Abstract
Blood pressure (BP) monitors equipped with atrial fibrillation (AF) detection algorithm are attractive screening tools for AF in elderly hypertensives. This study assessed the diagnostic accuracy of a novel cuffless pocket‐size self‐BP monitor (Freescan, Maisense) equipped with an AF detection algorithm, which displays results for the detection of “AF” or “Arrhythmia” during routine BP measurement. Subjects aged >65 years or 60‐65 years with hypertension, diabetes, or cardiovascular disease were subjected to BP measurements using the Freescan device with simultaneous continuous Holter electrocardiography (ECG) monitoring. Readings with device notification “Instability” (29%) or “Error” (20%) were discarded. Data from 136 subjects with five valid Freescan BP measurements were analyzed (age 73.8 ± 7.1 years, males 63%, treated hypertensives 88%, AF in ECG 21%). Analysis of 680 Freescan readings vs ECG revealed specificity 99%, sensitivity 67%, and diagnostic accuracy 93% for AF diagnosis. When the “Arrhythmia” notification was considered as AF diagnosis, the sensitivity was improved (93%, 96%, and 93%, respectively). Analysis of AF diagnosis in subjects (diagnosis defined as at least three of five readings indicating “AF” or “Arrhythmia”) revealed specificity, sensitivity, and diagnostic accuracy for AF detection at 94%, 100%, and 95%, respectively. These data suggest that the Freescan cuffless device could be used as a useful screening tool for AF detection during routine self‐measurement of BP in the elderly.
Keywords: atrial fibrillation, automated, blood pressure measurement, cuffless, screening
1. INTRODUCTION
Atrial fibrillation (AF) is the most common sustained arrhythmia with increasing prevalence in the elderly and is associated with 5‐fold increase in stroke risk.1 AF often is asymptomatic or paroxysmal and may remain undiagnosed for long time until a stroke event occurs.1 The European Society of Cardiology (ESC) recommends opportunistic screening for AF in patients >65 years to allow early detection of asymptomatic AF.1
Hypertension and AF often coexist, particularly in the elderly, as demonstrated in recent outcome trials of novel oral anticoagulants in AF patients of whom 50%‐90% had hypertension.2 In the last decade, automated oscillometric blood pressure (BP) monitors equipped with an algorithm specific for AF detection during BP measurement have been developed.3 In 2013, the UK National Institute for Health and Care Excellence (NICE) recommended the automated upper‐arm cuff BP monitor Microlife Afib for opportunistic AF screening during routine office BP measurement in primary care in subjects aged ≥65 years.4 A recent meta‐analysis of 11 studies assessing the diagnostic accuracy of an AF detection algorithm during automated BP measurement vs reference electrocardiography (ECG) showed high sensitivity (95%), specificity (94%), and accuracy (94%) for AF detection.3
A novel pocket‐size cuffless device for self‐BP monitoring (Freescan, Maisense Inc), which is equipped with an AF detection algorithm during BP measurement has been developed. This study investigated the diagnostic accuracy of this device for AF detection routine BP measurement in elderly individuals.
2. METHODS
2.1. Test device
The Freescan device (Maisense Inc) is a pocket‐size (95.5 × 37 × 22 mm), light (60 g) cuffless BP monitor (Figure 1). Its BP measurement accuracy has been validated using the ANSI/AAMI/ISO 2013 protocol in static conditions shortly after BP calibration for each individual using a mercury sphygmomanometer.5 Details on the BP measurement technology of this novel device have been reported.5 In brief, the device has three embedded electrodes and one force sensor. The user applies the force sensor on her/his radial artery, while holding the device with her/his other hand from the embedded electrodes. By continuously pressing the central button, radial pulse wave is identified by the force sensor, while a single‐lead ECG is provided by touching the electrodes. A successful self‐measurement of BP and heart rate is obtained within 10 seconds. In case of inability or uncertainty of the device to detect good‐quality pulse wave, an “Error” (BP and heart rate not displayed) or “Instability” notification (BP and heart rate values displayed but with a warning) appears on the screen, respectively. Using a mobile phone app (myFreescan app), the results are transferred via Bluetooth to an online personal Patient Care System (PCS) in the official Maisense website. Measurement details are accessible using either mobile phone or PC.
Figure 1.
The Freescan cuffless self‐blood pressure monitor equipped with atrial fibrillation detection algorithm
Atrial fibrillation detection is a new feature of the Freescan device based on ECG evaluation of R‐R intervals. It incorporates a feature which extracts the variability of RR intervals while considering Shannon entropy and Markov processing.6, 7 This approach further incorporates the denoise autoencoder and deep neural network as the classifier to interpret the types of arrhythmia (AF/non‐AF).8, 9 To decrease the false‐positive rate, an additional approach is applied which integrates the weight of P‐wave absence for AF diagnosis with the decision value of deep neural network.
Atrial fibrillation or arrhythmia detection by the Freescan device is displayed on its screen detects with a multiple‐heart symbol aside to the BP and heart rate values. In the online PCS website, BP and heart rate values are accompanied by the indication “AF” or “Arrhythmia” (if arrhythmia other than AF is identified). The Freescan and its AF detection algorithm have European Conformity (CE) medical certificates. In the present study, analysis was based on data obtained from the PCS website.
2.2. Reference AF evaluation
Continuous Holter ECG monitoring was used as reference method for AF detection using the SpiderView multichannel system recorder (ELA Medical, Sorin Group). Recordings were downloaded and assessed using the EasyScope Multiday ELA Medical software.
2.3. Participants
Subjects were recruited from a Hypertension Outpatient Clinic. Inclusion criteria were as follows: (a) age >65 years or, (b) age 60‐65 years with hypertension, or diabetes, or cardiovascular disease (coronary heart disease, heart failure, stroke). Exclusion criteria were pacemaker implantation or unwillingness to participate.
2.4. Validation study
Participants had a single office BP measurement using a validated professional upper‐arm cuff oscillometric device with appropriate cuff size (www.stridebp.org). A brief training and familiarization session was performed for participants to self‐measure their BP using the Freescan device. A Holter ECG monitor was fitted on participants, as reference method for AF detection. Time was synchronized in Freescan and Holter devices. Under continuous ECG monitoring, participants were asked to self‐measure their BP using the Freescan device. Up to 15 attempts were allowed until 5 valid (no “Error” or “Instability” notification) BP readings were obtained. Then, the Freescan device data were Bluetooth transferred to the myFreescan mobile app and then uploaded to the online PCS in the Maisense website. Holter ECG strips were downloaded and reviewed independently by two experienced physicians (AK and KGK or IA) and disagreement was resolved by an expert cardiologist (AD). The Freescan device results were compared to the ECG at the same time‐points. The study protocol was approved by the hospital scientific committee and participants signed informed consent.
2.5. Sample size calculation
With estimated prevalence of AF around 20%, a minimum sample size of 535 readings (including 107 with AF) would be required to achieve a study power of at least 80% in order to detect a change in sensitivity from 80% to 90% with significance level at 0.05.10 For an average number of four valid readings per subject (five readings with failures 20%), at least 134 subjects of whom 27 with AF need to be included.
2.6. Analysis
Subjects with at least five valid Freescan readings were included. Analysis was performed for (a) individual “readings” and (b) individual “subjects.” “Reading‐to‐reading” analysis of all valid Freescan readings vs the corresponding Holter ECG tracing (assessed 1 minute before, during and 1 minute after each Freescan reading) was performed. The sensitivity, specificity, and accuracy of the Freescan device for AF detection (with exact Clopper‐Pearson confidence intervals [CI]) were determined based on true‐ and false‐positive and true‐ and false‐negative AF Freescan readings (MedCalc Software bvba; https://www.medcalc.org; 2019). “Subjects” analysis was performed by considering AF diagnosis if at least three of five Freescan readings per subject indicated AF. Sensitivity, specificity, and accuracy of the Freescan device for AF detection were determined using the same methodology as for reading‐to‐reading analysis. Both analyses were performed by regarding the “Arrhythmia” notification as AF diagnosis and also as non‐AF.
The Kolmogorov‐Smirnov test was used to assess normality of continuous variables. Mann‐Whitney test was used for comparing two independent groups. Chi‐squared test was used to compare categorical variables. Statistical analysis was performed using the IBM SPSS Statistics 25 (SPSS Inc) software. A P value <.05 was considered statistically significant. Results are expressed as mean ± standard deviation (SD).
3. RESULTS
3.1. Participant's characteristics
A total of 163 subjects were screened and two with SR were excluded (one due to age criterion and one due to technical issue of the Holter device). One subject aged 54 years with sustained AF was included. Thus, data from 161 subjects providing 1486 Freescan measurements were considered for analysis. Readings with device notification “Instability” (29%) and those with “Error” (20%) were discarded. A total of 25 subjects were excluded due to inability to obtain five valid readings. Thus, data of 136 subjects with five valid Freescan BP measurements were analyzed (age 73.8 ± 7.1 years, males 63%, treated hypertensives 88%, AF in ECG 21%; Table 1). Participants who were excluded had more readings (14.8 vs 8.2 per subject), were more frequently females (63% vs 36%), had higher office BP (139 vs 132 mm Hg) and lower heart rate (71 vs 60 bpm) than those analyzed (Table 2).
Table 1.
Participants' characteristics
| Variable |
Non‐AF subjects (n = 108) |
AF subjects (n = 28) |
All (n = 136) |
|---|---|---|---|
| N of measurements (total) | 870 | 247 | 1117 |
| N of valid measurements analyzed | 540 | 140 | 680 |
| Age (y)* | 72.9 ± 6.4 | 77.0 ± 8.9 | 73.8 ± 7.1 |
| Body mass index (kg/m2) | 27.9 ± 4.2 | 29.1 ± 3.6 | 28.2 ± 4.1 |
| Males (%) | 64 (59) | 22 (79) | 86 (63) |
| Wrist circumference (cm) | 17.8 ± 1.6 | 18.4 ± 1.5 | 17.9 ± 1.6 |
| Antihypertensive treatment (%) | 95 (88) | 25 (89) | 120 (88) |
| Office systolic BP (mm Hg) | 131.4 ± 16.2 | 126.5 ± 16.9 | 130.4 ± 16.4 |
| Office diastolic BP (mm Hg) | 73.9 ± 10.9 | 77.6 ± 11.8 | 74.6 ± 11.2 |
| Office pulse rate (b.p.m.)* | 69.2 ± 9.7 | 78.1 ± 17.0 | 71.0 ± 12.0 |
Abbreviations: AF, atrial fibrillation; BP, blood pressure.
P < .05 for comparisons among groups.
Table 2.
Characteristics of subjects included in the analysis vs those excluded due to repeated readings with “Error” or “Instability” notification
| Variable | Analyzed subjects | Excluded subjects | P |
|---|---|---|---|
| N of subjects | 136 | 25 | ‐ |
| N of measurements (total) | 1,117 | 369 | <.01 |
| N of measurements per subject | 8.2 ± 3.2 | 14.8 ± 1.7 | <.01 |
| Subjects with AF (%) | 28 (21) | 3 (12) | NS |
| Age (y) | 73.8 ± 7.1 | 72.7 ± 5.7 | NS |
| Body mass index (kg/m2) | 28.2 ± 4.1 | 28.9 ± 2.7 | NS |
| Males (%) | 86 (63) | 9 (36) | 0.01 |
| Wrist circumference (cm) | 17.9 ± 1.6 | 17.4 ± 1.4 | NS |
| Antihypertensive treatment (%) | 120 (88) | 23 (92) | NS |
| Office systolic BP (mm Hg) | 130.4 ± 16.4 | 139.2 ± 15.7 | <.01 |
| Office diastolic BP (mm Hg) | 74.6 ± 11.2 | 75.1 ± 8.6 | NS |
| Office pulse rate (b.p.m.) | 71.0 ± 12.0 | 60.2 ± 7.6 | <.01 |
Abbreviations: AF, atrial fibrillation; BP, blood pressure.
3.2. Reading‐to‐reading analysis
Analysis of 680 valid measurements showed specificity 99%, sensitivity 67%, and diagnostic accuracy 93% for AF diagnosis, by considering “Arrhythmia” display as “non‐AF” display. In 51% of readings with “Arrhythmia” display, the ECG documented AF. When “Arrhythmia” display was considered as “AF,” the specificity, sensitivity, and diagnostic accuracy for AF diagnosis were 93%, 96%, and 93%, respectively (Figure 2).
Figure 2.
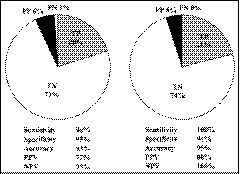
Readings' analysis (left panel): diagnostic accuracy of valid Freescan readings in detecting atrial fibrillation. Subjects' analysis (right panel): diagnostic accuracy of the Freescan device in detecting atrial fibrillation by considering positive diagnosis if at least three of five readings indicate atrial fibrillation. PPV, positive predictive value; NPV, negative predictive value
3.3. Subjects' analysis
Analysis of 136 subjects with five valid Freescan measurements and by considering AF diagnosis if at least three of five Freescan readings indicated AF, showed specificity 100%, sensitivity 75%, and diagnostic accuracy 95% for AF diagnosis. In this analysis, “Arrhythmia” display was considered as “non‐AF.” When “Arrhythmia” display was considered as “AF,” then the specificity, sensitivity, and diagnostic accuracy for AF diagnosis were 94%, 100%, and 95%, respectively (Figure 2).
4. DISCUSSION
There is increasing interest in the development of novel portable devices able to detect AF.3, 11, 12 AF detection algorithms can be efficiently incorporated in BP measuring devices and this novel technology facilitates the early detection of asymptomatic AF during routine BP measurement in the elderly.3, 11
This study assessed the diagnostic accuracy of a novel pocket‐size cuffless BP monitor for AF screening during routine self‐measurement of BP in the elderly. Overall, the device appeared to have satisfactory accuracy as a screening method for AF detection with high specificity and sensitivity. The sensitivity was further improved when the “Arrhythmia” display was considered as “AF.”
The Freescan device is a cuffless BP monitor which has been validated for BP measurement accuracy in static conditions shortly after individual BP calibration.5 The incorporated algorithm for AF detection is a new feature which might be useful for screening in the elderly. The sensitivity and specificity for AF detection were satisfactory for both readings' and subjects' analyses. However, the optimal sensitivity and specificity were obtained when (a) “Arrhythmia” display was regarded as “AF,” and (b) AF diagnosis was based on at least three out of five consecutive readings. It should be noted that the Freescan device provides a 10‐sec single‐lead ECG strip available for review on the online PCS website (Figure 3). The high diagnostic accuracy of the Freescan device together with its portable pocket‐size design allowing assessments at multiple time‐points and in different settings, might render this device an effective and practical screening tool.
Figure 3.
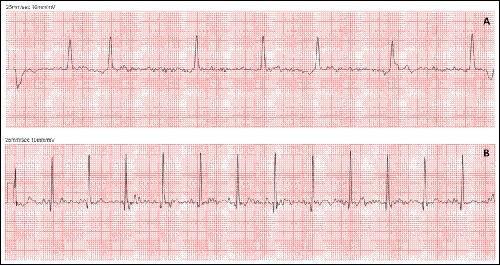
Ten‐sec single‐lead ECG strip provided by the Freescan device during blood pressure measurement and available for review in the Patient Care System (PCS, Maisense website). A; atrial fibrillation, B; sinus rhythm
This study included elderly subjects who are the target population recommended for asymptomatic AF screening.1 In this population, 20% of the Freescan readings gave Error notification and 29% Instability notification. Possible reasons might be either device‐related (embedded electrodes or force sensor) or subject‐related (anatomic or hemodynamic characteristics). In a previous validation study of the test device,5 its performance was considerably better, yet in younger individuals. Analysis of excluded subjects (<5 valid readings) did not reveal age, AF, or wrist circumference as a possible factor influencing the performance of the device, yet the exclusion rate was almost two‐fold more common in women. Further technological development is required to improve the device performance, particularly in elderly women.
Guidelines define an AF episode if its duration is at least 30 seconds documented by ECG monitoring or intracardiac electrogram monitoring, or if <30 seconds, is present throughout the ECG monitoring tracing.13 Since a Freescan reading is usually obtained within 10 seconds (embedded ECG of 10 seconds), this study used the rule ≥3 of 5 AF Freescan readings for defining AF. This “majority rule” has been used in previous studies with automated BP devices with AF detection algorithm and has been shown to decrease false‐positive findings.3 Given the time required to obtain a single Freescan reading (10 seconds) and the “Instability” and “Error” indication issues, requiring five valid readings appeared to be a reasonable approach taking into account the device performance and the need of practical clinical application. When the first three readings indicate AF, no more readings are needed and an AF diagnosis can be made with high accuracy.
The diagnostic accuracy of the Freescan device in detecting AF appears to be comparable to that of upper‐arm automated oscillometric BP monitors equipped with AF detection algorithm.3 In a previous meta‐analysis, the pooled sensitivity, specificity, and accuracy of such devices was 95%, 94%, and 94%, respectively, which are comparable to the findings of this study.3 The Freescan device has the additional advantage of pocket size, which allows for multiple readings in different settings. Moreover, when compared with other technologies developed for AF detection, including mobile applications, wrist‐worn wearables, and other devices, the diagnostic accuracy for AF detection was similar.12
In conclusion, the Freescan device appeared to have high sensitivity and specificity in detecting AF during routine cuffless BP measurement in the elderly, especially when at least five valid readings are obtained and at least three of them indicate “AF” and/or “Arrhythmia.” Further technological development is desirable to improve the performance of the device in obtaining valid measurements.
CONFLICT OF INTEREST
GSS received consultation fees by Maisense for the development of blood pressure measurement technology. For other authors nothing to declare.
AUTHOR CONTRIBUTIONS
Konstantinos G. Kyriakoulis, MD, Anastasios Kollias, MD, PhD, and George S. Stergiou, MD, PhD, FRCP involved in study conception and design; acquisition of data; analysis and interpretation of data; drafting of manuscript; and critical revision. Ioannis Anagnostopoulos, MD, Areti Gravvani, MD, Petros Kalogeropoulos, MD, and Antonios Destounis, MD, PhD, involved in acquisition of data; analysis and interpretation of data; and critical revision.
Kyriakoulis KG, Kollias A, Anagnostopoulos I, et al. Diagnostic accuracy of a novel cuffless self‐blood pressure monitor for atrial fibrillation screening in the elderly. J Clin Hypertens. 2019;21:1797–1802. 10.1111/jch.13730
Funding information
The study was funded by Maisense, Taiwan through the University of Athens Special Account for Research Grants.
REFERENCES
- 1. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893‐2962. [DOI] [PubMed] [Google Scholar]
- 2. Manolis AJ, Rosei EA, Coca A, et al. Hypertension and atrial fibrillation: diagnostic approach, prevention and treatment. Position paper of the working group 'hypertension arrhythmias and thrombosis' of the european society of hypertension. J Hypertens. 2012;30:239‐252. [DOI] [PubMed] [Google Scholar]
- 3. Stergiou GS, Kyriakoulis KG, Stambolliu E, et al. Blood pressure measurement in atrial fibrillation: review and meta‐analysis of evidence on accuracy and clinical relevance. J Hypertens. 2019;37(12):2430‐2441; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4. National Institute for Health and Care Excellence . WatchBP home A for opportunistically detecting atrial fibrillation during diagnosis and monitoring of hypertension. 2013. https://www.nice.org.uk/guidance/MTG13. Accessed July 23, 2019 .
- 5. Boubouchairopoulou N, Kollias A, Chiu B, et al. A novel cuffless device for self‐measurement of blood pressure: concept, performance and clinical validation. J Hum Hypertens. 2017;31:479‐482. [DOI] [PubMed] [Google Scholar]
- 6. Dash S, Chon KH, Lu S, Raeder EA. Automatic real time detection of atrial fibrillation. Ann Biomed Eng. 2009;37:1701‐1709. [DOI] [PubMed] [Google Scholar]
- 7. Moody GB, Mark RG. A new method for detecting atrial fibrillation using R‐R intervals. Comput Cardiol. 1983;10:227‐230. [Google Scholar]
- 8. Xiong P, Wang H, Liu M, Zhou S, Hou Z, Liu X. ECG signal enhancement based on improved denoising auto‐encoder. Eng Appl Artif Intell. 2016;52:194‐202. [Google Scholar]
- 9. Xiong Z, Stiles MK, Zhao J. Robust ECG signal classification for detection of atrial fibrillation using a novel neural network. Computing in Cardiology. 2017;44:1‐4. [Google Scholar]
- 10. Bujang MA, Adnan TH. Requirements for minimum sample size for sensitivity and specificity analysis. J Clin Diagn Res. 2016;10:YE01‐YE06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kollias A, Destounis A, Kalogeropoulos P, Kyriakoulis KG, Ntineri A, Stergiou GS. Atrial fibrillation detection during 24‐hour ambulatory blood pressure monitoring: comparison with 24‐hour electrocardiography. Hypertension. 2018;72:110‐111. [DOI] [PubMed] [Google Scholar]
- 12. Giebel GD, Gissel C. Accuracy of mHealth devices for atrial fibrillation screening: systematic review. JMIR Mhealth Uhealth. 2019;7:e13641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/ SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Europace. 2018;20:157‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]


