Abstract
Updated clinical practice guidelines for screening blood pressures in pediatric patients were published in 2017. They differ from the previous guideline, known as the Fourth Report, providing updated population normal values and blood pressure categorization. We hypothesized that the prevalence of abnormal blood pressure in children and adolescents would be higher using the new clinical practice guidelines. We present a cross‐sectional study of screening blood pressure values for children 3 to 18 years of age obtained during well‐child visits at a primary care clinic. All blood pressure values were categorized using both the Fourth Report and the Clinical Practice Guideline. A total of 2635 blood pressure measurements were extracted, and 2600 were eligible for analysis. Using the clinical practice guideline, the prevalence of hypertension increased to 17.85% compared to 9.5% per the Fourth Report (P < 0.0001). Of those patients classified as having a normal blood pressure by the Fourth Report, 12% changed to abnormal when applying the Clinical Practice Guideline. All subgroups had a significant increase in the prevalence of abnormal blood pressure. The most dramatic increase in the prevalence of stage 1 and stage 2 hypertension was seen in six patient subgroups: males, 3‐12 years of age, Hispanic ethnicity, race designated as other, normal weight, and overweight. Applying the new Clinical Practice Guideline increased the prevalence of elevated blood pressure and stage 1 and stage 2 hypertension in children and adolescents, requiring more follow‐up and intervention than previously expected for this patient population.
Keywords: blood pressure, guidelines, pediatric
1. INTRODUCTION
A new clinical practice guideline (CPG) for pediatric hypertension (HTN) was published in 2017, the first since the Fourth Report in 2004, drawing attention to both the importance of diagnosing and treating pediatric HTN as well as the relative paucity of evidence about the topic.1, 2 Though prior studies regarding prevalence have been limited, it has been estimated that 3.6%‐4.5% of children meet criteria for clinical HTN based on the prior guidelines, and one study estimated another 3.4% meet criteria for prehypertension.3, 4 A systematic review showed that childhood blood pressure (BP) is predictive of BP in adulthood, and there is strong evidence in the adult population that HTN leads to increased cardiovascular morbidity and mortality.5, 6 Though the CPG notes that insufficient longitudinal data are available, it is reasonable to extrapolate that pediatric HTN will similarly increase lifelong morbidity and mortality, and available evidence supports this theory.7
In the CPG, the delineating cutoffs for HTN and the BP percentile tables have changed to reflect normal weight children only and to align with new adult HTN guidelines also published in 2017.2, 8 This includes changing BP categorization for everyone 13 years and older to be the same as adult with absolute BP value cutoffs rather than using BP percentiles. With the obesity epidemic there has been evidence of a significant increase in pediatric HTN9, 10 and as the new BP percentiles are based on normal weight children, it seems likely that prevalence in the pediatric population will further increase as these guidelines are adopted. Though National Health and Nutrition Examination Survey (NHANES) data have been used to predict the increase in adults diagnosed with abnormal BPs, limited evidence is available to describe how the new guidelines will impact prevalence of elevated BP and HTN diagnoses throughout childhood.
In this study, we evaluated a cross‐sectional sample of screening BP measurements for patients age 3‐18 years to answer the question of how the CPG will impact prevalence of elevated BP and HTN diagnoses in childhood. Prevalence of prehypertension and stage 1 or stage 2 HTN based on the Fourth Report from 2004 was compared to prevalence of elevated BP and stage 1 or stage 2 HTN based on the 2017 CPG.
2. RESEARCH DESIGN AND METHODS
This cross‐sectional study began with data extraction from the electronic medical record (EMR) for well‐child visits between July and December 2017 at four primary care clinics within the same academic institution. Well‐child visits were identified using ICD‐10‐CM codes Z00.121 and Z00.129, and patients from ages 3 to 18 years were included. The following variables were extracted from the EMR for analysis: patient age, gender, race, ethnicity, height percentile, body mass index (BMI) percentile, first screening BP collected during the well‐child visit, systolic and diastolic BP percentiles, and patients’ systolic and diastolic BP classifications. Data extraction did not include any information on method of BP measurement. Standard protocol for the clinic is to obtain screening oscillometric readings using a device that is validated in pediatrics. Confirmation of abnormal BP values is performed using the ausculatory method. Only the initial BP measurement was extracted for the purposes of this study, because follow‐up measurements were not captured by the EMR in a way that can be queried and extracted without manual chart review. As part of the EMR normal functionality for the clinic, each BP value was assigned to one of the four categories of normal, prehypertension, stage 1 HTN, and stage 2 HTN based on the Fourth Report. Data extraction was performed by medical informatics specialists and exported to a de‐identified Microsoft Excel spreadsheet. The same blood pressure values were used to compare BP classification between the Fourth Report and the CPG. After data extraction, BP values were assigned to one of the four categories of normal, elevated BP, stage 1 HTN, or stage 2 HTN based on the CPG. SAS version 9.4 was used to calculate BP percentiles ≤ 95th percentile. For BP values > 95th percentile, the UpToDate® Calculator: Blood Pressure Percentiles for Boys/Girls 0‐17 Years Old (Wolters Kluwer Health) was used to differentiate stage 1 from stage 2 HTN. When applying the new CPG, blood pressure percentiles were used to categorize BP for children 3‐12 years of age and absolute BP values were used for those 13 years and older as recommended.
Other variables such as age, continuous and categorical variable (3‐12, 13‐18), gender, race (Caucasian, African American, Native American, and other), ethnicity (Hispanic or non‐Hispanic), and weight status (underweight, normal weight, overweight, and obese) were included in the study.
2.1. Statistical methods
Descriptive statistics were calculated for all study variables. Differences in blood pressure percentiles, as measured by the Fourth Report and the updated CPG, were evaluated by paired t test and the Interclass correlation (ICC) and corresponding 95% confidence intervals (95% CI). ICC and 95% CI were calculated based on single rating (k = 2), absolute‐agreement, two‐way mixed effects model. Weighted Cohen’s kappa statistics and 95% CIs were calculated to examine the level of agreement between the Fourth Report and CPG in classifying individuals into different blood pressure categories. Similarly, Bowker’s test of symmetry was used to examine significant classification differences between the two guidelines. Association between change in blood pressure categories and patient characteristics, such as age, gender, and weight status, was evaluated by chi‐square test of independence, and logistic regression analysis was performed to obtain odds ratios (OR) and 95% confidence intervals (95% CI). A level of 0.05 was used for statistical significance. ICC was calculated using SPSS version 24, whereas, all other analyses were performed using SAS version 9.4.
3. RESULTS
A total of 2635 screening blood pressure measurements were extracted. Six cases were excluded because BP values were absent from the data. An additional 29 cases were excluded due to missing information for height or weight. The study sample’s mean age was nine (SD = 4.3) years, 52% male, and 57% white. The majority of patients (76%) were under 13 years of age. Of the 1087 (41%) patients who provided ethnicity, 454 (42%) affirmed Hispanic ethnicity. Fifty‐six percent were at or below normal BMI. Demographic characteristics of the participants are summarized in Table 1.
Table 1.
Characteristics of the study participants (n = 2600)
| Variable | n (%) |
|---|---|
| Age | |
| Median (Min, Max) | 9.00 (3.00,18.00) |
| Gender | |
| Male | 1352 (52.00) |
| Female | 1248 (48.00) |
| Race | |
| White | 1474 (74.71) |
| African American | 350 (17.764) |
| American Indian/Alaska Native | 43 (2.18) |
| Asian | 46 (2.33) |
| Native Hawaiian/Pacific Islander | 4 (0.20) |
| Multiracial | 56 (2.84) |
| Ethnicity | |
| Hispanic | 454 (42.38) |
| Non‐Hispanic | 618 (57.65) |
| BMI | |
| Underweight | 259 (10.03) |
| Normal weight | 1198 (46.38) |
| Overweight | 436 (16.88) |
| Obese | 690 (26.71) |
| Systolic blood pressure (mean ± SD) | 106.29 ± 11.55 |
| Diastolic blood Pressure (mean ± SD) | 65.76 ± 8.35 |
Both systolic and diastolic blood pressure percentiles increased significantly when comparing the CPG to the Fourth Report, as demonstrated in Tables 2 and 3. Table 4 illustrate how the prevalence of abnormal blood pressures changed when applying the CPG. Using the Fourth Report, the prevalence of stage 1 HTN or stage 2 HTN was 9.5%. Using the CPG, the prevalence increased to 17.85%. Overall, approximately 12% of blood pressures changed from normal to abnormal when applying the CPG. The level of agreement between the two guidelines in classifying pediatric patients into different blood pressure categories indicated Kappa statistics of 0.71 (95% CI: 0.69, 0.73). The P‐value for Bowker’s test of symmetry was <0.0001, indicating a significant difference in the prevalence of abnormal blood pressures between the two guidelines.
Table 2.
Systolic and diastolic blood pressure percentiles according to pediatric hypertension guidelines (n = 2600)
| Type of measurement |
Blood pressure percentiles Mean ± SD |
P‐value* | |
|---|---|---|---|
| 2004 Fourth Report | 2017 CPG | ||
| Systolic blood pressure | 65.19 ± 22.96 | 69.33 ± 22.82 | <0.0001 |
| Diastolic blood pressure | 71.34 ± 18.40 | 73.14 ± 19.89 | <0.0001 |
Paired t test was used to evaluate difference between blood pressure percentiles.
Table 3.
Blood pressure categories according to pediatric hypertension guidelines (n = 2600)
| BP categories | Blood pressure | |
|---|---|---|
|
2004 Fourth Report n (%) |
2017 CPG n (%) |
|
| Normal BP | 1935 (74.42) | 1713 (65.88) |
| Elevated BP/ Prehypertension | 418 (16.08) | 423 (16.27) |
| Stage 1 HTN | 223 (8.58) | 417 (16.04) |
| Stage 2 HTN | 24 (0.92) | 47 (1.81) |
Table 4.
Changes in blood pressure categories according to pediatric hypertension guidelines (n = 2600)
| Clinical Practice Guidelines (Updated 2017) | ||||
|---|---|---|---|---|
| Normal BP | Elevated BP | Stage 1 HTN | Stage 2 HTN | |
| Fourth Report (2004) Guidelines | ||||
| Normal BP | 1698 (87.75) | 230 (11.89) | 6 (0.31) | 1 (0.05) |
| Prehypertension | 15 (3.59) | 177 (42.34) | 223 (53.35) | 3 (0.72) |
| Stage 1 HTN | 0 | 16 (7.17) | 188 (84.30) | 19 (8.52) |
| Stage 2 HTN | 0 | 0 | 0 | 24 (100.00) |
Bolded numbers represent patients for whom blood pressure categories stayed the same from the Fourth Report to the Clinical Practice Guideline
Compared to the Fourth Report, the CPG resulted in a statistically significant increase in the prevalence of abnormal blood pressure for each subgroup according to participant characteristics (P < 0.0001). Table 5 illustrates the impact of the CPG by demographic and other characteristics of the patients. Age, gender, and weight status were significantly associated with change in blood pressure categories. Results of the logistic regression analysis showed that the odds of changing blood pressure categories from the Fourth Report to CPG were 1.60 (95% CI: 1.25, 2.05) times more likely among <13 year old compared to 13 years or older and 1.88 (95% CI: 1.54, 2.30) times higher among males compared to females. Similarly, change in blood pressure categories was more likely among overweight and obese pediatric patients than normal weight (OR: 1.40, 95% CI: 1.07, 1.83 and OR: 1.54, 95% CI: 1.22, 1.94, respectively). As shown in Figure 1, the subgroups with the highest prevalence of stage 1 or stage 2 hypertension using the CPG were those whose race was designated as American Indian/Alaska Native (28%) or other (22%), and those who were overweight (20%) or obese (25%). The subgroups with the highest percent increase in stage 1 and stage 2 HTN using the CPG compared to the Fourth Report included male gender (107% increase), ages 3‐12 years (105% increase), Hispanic ethnicity (131% increase), race designated as other (109% increase), normal weight (99%), and overweight status (128% increase). The percent increase in hypertension categorization for each patient subgroup is summarized in Table 5.
Table 5.
Blood pressure categories according to pediatric hypertension guidelines by patient characteristics
| Variable | Normal BP | Elevated | Stage 1 | Stage 2 | Percent increase in HTN from the FR to the CPG | ||||
|---|---|---|---|---|---|---|---|---|---|
| FR | CPG | FR | CPG | FR | CPG | FR | CPG | ||
| n = 1935 (%) | n = 1713 (%) | n = 418 (%) | n = 423 (%) | n = 223 (%) | n = 417 (%) | n = 24 (%) | n = 47 (%) | 88% | |
| Age group | |||||||||
| 3‐12*(n = 1973) | 1531 (77.60) | 1308 (66.29) | 270 (13.68) | 312 (15.81) | 158 (8.01) | 324 (16.42) | 14 (0.71) | 29 (1.47) | 105% |
| 13‐18*(n = 627) | 404 (64.43) | 405 (64.59) | 148 (23.60) | 111 (17.70) | 65 (10.37) | 93 (14.83) | 10 (1.59) | 18 (2.87) | 48% |
| Sex | |||||||||
| Male*(n = 1352) | 977 (72.26) | 829 (61.32) | 246 (18.30) | 256 (18.93) | 118 (8.73) | 239 (17.68) | 11 (0.81) | 28 (2.07) | 107% |
| Female* (n = 1248) | 958 (76.76) | 884 (70.83) | 172 (13.78) | 167 (13.38) | 105 (8.41) | 178 (14.26) | 13 (1.04) | 19 (1.52) | 67% |
| Race | |||||||||
| White * (n = 1474) | 1095 (74.29) | 964 (65.40) | 239 (16.21) | 247 (16.76) | 126 (8.55) | 235 (15.94) | 14 (0.95) | 28 (1.90) | 88% |
| Black * (n = 350) | 263 (75.14) | 230 (65.71) | 53 (15.14) | 65 (18.57) | 30 (8.57) | 48 (13.71) | 4 (1.14) | 7 (2.00) | 62% |
| AI/AN* (n = 43) | 26 (60.47) | 22 (51.16) | 10 (23.26) | 9 (20.93) | 6 (13.95) | 11 (25.58) | 1 (2.33) | 1 (2.33) | 71% |
| Other* (n = 106) | 77 (72.64) | 66 (62.26) | 18 (16.98) | 17 (16.04) | 11 (10.38) | 22 (20.75) | 0 (0) | 1 (0.94) | 109% |
| Ethnicity | |||||||||
| Hispanic* (n = 454) | 342 (75.33) | 297 (65.42) | 77 (16.96) | 76 (16.74) | 33 (7.27) | 73 (16.08) | 2 (0.44) | 8 (1.76) | 131% |
| Non‐Hispanic* (n = 618) | 474 (76.70) | 430 (69.58) | 88 (14.24) | 95 (15.37) | 53 (8.58) | 85 (13.75) | 3 (0.49) | 8 (1.29) | 66% |
| Weight status | |||||||||
| Underweight* (n = 259) | 209 (80.69) | 191 (73.75) | 32 (12.36) | 36 (13.90) | 18 (6.95) | 30 (11.58) | 0 (0) | 2 (0.77) | 78% |
| Normal* (n = 1198) | 955 (79.72) | 853 (71.20) | 158 (13.19) | 176 (14.69) | 81 (6.76) | 156 (13.02) | 4 (0.33) | 13 (1.09) | 99% |
| Overweight* (n = 436) | 308 (70.64) | 270 (61.93) | 89 (20.41) | 77 (17.66) | 37 (8.49) | 85 (19.50) | 2 (0.46) | 4 (0.92) | 128% |
| Obesity* (n = 690) | 451 (65.36) | 387 (56.09) | 134 (19.42) | 133 (19.28) | 87 (12.61) | 142 (20.58) | 18 (2.61) | 28 (4.06) | 62% |
HTN = Stage 1 or Stage 2 hypertension
Using the CPG resulted in significant increases in abnormal blood pressures in each subgroup (Bowker’s test of symmetry, P < 0.0001).
Figure 1.
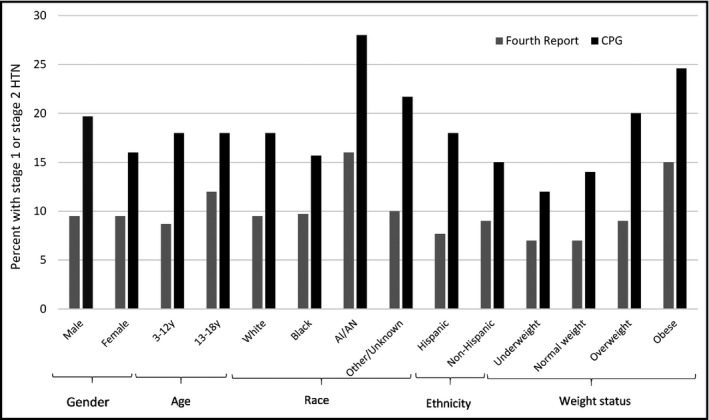
Percent of patients in various patient groups with stage 1 or stage 2 hypertension using the Fourth Report and Clinical Practice Guidelines (CPG)*. *Clinically significant increase for every patient characteristic reported (P < 0.0001). AI = American Indian. AN = Alaska Native
4. DISCUSSION
The results of this study indicate that implementing the new CPG will result in a statistically significant increase in all categories of elevated BP. To our knowledge, this is the first study to compare the impact of utilizing the Fourth Report versus the new CPG for all age groups and patient groups. The increased prevalence of elevated BP and HTN was most pronounced in six subpopulations: males, those under 13 years of age, race designation as other, Hispanic ethnicity, and normal weight and overweight children. This data also show the potential impact on the number of patients in whom pharmacotherapy would be indicated based on classification alone, with nearly double the amount of patients classifying as stage 2 hypertension. Transitioning to the new CPG will affect all ages and demographics.
Compared to other studies, there is a higher than expected proportion of HTN in patients included in this study using either set of guidelines. In the current study, 9.5% of the study participants were hypertensive according to the Fourth Report, compared with the 3.6%‐4.5% estimated nationally.3, 4 Using the CPG, this is again noted with 17.9% of our patients meeting criteria for stage 1 or 2 HTN. Since publication of the CPG, a study by Khoury and colleagues investigated the sensitivity of the CPG for detecting patients with target organ damage in children ages 10‐18 who were also part of a study regarding obesity and diabetes. In that population, a hypertension prevalence of 8% using the Fourth Report and 13% with the CPG was reported.11 A Morbidity and Mortality Weekly Report from the CDC evaluated NHANES participants aged 12‐19 and reported an estimated HTN prevalence of only 1.5% using the Fourth Report which more than doubled to 4.2% using the CPG.12 There has also been a recent study evaluating the performance of the provided simplified screening tables by Yang et al13 which reports a 7.4% prevalence of any elevated BP using NHANES III. The percent change in diagnoses from the 2004 to the 2017 guidelines is also different between these studies and our own. Compared to the CDC estimate, there is an increased prevalence of obesity in our population (26.7% compared to 21.8%) which may help to explain the increased blood pressures in this patient sample.12 Additionally, all blood pressure values used in the current study are for screening purposes and would require confirmatory repeat values before making a diagnosis. If the blood pressure was obtained using improper technique, the screening blood pressure may be falsely elevated.
The updates made to the CPG included removing data from normative tables for children who were overweight and obese, which would expect to result in those above normal weight having an increase in BP prevalence when compared with older guidelines. Further analysis would be needed to explain why those of normal and overweight status were at higher risk than obese status for being classified as stage 1 or stage 2 HTN in the current study. Additionally, the implementation of the CPG changes all children 13 and above to be classified by absolute blood pressure rather than by percentile explaining why changes to the BP percentile categories had less impact on those over 13. It is difficult to make any conclusions based on race or ethnicity in this study given the large number of patients for which these data were unavailable.
One limitation of this study is that it includes single office visit measurements representing the initial screening blood pressure only and does not account for repeat blood pressures that may have been performed. This limitation may also contribute to the increased prevalence of hypertension in our study compared to other estimates. While these screening measurements cannot be used to make a final diagnosis, abnormal values and percentiles necessitate obtaining additional BP measurements during the course of the clinic visit and may indicate the need for further follow‐up. The data were obtained and de‐identified through medical informatics, meaning no information could be verified or missing information recovered. This was particularly a problem with identifying ethnicity as it was not recorded for more than half of the included patients. Other risk factors for HTN such as prematurity or use of certain medications were not included in the data set and could impact the generalizability of this study. The data extracted also included BP decision support from the EMR which was customized by an internal informatics team. These data were found to have some errors in BP classification requiring manual verification and therefore the potential to introduce human error.
Given the significantly increased frequency of abnormal blood pressure readings with CPG implementation, it will be important to develop and improve EMR decision support tools to facilitate implementation. Without these tools, workflow or time to full implementation may be significantly delayed, affecting appropriate follow‐up and treatment of patients with abnormal blood pressures. The option to use the simplified blood pressure table, which only factors in age and gender, is described in the CPG and requires less decision support. However, only utilizing the simplified table provided in the CPG may also increase the need for follow‐up and further evaluation, as it is based on the 5%ile of height. As expected, two studies have shown the simplified table to have high sensitivity but lower specificity leading to a higher false positive rate.13, 14
In conclusion, this review indicates prevalence of elevated blood pressure and hypertension will increase significantly in all populations with implementation of the CPG. This can be expected to lead to more follow‐up, evaluation, and treatment than previously indicated. Recommendations for screening for secondary causes have also changed as essential hypertension, including related to obesity, is increasing in the pediatric population. Future study and follow‐up will be needed to determine the full population impact in terms of follow‐up, screening, and treatment.
CONFLICT OF INTEREST
The authors report no conflicts of interest to disclose.
Condren M, Carter J, Mushtaq N, et al. The impact of new guidelines on the prevalence of hypertension in children: A cross‐sectional evaluation. J Clin Hypertens. 2019;21:510–515. 10.1111/jch.13512
REFERENCES
- 1. Flynn JT, Kaelber DC, Baker‐Smith CM, et al. Practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. [DOI] [PubMed] [Google Scholar]
- 2. Falkner B, Daniels SR. Summary of the fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Hypertension. 2004;44(4):387‐388. [DOI] [PubMed] [Google Scholar]
- 3. Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874‐879. [DOI] [PubMed] [Google Scholar]
- 4. Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school‐aged children. Pediatrics. 2004;113(3 Pt 1):475‐482. [DOI] [PubMed] [Google Scholar]
- 5. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta‐regression analysis. Circulation. 2008;117(25):3171‐3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903‐1913. [DOI] [PubMed] [Google Scholar]
- 7. Theodore RF, Broadbent J, Nagin D, et al. Childhood to early‐midlife systolic blood pressure trajectories: early‐life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66(6):1108‐1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):2199‐2269. [DOI] [PubMed] [Google Scholar]
- 9. Chiolero A, Cachat F, Burnier M, Paccaud F, Bovet P. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. J Hypertens. 2007;25(11):2209‐2217. [DOI] [PubMed] [Google Scholar]
- 10. Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988–2008. Hypertension. 2013;62(2):247‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Khoury M, Khoury PR, Dolan LM, Kimball TR, Urbina EM. Clinical implications of the revised AAP pediatric hypertension guidelines. Pediatrics. 2018;142(2):e20180245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jackson SL, Zhang Z, Wiltz JL, et al. Hypertension Among Youths—United States, 2001–2016. MMWR Morb Mortal Wkly Rep. 2018;67:758‐762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang L, Hou Y, Zhao M, Bovet P, Xi B. Simplified blood pressure tables based on different height percentiles for screening elevated blood pressure in children. J Hypertension. 2019;37(2):292‐296. [DOI] [PubMed] [Google Scholar]
- 14. Stabouli S, Nika T, Kollios K, Antza C, Doundoulakis I, Kotsis V. Performance of simplified tables for high blood pressure screening in a European pediatric population. J Hypertension. 2018;36(1):510‐5. [DOI] [PubMed] [Google Scholar]


