Abstract
The recent American hypertension guidelines recommended a threshold of 130/80 mmHg to define hypertension on the basis of office, home or ambulatory blood pressure (BP). Despite recognizing the potential advantages of automated office (AO)BP, the recommendations only considered conventional office BP, without providing supporting evidence and without taking into account the well documented difference between office BP recorded in research studies versus routine clinical practice, the latter being about 10/7 mmHg higher. Accordingly, we examined the relationship between AOBP and awake ambulatory BP, which the guidelines considered to be a better predictor of future cardiovascular risk than office BP. AOBP readings and 24‐hour ambulatory BP recordings were obtained in 514 untreated patients referred for ambulatory BP monitoring in routine clinical practice. The relationship between mean AOBP and mean awake ambulatory BP was examined using linear regression analysis with and without adjustment for age and sex. Special attention was given to the thresholds of 130/80 and 135/85 mmHg, the latter value being the recognized threshold for defining hypertension using awake ambulatory BP, home BP and AOBP in other guidelines. The mean adjusted AOBP of 130/80 and 135/85 mmHg corresponded to mean awake ambulatory BP values of 132.1/81.5 and 134.4/84.6 mmHg, respectively. These findings support the use of AOBP as the method of choice for determining office BP in routine clinical practice, regardless of which of the two thresholds are used for diagnosing hypertension, with an AOBP of 135/85 mmHg being somewhat closer to the corresponding value for awake ambulatory BP.
Keywords: ambulatory blood pressure, blood pressure measurement, hypertension diagnosis, regression analysis
1. INTRODUCTION
The recent guidelines of the American College of Cardiology/American Heart Association (ACC/AHA) recommended a new blood pressure (BP) threshold of ≥130/80 mmHg for diagnosing hypertension.1 This threshold was applied to office BP, awake ambulatory (A)BP and home BP. In other guidelines,2, 3 the threshold for office BP is 140/90 mmHg which is 5/5 mmHg higher than the corresponding value for awake ABP and home BP. The threshold of 135/85 mmHg for defining hypertension with awake ABP is based on clinical outcome data,4 whereas the threshold of 130 mmHg for office BP was based upon studies in which patients with readings taken in an office or clinic setting at this lower level seemed to benefit from antihypertensive drug therapy.
The American guidelines1 also did not distinguish between a research quality BP recorded according to standard BP measurement guidelines and a BP reading obtained in routine clinical practice. The mean routine office BP is about 10/7 mmHg higher than a research quality office BP reading and about 15/8 mmHg higher than the mean awake ABP.5 Nonetheless, the ACC/AHA guidelines have proposed the same threshold (130/80 mmHg) for both office BP and awake ABP.
Although the ACC/AHA guidelines recommended conventional (manual or electronic) methods for recording office BP by clinic staff, they also expressed support for automated office (AO)BP measurement, which involves taking three to five readings with a fully automated oscillometric sphygmomanometer, while the patient rests alone in a quiet place. AOBP is also the preferred method for office BP in the evidence‐based Hypertension Canada guidelines.3 AOBP devices differ from other oscillometric sphygmomanometers which require activation by either the health professional or patient immediately before the first reading is recorded, a technique sometimes referred to as “attended AOBP.” Since mean awake ABP is 15/8 mmHg lower than mean routine office BP, when recorded either manually or electronically, it is of interest to examine the relationship between the awake ABP and AOBP at the threshold for diagnosing hypertension in routine clinical practice. Until now, comparisons between AOBP and awake ABP have mostly involved a comparison of mean BP values in hypertensive patients who were already receiving antihypertensive drug therapy.
Accordingly, we have conducted a linear least squares regression analysis to compare awake ABP with AOBP readings obtained in untreated patients in routine clinical practice to assess the relationship between these two techniques for BP measurement over a wide range of readings, with special attention given to an AOBP of 130/80 and 135/85 mmHg, the thresholds for diagnosing hypertension using ambulatory BP monitoring (ABPM) in the new American guidelines1 and in Europe and Canada,2, 3 respectively.
2. METHODS
2.1. Patient population and procedures
Subjects for this study were recruited from two separate patient populations, referrals to the Sunnybrook Health Sciences Centre (Toronto, ON, Canada) ABPM monitoring unit and referrals to a community‐based hypertension specialist for ABPM and/or consultation (Kingston, ON, Canada). All participants were untreated for hypertension. In both centers, AOBP and 24‐hour ABPM were performed as part of routine clinical practice and not in the context of a research study. As a result, study participants were not told of their participation in a research study and were not required to provide informed consent. All patient data were collected prospectively and data used for statistical analysis was anonymized.
At the Sunnybrook Health Sciences ABPM unit, patients had their AOBP recorded prior to undergoing 24‐hour ABPM using a BpTRU model 100, which took an initial test BP reading in the presence of the ABPM technician followed by five readings at 1 or 2 minute intervals with the patients resting alone in a separate room. There was no additional rest period before the first BP reading. The mean of the last five readings was automatically averaged by the BpTRU device and the resulting AOBP value was noted. ABPM was obtained on a weekday using a Spacelabs model 90207 monitor with the patients instructed to engage in their usual daily activities. Readings were taken at 15 minute intervals between 0800‐2200 h and every 30 minute during the night. Mean awake ABP was calculated from the subject’s actual awake period as recorded in a diary. Additional details of the procedures followed have been published previously.6
Subjects referred for 24‐hour ABPM to the community‐based cardiac and hypertension specialty center at the Kingston Heart Clinic routinely had their AOBP measured upon arrival, using the BpTRU. In this instance, readings were recorded in the patient waiting area, with the subjects seated alone and without any conversation. The mean of the five AOBP readings was obtained as noted above. At the end of the visit, ABPM recordings were initiated with readings recorded every 30 minute from 0700 to 2200 h (awake ABP) and at 60 minute intervals during the night (asleep ABP) using a Spacelabs 90207 monitor (Spacelabs Healthcare, Snoqualmie, WA, USA). Details of the procedures followed have been published previously.7
2.2. Statistical analysis
Descriptive statistics for demographic characteristics, AOBP and awake ABP were calculated for all subjects and for each group individually. Differences between BP readings were examined using Student’s Paired t‐test and Pearson’s correlation. Linear ordinary least squares regression models were estimated separately and combined for each group, in which ABP was regressed on AOBP alone and adjusted for age and gender. The statistical analyses were performed using SPSS version 24.0 software (SPSS Inc, Chicago, IL, USA) for Macintosh. A two‐tailed P < 0.05 was considered as the significant level for all analyses.
3. RESULTS
Demographic data for the study participants and for each of the two groups separately are shown in Table 1. There were 254 subjects at the Sunnybrook Health Sciences Centre site and 260 at the Kingston Heart Clinic. Overall, mean systolic AOBP (141.7 ± 16.8) in the 514 participants was higher (mean difference 4.3, 95% CI 3.1‐5.5; P < 0.001) than the mean awake ABP (137.4 ± 12.6). For the 254 Sunnybrook patients, the mean systolic AOBP was 140.6 ± 14.9/84.6 ± 11.0 mmHg compared to a mean awake ABP of 135.3 ± 12.4/81.0 ± 10.2 mmHg (P < 0.001/P < 0.001). For the 260 Kingston Heart Clinic patients, the mean systolic AOBP was 142.6 ± 18.4/85.6 ± 10.1 mmHg compared to a mean awake ABP of 139.4 ± 12.6/82.9 ± 9.4 mmHg (P < 0.001/P = 0.001).
Table 1.
Descriptive statistics of study participants
| Variable |
Kingston n = 260 |
Sunnybrook n = 254 |
Overall n = 514 |
|---|---|---|---|
| Male % (number) | 53.1 (138) | 47.6 (121) | 50.4 (259) |
| Age Mean (SD) | 56.5 (14.8) | 56.8 (15.1) | 56.7 (15.2) |
| Awake ambulatory BP | |||
| Systolic BP Mean (SD) | 139.4 (12.6) | 135.3 (12.4) | 137.4 (12.6) |
| Diastolic BP Mean (SD) | 82.9 (9.4) | 81.0 (10.2) | 82.0 (9.8) |
| Automated office BP | |||
| Systolic BP Mean (SD) | 142.6 (18.4) | 140.6 (14.9) | 141.7 (16.8) |
| Diastolic BP Mean (SD) | 85.6 (10.1) | 84.6 (11.0) | 85.1 (10.5) |
Results for the two sub‐groups exhibited similar relationships between AOBP and awake ABP (Table 1). There was a statistically significant correlation for systolic/diastolic BP between the AOBP and awake ABP in the 514 subjects (r = 0.70/r = 0.61; P < 0.001/P < 0.001). The strength of the association between the systolic AOBP and awake ABP in the Sunnybrook subjects (r = 0.79) was significantly stronger (P < 0.001) than for the Kingston subjects (r = 0.54), but the values were closer for diastolic BP (r = 0.69 and r = 0.61, respectively; P = 0.117).
The relationship between the mean AOBP and mean awake ABP values at possible thresholds for diagnosing hypertension alone and adjusted for age and gender was examined further (Tables 2 and 3). The linear regression models (intercepts and unstandardized B coefficients) were used as they provided the best fit to estimate values of awake ABP corresponding to AOBP readings of 130/80 and 135/85 mmHg alone and adjusted for age and gender. For all 514 patients, mean adjusted systolic AOBP readings of 130 and 135 mmHg corresponded to mean awake ambulatory systolic BP of 132.1 and 134.4 mmHg, respectively (Table 2). A mean adjusted diastolic AOBP of 80 and 85 mmHg corresponded to a mean awake ABP of 81.5 and 84.6 mmHg, respectively (Table 3). For all patients, both age and gender were significantly associated with diastolic but not systolic ABP. Diastolic awake ABP was 1.3 mmHg higher in male than in female patients and each 10‐year increase in age was associated with 0.6 mmHg decrease in diastolic ABP.
Table 2.
B coefficients (standard error) for awake systolic ambulatory (A)BP and automated office (AO)BP in linear regression models unadjusted and adjusted for age and sex
| Variable |
Kingston n = 260 |
Sunnybrook n = 254 |
Overall n = 514 |
|||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| AOBPa | 0.369 (0.036)** | 0.355 (0.039)** | 0.574 (0.038) * | 0.588 (0.038)** | 0.454 (0.026)** | 0.463 (0.028)** |
| Sex (Male)a | — | 0.229 (1.345) | — | 2.537 (1.121)* | — | 1.576 (0.898) |
| Age (y)a | — | 0.045 (0.049) | — | −0.050 (0.038) | — | −0.017 (0.031) |
| Intercept | 86.8 | 86.0 | 54.6 | 54.2 | 73.0 | 71.9 |
| r 2 | 0.292 | 0.294 | 0.480 | 0.495 | 0.366 | 0.371 |
| Awake ABP @ AOBP 130 mmHg | 134.8 | 132.2 | 129.2 | 130.7 | 132.0 | 132.1 |
| Awake ABP @ A0BP 135 mmHg | 136.6 | 134.0 | 132.1 | 133.6 | 134.3 | 134.4 |
a B coefficients with their standard errors.
*P < 0.05;
**P < 0.001.
Table 3.
B coefficients (standard error) for awake diastolic ambulatory (A)BP and automated office (AO)BP in linear regression models unadjusted and adjusted for age and sex
| Variable |
Kingston n = 260 |
Sunnybrook n = 254 |
Overall n = 514 |
|||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| AOBPa | 0.566 (0.046)** | 0.537 (0.049)** | 0.725 (0.036)** | 0.680 (0.038)** | 0.654 (0.029)** | 0.618(0.031)** |
| Sex (Male)a | — | 1.367 (0.960) | — | 1.301 (0.787) | — | 1.287 (0.624)* |
| Age (y)a | — | −0.035 (0.033) | — | −0.081 (0.027) * | — | −0.059 (0.022)* |
| Intercept | 34.4 | 38.1 | 19.7 | 27.5 | 26.9 | 32.0 |
| r 2 | 0.366 | 0.375 | 0.616 | 0.635 | 0.493 | 0.506 |
| Awake ABP @ AOBP 80 mmHg | 79.7 | 81.1 | 77.5 | 81.9 | 79.2 | 81.5 |
| Awake ABP @ A0BP 85 mmHg | 82.5 | 83.7 | 81.4 | 85.3 | 82.5 | 84.6 |
a B coefficients with their standard errors.
*P < 0.05;
**P < 0.001.
For the Sunnybrook sub‐group, mean adjusted systolic AOBP of 130 and 135 mmHg corresponded to a mean awake ambulatory systolic BP of 132.2 and 134.0 mmHg, and diastolic AOBP of 80 and 85 mmHg corresponded to 81.9 and 85.3, respectively. For the Kingston Heart Centre patients, a mean adjusted systolic AOBP of 130 and 135 mmHg corresponded to a mean awake systolic BP of 130.7 and 133.6 mmHg, and diastolic AOBP of 80 and 85 mmHg corresponded to 81.1 and 83.7, respectively.
AOBP was higher than awake ABP above a systolic BP of 135 mmHg and lower when awake ABP was <135 mmHg (Figure 1). There was an increasing white coat effect at higher systolic awake ABP readings, with the difference between the mean AOBP and awake ABP becoming progressively greater. Conversely, as systolic awake ABP readings fell below 135 mmHg, the mean AOBP reading became progressively lower than the awake ABP. Similar patterns were noted in the two sub‐groups and for diastolic BP at 80 and 85 mmHg (Figure 2).
Figure 1.
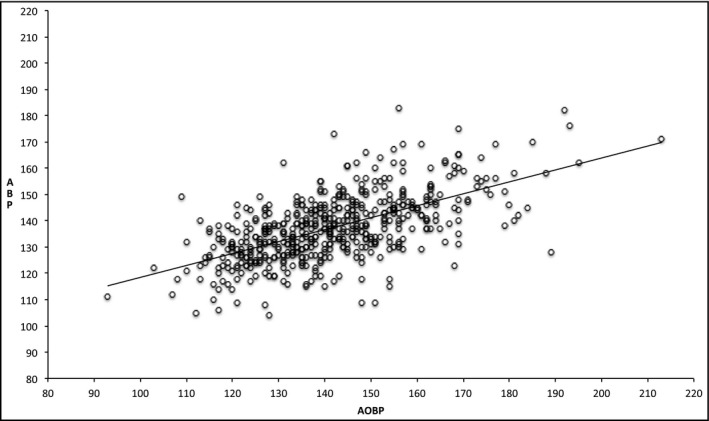
Scatter plot and regression line for the association between awake ambulatory (A)BP and automated office (AO)BP for systolic BP (n = 514)
Figure 2.
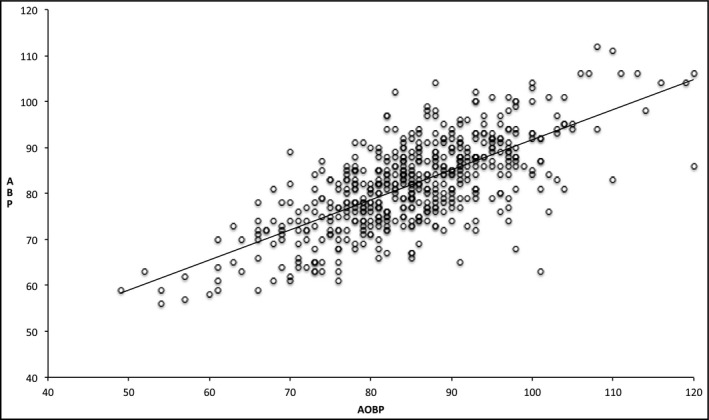
Scatter plot and regression line for the association between awake ambulatory (A)BP and diastolic automated office (AO)BP for diastolic BP (n = 514)
4. DISCUSSION
The threshold for defining hypertension has always been somewhat arbitrary, since the relationship between BP and risk of cardiovascular events is continuous and not binary. As noted in the ACC/AHA guidelines report,1 there is mounting evidence that AOBP is the preferred method for evaluating an individual’s BP in clinical practice. The AOBP threshold of greatest interest for defining hypertension based upon office BP would either be a reading of 130/80 mmHg (recent ACC/AHA guidelines1) or 135/85 mmHg (Canadian guidelines3). From the present data obtained in routine clinical practice, it appears that the closest point of equivalence to an AOBP of 135/85 mmHg is a mean awake ABP of 134.4/84.6 mmHg. If one considers the mean office BP threshold proposed for diagnosing hypertension in the ACC/AHA guidelines, a mean AOBP of 130/80 mmHg in our patient population was slightly lower than the corresponding awake ABP value of 132.1/81.5 mmHg. Thus, the AOBP recorded in our patients in routine clinical practice and their awake ABP were almost identical at the awake ABP threshold recommended by European2, 4 and Canadian3 guidelines for diagnosing hypertension (135/85 mmHg). However, the findings in the present study suggest that the awake ABP may be 2.1/1.5 mmHg higher than an AOBP of 130/80 mmHg, if the latter was being used to screen patients for possible hypertension.
Patients referred to two different ABPM centers were included in this study to maximize the generalizability of the results to routine clinical practice. AOBP may be recorded in different settings in the community using different devices which take between 3 and 5 BP readings. ABPM is also not always recorded using the same protocol with differences in the frequency of readings and in the designation of awake versus asleep periods. Such variations in technique may produce small differences in mean BP readings. By studying subjects in two centers, we have likely obtained a more representative sample of untreated patients undergoing assessment for possible hypertension using both AOBP and ABPM in a community setting.
The American guidelines selected an office BP of 130/80 mmHg based upon the benefits of treatment below this value, especially in patients with a higher cardiovascular risk. It appears that the decision to match 130/80 mmHg for office BP to an identical reading for awake ABP and home BP was somewhat arbitrary, as no evidence was presented to support the equivalence of these values. Although these guidelines also recognized the potential advantages of AOBP over conventional office BP measurement, the recommendations for performing office BP were still based upon traditional methods of BP measurement. From a practical standpoint, it would seem appropriate to use AOBP, regardless of the threshold for defining hypertension, since there are no similar equivalence data in untreated patients in routine clinical practice comparing office BP and awake ABP with either manual or attended oscillometric BP measurements.
The ACC/AHA guidelines recommended that 2‐3 office BP readings be taken using an oscillometric sphygmomanometer. Although data comparing manual office BP and awake ABP at 130/80 mmHg in routine clinical practice are limited, there are data on duplicate oscillometric BP and awake ABP obtained in routine clinical practice from the Spanish ABPM Registry in over 39 000 treated hypertensive patients attending the offices of their primary care physicians.8
In 27 211 patients in the registry with a systolic office BP ≥ 140 mmHg, the mean office BP was 159.5/88.8 mmHg compared to a mean awake ABP of 135.0/78.0 mmHg. Closer to the new threshold for diagnosing hypertension of 130/80 mmHg, in 5028 patients treated for hypertension with a systolic office BP of 120‐139 mmHg, the mean office reading was 131.5/81.0 compared to a mean awake ABP of 125.9/75.6 mmHg. Thus, duplicate oscillometric office BP readings recorded using validated electronic sphygmomanometers close to the threshold of 130/80 mmHg in routine clinical practice were 5.6/5.4 mmHg higher than the awake ABP. As for a threshold of 135/85 mmHg, a mean oscillometric office BP of 135/83 mmHg, recorded in duplicate in patients in the registry with a systolic BP of 130‐139 mmHg, was equivalent to a mean awake ABP of 127/76 mmHg (Alejandro de la Sierra, personal communication). Thus, attended oscillometric office BP readings of about 130/80 or 135/85 mmHg in treated hypertensive patients were still associated with a white coat effect, which was not seen in the comparison between AOBP and awake ABP in untreated patients in the present study. Differences in the relationship between office BP and awake ABP in treated and untreated patients at a systolic BP < 130 mmHg have been noted previously.9
On the basis of these data, it would seem more appropriate to substitute AOBP for the attended oscillometric BP readings recommended in the American and European guidelines for BP measurement in clinical practice, if the office BP and awake ABP are to be considered equivalent at either 130/80 or 135/85 mmHg, since the mean AOBP values in our study in routine clinical practice were similar to the mean awake ABP at these thresholds.
Although these data do not resolve the question of which threshold should be used to define hypertension in clinical practice, they at least provide us with a measure of office BP which approximates the awake ABP and home BP in patients untreated for hypertension. AOBP also has the advantage of being consistent from visit to visit and when recorded in different locations, including an examining room, a waiting room, a community pharmacy or an ABPM unit.7, 10, 11
Now that guidelines for office BP measurement are expressing a preference for oscillometric BP over manual BP readings, some critics of AOBP have questioned the necessity of having the patient resting quietly and alone during the recording of multiple oscillometric BP readings.12 It is conceivable that recording AOBP in the presence of a nurse or physician (called “attended AOBP” by the authors) in a research setting with strict adherence to BP measurement guidelines, especially no conversation, might produce office BP readings which are close to an unattended AOBP. However, there is no evidence that such conditions will be successfully duplicated in routine clinical practice.13 As noted in the data from the Spanish ABPM Registry,8 a clinically important white coat effect with attended oscillometric office BP readings was still present in primary care settings at the threshold of 130/80 mmHg. The difference was even greater in hypertensive patients who had an office BP 25.5/10.8 mmHg higher than the mean awake ABP. Moreover, the promotion of standard BP measurement guidelines by organizations such as the American Heart Association during past decades has not solved the problem of a white coat effect, whereas AOBP substantially reduces the number of patients with office BP readings higher than the awake ABP.5 Finally, apart from having sufficient office space, there is no apparent advantage in having staff present when BP is being recorded with an automated, oscillometric device.
The present analysis also raises interesting questions concerning target BP below 130/80 mmHg. It is apparent that office BP becomes lower than the awake ABP in this range,9 a similar finding also reported in SPRINT,14 which used both attended and unattended office BP measurement.15 Data from the Spanish ABPM Registry, from manual BP in untreated subjects and in treated patients in family practice all report an office BP lower than the awake ABP when office systolic BP is <130 mmHg or lower.9 Other meta‐analyses suggest that ABPM is a good predictor of cardiovascular outcomes when systolic BP is <130 mmHg,16 so that ABPM may still be the gold standard for BP measurement at target BP. Further research is required to establish the best technique for determining if target BP has been achieved after the initiation of antihypertensive drug therapy, likely a combination of an automated office and out‐of‐office BP.
In conclusion, when it comes to screening for hypertension in the office, AOBP should be the preferred method for BP measurement, regardless of whether the threshold for defining hypertension is 135/85 or 130/80 mmHg. The present data show a slightly closer relationship between AOBP and awake ABP at an AOBP of 135/85 mmHg. Clinic staff should not be present when BP is being recorded with an oscillometric device, if increases in office BP due to a white coat effect are to be avoided. Finally, the techniques for measuring office BP at target for drug therapy will need to be re‐evaluated now that it is clear that office BP is lower than the corresponding ambulatory BP in the normotensive BP range. A forthcoming Statement on Blood Pressure Measurement from the American Heart Association will discuss in greater detail the potential role for AOBP in routine clinical practice.
CONFLICT OF INTEREST
No conflict of interest to disclose.
Myers MG, Matangi M, Kaczorowski J. Comparison of awake ambulatory blood pressure and automated office blood pressure using linear regression analysis in untreated patients in routine clinical practice. J Clin Hypertens. 2018;20:1696–1702. 10.1111/jch.13409
REFERENCES
- 1. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269‐1324. [DOI] [PubMed] [Google Scholar]
- 2. Mancia G, Fagard R, Krzysztof N, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension. J Hypertens. 2013;31:1281‐1357. [DOI] [PubMed] [Google Scholar]
- 3. Leung AA, Nerenberg KA, Daskalopoulou SS, et al. Hypertension Canada’s 2016 CHEP Guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention and treatment of hypertension. Can J Cardiol. 2016;32:569‐588. [DOI] [PubMed] [Google Scholar]
- 4. O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731‐1768. [DOI] [PubMed] [Google Scholar]
- 5. Myers MG. A short history of automated office blood pressure – 15 years to SPRINT. J Clin Hypertens. 2016;18(8):721‐724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Myers MG. A proposed algorithm for diagnosing hypertension using automated office blood pressure measurement. J Hypertens. 2010;28:703‐708. [DOI] [PubMed] [Google Scholar]
- 7. Armstrong D, Matangi M, Brouillard D, Myers MG. Automated office blood pressure – being alone and not location is what matters most. Blood Press Monit. 2015;20:204‐208. [DOI] [PubMed] [Google Scholar]
- 8. de la Sierra A, Banegas JR, Divison JA, et al. Ambulatory blood pressure in hypertensive patients with inclusion criteria for the SPRINT trial. J Am Soc Hypertens. 2016;10:947‐953. [DOI] [PubMed] [Google Scholar]
- 9. Myers MG, Kaczorowski J. Office blood pressure is lower than awake ambulatory blood pressure at lower targets for treatment. J Clin Hypertens. 2017;19:1210‐1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Myers MG, Valdivieso M, Kiss A. Consistent relationship between automated office blood pressure recorded in different settings. Blood Press Monit. 2009;14:108‐111. [DOI] [PubMed] [Google Scholar]
- 11. Chambers LW, Kaczorowski J, O’Reilly S, Ignagni S, Hearps S. Comparison of blood pressure measurements using an automated blood pressure device in community pharmacies and family physicians’ offices: a randomized controlled trial. CMAJ Open. 2013;1:E37‐E42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stergiou G, Kollias A, Parati G, O’Brien E. Office blood pressure measurement. The weak cornerstone of hypertension diagnosis. Hypertension. 2018;71:813‐815. [DOI] [PubMed] [Google Scholar]
- 13. Myers MG. The fallacy of attended automated blood pressure. Am J Hypertens. 2018;31:755‐757. [DOI] [PubMed] [Google Scholar]
- 14. Drawz PE, Pajewski NM, Bates JT, et al. Effect of intensive versus standard clinic‐based hypertension management on ambulatory blood pressure. Hypertension. 2017;69:51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson KC, Whelton PK, Cushman WC, et al. Blood pressure measurement in SPRINT (Systolic blood pressure intervention trial). Hypertension. 2018;71:840‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Myers MG. Statistical analysis as a cause of white coat hypertension. J Hypertens. 2017;35:707‐709. [DOI] [PubMed] [Google Scholar]


