Abstract
Recently, the 2017 ACC/AHA released new hypertension guidelines and proposed a redefinition of hypertension from 140/90 to 130/80 mm Hg. This study assesses the impact of the lower threshold for hypertension diagnosis on the association of hypertension with target organ damage (TOD). Health checks were conducted in a community‐dwelling population in Shanghai in 2017 (N = 10 826; 43.26% mean, age 62 ± 12 years [range 29‐95 years]). Subclinical TOD indices were quantified in terms of left ventricular hypertrophy (LVH) by electrocardiogram (Sokolow‐Lyon standard), estimated glomerular filtration rate (eGFR), and presence of proteinuria. Information on clinical TOD was obtained by questionnaire. Arteriosclerotic cardiovascular disease (ASCVD) was determined by the 2013 ACC/ AHA recommended guidelines. Compared to the higher threshold (140/90 mm Hg), the lower threshold (130/80 mm Hg) was associated with variable rates of increased detection of hypertension and TOD: (a) Hypertension: incidence of hypertension, 29.5% (51.8%‐81.5%) increase in persons with hypertension if the threshold of 130/80 mm Hg is used; (b) Subclinical TOD: LVH, 20.8%; eGFR (30‐60 mL/min per 1.73 m2), 23.7%; proteinuria, 23.5%; (c) Clinical TOD: chronic kidney disease (CKD) IV (eGFR<30 mL/min per 1.73 m2), 3.1%; diabetes (fasting glucose ≥7.0 mmol/L or HbA1C>7.0%), 24.3%; stroke, 26.4%; chronic heart disease, 28.1%; acute myocardial infarction, 19.5% (69.4% to 88.9% of total of 36); ASCVD ≥10%, 29.3%. The lower threshold was associated with a significantly higher detection rate of clinical and subclinical TOD of approximately 20% compared to the higher threshold. 15%‐20% of TOD and 29% of ASCVD were also found below the lower threshold of hypertension.
Keywords: arteriosclerotic cardiovascular disease (ASCVD), high threshold of hypertension, low threshold of hypertension, new hypertension guidelines, target organ damage
1. INTRODUCTION
Hypertension, as the most important cause of global disease burden,1 leads to damage of crucial organs, such as heart, brain, and kidney. Recently, new guidelines for management of hypertension were released by the American College of Cardiology (ACC) and the American Heart Association (AHA), proposing lower treatment thresholds than those recommended in previous guidelines.2 Compared to thresholds of systolic blood pressure of 140 mm Hg or diastolic blood pressure of 90 mm Hg suggested by previous guidelines,3 new guidelines define hypertension as a systolic blood pressure of 130 mm Hg or above or a diastolic blood pressure of 80 mm Hg or above.2
The change to a lower threshold (130/80 mm Hg) was supported by evidence from publications including SPRINT (Systolic Blood Pressure Intervention Trial) and The Lancet 2016 meta‐analysis of randomized controlled trials of antihypertensive medications.4, 5 Evidence from SPRINT demonstrated that in higher risk patients without diabetes, treating hypertension to a more intensive target (<120/80 mm Hg) significantly reduced incident cardiovascular events, compared to standard treatment targets (<140/90 mm Hg).4 The Lancet meta‐analysis showed that, among people with a baseline systolic blood pressure of ≥130 mm Hg, a blood pressure reduction of about 25% was beneficial in preventing cardiovascular events, especially stroke and heart failure.5
This dramatic change has been a worldwide concern with potential global impact.6, 7, 8, 9, 10 According to the lower blood pressure threshold of 130/80 mm Hg, the prevalence of hypertension or uncontrolled hypertension in Asian countries will significantly increase by 25%‐50%.6, 10 The intensity of antihypertensive treatment may be increased for stricter blood pressure control, theoretically leading to increasing cost for medication and care by health professionals. However, treating early and intensively, in line with the life course approach proposed by the Lancet Hypertension Commission in 2016,11 may prevent the development of resistant hypertension, reduce blood pressure‐related morbidity and mortality, and lower healthcare costs in a long‐term prospect, especially in Asians whose blood pressure‐related cardiovascular disease are more common than Westerners.12 We sought to examine the possible implications of the new definition of hypertension for hypertension management in Chinese communities.
2. METHODS
A total of 10,826 participants (age 29‐95 years) from a community in Shanghai were enrolled for health checks in 2017. All the participants in the population surveyed were of Asian ancestry. Medical history collection, physical examination, blood examination, and questionnaire survey were performed.
2.1. Medical history collection
Investigators conducted surveys on participants at the survey site. A standardized epidemiological survey questionnaire was adopted. Data collected included demographic data, medical history, history of smoking, and drinking of alcohol. All survey correspondents were trained in the same questionnaire skills.
2.2. Physical examination
All the subjects received detailed physical examination by trained physicians, including physical measurement (height, weight, heart rate) and resting systolic and diastolic blood pressure measurement. Height was accurate to 0.1 cm; weight was accurate to 0.1 kg. Body mass index (BMI) was calculated as BMI = weight/height2 (kg/m2).
After sitting quietly for 5 minutes, blood pressure was measured once in the non‐dominant arm of each subject by the surveyor using OMRON Model 1 Plus (Japan). All medical examiners receive unified training.
2.3. Serological detection
Biochemical indicators include fasting blood glucose (FPG), glycosylated hemoglobin (HbA1C), serum creatinine (Scr), estimated glomerular filtration rate (eGFR), total cholesterol (TC), triglycerides (TG), low‐density lipoprotein cholesterol (LDL‐C), and high‐density lipoprotein cholesterol (HDL‐C).
Blood glucose level was measured by glucose kinase method. HbA1C was measured by high‐performance liquid chromatography (Bio‐Rad, USA). Blood lipids, including TG, total cholesterol, LDL‐C and HDL‐C, were measured by Beckman CX7 biochemical automatic analyzer.
2.4. Diagnostic criteria
Subclinical TOD indices were quantified in terms of left ventricular hypertrophy (LVH) by electrocardiogram (Sokolow‐Lyon standard), decreased eGFR (30‐60 mL/min per 1.73 m2), and presence of proteinuria.
For clinical TOD, chronic kidney disease (CKD) IV was defined as eGFR<30 mL/min per 1.73 m2, and diabetes as fasting glucose ≥7.0 mmol/L or HbA1C>7.0% or application of any hypoglycemic agent; medical history of stroke, coronary heart disease (CAD), and acute myocardial infarction (AMI) was obtained by questionnaire.
2.5. Arteriosclerotic cardiovascular disease
The risk of cardiovascular disease was assessed using the first severe arteriosclerotic cardiovascular disease (ASCVD) event risk assessment method in 10 years as per recommended by the 2013 ACC/ AHA Guidelines.13The method is mainly used to predict the possibility of the first serious ASCVD event in adults aged 40‐79 years, which contains information on age, sex, total cholesterol, HDL‐C, systolic blood pressure, and smoking history. ASCVD risk in the AHA/ACC hypertension guidelines was defined as ≥10%.13
We used the two thresholds to screen the same population for hypertension and TOD separately and compared the difference of the results using a one‐tailed, one‐sample z test for proportions. Independent t test was used to compare demographic characteristics between male and female (SPSS 24.0). Significance level was set at 0.05.
The study was approved by the ethics committee of Ruijin hospital North affiliated to the Medical College of Shanghai Jiaotong University. All subjects signed a written informed consent.
3. RESULTS
A total of 10 826 subjects were enrolled (4683 men and 6143 women) for analysis. The mean age of the study population was 62 ± 12 years. The main demographic characteristics of the study population are shown in Table 1.
Table 1.
General characteristics of male and female subjects
| Total | Male | Female | P value | |
|---|---|---|---|---|
| N | 10826 | 4683 | 6143 | |
| Age (Y) | 62.23±12.02 | 62.97±11.81 | 61.67±12.14 | <.001 |
| Height (cm) | 159.76±8.58 | 166.23±6.68 | 154.83±6.26 | <.001 |
| Weight (kg) | 62.91±10.63 | 68.69±10.14 | 58.50±8.71 | <.001 |
| BMI (kg/m2) | 24.59±3.35 | 24.84±3.27 | 24.41±3.41 | <.001 |
| SBP (mm Hg) | 136.43±19.63 | 137.16±18.74 | 135.87±20.27 | .001 |
| DBP (mm Hg) | 85.55±10.38 | 87.57±10.54 | 84.01±9.99 | <.001 |
| PP (mm Hg) | 50.88±16.03 | 49.59±14.87 | 51.86±16.79 | <.001 |
| HR (bpm) | 73.98±11.34 | 71.74±11.31 | 75.68±11.06 | <.001 |
| Hb (g/L) | 137.42±14.65 | 147.59±12.11 | 129.71±11.34 | <.001 |
| FDG (mmol/L) | 5.36±1.59 | 5.43±1.66 | 5.30±1.52 | <.001 |
| HbA1c (%) | 5.79±0.97 | 5.83±1.03 | 5.76±0.91 | .001 |
| Cr (mmol/L) | 71.76±20.96 | 82.29±18.73 | 63.73±18.92 | <.001 |
| eGFR(mL/min/1.73 m2) | 87.92±15.99 | 86.44±15.22 | 89.05±16.47 | <.001 |
| TC (mmol/L) | 5.01±0.99 | 4.79±0.94 | 5.18±0.99 | <.001 |
| TG (mmol/L) | 1.63±1.23 | 1.66±1.28 | 1.61±1.19 | .023 |
| HDL (mmol/L) | 1.40±0.36 | 1.29±0.33 | 1.48±0.36 | <.001 |
P value: male vs. female comparison.
Abbreviations: BMI, body mass index; Cr, serum creatinine; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; FDG, fasting blood glucose; Hb, hemoglobin; HbAlc, glycosylated hemoglobin; HDL, high‐density lipoprotein cholesterol; HR, heart rate; LDL, low‐density lipoprotein cholesterol; PP, pulse pressure; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides.
As shown in Table 2 and Figure 1, 8821 participants (81.5% of the whole cohort) were diagnosed with hypertension by the lower threshold (130/80 mm Hg), compared to 5607 (52%) by the higher threshold (140/90 mm Hg), with an increase of 29.5%.
Table 2.
Subclinical and clinical TOD between lower threshold (130/80 mm Hg) and higher threshold (140/90 mm Hg) of hypertension diagnosis
| Total | BP≥130/80 mm Hg | BP≥140/90 mm Hg | Detection increased (%) | |
|---|---|---|---|---|
| Blood Pressure | 10826 | 8821 | 5607 | 29.7† |
| LVH | 684 | 591 | 449 | 20.8† |
| Urine protein | 285 | 262 | 195 | 23.5† |
| Diabetic (G≥7.0 /HbA1c>7.0%) | 1107 | 994 | 725 | 24.3† |
| CKD (eGFR<60 mL/min/1.73 m2) | 585 | 491 | 359 | 22.6† |
| CAD | 394 | 328 | 217 | 28.1† |
| STROKE | 349 | 289 | 197 | 26.4† |
| AMI | 36 | 32 | 25 | 19.5* |
| ASCVD≥10% | 4922 | 4453 | 3010 | 29.3† |
Abbreviations: AMI, acute myocardial infarction; ASCVD, arteriosclerotic cardiovascular disease; CAD, coronary heart disease; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; LVH, left ventricular hypertrophy; TOD, target organ damage.
P < .010.
P < .0001.
Figure 1.
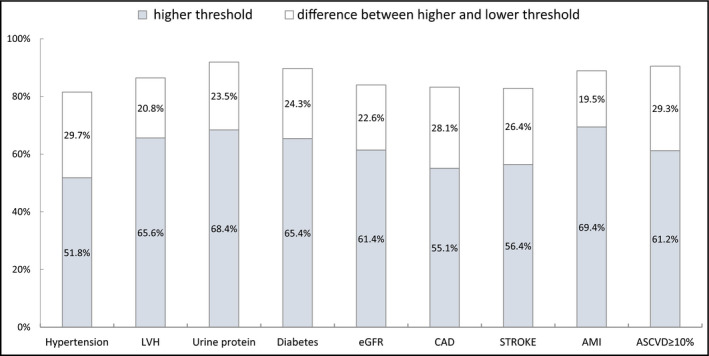
The impact of the lower threshold (130/80 mm Hg) of hypertension diagnosis on the association of hypertension with target organ damage compared to the higher threshold (140/90 mm Hg). LVH, left ventricular hypertrophy; eGFR, estimated glomerular filtration rate; CAD, coronary heart disease; AMI, acute myocardial infarction; ASCVD, Arteriosclerotic cardiovascular disease
For subclinical TOD, the rates of detection for LVH, decreased eGFR (30‐60 mL/min per 1.73 m2) and presence of proteinuria increased by 20.8% (65.6% to 86.4% of total of 684), 23.7% (60.9% to 84.6% of total of 553), and 23.5% (65.6% to 86.4% of total of 553), respectively, in relation to the higher threshold (Table 2).
Similar rates of increase were found in screening for clinical TOD such as CKD IV (by 3.1%; 68.8% to 71.9% of total of 32), diabetes (by 24.3%; 65.5% to 89.8% of total of 1107), stroke (by 26.4%; 56.4% to 82.8% of total of 349), CAD (by 28.1%; 55.1% to 83.2% of total of 394), and AMI (by 19.5%; 69.4% to 88.9% of total of 36) (Table 2).
ASCVD ≥10%, which designates a 10‐year high risk of cardiovascular disease, was found in 4922 patients by the lower threshold, with an increase of 29.3% compared to the 3010 by the high threshold. From results shown in Table 2, an average of 80% of the extra patients included using the lower threshold were detected with TOD and 90% with ASCVD ≥10%. In addition, in a general population, the increase was 13.3% for the patients requiring therapy at high risk to 130/80 mm Hg, while 16.5% increased for the patients not requiring therapy at low risk to 130/80 mm Hg, respectively. The prevalence of two systolic/diastolic blood pressure thresholds has been estimated in Table 3. If we apply the lower threshold (130/80 mm Hg) to the population compared to the higher threshold (140/90 mm Hg), the prevalence of hypertension increased 19%‐39% across the age range.
Table 3.
Prevalence of hypertension based on lower threshold (130/80 mm Hg) and higher threshold (140/90 mm Hg)
| Sex | BP≥130/80 mm Hg | BP≥140/80 mm Hg | Detection increased (%) | |||
|---|---|---|---|---|---|---|
|
Male (n=3999) |
Female (n=4822) |
Male (n=2603) |
Female (n=3004) |
Male 29.8%† |
Female 29.6%† |
|
| 29‐44 | 431 | 458 | 249 | 164 | 34.1%† | 37.4%† |
| 45‐54 | 381 | 568 | 218 | 255 | 36.2%† | 39.2%† |
| 55‐64 | 981 | 1269 | 625 | 783 | 31.6%† | 31.1%† |
| 65‐74 | 1724 | 1909 | 1163 | 1319 | 27.8%† | 25.8%† |
| ≥75 | 482 | 618 | 348 | 483 | 24.0%† | 19.0%† |
P < .0001.
4. DISCUSSION
In this study, compared to the higher threshold of 140/90 mm Hg, the lower threshold of 130/80 mm Hg led to a significant rise of prevalence of hypertension along with higher rates of detection for patients with clinical, subclinical TOD, or high 10‐year ASCVD risk. Some 15%‐20% of TOD was still detected below the lower threshold of hypertension in the same cohort.
The concept of pre‐hypertension, defined as systolic blood pressure of 120‐139 mm Hg or diastolic blood pressure of 80‐89 mm Hg, has been removed from the 2017 guidelines and replaced by the new hypertension definition.2 In our study, pre‐hypertension population with high range of systolic blood pressure (130‐139/80‐89 mm Hg) seemed to be associated with the differences in screening results between the two groups. There have been many studies14, 15, 16, 17, 18, 19, 20, 21 on the correlation between pre‐hypertension and all types of TOD.
The new guidelines2 do not consider asymptomatic organ damage such as LVH or increased urinary protein excretion, whose detection could be important for cardiovascular risk assessment and may even lead to corresponding treatments. Previous studies showed that individuals with LVH had higher risks of CV and all‐cause mortality,22, 23, 24, 25 and pre‐hypertension was found to be an independent risk factor for unfavorable left ventricular functional and structural changes.14, 15, 16, 17 It is also an independent predictor of decreased eGFR in the general population, especially in the elderly.20 Our study showed that the lower threshold significantly raised the detection rates of LVH, decreased eGFR, and presence of proteinuria, in which case antihypertensive treatments targeted at regression or prevention of the subclinical TOD could be started at an earlier stage and may improve prognosis.
For clinical TOD, meta‐analysis showed that pre‐hypertension was associated with increased risk of CAD even at a low range19 and was associated with incident stroke mainly at higher values within the prehypertensive range (systolic blood pressure of 130‐139 mm Hg or diastolic blood pressure of 85‐89 mm Hg).18 In our study, the pre‐hypertension population had higher relative detection rates for CAD, AMI, and stroke by 28.1%, 19.5%, and 26.4%, respectively, which may reflect their potential relationships. According to another meta‐analysis, pre‐hypertension was also considered a potential cause of CKD,21 with gender and ethnic differences, but we only found a relatively small difference between the screening results of CKD (3.1%), perhaps due to the small sample size.
In addition, we found that there was still 15%‐20% of TOD below the lower threshold, which may be related to age, diabetes, hyperlipidemia, and other risk factors.
The lower threshold of hypertension also led to a higher detection rate for those with high 10‐years risk of ASCVD (≥10%). This suggests that these individuals may need to have blood pressure monitoring or TOD screening more frequently and commence antihypertensive treatment if necessary, as recommended by the new guidelines.2 This would lead to cost elevation for social medical care.
The new guidelines, especially the new definition of hypertension, have caused great response and heated discussion internationally. Different countries published their own understanding of the new guidelines and analyzed their possible impact according to their own national conditions.6, 7, 8, 9, 10 However, the current Chinese guidelines are unlikely to be adjusted according to the new threshold,10 as there are concerns of higher priority in management of hypertension in China, especially the low awareness of hypertension.26 Still, as our study showed the new threshold did improve the screening rate for target organ injury in the community, which might eventually be proven beneficial for cardiovascular disease prevention in the long‐term.
This study has some limitations. As a cross‐sectional study, the causal relationship between blood pressure level and various target organ damage could not be confirmed. The sampling method is cluster sampling, so the existence of selection bias cannot be ruled out. Regarding the survey of clinical TOD, we used the questionnaire mode, and it is difficult to determine whether the respondent's answer is true or not. Other risk factors for TOD, such as waist or hip circumference and carotid artery plaques, were not widely collected in this study. We found that the detection rate of various TOD significantly increased after application of the lower threshold of hypertension, but whether the new standard is suitable as a target for hypertension treatment in the Chinese community, more studies are required, and findings should be confirmed by future prospective studies.
5. CONCLUSION
Our study found that the lower threshold of hypertension of 130/80 mm Hg was associated with a significantly higher detection rate of clinical and subclinical TOD of approximately 20% compared to the higher threshold of 140/90 mm Hg. In the same cohort, some 15%‐20% of TOD was also found below the lower threshold of hypertension.
CONFLICT OF INTEREST
The authors declare no conflict of interest in relation to the current study.
AUTHORS CONTRIBUTIONS
Junli Zuo, Shuping Zheng and Alberto Avolio were involved in the conception of the work. Qian Wang, Huijuan Chao, and Shuping Zheng were involved in data curation. Qian Wang, Huijuan Chao, and Junli Zuo were involved in drafting the work. Qian Wang, Huijuan Chao, Shuping Zheng, Isabella Tan, Mark Butlin, and Junli Zuo were involved in formal analysis. Junli Zuo was involved in the final approval of the version to be published. Junli Zuo, Alberto Avolio, Shuping Zheng, Isabella Tan, and Mark Butlin were involved in the whole process of writing, reviewing and editing. Junli Zuo and Alberto Avolio came to an agreement to be accountable for all aspects of the work.
ACKNOWLEDGMENTS
We gratefully acknowledge the invaluable assistance of the physicians of the Department of Geriatric Medicine Ruijin Hospital North, Shanghai Jiaotong University School of Medicine and Jiading District Jiangqiao Community Health Service Center, the study would not have been possible without their support.
Wang Q, Chao H, Zheng S, et al. Impact of new hypertension guidelines on target organ damage screening in a Shanghai community‐dwelling population. J Clin Hypertens. 2019;21:1450–1455. 10.1111/jch.13677
Qian Wang and Huijuan Chao contributed equally to this work.
Funding information
Project Supported by the National Natural Science Foundation of China (Grant No. 81500190) and Shanghai Municipal Commission of Health and Family Planning (Grant No. 201740128; No. 201840087). Shanghai Jiading Science and Technology Committee (JDKW‐2017‐W12).
Contributor Information
Shuping Zheng, Email: 1768748865@qq.com.
Junli Zuo, Email: zuo-junli@163.com.
REFERENCES
- 1. Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Comparative risk assessment collaborating G. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347‐1360. [DOI] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269‐1324. [DOI] [PubMed] [Google Scholar]
- 3. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 4. SPRINRT Research Group , Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta‐analysis. Lancet. 2016;387:957‐967. [DOI] [PubMed] [Google Scholar]
- 6. Kario K. Global impact of 2017 American Heart Association/American College of Cardiology Hypertension Guidelines: a perspective from japan. Circulation. 2018;137:543‐545. [DOI] [PubMed] [Google Scholar]
- 7. Mancia G, Corrao G. Global impact of the 2017 American College Of Cardiology/American Heart Association Hypertension Guidelines: a perspective from Italy. Circulation. 2018;137:889‐890. [DOI] [PubMed] [Google Scholar]
- 8. Schiffrin EL. Global impact of the 2017 American College of Cardiology/American Heart Association Hypertension Guidelines: a perspective from Canada. Circulation. 2018;137:883‐885. [DOI] [PubMed] [Google Scholar]
- 9. Wander GS, Ram CVS. Global impact of 2017 American Heart Association/American College of Cardiology Hypertension Guidelines: a perspective from India. Circulation. 2018;137:549‐550. [DOI] [PubMed] [Google Scholar]
- 10. Wang JG, Liu L. Global impact of 2017 American College Of Cardiology/American Heart Association hypertension Guidelines: a perspective from china. Circulation. 2018;137:546‐548. [DOI] [PubMed] [Google Scholar]
- 11. Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the lancet commission on hypertension. Lancet. 2016;388:2665‐2712. [DOI] [PubMed] [Google Scholar]
- 12. Kario K, Chen CH, Park S, et al. Consensus document on improving hypertension management in Asian patients, taking into account Asian characteristics. Hypertension. 2018;71:375‐382. [DOI] [PubMed] [Google Scholar]
- 13. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College Of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2013;2014(129):S76‐99. [DOI] [PubMed] [Google Scholar]
- 14. Brown DW, Giles WH, Croft JB. Left ventricular hypertrophy as a predictor of coronary heart disease mortality and the effect of hypertension. Am Heart J. 2000;140:848‐856. [DOI] [PubMed] [Google Scholar]
- 15. Sundstrom J, Lind L, Arnlov J, Zethelius B, Andren B, Lithell HO. Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation. 2001;103:2346‐2351. [DOI] [PubMed] [Google Scholar]
- 16. Bella JN, Palmieri V, Roman MJ, et al. Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle‐aged and elderly adults: The strong heart study. Circulation. 2002;105:1928‐1933. [DOI] [PubMed] [Google Scholar]
- 17. Kane GC, Karon BL, Mahoney DW, et al. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856‐863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee M, Saver JL, Chang B, Chang KH, Hao Q, Ovbiagele B. Presence of baseline prehypertension and risk of incident stroke: a meta‐analysis. Neurology. 2011;77:1330‐1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guo X, Zhang X, Guo L, et al. Association between pre‐hypertension and cardiovascular outcomes: a systematic review and meta‐analysis of prospective studies. Curr Hypertens Rep. 2013;15:703‐716. [DOI] [PubMed] [Google Scholar]
- 20. Garofalo C, Borrelli S, Pacilio M, et al. Hypertension and prehypertension and prediction of development of decreased estimated GFR in the general population: a meta‐analysis of cohort studies. Am J Kidney Dis. 2016;67:89‐97. [DOI] [PubMed] [Google Scholar]
- 21. Li Y, Xia P, Xu L, Wang Y, Chen L. A meta‐analysis on prehypertension and chronic kidney disease. PLoS One. 2016;11:e0156575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the strong heart study. Circulation. 2007;115:221‐227. [DOI] [PubMed] [Google Scholar]
- 23. Kim SH, Cho GY, Baik I, et al. Early abnormalities of cardiovascular structure and function in middle‐aged Korean adults with prehypertension: the Korean genome epidemiology study. Am J Hypertens. 2011;24:218‐224. [DOI] [PubMed] [Google Scholar]
- 24. Markus MR, Stritzke J, Lieb W, et al. Implications of persistent prehypertension for ageing‐related changes in left ventricular geometry and function: the monica/kora augsburg study. J Hypertens. 2008;26:2040‐2049. [DOI] [PubMed] [Google Scholar]
- 25. Urbina EM, Khoury PR, McCoy C, Daniels SR, Kimball TR, Dolan LM. Cardiac and vascular consequences of pre‐hypertension in youth. J Clin Hypertens (Greenwich). 2011;13:332‐342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sheng CS, Liu M, Kang YY, et al. Prevalence, awareness, treatment and control of hypertension in elderly chinese. Hypertens Res. 2013;36:824‐828. [DOI] [PubMed] [Google Scholar]


