Abstract
Single‐site, intensive, community‐based blood pressure (BP) intervention programs have led to BP improvements. The authors examined the American Heart Association's Check. Change. Control. (CCC) program (4069 patients/18 cities) to determine whether BP interventions can effectively be scaled to multiple communities, using a simplified template and local customization. Effectiveness was evaluated at each site via site percent enrollment goals, participant engagement, and BP change from first to last measurement. High‐enrolling sites frequently recruited at senior residential institutions and service organizations held hypertension management classes and utilized established and new community partners. High‐engagement sites regularly held hypertension education classes and followed up with participants. Top‐performing sites commonly distributed BP cuffs, checked BP at engagement activities, and trained volunteers. CCC demonstrated that simplified community‐based hypertension intervention programs may lead to BP improvements, but there was high outcomes variability among programs. Several factors were associated with BP improvement that may guide future program development.
Keywords: blood pressure management, hypertension intervention programs
1. Introduction
Hypertension is the leading cause of cardiovascular disease in the United States, affecting more than 78 000 000 adults.1 In 2010, the American Heart Association (AHA) set the ambitious goal of improving the cardiovascular health of all Americans by 20% and reducing deaths from cardiovascular disease and stroke by 20% by the year 2020.2 Pivotal to this goal is the development of prevention strategies that are simple, cost‐effective, sustainable, and scalable.
The AHA has recently supported two large‐scale, multifaceted, quality improvement efforts designed to assess the impact of pharmacists and/or community health workers, as well as the signature Heart360 information health technology, on lowering people's blood pressure (BP).3, 4 Both of these academic‐community partnership initiatives were effective; however, they were also resource‐intensive in terms of cost and staffing, raising the question of whether such programs could be effective and scalable with less academic and financial support. Furthermore, it was unclear whether the findings from these initiatives could be generalized to other regions of the United States.
In 2013, the AHA launched the Check. Change. Control. (CCC) BP program, which was a multi‐intervention community‐based initiative to improve BP control in 18 cities in the United States. AHA staff and volunteers in each geographic area worked with businesses, institutions, and community partners to build health campaigns targeting BP self‐management. Each city's campaign had four mandatory implementation components: (1) the AHA's multicultural director in each city oversaw the design of the community‐based program; (2) community partners were utilized as a place for program implementation, volunteer health mentor recruitment, and/or participant recruitment; (3) volunteer health mentors (lay persons or health professionals who were trained by national and regional AHA staff leadership) provided education, followed participants, and/or provided assistance for BP uploads; and (4) the Heart360 online BP monitoring tool was used to track BP trends and uploads. In addition to these four strategies, all 18 sites were allowed to customize a campaign for their community setting. As a result, CCC presented a unique opportunity to evaluate 18 similar—albeit separate—simultaneous experiments in community‐based BP control.
In order to assess the ability of the CCC program to reduce BP, we evaluated the program's ability to: (1) enroll participants, (2) sustain participation, and (3) improve BP control. By comparing the differential features and outcomes of these 18 mini‐campaigns, we gained insight into which campaign features most correlated with success.
2. Methods
2.1. Campaigns
The national AHA office selected sites for CCC participation based on the city's percentage of minorities, the prevalence of coronary heart disease in the geographic area, and the presence of an AHA multicultural director. Each invited AHA multicultural director was required to complete a grant application on their projected program; the application required a specific program format to keep general consistency between all programs. The applications were reviewed by the AHA's High Blood Pressure Advisory Group, a standing advisory committee of hypertension experts across the United States. The AHA selected 18 programs based on its overall budget and interest from its markets in select geographic areas. Sites were selected in Birmingham/Montgomery, AL; Los Angeles, CA; San Francisco, CA; Washington, DC; Miami, FL; Atlanta, GA; Chicago, IL; Baltimore, MD; Detroit, MI; St. Louis, MO; Charlotte, NC; New York, NY/NJ; Cleveland, OH; Philadelphia, PA; Memphis, TN; Dallas/Fort Worth, TX; Houston, TX; and Richmond, VA. Any adult older than 18 years living in one of the targeted geographic areas was eligible to participate in the CCC program. Enrollment occurred at enrollment kickoff events.
2.2. Data collection
Data were collected in three distinct phases: program planning, preimplementation, and postimplementation. During the program planning phase, which took place 6 months prior to campaign launch, each site completed a grant application outlining planned campaign implementation activities and use of the $20 000 budget. Planned campaign features were abstracted from these grants by researchers (MLA and ECO) at the Duke Clinical Research Institute (DCRI, Durham, NC). During the preimplementation phase, which took place within the month of campaign implementation, campaign directors were asked to complete a questionnaire via SharePoint (Microsoft Office SharePoint 2007 Technologies, Redmond, WA). This questionnaire contained both discrete and open‐ended items. Researchers at the DCRI prepopulated the questionnaire with planned activities and features abstracted from the grant application, gathering any missing data on preimplementation plans and activities (Table S1). During the postimplementation phase, which took place 1 to 3 months after completion of the intervention, individual telephone interviews were conducted with each campaign director using a standardized script. Interviews were conducted by a single study author (AMA), audiotaped, and then subsequently transcribed. Another researcher (RPU) listened during the interviews and took in‐depth notes on themes of interest. Postimplementation data were used to characterize implementation successes and challenges and to describe the actual components of each campaign.
BP and demographic data logged by participants were obtained via the Heart360 tool, which was developed by the AHA as a Web‐based personal health portal to facilitate self‐monitoring and information exchange with providers (www.heart360.org). BP data from Heart360 was used to estimate enrollment, engagement, and BP outcomes for each of the 18 campaigns, as well as for the overall program.
2.3. Survey instruments
The telephone interview guide for the postimplementation survey was developed to elicit information regarding the successes and challenges of enrolling participants; engaging participants; tracking enrollment and engagement; and working with Heart360 software, community partners, and volunteer mentors. Additionally, the interview guide provided information about the campaign director's experience and background, as well as detailed use of the $20 000 budget. Questions were open‐ended and the interview was designed to last about 60 minutes. The final script was agreed upon by all study authors. The interview guide was piloted with a campaign director from a separate CCC site. Modifications were made for clarity and length. A full interview guide can be found in Figure S1.
2.4. Statistical analysis
2.4.1. Qualitative data methods
A preliminary coding scheme was developed deductively prior to data collection. The overarching framework was to identify the successes and challenges of implementing the CCC program. All transcripts were prepared by a professional transcriber, and a sample of transcripts was checked against the recordings to ensure accuracy. After the data were collected, two independent coders reviewed each of the transcripts and wrote descriptive memos about emerging themes. Since additional themes and concepts emerged during transcript review, the codebook was modified until no new concepts were found; at this point, the codebook was considered final. Two authors (MLA and AMA) used the constant comparative method of qualitative data analysis to code and synthesize recurrent themes in the transcripts.5, 6 Differences were resolved by a third investigator (RPU) or a negotiated group consensus, if necessary. All coding was performed manually. Categorical variables on enrollment, engagement, and campaign features were extracted to evaluate an association between campaign features and outcomes.
2.4.2. Quantitative outcomes
We evaluated three prospectively defined outcomes of interest (all calculated from Heart360 BP data): (1) participant enrollment, (2) participant engagement, and (3) BP change (comparing first and last recorded values for systolic and diastolic BP). The primary outcome was participant engagement, defined as the percent of participants with at least eight BPs entered at any time over a 4‐month period. The secondary outcome was participant enrollment, derived by dividing the actual enrollment for the study duration by the expected enrollment, as specified in the site's grant application. Each AHA multicultural director, in concert with national AHA leadership, specified projected enrollment estimates prior to campaign initiation. BP changes were defined in three ways: (1) average change in systolic BP, (2) average change in diastolic BP, and (3) the proportion of enrollees who moved from a higher to lower BP category. Average changes in systolic and diastolic BP were obtained by subtracting the first measurement from the last measurement.4 If a participant did not enter measurements consistently throughout the full‐month4 period, then the last BP entered was used as the participant's final BP for the campaign. BP categories were defined as normotensive (<120/80 mm Hg), prehypertensive (>120/80 mm Hg, but <140/90 mm Hg), and hypertensive (≥140/90 mm Hg). We calculated these three outcomes at the participant and site level. All data on outcomes were obtained using the Heart360 tool. We excluded impossible systolic BP (<60 mm Hg or >275 mm Hg) and diastolic BPs (<40 mm Hg or >160 mm Hg). We excluded 0 systolic BPs and 23 diastolic BP uploads. After excluding these 23 uploads, four patients were excluded from our analysis.
Four sensitivity analyses examined systolic and diastolic BP changes by distinct number of BP uploads (n=at least 2, 4, 6, and 8 BP values); P values for changes in systolic and diastolic BPs were compared using the Wilcoxon signed‐rank test. We examined the association between the number of uploads and actual BP change for both systolic and diastolic BP using the Spearman correlation coefficient.
Campaign sites were divided based on performance for each outcome into lowest (25th), middle (50th), and highest (25th) performance according to percentile distributions. Pearson chi‐square tests were used to compare categorical variables. Kruskal‐Wallis tests were used to compare continuous or ordinal variables. Using mixed‐methods research,7, 8 we then compared program features and characteristics with outcomes. All P values were two‐sided and significant at P<.05. All statistical analyses were conducted using SAS statistical software, version 9.4 (SAS Institute, Inc, Cary, NC). Given the lack of personal identifiers, our analysis was exempt from institutional review board review.
3. Results
3.1. Site demographics
Between January 1, 2013, and March 31, 2013, 4069 adults were enrolled into the CCC program at 18 US sites. The median age of participants at each site was 51 years (interquartile range 41–62 years). Female participants comprised 74.5% of the study cohort. Overall, 40.6% of participants had an initial systolic BP ≥140 mm Hg and/or a diastolic BP ≥90 mm Hg.
3.2. Overall outcomes
Based on targeted enrollment projections from the national AHA office, the actual overall enrollment in CCC was 40.8% of the prospectively defined goals (4069/9980). Overall, campaign participants had a mean upload of four (standard deviation [SD] 6.3) BPs. Sustained high‐level patient engagement (8+ BP entries over 4 months) was observed in 20.7% of participants. The overall mean campaign reduction in systolic and diastolic BPs was −7.5 (SD±20.1) mm Hg and −3.3 mm Hg (SD±11.2 mm Hg), respectively. Overall, approximately 32.7% of participants moved from either the uncontrolled hypertension or prehypertensive BP categories to a lower (prehypertensive or normotensive) BP category.
3.3. Site‐based outcomes
There was significant site variation with regard to outcomes. Expected enrollment ranged from 350 to 1200 among the 18 sites, based on national office determination. Actual enrollment ranged from 74 to 422 participants; percent of actual vs expected enrollment for each site ranged from 9.3% to 120.6%. Engagement, which was defined as more than eight recorded BPs over a 4‐month period, averaged 14.7% and ranged from 0% to 52.8% among the 18 sites. Initial mean campaign BP ranged from 121/76 mm Hg to 156/89 mm Hg (Figure 1). Site change in systolic BP ranged from −29.3 mm Hg to +7.7 mm Hg. Site change in diastolic BP ranged from −9.9 mm Hg to +1.8 mm Hg. The site proportion of participants who moved from a higher to lower BP category ranged from 0% to 65.3% (Table 1).
Figure 1.
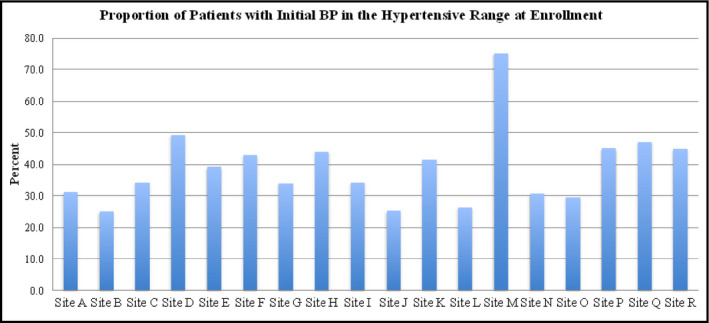
Patients with initially high blood pressure (BP). The proportion of patients in each market with an initially high BP, among 18 Check. Change. Control (CCC) sites
Table 1.
Participant Outcomes of Enrollment, Engagement, and BP Change, According to Campaign
| Campaign ID | No. Enrolled | No. Expected for Enrollment | Enrolled, % | Engagement | Average Change in Diastolic BP | Average Change in Systolic BP | Higher to Lower BP Category, % |
|---|---|---|---|---|---|---|---|
| Site A | 74 | 800 | 9.3 | 1.4 | −0.4 | −1.0 | 9.4 |
| Site B | 116 | 1200 | 9.7 | 17.2 | −3.7 | −3.1 | 25.7 |
| Site C | 217 | 1150 | 18.9 | 7.4 | −2.6 | −2.5 | 27.3 |
| Site D | 154 | 730 | 21.1 | 15.6 | −2.9 | −4.1 | 39.0 |
| Site E | 281 | 1150 | 24.4 | 0.0 | 0.8 | −1.0 | 23.1 |
| Site F | 91 | 350 | 26.0 | 5.5 | −3.6 | −9.3 | 36.8 |
| Site G | 118 | 350 | 33.7 | 25.4 | −1.0 | −2.5 | 27.5 |
| Site H | 150 | 350 | 42.9 | 2.7 | −2.1 | −7.8 | 31.1 |
| Site I | 211 | 450 | 46.9 | 15.6 | 1.8 | −2.6 | 19.4 |
| Site J | 166 | 350 | 47.4 | 9.0 | −1.3 | −1.3 | 23.7 |
| Site K | 176 | 350 | 50.3 | 0.6 | −3.5 | 7.7 | 0.0 |
| Site L | 206 | 350 | 58.9 | 2.4 | −1.7 | −2.3 | 24.2 |
| Site M | 322 | 500 | 64.4 | 46.3 | −9.9 | −29.3 | 65.3 |
| Site N | 304 | 450 | 67.6 | 8.9 | −3.3 | −5.5 | 39.8 |
| Site O | 356 | 400 | 89.0 | 15.2 | −1.2 | −2.6 | 24.6 |
| Site P | 329 | 350 | 94.0 | 2.4 | −2.3 | −5.7 | 27.8 |
| Site Q | 376 | 350 | 107.4 | 25.0 | −3.2 | −4.1 | 33.9 |
| Site R | 422 | 350 | 120.6 | 52.8 | −4.0 | −8.4 | 28.3 |
Abbreviations: BP, blood pressure; ID, identification.
3.4. Program activities
Program activities are described in Tables 2 and 3. The AHA sites trained volunteer health mentors to carry out CCC programs and interact with program participants; these volunteer health mentors were from both healthcare and nonhealthcare backgrounds. Each CCC program was given $20 000 for implementation, which was used in various ways to create incentives, training or training materials, marketing, staffing support or stipends, and purchase electronic and Wi‐Fi devices (Figure S2). Selected community partners for each site varied significantly and included churches (15/18 programs), higher education institutions (10/18), private sorority or fraternity societies (11/18), healthcare institutions (12/18), community health centers (7/18), and businesses (11/18) (Table S2). Programs were conducted in multiple settings. Table 2 shows that the most common program implementation sites were churches, healthcare institutions, community or recreation centers (including YMCAs), worksite wellness programs (eg, insurance companies), other businesses (eg, pharmacies, insurance companies), or other (eg, private societies or organizations, apartment complexes).
Table 2.
Enrollment Activities and Characteristics of the CCC Program
| Enrollment Characteristics | No. of Campaigns | Proportion of Campaigns, % |
|---|---|---|
| Enrollment mechanisms: recruitment locations | ||
| Churches | 16 | 88.9 |
| Healthcare institution (composite) | 7 | 38.9 |
| Hospital | 3 | 16.7 |
| Health clinic | 6 | 33.3 |
| Other (cardiac rehab/physical therapy) | 2 | 11.1 |
| Community places (composite) | 4 | 22.2 |
| Community center (including YMCA) | 3 | 16.7 |
| Recreation center | 1 | 94.4 |
| Senior center | 3 | 16.7 |
| Worksite wellness (or businesses) | 8 | 44.4 |
| Higher education institution | 3 | 16.7 |
| Other recruitment locations (composite) | 10 | 55.6 |
| Private societies or organizations (sororities/fraternities) | 7 | 38.9 |
| Apartment complex (senior living complex) | 3 | 16.7 |
| Other | 5 | 27.8 |
| Enrollment mechanisms: health events | ||
| Enrollment education events | 13 | 72.2 |
| Nutrition/label reading | 1 | 5.6 |
| Cooking classes | 9 | 50 |
| Hypertension management | 6 | 33.3 |
| CPR classes | 1 | 5.6 |
| PTES presentations (stroke education) | 3 | 16.7 |
| Exercise classes | 4 | 22.2 |
| Life's Simple 7 (online educational/goal setting tool) | 2 | 11.1 |
| BP screenings | 13 | 72.2 |
| Enrollment mechanisms: kickoff event | ||
| Kickoff event held | 16 | 88.9 |
| Local or national celebrity | 5 | 27.8 |
| Enrollment mechanisms: incentives | ||
| Who received incentives (composite) | 18 | 100 |
| Incentives for AHA staff | 0 | 0 |
| Incentives for participants | 17 | 100 |
| Incentives for community partners | 5 | 27.8 |
| Incentives for volunteer mentors | 8 | 44.4 |
| Types of incentives | ||
| BP cuffs | 6 | 33.3 |
| Gift cards | 7 | 38.9 |
| Public recognition | 2 | 11.1 |
| Mini‐grants | 1 | 5.6 |
| Other prizes/giveaways | 15 | 83.3 |
| Other | 6 | 33.3 |
Abbreviations: AHA, American Heart Association; BP, blood pressure; CCC, Check. Change. Control.; CPR, cardiopulmonary resuscitation; PTES, Power To End Stroke; YMCA, Young Men's Christian Association.
Table 3.
Engagement Characteristics of the CCC Program
| Engagement Characteristics | No. of Sites | Campaigns, % |
|---|---|---|
| Participant engagement mechanisms | ||
| Communication with participants | 17 | 94.4 |
| Incentives | 16 | 88.9 |
| Messages through Heart360 | 7 | 38.9 |
| Health activities or community events | 16 | 88.9 |
| Access points | 10 | 55.6 |
| Health events | ||
| Engagement education events (composite) | 15 | 83.3 |
| Nutrition/label reading | 8 | 44.4 |
| Cooking classes | 12 | 66.7 |
| Hypertension management | 6 | 33.3 |
| CPR classes | 3 | 16.7 |
| PTES presentations (stroke education) | 6 | 33.3 |
| Exercise classes | 12 | 66.7 |
| Life's Simple 7 (online educational/goal setting tool) | 1 | 5.6 |
| BP screenings | 8 | 44.4 |
| Communication to encourage uploads | ||
| Contacted by AHA staff | 4 | 22.2 |
| Contacted by volunteer mentors | 18 | 100.0 |
| Contacted by volunteer lead | 5 | 27.8 |
| Contacted by Heart360 | 4 | 22.2 |
| Contacted via text | 3 | 16.7 |
| Contacted via phone call | 11 | 61.1 |
| Contacted via e‐mail | 14 | 77.8 |
| Contacted via face‐to‐face | 9 | 50.0 |
| Contacted via other | 1 | 5.6 |
| Engagement mechanisms: Heart360 help | ||
| Way for help provided | 16 | 88.9 |
| Wi‐Fi hot spots | 1 | 5.6 |
| Phone contact CCC team | 9 | 50.0 |
| 1‐800‐number | 6 | 33.3 |
| Buddy system | 1 | 5.6 |
| Educational resources | 2 | 11.1 |
| Heart360 kiosk | 1 | 5.6 |
| AHA support staff at engagement sites | 4 | 22.2 |
| Access points | 1 | 5.6 |
| Other | 3 | 16.7 |
Abbreviations: AHA, American Heart Association; BP, blood pressure; CCC, Check. Change. Control.; CPR, cardiopulmonary resuscitation; PTES, Power To End Stroke.
Events conducted during the enrollment and engagement periods varied significantly and included hypertensive management classes, cooking and nutrition classes, Power To End Stroke (an AHA tool) presentations, Life's Simple 7 (an AHA tool), and BP screenings. Incentives played a significant role in attempted program enrollment and engagement, and included small giveaways, BP cuffs, gift cards, and public recognition. In order to promote engagement among participants, each program employed a variety of tactics (Table 2). The most common approaches were communication to participants, incentives, and health activities and/or community events. Some programs either created access points (a place for participants to have their BP checked and/or to upload BPs) or implemented programs in places that already had access points. Table 3 shows how communication to participants varied; most programs had a mechanism in place to help program participants experiencing problems with Heart360 (eg, password issues, difficulty in uploading, no computer).
3.5. Features of the highest 25th, middle 50th, and lowest 25th campaigns
3.5.1. Enrollment
The mean patient enrollment was 371 for the four top‐performing (highest 25th) sites, 202 for the middle 50th (n=10), and 140 for the lowest 25th (n=4); P=.001. Compared with the lower 25th and middle 50th sites, the highest 25th sites were more likely to recruit from senior living facilities and involve service organizations such as minority‐based fraternities and sororities (75% for the highest 25th, 70% for the middle 50th, and 0% for the lowest 25th; P=.047). Top‐enrolling sites had a greater number of kickoff events (≥7 events: 75% for the highest 25th, 20% for the middle 50th, and 0% for the lowest 25th; P=.04) and were more likely to have built their campaign around community partners (Table 4).
Table 4.
Campaign‐Level Characteristics and Outcomes by Lowest, Middle, and Highest Performing Groups
| Program Characteristics | Overall (n=18) | Group 1 Lowest 25th (n=4) | Group 2 Middle 50th (n=10) | Group 3 Highest 25th (n=4) | P Value |
|---|---|---|---|---|---|
| Systolic BP change,a mm Hg, mean (SD) | −4.7 (7.2) | 1.1 (4.4) | −3.5 (1.3) | −13.7 (10.4) | .001 |
| Engagement mechanism | |||||
| Hypertension management classes, % | 33.3 | 0 | 30 | 75 | .09 |
| Incentives community partner, % | 22.2 | 25 | 0 | 75 | .01 |
| Communication to participants | |||||
| Phone call, % | 61.1 | 25 | 60 | 100 | .1 |
| Text, % | 16.7 | 0 | 10 | 50 | .13 |
| Volunteer leads to oversee program, % | 16.7 | 0 | 10 | 50 | .13 |
| Program enrollment,a mean, % (No.) | 51.8 (226) | 14.7 (140) | 46.2 (202) | 114.0 (371) | .001 |
| Recruitment location | |||||
| Senior living complex/service organizations | 55.6 | 0 | 70 | 75 | .047 |
| Churches | 88.9 | 100 | 90 | 75 | .54 |
| Worksite wellness | 44.4 | 100 | 30 | 25 | .047 |
| Enrollment education events | |||||
| Hypertension management classes | 33.3 | 50 | 10 | 75 | .056 |
| Kickoff events, ≥7 events | 25 | 0 | 20 | 75 | .04 |
| Community partners, both new and existing partnerships | 55.6 | 0 | 70 | 75 | .02 |
| Program engagement,a mean, % (No.) | 14.1 (39) | 10.4 (15) | 11.6 (21) | 23.9 (95) | .001 |
| Engagement mechanism | |||||
| Hypertension management classes, % | 33.3 | 25 | 20 | 75 | .15 |
| Communication encourage uploads | |||||
| Face‐to‐face contact, % | 50 | 25 | 40 | 75 | .08 |
| E‐mail, % | 77.8 | 100 | 90 | 25 | .02 |
| Engagement tracking | |||||
| Paper logs | 38.9 | 0 | 40 | 75 | .11 |
Abbreviations: BP, blood pressure; SD, standard deviation.
Performing groups were defined separately for each outcome.
3.5.2. Engagement
The highest 25th sites had a mean continuous patient engagement of 37.4%, the middle 50th 10.0%, and the lowest 25th 1.1%. Compared with the lowest 25th and middle 50th sites, the highest 25th engagement sites were more likely to have hypertension management classes and face‐to‐face contact with participants, but were less likely to use e‐mails as a means of communicating the need for BP uploads (100% for the highest 25th, 90% for the middle 50th, and 25% for the lowest 25th; P=.02). Although nonsignificant, the highest 25th sites were more likely to keep backup logs of participant information, including BPs at enrollment and engagement events (Table 4).
3.5.3. BP change
The highest 25th sites experienced a −13.7 mm Hg average reduction in BP, the middle 50th a −3.3 mm Hg average reduction, and the lowest 25th a +1.1 mm Hg average increase in systolic BP. Compared with the lowest 25th and middle 50th, the highest 25th sites for systolic BP change were more likely to hold hypertension management classes and give incentives to community partners for purposes of promoting engagement (75% for the highest 25th, 25% for the middle 50th, and 0% for the lowest 25th; P=.01). Highest 25th sites for systolic BP change were also more likely to call or text participants in hopes of encouraging BP upload to Heart360 (Table 4).
3.6. Relationship of upload frequency to BP change
We analyzed whether participants who provided more frequent BP uploads experienced greater BP changes. We found that there was a significant association (P<.001) between increasing BP uploads and greater declines in systolic and diastolic BP (Figures 2 and 3). Participants with four or more BPs (n=1492) had mean systolic BP reductions of 9.9 mm Hg (SD±21.1, P<.0001) vs 7.5 mm Hg for those with fewer than four uploads (n=2092). For participants with six or more BP uploads (n=1131), BP reduction was −11.7 mm Hg. For those with eight or more uploads (n=845), the mean systolic decrease was −13.9 mm Hg (Table S3).
Figure 2.
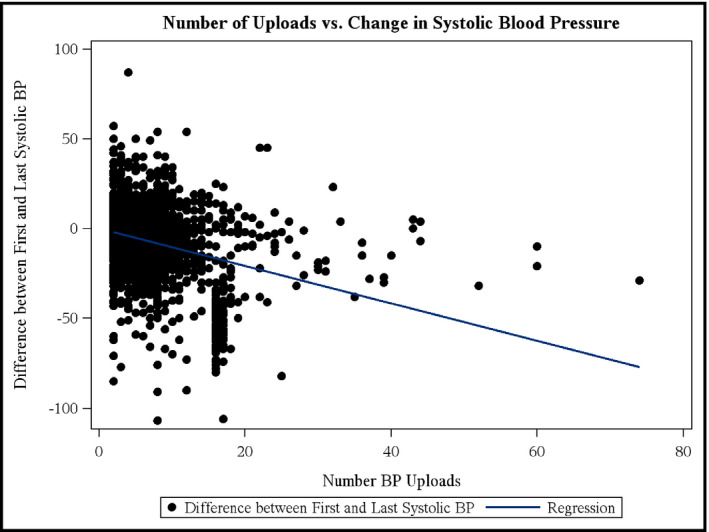
Number of uploads and change in systolic blood pressure (BP). The relationship between the number of BP uploads and change in systolic BP (first recorded to last recorded BP). Spearman correlation coefficient=−.271727, P<.0001
Figure 3.
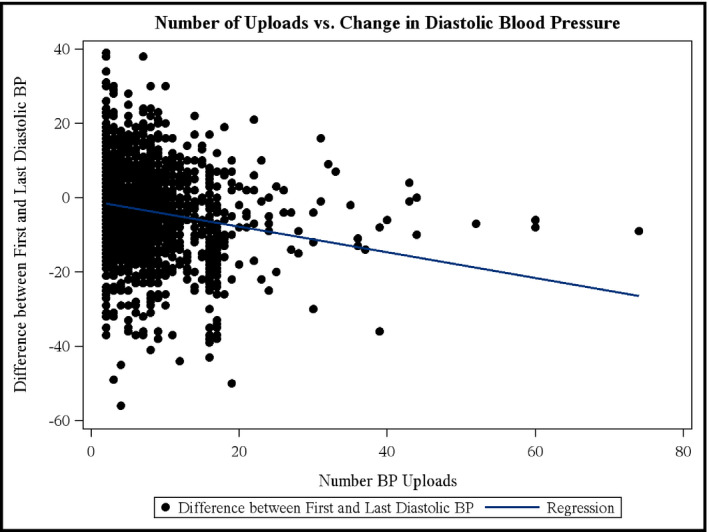
Number of uploads and change in diastolic blood pressure (BP). The relationship between the number of BP uploads and change in diastolic BP (first recorded to last recorded BP). Spearman correlation coefficient=−.17, P<.0001
4. Discussion
The AHA CCC pilot program represents a novel national implementation initiative to simultaneously lower BP levels across 18 separate US communities. The sites all used common simple practical tools and strategies but developed individual campaign customization based on local community input and opportunity. This CCC initiative achieved patient recruitment and lowered BPs. Sustained patient engagement in the campaigns was challenging, but, when achieved, engagement appeared to correlate with better BP control. Variability among campaign strategies allowed us to identify which campaign features were most associated with success.
Several prior studies have demonstrated that the use of health information technology and/or community health workers can promote improved hypertension control.9, 10, 11, 12, 13, 14, 15, 16 Yet many of these programs required significant resources, and their durability, scalability, and generalizability to other settings was unclear. The AHA's Check It, Change It program demonstrated significant BP reduction among 2000 participants from eight Durham, NC outpatient clinics over a 6‐month period. The Check It, Change It program, which cost more than $1.5 million to implement, utilized community health coaches, pharmacists, and Heart360 in partnership with physician practices to lower BP on a population level. The CCC program extends this prior work by demonstrating that: (1) community‐based implementation campaigns could be simultaneously launched across multiple diverse settings; (2) despite using modest monetary resources, the sites successfully enrolled participants and achieved BP control; and (3) program evaluation of the individual campaigns was able to identify attributes associated with more or less success. This type of implementation study is rarely conducted in community implementation programs but provides a unique opportunity to instruct future community‐based campaigns.
Historically, little research has focused on finding which specific factors are responsible for improvement in patient outcomes among those participating in community‐based hypertension programs.20, 21, 22 Using a mixed‐methods approach, we descriptively identified several campaign‐level aspects associated with the lowest‐ and highest‐performing community sites. We found that several factors were critical to improved BP control, including hypertension management education, direct and electronic participant contact (by volunteer health mentors to encourage Heart360 participation), and implementation of campaign activities at community sites frequented by participants.
The CCC program had a unique design, given that it was built on AHA's geographical staffing infrastructure; was conducted using as little as $20 000 for most programs; and was designed, implemented, and conducted in communities without significant input from researchers. Despite some underlying similarities, several sites clearly succeeded at enrolling, engaging, and lowering BPs. Other sites appeared to have less established relationships with community partners and did not successfully enroll participants, partly due to overly aggressive geographical and minority population‐specific goals set by the national office. Overall, patient engagement was a challenge, but several sites achieved modest engagement numbers. These particular sites were much more likely to use volunteer health mentors to establish relationships and personally encourage participants to upload BPs. These volunteer health mentors were also more likely to help participants log in to Heart360 accounts. Modest engagement sites were also more likely to have backup logs for BP recordings at large events, just in case demand exceeded computer capacity to enter BPs via the Heart360 Web site. More importantly, the most successful sites consistently taught participants about hypertension control and encouraged them to track their BP numbers. Despite variability among the 18 sites, the CCC program reduced BP overall. Some sites, especially those enrolling hypertensive patients and those that were able to keep patients engaged, experienced more significant declines in BP. These sites were also much more likely to stay personally engaged with participants through phone calls, face‐to‐face contact, or texts.
5. Study limitations
Our analysis has several limitations. First, this was a community‐based implementation effort with little input from researchers with regard to the conduct of CCC. However, AHA's High Blood Pressure Advisory Group, comprised of experts in hypertension research, conceived the structural design of CCC and selected sites based on grant applications mandating a specific format to keep general consistency based on proven interventions previously developed through research. Despite the limited input from researchers after the program was initiated (which was the intention of the CCC effort), our research team was able to collect objective data on enrollment, engagement, and BP change as a result of campaign participation. Second, BP data were not obtained using a standardized approach. Participants or campaign staff checked BPs using a variety of BP cuffs and uploaded them into the Heart360 system; therefore, we cannot attest to the accuracy of the BPs that were entered. Nonetheless, we did perform quality checks on the data for inaccurate BP entries, and outlier or impossible BPs were either deleted from the analysis or imputed to avoid significantly biasing the results. Third, the CCC program did not include “control” geographic communities as a part of its design; these control communities could have contributed to a more accurate estimate of the impact of the AHA CCC program. However, the goal was distinct from a traditional research study, and was primarily meant to understand the impact of 18 simultaneous real‐word hypertension programs. Fourth, the relationship between greater engagement and greater BP reduction change may have in part been due to bias from BP regression to the mean and healthy adherer effects. Although, if healthy adherer effects played a role, we would expect that traditionally nonadherent populations would be expected to have a greater effect. Fifth, we did not have participant information on medical history of hypertension or other comorbidities, socioeconomic status, participant family support, physician visits, changes in antihypertensive medication regimen, or medical history of hypertension or other comorbidities—any of which could have confounded the relationship between CCC and improved BP. We expect that future campaigns will collect and evaluate how these data may contribute to BP outcomes. Sixth, race and ethnicity data in Heart360 were missing in 59% of participants. Finally, while we believe the AHA CCC program is generalizable, we acknowledge that the AHA field staff played a critical role in overseeing the development of each geographic program. The cost of the AHA staff are not accounted for in this analysis.
6. Conclusions
CCC was a novel community‐based initiative that demonstrated reduction in BP among 18 community sites. Future efforts could focus on modeling the implementation features of top‐performing sites. We have identified several factors associated with campaign BP improvement that may guide future implementation of such initiatives in other communities.
Conflict of interest
Dr Anderson reports no relevant disclosures. Dr Peragallo‐Urrutia reports no relevant disclosures. Dr O'Brien reports research funding from Janssen, BMS, GSK, and Merck, and serves on the advisory board for Portola. Dr Allen LaPointe reports no relevant disclosures. Ms Crawford reports employment with the American Heart Association. Mr Christian reports no relevant disclosures. Ms McCoy reports no relevant disclosures. Ms Webb reports no relevant disclosures. Ms Alexander reports no relevant disclosures. Dr Saha‐Chaudhuri reports no relevant disclosures. Mr Wayte reports employment with the American Heart Association. Dr Peterson reports research funding for the American College of Cardiology, American Heart Association, Eli Lilly & Company, Janssen Pharmaceuticals, and the Society of Thoracic Surgeons (all significant); and consulting (including CME) for Merck & Co (modest), Boehringer Ingelheim, Genentech, Janssen Pharmaceuticals, and Sanofi‐Aventis (all significant).
Supporting information
Acknowledgments
The authors would like to acknowledge and thank the AHA market directors, volunteer health mentors, and community partners who made the Check. Change. Control. program possible. We also thank the AHA's High Blood Pressure Science Advisory Group for conceiving the idea of the Check. Change. Control. program. The authors would like to thank Erin Hanley, MS, for her editorial contributions to this manuscript. Ms Hanley has not received compensation for her contributions, apart from their employment at the institution where this study was conducted. Ms Hanley is an employee of the Duke Clinical Research Institute, Duke University Medical Center, Durham, NC.
Anderson ML, Peragallo Urrutia R, O'Brien EC, et al. Outcomes of a multi-community hypertension implementation study: the American Heart Association's Check. Change. Control. program. J Clin Hypertens. 2017;19:479–487. 10.1111/jch.12950
Funding information
The Check. Change. Control. program was funded by the American Heart Association. The analysis of Check. Change. Control. was supported in part by the American Heart Association and the Duke Clinical Research Institute.
References
- 1. Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. [DOI] [PubMed] [Google Scholar]
- 2. Lloyd‐Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 3. Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist‐led, American Heart Association Heart360 Web‐enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes. 2013;6:157–163. [DOI] [PubMed] [Google Scholar]
- 4. Thomas KL, Shah BR, Elliot‐Bynum S, et al. Check it, change it: a community‐based, multifaceted intervention to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2014;7:828–834. [DOI] [PubMed] [Google Scholar]
- 5. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook, 3rd edn. Thousand Oaks, CA: SAGE Publications, Inc.; 2014. [Google Scholar]
- 6. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Transaction Publishers; 1967. [Google Scholar]
- 7. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research, 2nd Edition. Thousand Oaks, CA: SAGE Publications, Inc.; 2011. [Google Scholar]
- 8. Teddlie C, Tashakkori A. Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences. Thousand Oaks, CA: SAGE Publications, Inc.; 2009. [Google Scholar]
- 9. Victor RG, Ravenell JE, Freeman A, et al. A barber‐based intervention for hypertension in African American men: design of a group randomized trial. Am Heart J. 2009;157:30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Green BB, Ralston JD, Fishman PA, et al. Electronic communications and home blood pressure monitoring (e‐BP) study: design, delivery, and evaluation framework. Contemp Clin Trials. 2008;29:376–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. BMJ. 2005;331:493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brownstein JN, Chowdhury FM, Norris SL, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32:435–447. [DOI] [PubMed] [Google Scholar]
- 13. Zoellner J, Connell C, Madson MB, et al. HUB city steps: a 6‐month lifestyle intervention improves blood pressure among a primarily African‐American community. J Acad Nutr Diet. 2014;114:603–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dye CJ, Wililams JE, Evatt JH. Improving hypertension self‐management with community health coaches. Health Promot Pract. 2015;16:271–281. [DOI] [PubMed] [Google Scholar]
- 15. Banack HR, Grover S, Kaouche M, Marchand S, Lowensteyn I. The MyHealthCheckup study: training graduate students to implement cardiovascular risk screening programs in community pharmacies. Can Pharm J (Ott). 2012;145:268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Williams LB, Franklin B, Evans MB, Jackson C, Hill A, Minor M. Turn the beat around: a stroke prevention program for African‐American churches. Public Health Nurs. 2016;33:11–20. [DOI] [PubMed] [Google Scholar]
- 17. Dodani S, Beayler I, Lewis J, Sowders LA. HEALS hypertension control program: training church members as program leaders. Open Cardiovasc Med J. 2014;8:121–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aycock DM, Kirkendoll KD, Gordon PM. Hypertension education and screening in African American churches. J Community Health Nurs. 2013;30:16–27. [DOI] [PubMed] [Google Scholar]
- 19. Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to control hypertension: cluster‐randomized clinical trial main effects. Circulation. 2014;129:2044–2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morgado M, Rolo S, Castelo‐Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm. 2011;33:132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lu Z, Cao S, Chai Y, et al. Effectiveness of interventions for hypertension care in the community–a meta‐analysis of controlled studies in China. BMC Health Serv Res. 2012;12:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ferrara AL, Pacioni D, Di Fronzo V, et al. Lifestyle educational program strongly increases compliance to nonpharmacologic intervention in hypertensive patients: a 2‐year follow‐up study. J Clin Hypertens (Greenwich). 2012;14:767–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


