Abstract
The purpose of this study was to assess the effects of renin‐angiotensin system (RAS) inhibitors vs other antihypertensive agents on cardiovascular outcomes in hypertensive black patients. The authors performed a systematic review and meta‐analysis of studies that compared the effects of angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) with calcium channel blockers (CCBs), diuretics, and β‐blockers in hypertensive black patients on cardiovascular outcomes. A total of 38,983 patients with a mean age of 60 years and mean follow‐up of 4 years were included in our meta‐analysis. No significant differences were found in all‐cause mortality, myocardial infarction, heart failure, and cardiovascular mortality rates among patients treated with RAS inhibitors compared with CCBs, diuretics, and β‐blockers. The incidence of stroke was significantly increased in patients treated with RAS inhibitors compared with CCBs (odds ratio, 1.56; 95% confidence interval, 1.31–1.87 [P<.00001]; I 2=0%) and diuretics (odds ratio, 1.59; 95% confidence interval, 1.16–2.17 [P=.004]; I 2=56%) but not β‐blockers.
Hypertension (HTN) in African Americans is often more severe and resistant to antihypertensive therapy and leads to earlier target organ damage and higher cardiovascular (CV) events compared with whites.1, 2, 3 Response to antihypertensive drug classes may be different among different age and race subgroups. Black and elderly patients exhibit better blood pressure (BP) response to thiazide diuretics or long‐acting calcium channel blockers (CCBs), provided they don't have a specific indication for angiotensin‐converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) such as heart failure (HF) or proteinuric chronic kidney disease.4 In contrast, younger white patients respond better to ACE inhibitors or ARBs.4, 5, 6 The observed differences may be the result of lower plasma renin activity in hypertensive blacks.7 A recent analysis of New York City Health and Hospital Corporation's clinical data showed significantly higher all‐cause mortality and myocardial infarction (MI) rates in hypertensive blacks treated with ACE inhibitors.8 We sought to review and analyze CV outcomes in hypertensive blacks treated with different antihypertensive classes.
Methods
Search Strategy
Systematic electronic search was performed on MEDLINE (PubMed interface), Embase, and Cochrane Central Registry of Controlled Trials (CENTRAL) with no language limitations. Using the MESH terms, we searched the following key terms: hypertension, blacks, angiotensin‐converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, diuretics, and β‐blockers. Two reviewers (M.P. and A.B.) independently screened titles and abstracts based on inclusion and exclusion criteria. After eliminating irrelevant studies, full‐text reports were reviewed. Review articles were excluded. Subsequently, we performed a hand search of all included randomized clinical trials and observational studies until no further relevant studies were identified. Finally, a total of four studies were identified.
Study Selection
We included randomized clinical trials and observational studies published as original articles in peer‐reviewed scientific journals. We studied hypertensive blacks who were treated with ACE inhibitors or ARBs compared with CCBs, diuretics, and β‐blockers. We excluded studies that were performed in nonblacks.
Outcomes Assessed
The primary outcomes measured were all‐cause mortality, MI, stroke, HF, and CV mortality. The secondary outcome measured was the composite outcome of all‐cause mortality, MI, stroke and HF.
Data Extraction and Quality
The data were independently extracted by two authors (M.P. and A.B.) using standardized protocol and reporting form. We extracted outcome measures data; study characteristics such as trial design, year of study, sample size, inclusion criteria and exclusion criteria, primary and secondary outcomes, and follow‐up duration; and baseline patient characteristics.
Risk of Bias
Cochrane's risk of bias tool was used to assess the individual risk of bias of each study. The Newcastle‐Ottawa tool was used for the quality assessment of cohort studies. Low‐quality studies had two or more quality assessment criteria qualified as high or unclear risk of bias. The small study effect, including publication bias, was tested using funnel plot and the Egger's test.
Data Analysis, Summary Measures, and Synthesis of Results
Systematic review and meta‐analysis was performed in compliance with the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) Statement. Meta‐analysis was performed by using Review Manager (RevMan) Version 5.2 (Nordic Cochrane Centre, The Cochrane Collaboration, 2012, Copenhagen, Denmark). Chi‐square test of heterogeneity and I 2 statistic of inconsistency were used to assess the heterogeneity between studies. I 2 values of 25%, 50%, and 75% were considered as low, moderate, and high heterogeneity, respectively.9 Significant heterogeneity was considered if the P<.05 or an I 2 statistic >25%. Pooled effect of intervention was measured using odds ratios (ORs) with 95% confidence intervals (CIs). DerSimonian and Laird's random‐effects model was used. Reported values are two‐tailed, and hypothesis‐testing results were considered statistically significant at P<.05. Significant heterogeneity between the studies was further explored using subgroup analyses.
Results
Study Selection
After electronic search of scientific literature with omission of duplicate trials and screening of titles followed by review of abstracts and full texts, four studies were identified and included in the meta‐analysis based on inclusion and exclusion criteria.8, 9, 10, 11 Of the four studies, three were subgroup analyses of randomized control trials 9, 10, 11 and one was a propensity‐matched cohort analysis.8 ACE inhibitors were compared with CCBs in the African American Study of Kidney Disease and Hypertension (AASK) trial,11 the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) trial,10 and Bangalore and colleagues8 diuretics in the ALLHAT trial10 and Bangalore and colleagues8 and β‐blockers in the AASK trial,11 Bangalore and colleagues, and the Losartan Intervention For Endpoint Reduction (LIFE) study.9 All included studies were deemed to be at low risk of bias.
Study Characteristics
A total of 38,983 patients with a mean age of 60 years and mean follow‐up of 4 years were included in our meta‐analysis. The characteristics of each study are shown in the Table. Baseline BP and BP reduction were not available in all studies. Because of variability in study design, baseline BP, and BP reduction among studies, we did not perform a separate meta‐analysis of these BP variables.
Table 1.
Interventions and Characteristics of Individual Studies
| Study | Study Design | Mean Age, y | Mean Follow‐Up Period | Antihypertensive Agent | Sample Size | Mean Follow‐Up, y | Mean Baseline BP, mm Hg | Mean Change of BP, mm Hg | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACE Inhibitor | CCB | Diuretic | BB | ACE Inhibitor | CCB | Diuretic | BB | |||||||
| LIFE Study (2004) | Randomized clinical trial | 65 | 4.8 y | Losartan/atenolol | 270/263 | 4.8 | 172/97.9 | – | – | 171.8/97.7 | −30.3/17.3 | – | – | −29.1/−17.2 |
| ALLHAT study (2005) | Randomized clinical trial | 66 | 4 y | Lisinopril/amlodipine/chlorthalidone | 3210/5369/3213 | 4 | 146.2/84.9 | 146.1/84.7 | 146.3/84.9 | – | −6.8/−5.6 | −8.8/−6.6 | −10.5/−6.6 | – |
| AASK trial (2006) | Randomized clinical trial | 55 | 4.1 y | Ramipril/amlodipine/metoprolol | 436/217/441 | 4.1 | 151/96 | 150/96 | – | 150/95 | −16/−14 | −17/−15 | – | −15/−14 |
| Bangalore et al. (2015) | Propensity match cohort | 50 | 6 mo | ACE/CCB/diuretic/BB | Total sample 25,564 | 6 | 144/83 | 153/87 | 148/85 | 138/80 | – | – | – | – |
Abbreviations: AASK, African American Study of Kidney Disease and Hypertension trial; ACE, angiotensin‐converting enzyme; ALLHAT, Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial; BB, β‐blocker; BP, blood pressure; CCB, calcium channel blocker; LIFE, Losartan Intervention For Endpoint Reduction trial.
RAS Inhibitors vs CCBs
No significant differences were found in all‐cause mortality (Figure 1a), MI (Figure 1b), HF (Figure 1d), and CV mortality rates when ACE inhibitors were compared with CCBs. However, the incidence of stroke was significantly increased in patients treated with ACE inhibitors (OR, 1.56; 95% CI, 1.31–1.87 [P<.00001]; I 2=0%) without significant heterogeneity among studies (Figure 1c). There was a trend towards significantly increased composite outcome with ACE inhibitors (OR, 1.27; 95% CI, 1.00–1.62 [P=.05]; I 2=79%) with significant heterogeneity among studies (Figure 1e). After the exclusion of the cohort study by Bangalore and colleagues, the association between treatment of ACE inhibitors and composite CV outcome became significant (OR, 1.14;95% CI, 1.03–1.25 [P=.01]; I 2=0%).
Figure 1.
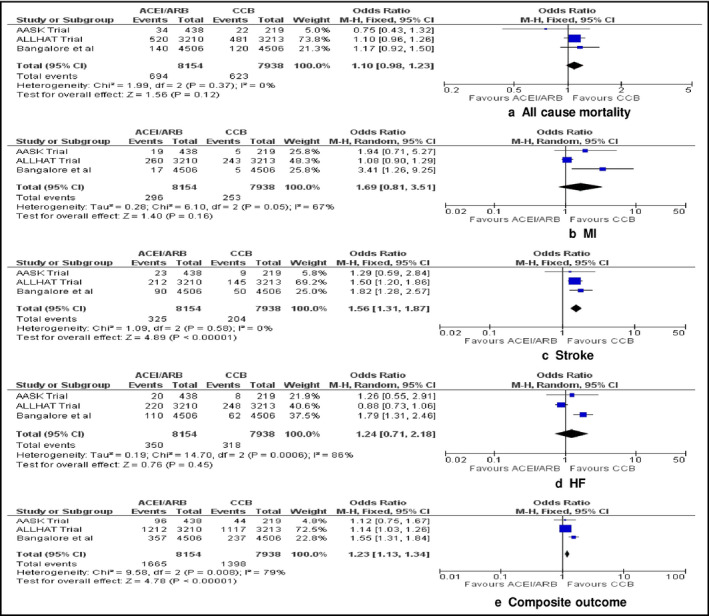
Random‐effect meta‐analysis of the effects of renin‐angiotensin system (RAS) inhibitors vs calcium channel blockers (CCBs) on all‐cause mortality, myocardial infarction, stroke, heart failure, and composite outcome. The figure presents number of events, number of patients in the treatment and control groups, odds ratio (OR) and 95% confidence interval (CI) for each trial, overall OR estimate with 95% CI and P value for association test, P value for heterogeneity test, and between‐trial inconsistency (I 2) measures. ACEI/ARB indicates angiotensin‐converting enzyme inhibitor/angiotensin receptor blocker.
RAS Inhibitors vs Diuretics
We did not detect any significant difference in all‐cause mortality (Figure 2a), MI (Figure 2b), HF (Figure 2d), and CV mortality rates when ACE inhibitors were compared with thiazide diuretics. The stroke rates were significantly higher in patients treated with ACE inhibitors (OR, 1.59; 95% CI, 1.16–2.17 [P=.004]; I 2=56%) (Figure 2c) without significant heterogeneity among studies. A trend towards increased composite CV outcomes was observed (P=.05) (Figure 2e).
Figure 2.
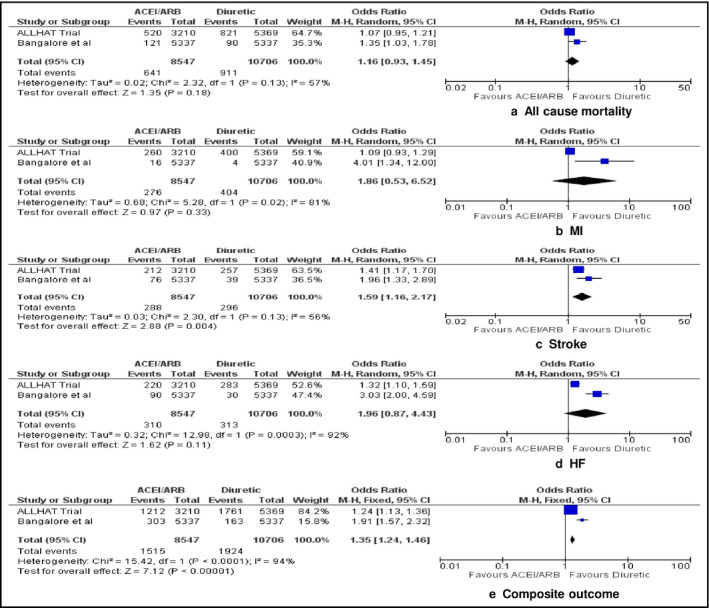
Random‐effect meta‐analysis of the effects of renin‐angiotensin system (RAS) inhibitors vs diuretics on all‐cause mortality, myocardial infarction, stroke, heart failure, and composite outcome. The figure presents number of events, number of patients in the treatment and control groups, odds ratio (OR) and 95% confidence interval (CI) for each trial, overall OR estimate with 95% CI and P value for association test, P value for heterogeneity test, and between‐trial inconsistency (I 2) measures. ACEI/ARB indicates angiotensin‐converting enzyme inhibitor/angiotensin receptor blocker.
RAS Inhibitors vs β‐Blockers
No significant differences were found in all‐cause mortality (Figure 3a), MI (Figure 3b), stroke (Figure 3c), HF (Figure 3d), and CV mortality when RAS inhibitors were compared with β‐blockers. However, there was a significantly increased composite outcome with RAS inhibitors (OR, 1.20; 95% CI, 1.03–1.40 [P=.02]; I 2=81%) with significant heterogeneity among studies (Figure 3e). As certain side effects such as cough and angioedema are more frequent with ACE inhibitors than ARBs and may lead to differences in medication adherence, we performed subgroup analysis of studies with ACE inhibitors only with exclusion of the LIFE study. No significant differences in all‐cause mortality, MI, stroke, HF, CV mortality, and composite outcome were found between groups.
Figure 3.
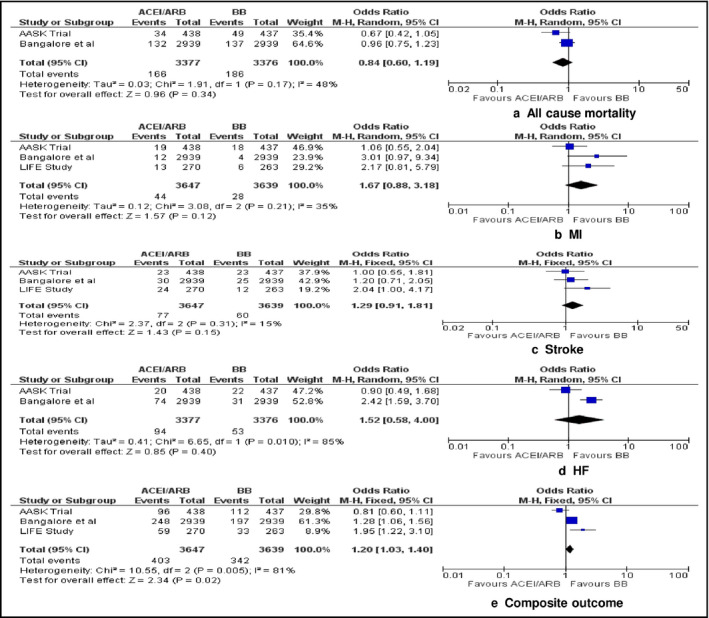
Random‐effect meta‐analysis of the effects of renin‐angiotensin system (RAS) inhibitors vs β‐blockers on all‐cause mortality, myocardial infarction, stroke, heart failure, and composite outcome. The figure presents number of events, number of patients in the treatment and control groups, odds ratio (OR) and 95% confidence interval (CI) for each trial, overall OR estimate with 95% CI and P value for association test, P value for heterogeneity test, and between‐trial inconsistency (I 2) measures. ACEI/ARB indicates angiotensin‐converting enzyme inhibitor/angiotensin receptor blocker.
The funnel plot did not show asymmetry consistent with publication bias, and the Egger's test was not significant for the outcomes studied.
Discussion
Our meta‐analysis compared the effects of RAS inhibitors with other main classes of antihypertensive agents in hypertensive blacks and showed no significant difference in all‐cause mortality, MI, HF, and CV death among patients treated with RAS inhibitors, CCBs, diuretics, and β‐blockers. The incidence of stroke was higher in patients treated with ACE inhibitors compared with CCBs and diuretics.
Hypertensive blacks are considered to have suppressed plasma renin activity and dietary salt‐induced suppression of renin production and fit the Laragh and Sealey model of volume‐expanded hypertension.12 However, prior studies have not confirmed this perception as they showed higher RAS activation and blunted suppression of intrarenal RAS activity compared with whites after high sodium intake.12, 13, 14 Hypertensive blacks are more likely to be obese; have higher apnea‐hypopnea index, dietary salt intake, and salt sensitivity; and lower dietary intake of potassium and socioeconomic status compared with hypertensive whites.15 These confounding factors may explain differential interracial response to specific antihypertensive classes. Although high sodium intake is associated with less BP response to ACE inhibitors among all races, blacks with higher sodium intake exhibit consistently less BP reduction when treated with ACE inhibitors.16 However, the intraracial variability of BP response to monotherapy with RAS inhibitors is greater that the interracial variability.17 Based on the above we can conclude that race differences in BP response to RAS inhibitors are the result of differences in individual baseline characteristics rather than a single pathophysiologic mechanism.
A previous meta‐analysis of 13 clinical trials showed that ACE inhibitor monotherapy was associated with 4.6/2.8 mm Hg less BP reduction compared with other antihypertensives, with ACE inhibitor dose being the only factor mitigating the BP difference.18 These differences in BP response were similar to those reported by the ALLHAT trial.10 The BP data provided by individual studies were not sufficient for accurate meta‐analysis of BP reduction. Furthermore, the medication regimens and doses differ in each study. Therefore, the heterogeneity among studies would be a limiting factor for meta‐analysis of BP reduction. However, the currently available data suggest that the differences in stroke rates were driven mainly by the ALLHAT trial and the study by Bangalore and colleagues. Although the analysis by Bangalore and colleagues did not provide BP data, the ALLHAT trial showed poorer BP control with lisinopril compared with amlodipine and chlorthalidone. Therefore, the most likely explanation for the differences in stroke rates is less BP reduction with ACE inhibitor/ARBs monotherapy.
Both ACE inhibitors and ARBs seem to have anti‐inflammatory effects. A prospective controlled double‐blind study of hypertensive patients suggested that treatment with olmesartan significantly reduced a panel of inflammation markers (high‐sensitivity C‐reactive protein, tumor necrosis factor α, and interleukin 6) compared with controls.19 In a smaller randomized controlled trial of 21 hypercholesterolemic volunteers, both enalapril and losartan induced a small but stable decrease in levels of adhesion molecules.20 However, these mild anti‐inflammatory effects observed in a small number of patients may not have meaningful impact on stroke rates and CV outcomes if not accompanied by significant BP reduction.21
One of the main reasons RAS antagonists may be less effective antihypertensive agents in African Americans is the different dose response compared with whites.22 African Americans require higher doses of ACE inhibitors to achieve equivalent reductions in BP with whites.23 Furthermore, since hypertensive blacks are likely to require more than a single antihypertensive, the use of combination therapy including an ACE inhibitor or ARB effectively decreases BP and CV events24 and the combination with a diuretic may eliminate race‐specific differences in dose response.23 In addition, as the AASK trial results demonstrated, hypertensive blacks with target organ damage such as chronic kidney disease or HF may benefit from ACE inhibitors more than other hypertensive classes in spite of lesser BP reduction.11 Although we did not observe significant differences in HF between ACE inhibitors/ARBs and CCBs, the use of the latter as monotherapy should be discouraged in patients with reduced left ventricular function.
It is unclear whether ACE inhibitors and ARBs have similar effects on BP reduction in hypertensive blacks. The LIFE study showed that hypertensive blacks did not respond as favorably to losartan‐based treatment as nonblack patients with respect to CV outcomes despite greater electrocardiographic left ventricular hypertrophy reduction with losartan compared with atenolol.11 In our study, the sensitivity analysis of studies with ACE inhibitors after exclusion of the LIFE study, showed similar outcomes with ACE inhibitors and β‐blockers.
Study Limitations
There are some limitations to the interpretation of our data analysis. First, publication bias may still exist despite our best efforts to conduct a comprehensive search and the lack of statistical evidence for the existence of bias. Second, any meta‐analysis based on pooling of data from different trials with different inclusion criteria, different designs and populations, and variable follow‐up duration with differing attrition rates presents challenges. The antihypertensive regimens and dosages used in individual studies were also different and may have differential effects on outcomes. Third, the ability of the analyses to detect differences between regimens would have been diminished by incomplete adherence to assigned treatments and the extensive use of add‐on therapies. Fourth, outcomes evaluated here were not available as prespecified criteria or primary outcomes in all eligible trials. Fifth, we included mainly US‐based trials, thus our results may not be applicable to other black populations such as African blacks, representing different patterns of CV risk. Lastly, absence of analysis on BP reduction limits the interpretation of the differences in stroke rates.
Conclusions
This is a hypothesis‐generating analysis demonstrating similar effects of RAS inhibitors on all‐cause mortality, MI, HF, and CV mortality compared with CCBs and diuretics but higher stroke rates. The difference in stroke may be the result of lesser BP reduction with RAS inhibition as a consequence of interracial differences in sodium intake, salt sensitivity, and comorbid conditions. Therefore, future trials should specifically investigate baseline characteristics that lead to BP response variability and potentially to higher stroke rates with RAS inhibitor monotherapy.
Acknowledgment and Disclosure
The authors have no acknowledgments or conflicts of interest to declare and no funding for the current work. No ethical approval was needed.
J Clin Hypertens (Greenwich). 2017;19:344‐350. DOI: 10.1111/jch.12867. © 2016 Wiley Periodicals, Inc.
References
- 1. Flack JM, Sica DA, Bakris G, et al. Management of high blood pressure in Blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56:780–800. [DOI] [PubMed] [Google Scholar]
- 2. Brewster LM, van Montfrans GA, Kleijnen J. Systematic review: antihypertensive drug therapy in black patients. Ann Intern Med. 2004;141:614–627. [DOI] [PubMed] [Google Scholar]
- 3. Jolly S, Vittinghoff E, Chattopadhyay A, Bibbins‐Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. Am J Med. 2010;123:811–818. [DOI] [PubMed] [Google Scholar]
- 4. Materson BJ, Reda DJ, Cushman WC, et al. Single‐drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med. 1993;328:914–921. [DOI] [PubMed] [Google Scholar]
- 5. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 6. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 7. Blaufox MD, Lee HB, Davis B, et al. Renin predicts diastolic blood pressure response to nonpharmacologic and pharmacologic therapy. JAMA. 1992;267:1221–1228. [PubMed] [Google Scholar]
- 8. Bangalore S, Ogedegbe G, Gyamfi J, et al. Outcomes with angiotensin‐converting enzyme inhibitors vs other antihypertensive agents in hypertensive blacks. Am J Med. 2015;128:1195–1203. [DOI] [PubMed] [Google Scholar]
- 9. Julius S, Alderman MH, Beevers G, et al. Cardiovascular risk reduction in hypertensive black patients with left ventricular hypertrophy: the LIFE study. J Am Coll Cardiol. 2004;43:1047–1055. [DOI] [PubMed] [Google Scholar]
- 10. Wright JT Jr, Dunn JK, Cutler JA, et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005;293:1595–1608. [DOI] [PubMed] [Google Scholar]
- 11. Norris K, Bourgoigne J, Gassman J, et al. Cardiovascular outcomes in the African American Study of Kidney Disease and Hypertension (AASK) Trial. Am J Kidney Dis. 2006;48:739–751. [DOI] [PubMed] [Google Scholar]
- 12. Alderman MH, Cohen HW, Sealey JE, Laragh JH. Plasma renin activity levels in hypertensive persons: their wide range and lack of suppression in diabetic and in most elderly patients. Am J Hypertens. 2004;17:1–7. [DOI] [PubMed] [Google Scholar]
- 13. Price DA, Fisher ND, Osei SY, et al. Renal perfusion and function in healthy African Americans. Kidney Int. 2001;59:1037–1043. [DOI] [PubMed] [Google Scholar]
- 14. Price DA, Fisher ND, Lansang MC, et al. Renal perfusion in blacks: alterations caused by insuppressibility of intrarenal renin with salt. Hypertension. 2002;40:186–189. [DOI] [PubMed] [Google Scholar]
- 15. Flack JM, Staffileno BA. Hypertension in blacks. In: Johnson R, ed. Comprehensive Clinical Nephrology. London, UK: Mosby International; 1998. [Google Scholar]
- 16. Weir MR, Chrysant SG, McCarron DA, et al. Influence of race and dietary salt on the antihypertensive efficacy of an angiotensin‐converting enzyme inhibitor or a calcium channel antagonist in salt‐sensitive hypertensives. Hypertension. 1998;31:1088–1096. [DOI] [PubMed] [Google Scholar]
- 17. Mokwe E, Ohmit SE, Nasser SA, et al. Determinants of blood pressure response to quinapril in black and white hypertensive patients: the Quinapril Titration Interval Management Evaluation Trial. Hypertension. 2004;43:1202–1207. [DOI] [PubMed] [Google Scholar]
- 18. Peck RN, Smart LR, Beier R, et al. Difference in blood pressure response to ACE‐inhibitor monotherapy between black and white adults with arterial hypertension: a meta‐analysis of 13 clinical trials. BMC Nephrol. 2013;14:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fliser D, Buchholz K, Haller H; EUropean Trial on Olmesartan and Pravastatin in Inflammation and Atherosclerosis (EUTOPIA) Investigators . Antiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammation. Circulation. 2004;110:1103–1107. [DOI] [PubMed] [Google Scholar]
- 20. Graninger M, Reiter R, Drucker C, et al. Angiotensin receptor blockade decreases markers of vascular inflammation. J Cardiovasc Pharmacol. 2004;44:335–339. [DOI] [PubMed] [Google Scholar]
- 21. Sica D. Are there pleiotropic effects of antihypertensive medications or is it all about the blood pressure in the patient with diabetes and hypertension? J Clin Hypertens (Greenwich). 2011;13:301–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Weir MR, Saunders E; Trandolapril Multicenter Study Group . Renin status does not predict the anti‐hypertensive response to angiotensin‐converting enzyme inhibition in African‐Americans. J Hum Hypertens 1998;12:189–194. [DOI] [PubMed] [Google Scholar]
- 23. Flack J, Mensah GA, Ferrario CM. Using angiotensin converting enzyme inhibitors in African‐American hypertensives: a new approach to treating hypertension and preventing target‐organ damage. Curr Med Res Opin. 2000;16:66–79. [PubMed] [Google Scholar]
- 24. Weir MR, Bakris GL, Weber MA, et al. Renal outcomes in hypertensive black patients at high cardiovascular risk. Kidney Int. 2012;81:568–576. [DOI] [PubMed] [Google Scholar]


