Abstract
In clinical practice, ambulatory blood pressure monitoring (ABPM) tends to be used solely for diagnosing hypertension, especially to identify white‐coat and masked hypertension. However, ABPM can provide additional information to guide the management and drug treatment of hypertension. In this brief review, the general principles governing the use of ABPM in clinical practice, such as the devices and software, recording requirements, the thresholds for the day, night and 24‐hour periods and how often to repeat ABPM are summarized. The use of ABPM for diagnosing, determining the efficacy of treatment, and assessing the long‐term control of hypertension are discussed.
Keywords: ambulatory blood pressure/home blood pressure monitor, clinical management of high blood pressure, general, hypertension
1. INTRODUCTION
Although ambulatory blood pressure monitoring (ABPM) has been available for over 40 years, it has only recently been accepted as the most informative measurement of blood pressure (BP) behavior,1 with the recent American College of Cardiology/American Heart Association (ACC/AHA) hypertension management guidelines from the United States recommending ABPM for out‐of‐office measurement in clinical practice.2 However, international guidelines tend to focus on the use of ABPM for simply diagnosing hypertension, especially to identify white‐coat and masked hypertension, with little attention being given to the wider role for ABPM, such as assessing the response to therapy in patients with hypertension. Recent reviews have begun to draw attention to the wider applications of ABPM in clinical practice, which provide primary care physicians with many novel attributes to improve the management of patients with hypertension.3, 4, 5, 6
2. GENERAL PRINCIPLES GOVERNING THE USE OF ABPM IN PRACTICE
It is not the purpose of this article to give detailed recommendations for the use of ABPM in clinical practice. More detailed reviews have done this, but it is appropriate to summarize the principles governing the use of ABPM.6
Devices and software
Devices for ABPM must be validated independently according to the internationally accepted validation protocols, and specific validation may be required in special patient populations. There is now agreement that an international protocol for validation should apply for all BP measuring devices.7 The software should present ABPM data in a standardized single‐page report that should include: (1) a BP plot showing different windows of the 24‐h period identified and normal bands clearly demarcated showing the individual’s awake and asleep time intervals as reported by each individual; (2) summary statistics for BP and heart rate separately for the 24 h, the daytime (awake), the night‐time (asleep), and the white‐coat window periods; and (3) the raw BP data. The use of ABPM to monitor treatment can be greatly facilitated by software capable of providing a trend report with a historical display of day and night‐time pressures on ABPM over time (Figure 1).
Figure 1.
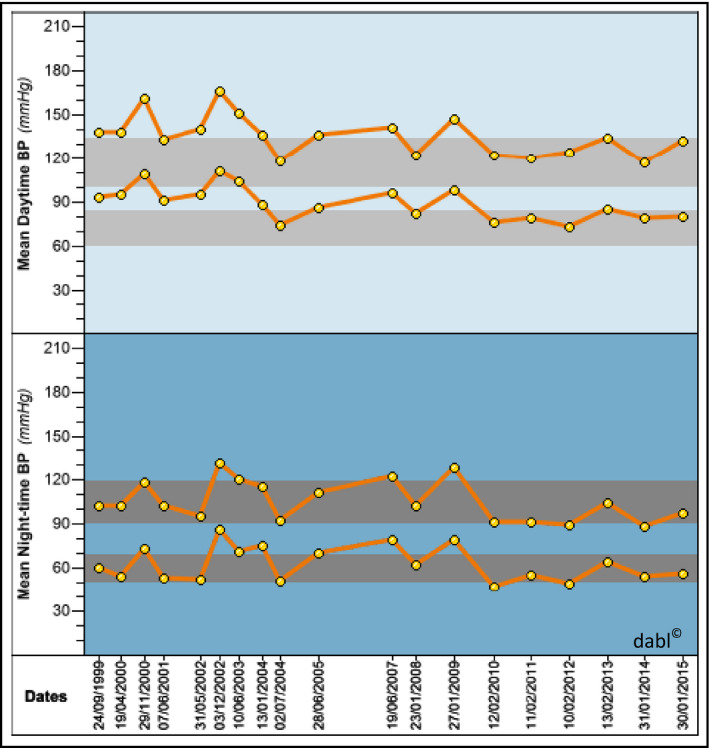
Longitudinal trend report using ABPM over 15 years in a single patient
Performing ABPM
The requirements for obtaining a satisfactory ABPM should ensure that: (1) measurements are taken at least every 30 minutes, or more frequently, throughout the entire 24‐hour period on a routine day; (2) the ABPM recording provides a minimum of 20 valid daytime (awake) and seven nighttime (asleep) measurements; and (3) that at least 70% of the expected 24‐hour readings are valid.
Ambulatory BP thresholds
The currently accepted thresholds for hypertension diagnosis on the basis of ABPM are a 24‐hour average of at least 130/80 mm Hg (systolic/diastolic), daytime (awake) average of at least 135/85 mm Hg, and nighttime (asleep) average of at least 120/70 mm Hg.1 However, lower thresholds, although not supported by outcome data, have been recommended in the ACC/AHA hypertension management guidelines.2 The previously recommended thresholds, which would equate to an office BP of 140/90 mm Hg, have been lowered to 125/75 mm Hg, 130/80 mm Hg, and 110/65 mm Hg for 24‐hour BP, daytime BP, and nighttime BP, respectively, but these levels must await confirmation in future studies.2
Nighttime BP evaluation
ABPM is particularly useful in assessing the severity of hypertension throughout the 24‐hour period, and especially to identify nocturnal hypertension and abnormal patterns of nocturnal behavior, such as nondipping, which is associated with a high risk for cardiovascular complications. Other nocturnal patterns on ABPM include reverse dipping (or nocturnal rising), extreme dipping, and the morning surge.
Repeated ABPM
Recommendations on when to repeat ABPM are based on many factors, including ABPM availability and clinical judgment, particularly because relevant evidence is limited. Although it is desirable to repeat ABPM to confirm the diagnosis of white‐coat or masked hypertension, because of the imperfect reproducibility of these diagnoses, repetition of ABPM becomes of even greater practical importance if BP‐lowering treatment is being prescribed. Considering the critical importance of optimal BP control in high‐risk populations, indications for repeating ABPM in such groups to evaluate 24‐hour BP control are as follows: (1) difficult or resistant hypertension; (2) presence of target organ damage; (3) high total cardiovascular risk (eg, those with diabetes mellitus); (4) positive family history of premature cardiovascular disease (eg, those with 10‐year cardiovascular risk scores > 10%); and (5) and to confirm effectiveness of treatment of nocturnal hypertension.
3. USE OF ABPM FOR THE DIAGNOSIS OF HYPERTENSION
The North American,8, 9 European1, 10 Japanese11 and Chinese12 bodies responsible for international and national guidelines, having carefully examined the evidence as to which method of BP measurement is best—office BP, home BP, or ABPM—have unanimously recommended ABPM as the “gold standard” technology for BP measurement. To add to this weight of international scientific opinion, the recently published ACC/AHA hypertension management guidelines have endorsed the use of ABPM in hypertension management, while recognizing that there will be difficulty in implementing its use in clinical practice.2 The recommendations from these groups are based on sound scientific evidence showing that ABPM is the most accurate and cost‐effective method of BP measurement and each has concluded that ABPM (or home measurement if ABPM is not available, declined, or not tolerated) should be performed in anyone who has had an elevated BP measurement ≥140/90 mm Hg recorded by any method of measurement. The rationale behind this recommendation is basically to confirm that the elevation of BP noted on office measurement is sustained and not caused by a white‐coat reaction, as may occur in some 25% of patients.13 Therefore, for the diagnosis of hypertension, anyone with a raised BP level by any method of measurement—casual, office, home, clinic, pharmacy, or kiosk—should be offered ABPM to confirm hypertension or to identify white‐coat hypertension wherever possible, and treatment should only be prescribed on the basis of an ABPM (with the possible exception of patients with markedly elevated office BP, eg >180/110 mm Hg) and office hypertension associated with target organ damage. However, target ABPM values to be achieved by treatment have not yet been identified through randomized intervention trials.
4. ABPM TO DETERMINE EFFICACY OF TREATMENT
ABPM has been shown to be beneficial in guiding drug prescribing. In one study, only 12% of patients achieved target BP with office BP compared with more than one third of patients with ABPM. Furthermore, 38% of patients had a change in their medication as a result of ABPM, 32% had a new medication started, and 14% of untreated patients with elevated office BP, who were candidates for drug treatment, were not started on medication because ABPM values were normal.14, 15 In one Spanish database, 700 000 elderly individuals would have been spared medication if ABPM, instead of office BP, had been performed.5 On the other hand, the percentage of patients considered eligible for treatment increased by 6% with ABPM, which amounted to 350 000 elderly patients. In this instance, casual BP was masking hypertension, which only became apparent with ABPM. Among patients eligible for treatment, only 37% had their BP controlled with casual BP, whereas this figure increased to 54% with ABPM. Although this finding indicates that when ABPM was used to assess BP in the community, the degree of BP control appeared much better than with casual methods of BP measurement, the daunting reality is that only half of all Spanish individuals were within the normal range for both casual BP and ABPM and less than half of individuals with elevated casual BP and ABPM were receiving antihypertensive medication.5 These results show that the use of ABPM ensures that the right people are treated with BP‐lowering drugs, with an overall reduction in the number of patients being incorrectly treated for hypertension. All of this means that ABPM can save money, and the extra costs of providing the technique would be more than offset by cost savings from better‐targeted treatment.
The concern of both the prescribing doctor and the treated patient is to know whether the treatment has restored BP to normal during the day and night, and the only way of confirming this is by repeating the ABPM. The next question is to decide when this should be performed and how the risk factor profile of the patient should influence this decision. In patients with a low‐risk profile, ABPM might be repeated every few months or office BP might be complimented by home BP monitoring until control is achieved. If the risk factor profile of the patient is high (evidence of target organ damage, previous cardiovascular event, family history, or comorbidities, such as diabetes mellitus), the need to achieve good BP control becomes more pressing. Therefore, once treatment is initiated, it would seem reasonable to repeat ABPM within a few weeks to determine whether adequate reduction has been achieved. If further adjustments in therapy are required, as may indeed be the case, repeat ABPM at multiweek intervals until control is achieved is justifiable. Concomitant use of home BP measurement may compliment and reduce the need to repeat ABPM.16
5. ASSESSING LONG‐TERM CONTROL OF TREATMENT
Once control of daytime and nighttime ABPM has been achieved, ABPM needs only be performed periodically to ensure 24‐hour BP control. Home BP measurement can be used to obtain confirmatory evidence that BP control is being maintained, at least for daytime BP.16, 17 Evidence is lacking for the use of ABPM to guide treatment in specific groups, other than acknowledgement that high‐risk groups, such as patients with chronic kidney disease, are more likely to benefit from having ABPM performed if for no other reason than to determine and treat nighttime BP, which is nearly always elevated in patients with moderate to severely reduced kidney function.1, 18, 19
6. CONCLUSIONS
We have briefly outlined the value of the many applications of ABPM in clinical practice in the hope that primary care physicians will see the technique as having much greater value than merely using ABPM to confirm the diagnosis of hypertension. We have made recommendations as to how ABPM might be used to initiate treatment and to assess the efficacy of BP‐lowering therapy over time. In doing so, we recognize that initially there will be a higher cost to healthcare providers, but this should be more than offset by improved BP control and the reduction of cardiovascular consequences of hypertension.
CONFLICT OF INTEREST
EOB has conducted validation studies for various manufacturers and advised manufacturers on device development. W.W., Editor, UptoDate (Wolters Kluwer), Safety Consultant for Novartis, Takeda, Teva (not related to content).
O'Brien E, White WB, Parati G, Dolan E. Ambulatory blood pressure monitoring in the 21st century. J Clin Hypertens. 2018;20:1108–1111. 10.1111/jch.13275
REFERENCES
- 1. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731‐1768. [DOI] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127‐e248. [DOI] [PubMed] [Google Scholar]
- 3. Staessen JA, Li Y, Hara A, Asayama K, Dolan E, O'Brien E. Blood Pressure Measurement Anno 2016. Am J Hypertens. 2017;30:453‐463. [DOI] [PubMed] [Google Scholar]
- 4. Dolan E, O'Brien E. How should ambulatory blood pressure measurement be used in general practice? J Clin Hypertens (Greenwich). 2017;19:218‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Banegas JR, de la Cruz JJ, Graciani A, et al. Impact of ambulatory blood pressure monitoring on reclassification of hypertension prevalence and control in older people in Spain. J Clin Hyperten (Greenwich). 2015;17:453‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stergiou G, Palatini P, Asmar R, et al. Blood pressure monitoring: theory and practice. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability Teaching Course Proceedings. Blood Press Monit. 2018;23:1‐8. [DOI] [PubMed] [Google Scholar]
- 7. Stergiou GS, Alpert B, Mieke S, et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. Hypertension. 2018;71:368‐374. [DOI] [PubMed] [Google Scholar]
- 8. Siu AL, US Preventive Services Task Force . Screening for high blood pressure in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015; 163:778‐786. [DOI] [PubMed] [Google Scholar]
- 9. Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada's 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016; 32:569‐588. [DOI] [PubMed] [Google Scholar]
- 10. National Institute for Health and Clinical Excellence (NICE) . The Clinical Management of Primary Hypertension in Adults. London, UK: National Institute for Health and Clinical Excellence; 2011. [Google Scholar]
- 11. Shimamoto K, Ando K, Fujita T, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253‐390. [DOI] [PubMed] [Google Scholar]
- 12. Liu LS, Writing Group of 2010 Chinese Guidelines for the Management of Hypertension . Chinese guidelines for the management of hypertension (in Chinese). Chin J Hypertens. 2010;2011:701‐742. [Google Scholar]
- 13. Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988;259:225‐228. [PubMed] [Google Scholar]
- 14. O'Brien E, Dolan E. Ambulatory blood pressure monitoring for the effective management of antihypertensive drug treatment. Clin Therapeutics. 2016;38:2142‐2151. [DOI] [PubMed] [Google Scholar]
- 15. Uallachain GN, Murphy G, Avalos G. The RAMBLER study: the role of ambulatory blood pressure measurement in routine clinical practice: a cross‐sectional study. Ir Med J. 2006;99:276‐279. [PubMed] [Google Scholar]
- 16. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008; 26:1505‐1530. [DOI] [PubMed] [Google Scholar]
- 17. Sheppard JP, Stevens R, Gill P, et al. Predicting Out‐of‐Office Blood Pressure in the Clinic (PROOF‐BP): derivation and validation of a tool to improve the accuracy of blood pressure measurement in clinical practice. Hypertension. 2016;67:941‐950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parati G, Ochoa JE, Bilo G, et al. Hypertension in chronic kidney disease part 1: out‐of‐office blood pressure monitoring: methods, thresholds, and patterns. Hypertension. 2016;67:1093‐1101. [DOI] [PubMed] [Google Scholar]
- 19. Parati G, Ochoa JE, Bilo G, et al. European Renal and Cardiovascular Medicine (EURECA‐m) working group of the European Renal Association‐European Dialysis Transplantation Association (ERA‐EDTA). Hypertension in chronic kidney disease part 2: role of ambulatory and home blood pressure monitoring for assessing alterations in blood pressure variability and blood pressure profiles. Hypertension. 2016;67:1102‐1110. [DOI] [PubMed] [Google Scholar]


