Abstract
The authors developed an equation to estimate 24‐hour urine sodium (24HUNa) using the average of three spot urine (SU) samples (morning‐first, morning, and evening) from 74 individuals and validated this equation using the average of three SU samples (morning‐first, daytime, and evening) from 174 additional individuals. Compared with previously published equations using a single SU sample, the currently developed equation using the average of three SU samples showed much lower bias from measured 24HUNa (−2.9 vs >10 mmol/24 h). The intraclass and concordance correlation coefficients of the proposed equation using the average of three SU samples were 0.909 and 0.832, respectively. The limits of agreement were −64.1–58.3 mmol/24 h and approximately 100 mmol/24 h for the currently developed and previously published equations, respectively. All equations showed a tendency to overestimate or underestimate 24HUNa in a manner dependent on the level of 24HUNa but irrespective of the number of SU samples considered. Nonetheless, among the currently tested equations, our equation using the average of three SU samples provided the best estimation of 24HUNa at a population level.
Excessive sodium intake is associated with high blood pressure (BP) and a greater risk for cardiovascular disease and stroke.1, 2 Thus, reducing sodium intake is important to prevent and treat cardiovascular disease. Moreover, accurate assessment of sodium intake is crucial in the evaluation and management of diseases associated with high sodium intake. Although measurement of 24‐hour urine sodium (24HUNa) is considered the most reliable method,3 24‐hour urine collection is cumbersome in many patients and often results in incomplete samples. For this reason, various equations to estimate 24HUNa from a single spot urine (SU) sample have been suggested by Kawasaki and colleagues,4 Tanaka and colleagues,5 and Brown and colleagues,6 as SU samples are convenient to collect. However, the amount of bias affecting the reported relationship7, 8 between cardiovascular disease and sodium intake estimated on the basis of equations using a single SU sample remains unclear, as validation against measured 24HUNa values revealed that most such equations provide significantly biased estimates of 24HUNa.9, 10, 11 Therefore, when interpreting the association found between high sodium levels and cardiovascular events, the measurement method should always be considered as a potential bias‐inducing factor.12 In our previous study, we suggested that using multiple SU samples to estimate 24HUNa may improve predictive capabilities.9
In the present study, we developed an equation to estimate 24HUNa using the average of three SU samples. We validated the developed equation on a study population different from that used in its development. Finally, we compared the predictive capability of the currently developed equation with that of previously published equations using a single SU sample.
Method
Study Population
For developing our equation for the estimation of 24HUNa using the average of three SU samples, the participants were recruited as described in detail elsewhere.9 The study was designed and performed in 2012 to estimate sodium intake of a general population from four cities by measurement of 24HUNa. Briefly, 502 participants from four cities in Korea (Paju, Seoul, Gyeongju, and Chuncheon) were recruited via the list‐assisted random‐digit‐dial method.13, 14 Three SU samples (morning‐first, morning, and evening), as well as 24‐hour urine samples, were collected from participants from Paju. The total number of participants with three SU samples and valid 24‐hour urine collection was 101 (development group). Only a single SU sample (morning‐first) was collected from the rest of the recruited participants (ie, those from Seoul, Gyeongju, and Chuncheon, as well as the remaining participants from Paju); while this sample was not used for equation development and validation in the present study, it was used in the previous study9 for the validation of previously published equations using a single SU sample.
For the purpose of external validation, 334 additional participants (validation group) from the Seoul and Gyeonggi Province were recruited as part of the 2014 Korea National Health and Nutrition Examination Survey, which is a representative national health survey performed in Korea. To achieve an anticipated intraclass correlation coefficient (ICC) of 0.75 (95% confidence interval width, 0.15) between measured 24HUNa and 24HUNa estimated based on the equation using multiple SU samples, the optimal size of the population for external validation (validation group) was calculated to be 132.15
To confirm that the 24‐hour urine samples were collected appropriately (ie, each sample contained all urine produced over the 24‐hour period), the values of self‐reported urine loss and urinary creatinine levels were considered.9, 14, 16, 17 Specifically, a 24‐hour urine sample was considered inappropriate if: self‐reported urine loss was >100 mL on more than one occasion for participants included in the development group or 50 mL on more than one occasion for participants included in the validation, respectively; or creatinine index was <0.7, calculated as the concentration of 24‐hour urine creatinine (mg/dL) divided by 21 times the body weight (kg). Although 24‐hour urine collection was determined as valid according to the above criteria, the development and validation groups involved only individuals whose 24‐hour urine creatinine excretion (24HUCr) was noted at 85% to 115% of the predicted value of urinary creatinine (PrUCr).4 After applying all sample validation criteria, the final development and validation groups consisted of 74 and 175 participants, respectively.
Hypertension was defined as systolic BP ≥140 mm Hg, diastolic BP ≥90 mm Hg, or current use of antihypertensive medication, with a previous diagnosis of hypertension. BP was measured using the oscillometric method (WatchBP Office; Microlife, Widnau, Switzerland) and the auscultatory method for participants included in the development and validation groups, respectively.
Protocol of Urine Collection
Participants included in the development group were provided with a 3‐L urine collection bag, a 600‐mL plastic beaker, and three 50‐mL BD Falcon tubes (BD, Franklin Lakes, NJ) labeled for urine collection at three points during the day (evening, morning‐first, and morning). The plastic beaker served to collect urine when voiding and to transfer the urine to the urine collection bag. The participants were instructed to discard the first voided urine (typically, urine voided around 9 am), and collect the urine voided during the following 24 hours while maintaining their usual daily routine. Regarding the SU samples, the participants were instructed to collect: 10 mL of evening urine, typically voided between 9 pm and 11 pm; 10 mL of morning‐first urine, collected from the first urine voided on the morning of the second day; and 10 mL of morning urine, typically voided around 9 am of the morning of the second day. The 10‐mL SU samples were separated from the voided urine collected in the plastic beaker and stored in the three 50‐mL Falcon tubes with corresponding labels. The remaining volume of voided urine was added to the urine bag. The participants brought all samples to a clinical trial center, where a 2‐mL aliquot of each SU sample was placed into a 3.6‐mL plastic tube (CryoTube, Nunc, Roskilde, Denmark) and sent to a central laboratory for measurement of sodium and creatinine concentration. The total volume of 24‐hour urine was measured using a mass cylinder after adding the remaining urine from the 50‐mL Falcon tubes into the 3‐L urine bag. The amount of 24‐hour urine sodium and creatinine, respectively, was calculated by multiplying the sodium and creatinine concentration by the volume of the 24‐hour urine.
On the other hand, the participants included in the validation group were provided with the following recipients: two 3‐L urine bags, one for daytime urine collection (from 7 am to 11 pm; total period, 16 hours) and the other for nighttime urine collection (from 11 pm to 7 am of the following morning; total period, 8 hours); a 600‐mL plastic beaker for collection of the voided urine and transfer into the 3‐L bags; and three 50‐mL BD Falcon tubes for collection of SU samples, with labeling referring to the time of collection (daytime, evening, and morning‐first). The participants were instructed to discard the morning‐first urine voided on the first day of the experiment, but to include the morning‐first urine voided on the second day. Regarding the SU samples, the participants were instructed to collect: 10 mL of daytime urine, typically voided between 1 pm and 6 pm; 10 mL of evening urine, typically voided between 9 pm and 11 pm; and 10 mL of morning‐first urine, from the first urine voided on the morning of the second day. The SU samples were collected in the three 50‐mL Falcon tubes and labeled correspondingly. While the protocol of urine collection differed between the development and validation group, all participants were instructed to maintain their usual daily routine during the experiment. At the clinical trial center, aliquots of the daytime and nighttime SU samples were prepared and sent to the central laboratory, where the concentration of sodium and creatinine was measured separately for daytime and nighttime urine. Similarly, the amount of urine sodium and creatinine was calculated separately for daytime and nighttime urine, by multiplying the corresponding concentrations and volumes. The total amount of 24‐hour urine sodium and creatinine was calculated by summing the amounts noted for the daytime urine, nighttime urine, and all SU samples.
The urine samples from the development group were transferred to a central laboratory (Green Cross LabCell, Yongin, Korea), where sodium concentration was measured using an ion‐selective electrode method (Modular DPE chemistry; Roche Diagnostics, Mannheim, Germany), and creatinine level was measured by the Jaffe reaction (Kinetic colorimetric assay, Roche Diagnostics). The urine samples from the validation group were analyzed at another laboratory (Seegene, Seoul, Korea), where sodium concentration was measured using an ion‐selective electrode method (Hitachi 7600 analyzer; Hitachi Co., Tokyo, Japan), and creatinine level was measured by the Jaffe reaction (Kinetic colorimetric assay, Roche Diagnostics). For 149 tested samples, the difference between the measurements reported by the two laboratories was 0.25 ± 2.93 mmol/L (percent difference, 0.64%±3.55%) for urine sodium concentration, and 2.1±3.6 mg/dL (percent difference, 1.92%±2.26%) for urine creatinine concentration.
Equation Development
The equation estimating 24HUNa using the average of three SU samples was developed via a protocol similar to that described in a previous study, and relying on the same hypotheses, namely:4, 9
24HUCr ≈ PrUCr
24‐HUNa/24HUCr ∝ SUNa/SUCr, where SUNa and SUCr represent the SU sodium and creatinine concentrations, respectively.
24‐HUNa ∝ SUNa/SUCr × PrUCr
PrUCr (mg/24 h) was calculated using the equations proposed by Kawasaki and colleagues4: for men, PrUcr = body weight (kg) × 15.1 + height (cm) × 7.4− age (years) × 12.4−80; for women, PrUCr = body weight (kg) × 8.6 + height (cm) × 5.1−age (years) × 4.7−75. These equations were employed because they showed the highest correlation with 24HUCr in a previous study9 and reflect the sex‐specific differences in urine creatinine excretion. The equation for estimating 24HUNa was developed by curve fitting of the measured 24HUNa against the ratio between the average value of three SUNa determinations and the average value of three SUCr determinations, multiplied by PrUCr.
Validation of the Developed Equation
The predictive capability of the developed equation was validated against data from the validation group. Furthermore, the predictive power of the equation using the average of three SU samples was also compared against that of equations using a single SU sample, previously developed by Kawasaki and colleagues,4 Tanaka and colleagues,5 Brown and colleagues (INTERSALT study),6 as well as the quadratic equation previously developed by our group.9
Statistical Analyses
The differences between measured and estimated 24HUNa values were analyzed using the paired t test. The predictive accuracy of each equation was assessed in terms of ICC and concordance correlation coefficient (CCC) between predicted and measured 24HUNa. The Bland‐Altman analysis of agreement was used to estimate the bias and limits of agreement between measured and estimated 24HUNa. The percentage error of limits of agreement was calculated as [1.96 × (standard deviation of the difference between measured and estimated 24HUNa)/(average of measured 24HUNa)] × 100.18 Statistical analyses were performed using MedCalc version 15.8 (MedCalc Software bvba; Ostend, Belgium). Curve fitting was performed using TableCurve 2D version 5.01 (Systat Software Inc., San Jose, CA). Null hypotheses of no difference were rejected if the respective P value was <.05.
Results
Participant Characteristics
The demographic and clinical characteristics of the study population, consisting of the development and validation group, are shown in Table 1. Mean age and prevalence of hypertension were higher in the development group than in the validation group. The 24HUNa and 24HUCr did not differ between the groups. No difference was detected between 24HUCr and PrUCr in either group (P=.145 and P=.869 for the development and validation groups, respectively).
Table 1.
Demographic and Clinical Characteristics of the Study Population
| Variables | Development Group | Validation Group | P Value |
|---|---|---|---|
| No. | 74 | 175 | |
| Age, mean (SD), y | 52.7 (11.0) | 46.2 (12.7) | <.001 |
| Men, No. (%) | 30 (40.5) | 68 (38.9) | .888 |
| Hypertension, No. (%) | 14 (18.9) | 15 (8.6) | .030 |
| Antihypertensive medications, No. (%) | 8 (10.7) | 15 (8.6) | .636 |
| Height, mean (SD), cm | 162.0 (9.8) | 163.2 (8.0) | .297 |
| Weight, mean (SD), kg | 62.0 (9.7) | 61.8 (11.0) | .891 |
| Serum creatinine, mean (SD), mg/dL | 0.78 (0.15) | 0.82 (0.17) | .088 |
| 24‐h urine sodium, mean (SD), mmol/24‐h | 151.6 (61.1) | 161.3 (61.3) | .258 |
| Men | 177.9 (68.6) | 185.8 (61.3) | .572 |
| Women | 133.6 (50.6) | 145.7 (56.2) | .221 |
| 24‐h urine creatinine, mean (SD), mg/24‐h | 1183.4 (312.9) | 1260.0 (363.7) | .095 |
| Men | 1487.7 (252.3) | 1630.8 (298.4) | .024 |
| Women | 975.9 (120.9) | 1024.3 (128.8) | .034 |
| Predicted 24‐h urine creatinine, mean (SD), mg/24‐h | 1201.0 (321.2) | 1258.6 (379.5) | .223 |
| Men | 1514.7 (270.8) | 1658.3 (307.8) | .030 |
| Women | 987.1 (101.2) | 1004.6 (94.0) | .311 |
Data are presented as mean (standard deviation [SD]) or numbers (percentage).
Table 2 shows the diurnal variation in urine sodium excretion and sodium/creatinine ratio. The morning‐first SUNa was lower than morning and evening SUNa in the development group and lower than daytime and evening SUNa in the validation group. As SUCr did not differ with collection time, the sodium/creatinine ratio was lower in the morning‐first SU sample than in the samples collected at other times of the day in both the development and the validation group.
Table 2.
Diurnal Variations in SU Sodium and Creatinine Excretion
| Sodium, mmol/L, mean (SD) | Creatinine, mg/L, mean (SD) | Sodium/Creatinine | |
|---|---|---|---|
| Development population | |||
| Morning‐first SU | 98.4 (43.8)a | 1022.3 (566.0) | 0.116 (0.059)b |
| Morning SU | 116.9 (50.1) | 1158.3 (664.5) | 0.126 (0.070) |
| Evening SU | 130.2 (56.7) | 1166.9 (710.0) | 0.139 (0.078) |
| Validation population | |||
| Morning‐first SU | 102.9 (45.4)c | 1105.5 (637.9) | 0.115 (0.064)d |
| Daytime SU | 115.6 (56.4)e | 1056.1 (653.8) | 0.137 (0.077) |
| Evening SU | 138.4 (59.9) | 1107.8 (578.3) | 0.148 (0.077) |
Data are presented as mean (standard deviation [SD]). a P=.023 vs morning spot urine (SU), P<.001 vs evening SU. b P=.021 vs evening SU. c P=.008 vs daytime SU, P<.001 vs evening SU. d P=.006 vs daytime SU, P<.001 vs evening SU. e P<.001 vs evening SU.
Equation for the Estimation of 24HUNa Using the Average of Three SU Samples
The best fitting curve of the equation using the average of three SU samples was obtained as: estimated 24HUNa = 43.5842 + 0.7855 × [(3SUNa/3SUCr) × PrUCr]−0.00004816 × [(3SUNa/3SUCr) × PrUCr]2, where 3SUNa and 3SUCr represent the sodium concentration (mmol/L) and creatinine concentration (mg/L), respectively, averaged over three SU samples.
Validation of the Developed Equation
The morning‐first SU sample from the validation population was used in the equations previously developed by Kawasaki and colleagues, Tanaka and colleagues, Brown and colleagues (INTERSALT study), and our group (quadratic equation) to estimate 24HUNa based on a single SU sample. The average of three SUNa and SUCr (sodium and creatinine concentrations, respectively, averaged over the morning‐first, daytime, and evening SU samples) from the validation group were used as descriptors in the equation developed in the present study. The 24HUNa estimated using each of the five equations (ie, one developed in the current study and four developed previously) was compared against measured 24HUNa (Table 3). All previously developed equations, which use a single SU sample, provided estimates of 24HUNa that differed significantly from the measured value. On the other hand, the equation developed in the present study, which uses the average of three SU samples, provided estimates of 24HUNa that were similar to the measured 24HUNa (Table 3, P=.120). The bias of the equation using the average of three SU samples was also much less pronounced than the bias of previously published equations (−2.9 vs >10 mmol/24 h). Nevertheless, estimates of 24HUNa correlated significantly with measured 24HUNa for all five equations evaluated. For the equation using the average of three SU samples, the ICC and CCC of the 24HUNa estimates against the measured 24HUNa were 0.909 and 0.832, respectively, indicating high accuracy. The predictive accuracy of the equation using the average of three SU samples persisted in both men and women participants.
Table 3.
Comparison of Measured and Estimated 24‐Hour Urine Sodium
| Equations | Sodium, mmol/24‐h, mean (SD) | Differencea | 95% CI | P Value | Range of Difference | r b | ICCc | CCCd |
|---|---|---|---|---|---|---|---|---|
| All (N=175) | ||||||||
| Kawasakie | 185.3 (49.2) | 24.1 (49.9) | 16.7–31.5 | <.001 | −151.0 to 148.9 | 0.612f | 0.748f | 0.546f |
| Tanakag | 147.0 (30.7) | −14.3 (49.0) | −21.6 to −7.1 | <.001 | −163.4 to 70.3 | 0.610f | 0.656f | 0.468f |
| INTERSALTh | 126.5 (29.2) | −34.8 (50.3) | −42.3 to −27.3 | <.001 | −192.6 to 69.2 | 0.580f | 0.621f | 0.356f |
| Quadratici | 149.2 (41.0) | −12.1 (49.1) | −19.4 to −4.8 | .001 | −156.9 to 114.3 | 0.602f | 0.715f | 0.542f |
| Equation using average of three SU | 158.4 (45.7) | −2.9 (31.2) | −7.5 to 1.7 | .120 | −121.1 to 50.9 | 0.869f | 0.909f | 0.832f |
| Men (n=68) | ||||||||
| Kawasaki | 204.4 (48.7) | 18.6 (52.7) | 5.8–31.4 | .005 | −109.1 to 148.3 | 0.561f | 0.707f | 0.517f |
| Tanaka | 158.9 (29.8) | −26.9 (51.0) | −39.3 to −14.6 | <.001 | −163.4 to 70.3 | 0.560f | 0.611f | 0.380f |
| INTERSALT | 152.0 (26.7) | −33.8 (51.5) | −46.3 to −21.4 | <.001 | −177.7 to 69.2 | 0.556f | 0.579f | 0.323f |
| Quadratic | 164.5 (43.9) | −21.3 (52.0) | −33.9 to −8.7 | .001 | −156.9 to 114.3 | 0.553f | 0.687f | 0.484f |
| Equation using average of three SU | 178.3 (46.6) | −7.5 (30.7) | −14.9 to −0.1 | .048 | −87.3 to 50.9 | 0.873f | 0.914f | 0.833f |
| Women (n=107) | ||||||||
| Kawasaki | 173.2 (45.7) | 27.5 (47.9) | 18.4–36.7 | <.001 | −151.0 to 148.9 | 0.575f | 0.721f | 0.492f |
| Tanaka | 139.4 (28.9) | −6.3 (46.2) | −15.1 to 2.6 | .1618 | −159.8 to 65.8 | 0.573f | 0.635f | 0.461f |
| INTERSALT | 110.2 (16.1) | −35.4 (49.8) | −45.0 to −25.9 | <.001 | −192.6 to 39.8 | 0.516f | 0.429j | 0.199f |
| Quadratic | 139.4 (36.1) | −6.2 (46.4) | −15.1 to 2.7 | .167 | −156.1 to 111.1 | 0.568f | 0.681f | 0.512f |
| Equation using average of three SU | 145.7 (40.6) | 0.04 (31.3) | −6.0 to 6.0 | .990 | −121.1 to 48.0 | 0.839f | 0.886f | 0.796f |
Abbreviations: CCC, concordance correlation coefficient; CI, confidence interval; ICC, intraclass correlation coefficient; SU, spot urine. Data are presented as mean (standard deviation [SD]). aDifference = estimated 24‐hour urine sodium – measured 24‐hour urine sodium, mean (SD). bPearson's correlation coefficient. cIntraclass correlation coefficient. dConcordance correlation coefficient. eEquation proposed by Kawasaki and colleagues.4 f P<.001. gEquation proposed by Tanaka and colleagues.5 hEquation proposed by Brown and colleagues.6 iEquation proposed by Rhee and colleagues.9 j P=.002.
In the Bland‐Altman analysis to determine the difference between measured and estimated 24HUNa, the standard deviation ranged between 49.0 and 50.4 for the previously published equations using a single SU sample, compared with 31.2 for the currently developed equation using the average of three SU samples (Figure). The percentage error of limits of agreement ranged between 59.7% and 61.2% for the previously published equations using a single SU sample, compared with 37.9% for the currently developed equation using the average of three SU samples. Nevertheless, all equations tended to overestimate or underestimate 24HUNa in a manner dependent on the level of 24HUNa and irrespective of the number of SU samples used (Figure).
Figure 1.
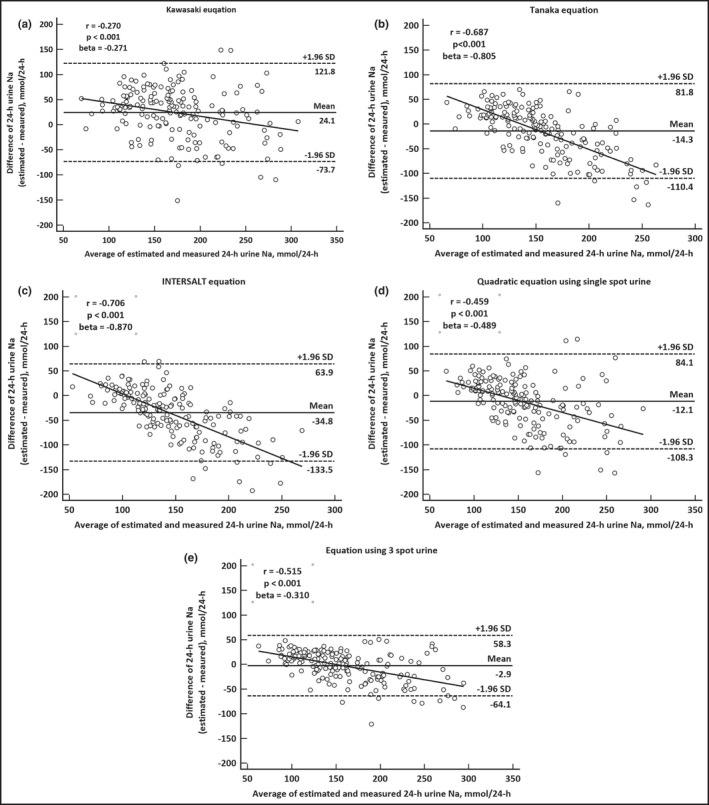
Bland‐Altman analysis for agreement between measured 24‐hour urine sodium and estimations provided by the five equations. (a) Kawasaki's equation, (b) Tanaka's equation, (c) INTERSALT equation, (d) quadratic equation using a single spot urine sample, and (e) the currently developed equation using the average of three spot urine samples.
Discussion
A single SU sample is typically used to estimate 24HUNa when evaluating population and individual sodium intake. However, such estimates of 24HUNa have limited clinical applicability because of the bias between the measured and estimated 24HUNa.9, 10, 11 We suggest a new method to estimate 24HUNa using the average of three SU samples, which can be applied to evaluate mean sodium intake in a population. The equation developed in the current study provided estimates of 24HUNa that were close to the measured values, with bias <3 mmol/24 h, and very high ICC and CCC. Comparatively, previously published equations using a single SU sample showed a bias of >10 mmol/24 h, which is in agreement with the report by Mente and colleagues,10 who found a bias of 13.6 mmol/24 h for the Kawasaki equation, which was the lowest among the bias values found for all tested equations using a single SU sample. However, we noted that, while using the average of three SU samples helped decrease the bias, the tendency of overestimation or underestimation persisted, albeit to a lower extent than for the previously published equations. For example, in our validation group, the maximum overestimates and underestimates provided by the equation using the average of three SU samples were 48.5 mmol/24 h and −121.2 mmol/24 h, respectively. For comparison, these values were 148.9 mmol/24 h and −151.0 mmol/24 h for the Kawasaki equation (data not shown). The reduced extent of overestimation or underestimation can be explained by the dilution bias of the regression model.19 We used two regression models to develop the equation, namely, one for the estimation of 24HUCr and the other for the estimation of 24HUNa. The persistence of the overestimation and underestimation trends implies that both the previously developed and currently proposed equations will yield a biased result for the estimation of sodium intake at the individual level. Nevertheless, the much lower bias noted for the currently proposed equation using the average of three SU samples suggests that a method using multiple SU samples may yield the closest estimate for the actual 24HUNa value of the studied population, although further improvement in accuracy is warranted.
Our study is the first to use the average of multiple samples to account for the diurnal (within‐day) variations of urine sodium excretion in the estimation of 24HUNa. Urinary sodium excretion varies diurnally as well as from day to day, and depends on the amount and timing of sodium intake.20, 21 In the present study, we also noted a significant diurnal variation in the urinary sodium/creatinine ratio. Thus, averaging multiple SU samples collected at different times may account for diurnal variation of urinary sodium excretion. Uechi and colleagues22 showed higher accuracy of an approach based on multiple SU sample collection compared with that of the Tanaka and INTERSALT equations. However, their Bland‐Altman analysis showed large limits of agreement (−144.9–141.7 mmol/d) even for reduced bias (−1.62 mmol/d). Moreover, the CCC was smaller than that noted for our equation, which was >0.8. The reason for these differences is likely related to the protocol of urine collection. Specifically, Uechi and colleagues collected three SU samples during daytime (between 1 pm and 4 pm), and compared the predicted 24HUNa against the measured 24HUNa, which was an average of two independently collected 24‐hour urine samples. Although they considered day‐to‐day variations in 24HUNa excretion, diurnal variation was not reflected in their equation. In addition, collecting two SU samples independently from the 24‐hour urine collection may yield a low CCC. Kawasaki and colleagues4 also collected and averaged multiple SU samples to develop and validate their equation. However, they collected only the second morning SU, not the daytime or evening SU samples. To test the possibility of accounting for diurnal variation in the previously developed equations based on a single SU sample, we replaced the value of the single sample in the Kawasaki equation with the average of three SU samples. Although ICC and CCC improved to 0.882 and 0.654, respectively, bias in the Bland‐Altman analysis was 33 mmol/24 h, and the limits of agreement ranged between −32.5 and 98.5 (data not shown), suggesting lower performance than the currently developed equation optimized for use of the average of the multiple SU samples.
Study Limitations
The main limitation of our study was that one of the three SU samples was collected at a different time for the development and validation groups. Specifically, the average for the development group included the morning SU sample collected at around 9 am, while the average for the validation group included the daytime SU sample collected between 1 pm and 6 pm. This difference in the collection time may account for some of the inaccuracy of the proposed model (eg, bias from the measured value), because of the diurnal variation, as mentioned above. Thus, to objectively evaluate the performance of the proposed equation, validation should be performed in another population, where the average is calculated considering for the morning‐first, morning (around 9 am), and evening SU samples. Finally, while we employed the average of three SU samples, increasing the number of SU samples considered may improve the estimation power of this approach, and forms the topic of future study.
Study Strengths
While employing equations that estimate sodium intake by using a single SU sample represents a convenient approach for evaluating the relationship between individual sodium intake and cardiovascular disease and events,7, 8, 23 the reliability of these estimations is questionable. In our study, we demonstrated that the estimation of 24HUNa via equations using a single SU sample had significant bias from measured 24HUNa, which is consistent with previous observations.9, 11 On the other hand, we showed that using multiple SU samples enables a significant improvement in the estimation of 24HUNa at the population level. Despite the fact that the tendency of overestimation or underestimation persisted, our proposed model still provided the best limits of agreement. Therefore, while the accuracy of all currently available equations is insufficient to warrant rigorous application for evaluating individual levels of sodium intake, the equation developed in the present study yields results with the lowest bias. Moreover, our results suggest that approaches based on using multiple SU samples are clearly more fit to be applied in the estimation of sodium intake, and future models involving further SU samples might improve on the performance reported herein.
Conclusions
The equation using the average of three SU samples provides an improved estimation of 24HUNa at the population level compared with the estimations achieved via equations using a single SU sample. Further validation in a different population is warranted.
Acknowledgments
This work was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention (2014‐E3500400) and the Ministry of Food and Drug Safety in 2012 (12162MFDS103).
Conflicts of Interest
The authors declare no competing financial interests in this study.
J Clin Hypertens (Greenwich). 2017;19:431–438. doi: 10.1111/jch.12922. © 2016 Wiley Periodicals, Inc.
References
- 1. He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52:363–382. [DOI] [PubMed] [Google Scholar]
- 2. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta‐analysis of prospective studies. BMJ. 2009;339:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 4. Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20:7–14. [DOI] [PubMed] [Google Scholar]
- 5. Tanaka T, Okamura T, Miura K, et al. A simple method to estimate populational 24‐h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103. [DOI] [PubMed] [Google Scholar]
- 6. Brown IJ, Dyer AR, Chan Q, et al. Estimating 24‐hour urinary sodium excretion from casual urinary sodium concentrations in Western populations: the INTERSALT study. Am J Epidemiol. 2013;177:1180–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–2238. [DOI] [PubMed] [Google Scholar]
- 8. O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. [DOI] [PubMed] [Google Scholar]
- 9. Rhee MY, Kim JH, Shin SJ, et al. Estimation of 24‐hour urinary sodium excretion using spot urine samples. Nutrients. 2014;6:2360–2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mente A, O'Donnell MJ, Dagenais G, et al. Validation and comparison of three formulae to estimate sodium and potassium excretion from a single morning fasting urine compared to 24‐h measures in 11 countries. J Hypertens. 2014;32:1005–1014. [DOI] [PubMed] [Google Scholar]
- 11. Ji C, Miller MA, Venezia A, et al. Comparisons of spot vs 24‐h urine samples for estimating population salt intake: validation study in two independent samples of adults in Britain and Italy. Nutr Metab Cardiovasc Dis. 2014;24:140–147. [DOI] [PubMed] [Google Scholar]
- 12. Rhee MY. High sodium intake: review of recent issues on its association with cardiovascular events and measurement methods. Korean Circ J. 2015;45:175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim SW, Lee SK, Hong SJ, Park SH. List‐assisted RDD sampling in Korea: testing the feasibility of national survey under within‐household selection. Int J Public Opin Res. 2012;24:79–92. [Google Scholar]
- 14. Rhee MY, Shin SJ, Park SH, Kim SW. Sodium intake of a city population in Korea estimated by 24‐h urine collection method. Eur J Clin Nutr. 2013;67:875–880. [DOI] [PubMed] [Google Scholar]
- 15. Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–1335. [DOI] [PubMed] [Google Scholar]
- 16. Knuiman JT, Hautvast JG, van der Heyden L, et al. A multi‐centre study on completeness of urine collection in 11 European centres. I. Some problems with the use of creatinine and 4‐aminobenzoic acid as markers of the completeness of collection. Hum Nutr Clin Nutr. 1986;40:229–237. [PubMed] [Google Scholar]
- 17. Murakami K, Sasaki S, Takahashi Y, et al. Sensitivity and specificity of published strategies using urinary creatinine to identify incomplete 24‐h urine collection. Nutrition. 2008;24:16–22. [DOI] [PubMed] [Google Scholar]
- 18. Critchley LA, Critchley JA. A meta‐analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91. [DOI] [PubMed] [Google Scholar]
- 19. Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ. 2010;340:c2289. [DOI] [PubMed] [Google Scholar]
- 20. Wesson LG Jr. Electrolyte excretion in relation to diurnal cycles of renal function. Medicine (Baltimore). 1964;43:547–592. [DOI] [PubMed] [Google Scholar]
- 21. Yamori Y, Kihara M, Fujikawa J, et al. Dietary risk factors of stroke and hypertension in Japan—Part 1: methodological assessment of urinalysis for dietary salt and protein intakes. Jpn Circ J. 1982;46:933–938. [DOI] [PubMed] [Google Scholar]
- 22. Uechi K, Asakura K, Ri Y, et al. Advantage of multiple spot urine collections for estimating daily sodium excretion: comparison with two 24‐h urine collections as reference. J Hypertens. 2016;34:204–214. [DOI] [PubMed] [Google Scholar]
- 23. Park S, Park JB, Lakatta EG. Association of central hemodynamics with estimated 24‐h urinary sodium in patients with hypertension. J Hypertens. 2011;29:1502–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]


