6 (3.1;4.2) | 3.5 (3.2;3.9) | 2.0 (1.6;2.3) | 0,4 (−0.1;1.0) | <0.001* |
| Δ DBP (mm Hg) | 0.9 (0.5;1.4) | 0.9 (0.7;1.2) | 0.3 (0.0;0.5) | −0.5 (−0.9;‐0.1) | <0.001* |
| Incidence % (N) | 12.4 (67) | 11.2 (165) | 8.5 (137) | 6.0 (41) | χ2 ≤ 0.001 # |
Data are expressed as mean (95% confidence interval) or as frequency (%).
ΔDBP, change in diastolic blood pressure; ΔSBP, change in systolic blood pressure.
Pvalue for trend by multiple regression analysis adjusted for age, sex, BMI z‐score, country of origin, physical activity, screen time, parental education, and basal value of the examined variables.
P by Linear‐by‐linear association.
4. DISCUSSION
We investigated cross‐sectionally and longitudinally the association between sleep duration, blood pressure, and the risk of elevated BP/hypertension in European schoolchildren participating in the IDEFICS study. The findings of the cross‐sectional analysis showed that blood pressure levels were associated with sleep duration, with increasing values observed going down through the sleep duration categories. The prevalence of elevated BP/hypertension also increased in children reporting shorter sleeping time. Moreover, shorter sleep duration at baseline predicted higher increases in SBP and DBP, and higher incidence of elevated BP/hypertension over the 2‐year follow‐up. In short, decreasing sleep duration paralleled increasing BP, suggesting that adequate hours of sleep are a potential factor in the control and prevention of high BP during childhood. Because of the major adverse health consequences of high BP over the life span, nocturnal sleep duration may be considered among the clinically relevant and potentially modifiable risk factor for high BP.
The association between sleep duration and hypertension in adult populations has been confirmed by systematic review and meta‐analyses.13, 15, 32 With regard to children and adolescents, the existing literature on sleep, hypertension, and cardiovascular disease is limited and relatively weak, as reported in a recent review.14
Considering cross‐sectional studies in children, Sampei et al showed a positive correlation between sleep duration and SBP,20 whereas Bayer et al found only a marginal lower BP in patients with the longest sleep duration.33 A Chinese study in 4902 children and adolescents found short sleep duration to be associated with a higher risk of hypertension only in boys aged 11‐14 years.17 In a longitudinal study, Wells and colleagues34 found that shorter sleep duration predicted increased risk of higher BP in Brazilian adolescents and that this association was mediated by body fat. Moreover, Archbold et al19 reported that increases in SBP and DBP were associated with decreased sleep time over a 5‐year period.
There are many pathways through which short sleep duration could potentially contribute to high BP in humans. Some studies suggested that short sleep duration could raise BP by increasing sympathetic nervous system activity, or by disrupting circadian rhythm and autonomic response.35, 36 It is well known that long‐term sleep curtailment may result in a stressful condition,37 possibly impacting BP regulation. In fact, a prolonged exposure to stress has been found to increase salt appetite and to impair renal sodium excretion.37 Moreover, the effect of sleep on BP could be also modulated by the influence of short sleep duration on body weight throughout the regulation of satiety and appetite, by reducing leptin levels and increasing ghrelin concentrations.37 Further studies would be required to substantiate the physiological bases of the sleep/BP connection.
Strength of the present study is the highly standardized phenotypic measurements within the participating European countries. In fact, all measurements were conducted according to detailed standard operation procedures.24, 27 Additional strengths of our study include the large sample size and the inclusion of a number of covariates possibly affecting both sleep patterns and BP.
The main limitation of our study is that sleep duration was self‐reported by the parents of the participants, and referred to a single weekday. However, a moderate agreement has been found in previous studies between self‐reported and objectively measured sleep duration (actigraphic monitoring).38 Thus, although self‐reported data are not as accurate as actigraphy, they are widely used particularly in children, due to their ease of use and minimal time and costs involved in data collection.39 Finally, no information was collected on daytime napping, sleep quality, and sleep disorders, including obstructive sleep apnea possibly linked to increased risk of elevated BP in children.40
In summary, our data showed that children with shorter sleep duration had a greater increase in SBP and DPB over time and, therefore, they might be at higher risk of developing hypertension during growth. They offer support to consider short sleep duration during childhood as a risk factor for elevated BP, also later in life. Our data reinforce the concept that more attention should be given to sleep duration during childhood and that a reduction in sleep deprivation could potentially contribute to prevent hypertension. Practical strategies include advice to parents to improve children's sleep habits by emphasizing the importance of maintaining a regular sleep/wake schedule, and by establishing a comfortable sleeping environment. Intervention studies aimed to the implementation of sleep hygiene could further confirm the efficacy of adequate sleep in reducing the risk of hypertension.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
This study was conducted as part of the IDEFICS study (http://www.idefics.eu). We gratefully acknowledge the financial support of the European Community within the Sixth RTD Framework Programme Contract no. 016181 (FOOD) and the grant support from EU for the IDEFICS study. We are grateful for the support provided by school boards, headmasters and communities. We thank the IDEFICS children and their parents for participating in this extensive examination.
Sparano S, Lauria F, Ahrens W, et al. Sleep duration and blood pressure in children: Analysis of the pan‐European IDEFICS cohort. J Clin Hypertens. 2019;21:572–578. 10.1111/jch.13520
REFERENCES
- 1. World Health Organization . A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2. Bell CS, Samuel JP, Samuels JA. Prevalence of hypertension in children. Hypertension. 2019;73(1):148‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Falkner B. The childhood role in development of primary hypertension. Am J Hypertens. 2018;31(7):762‐769. [DOI] [PubMed] [Google Scholar]
- 4. Meng L, Hou D, Zhao X, et al. Cardiovascular target organ damage could have been detected in sustained pediatric hypertension. Blood Press. 2015;24(5):284‐292. [DOI] [PubMed] [Google Scholar]
- 5. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta‐regression analysis. Circulation. 2008;117(25):3171‐3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daniels SR. What is the prevalence of childhood hypertension? it depends on the definition. JAMA Pediatr. 2018;172:519‐520. [DOI] [PubMed] [Google Scholar]
- 7. Thumann B, Bornhorst C, Michels N, et al. Cross‐sectional and longitudinal associations between psychosocial well‐being and sleep in European children and adolescents. J Sleep Res. 2019;28:e12783. [DOI] [PubMed] [Google Scholar]
- 8. Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115(1 Suppl):204‐216. [DOI] [PubMed] [Google Scholar]
- 9. Anujuo KO, Vrijkotte TG, Stronks K, Jean‐Louis G, Agyemang CO. Ethnic differences in sleep duration at 5 years, and its relationship with overweight and blood pressure. Eur J Public Health. 2016;26(6):1001‐1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Heart, Lung, and Blood Institute . (2012). How much sleep is enough? (2012). Available to: https://www.nhlbi.nih.gov/node/4606.
- 11. National Sleep Foundation 2014 Sleep in America Poll. Available at: https://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings---FINAL-Updated-3-26-14-.pdf.
- 12. Garaulet M, Ortega FB, Ruiz JR, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes (Lond). 2011;35(10):1308‐1317. [DOI] [PubMed] [Google Scholar]
- 13. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta‐analysis of prospective studies. Eur Heart J. 2011;32(12):1484‐1492. [DOI] [PubMed] [Google Scholar]
- 14. Fobian AD, Elliott L, Louie T. A Systematic Review of Sleep, Hypertension, and Cardiovascular Risk in Children and Adolescents. Curr Hypertens Rep. 2018;20(5):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Guo X, Zheng L, Wang J, et al. Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta‐analysis. Sleep Med. 2013;14(4):324‐332. [DOI] [PubMed] [Google Scholar]
- 16. Knutson KL, Van Cauter E, Rathouz PJ, et al. Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med. 2009;169(11):1055‐1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guo X, Zheng L, Li Y, et al. Association between sleep duration and hypertension among Chinese children and adolescents. Clin Cardiol. 2011;34(12):774‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bal C, Öztürk A, Çiçek B, et al. The relationship between blood pressure and sleep duration in turkish children: a cross‐sectional study. J Clin Res Pediatr Endocrinol. 2018;10(1):51‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Archbold KH, Vasquez MM, Goodwin JL, Quan SF. Effects of sleep patterns and obesity on increases in blood pressure in a 5‐year period: report from the Tucson Children's Assessment of Sleep Apnea Study. J Pediatr. 2012;161(1):26‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sampei M, Dakeishi M, Wood DC, Murata K. Impact of total sleep duration on blood pressure in preschool children. Biomed Res. 2006;27(3):111‐115. [DOI] [PubMed] [Google Scholar]
- 21. Martikainen S, Pesonen AK, Feldt K, et al. Poor sleep and cardiovascular function in children. Hypertension. 2011;58(1):16‐21. [DOI] [PubMed] [Google Scholar]
- 22. Ahrens W, Bammann K, Siani A, et al. The IDEFICS cohort: design, characteristics and participation in the baseline survey. Int J Obes (Lond). 2011;35(Suppl 1):S3‐S15. [DOI] [PubMed] [Google Scholar]
- 23. De Henauw S, Verbestel V, Mårild S, et al. The IDEFICS community‐oriented intervention programme: a new model for childhood obesity prevention in Europe? Int J Obes (Lond). 2011;35(Suppl 1):S16‐S23. [DOI] [PubMed] [Google Scholar]
- 24. Stomfai S, Ahrens W, Bammann K, et al. IDEFICS Consortium. Intra‐ and interobserver reliability in anthropometric measurements in children. Int J Obes (Lond). 2011; 35(Suppl 1):S45‐S51. [DOI] [PubMed] [Google Scholar]
- 25. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284‐294. [DOI] [PubMed] [Google Scholar]
- 26. Alpert BS. Validation of the Welch Allyn spot vital signs blood pressure device according to the ANSI/AAMI SP10: 2002. Accuracy and cost‐efficiency successfully combined. Blood Press Monit. 2007; 12(5):345‐347. [DOI] [PubMed] [Google Scholar]
- 27. Barba G, Buck C, Bammann K, et al. IDEFICS consortium. Blood pressure reference values for European non‐overweight school children: the IDEFICS study. Int J Obes (Lond). 2014;38(Suppl 2):S48‐S56. [DOI] [PubMed] [Google Scholar]
- 28. Flynn JT, Kaelber DC, Baker‐Smith CM, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. [DOI] [PubMed] [Google Scholar]
- 29. Vereecken CA, Covents M, Sichert‐Hellert W, et al. Development and evaluation of a self‐administered computerized 24‐h dietary recall method for adolescents in Europe. Int J Obes (Lond). 2008;32(Suppl 5):S26‐S34. [DOI] [PubMed] [Google Scholar]
- 30. Bammann K, Peplies J, Sjostrom M, et al. Assessment of diet, physical activity, biological, social and environmental factors in a multi‐centre European project on diet‐ and lifestyle related disorders in children (IDEFICS). J Public Health. 2006;14:279‐289. [Google Scholar]
- 31. International Standard . Classification of Education (ISCED) UNESCO 1997. http://www.unesco.org/education/information/nfsunesco/doc/isced_1997.htm.
- 32. Gangwisch JE. A review of evidence for the link between sleep duration and hypertension. Hypertens Am J. 2014; 27(10):1235‐1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bayer O, Neuhauser H, von Kries R. Sleep duration and blood pressure in children: a cross‐sectional study. J Hypertens. 2009;27(9):1789‐1793. [DOI] [PubMed] [Google Scholar]
- 34. Wells JC, Hallal PC, Reichert FF, Menezes AM, Araújo CL, Victora CG. Sleep patterns and television viewing in relation to obesity and blood pressure: evidence from an adolescent Brazilian birth cohort. Int J Obes (Lond). 2008;32(7):1042‐1049. [DOI] [PubMed] [Google Scholar]
- 35. Gangwisch JE. Epidemiological evidence for the links between sleep, circadian rhythms and metabolism. Obes Rev. 2009;10(Suppl 2):37‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. van Leeuwen W, Sallinen M, Virkkala J, et al. Physiological and autonomic stress responses after prolonged sleep restriction and subsequent recovery sleep in healthy young men. Sleep Biol Rhythms. 2018;16(1):45‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: from physiological to pathological conditions. Sleep Sci. 2015;8(3):143‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self‐reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838‐845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Matricciani L. Subjective reports of children's sleep duration: does the question matter? A literature review. Sleep Med. 2013;14(4):303‐311. [DOI] [PubMed] [Google Scholar]
- 40. Enright PL, Goodwin JL, Sherrill DL, Quan JR, Quan SF. Tucson children's assessment of sleep apnea study. Blood pressure elevation associated with sleep‐related breathing disorder in a community sample of white and Hispanic children: the Tucson children's assessment of sleep apnea study. Arch Pediatr Adolesc Med. 2003;157(9):901‐904. [DOI] [PubMed] [Google Scholar]


