Abstract
The posthospital discharge period is vulnerable for patients with coronavirus disease 2019 (COVID-19). The authors implemented a COVID-19 discharge pathway in the electronic medical record for UCHealth, a 12-hospital health care system, including an academic medical center (University of Colorado Hospital [UCH]), to improve patient safety by standardizing discharge processes for COVID-19 patients. There were 3 key elements: (1) building consensus on discharge readiness criteria, (2) summarizing discharge criteria for disposition locations, and (3) establishing primary care follow-up protocols. The discharge pathway was opened 821 times between April 20, 2020, and June 7, 2020. Of the 436 patients discharged from the hospital medicine service at UCH from April 20, 2020, and June 7, 2020, 18 (4%) were readmitted and 13 (3%) had a 30-day emergency department visit. The main trend observed was venous thromboembolism. This pathway allowed real-time integration of clinical guidelines and complex disposition requirements, decreasing cognitive burden and standardizing care for a complex population.
Keywords: patient safety, transitions of care, pathway
Introduction
Ineffective planning and coordination of care at time of discharge can contribute to adverse patient events.1–3 In the setting of the coronavirus disease 2019 (COVID-19) pandemic, the immediate postdischarge period is especially vulnerable given the unpredictable disease course, which can be complicated by late respiratory failure and venous thromboembolism (VTE).4,5 Additionally, the impact of the pandemic on marginalized communities has highlighted health disparities and added nuances to the COVID-19 discharge different from a typical inpatient discharge.6
Care pathways can deliver clinical guidelines to standardize care through the use of decision support and educational content, thereby decreasing cognitive load on clinicians, improving workflow efficiency, and reducing adverse events.7 With the surge of hospitalized patients with COVID-19 and rapidly changing recommendations for evaluation and management, a nimble pathway development and implementation process can quickly disseminate updates to clinicians and serve as a single source of guidance. Further, integration into the electronic health record (EHR) can embed pathways into usual clinical workflows so as to drive utilization.
At the study health system, multiple yet disjointed efforts were underway to provide care for patients with COVID-19. Some efforts focused on identifying appropriate discharge criteria, some on providing guidance on isolation upon discharge, and yet others on follow-up protocols. This article describes an initiative that developed and deployed an EHR-based COVID-19 discharge pathway to standardize transitions of care processes for COVID-19 patients in order to improve patient safety.
Methods
Setting
The initiative was implemented at a network of 12 hospitals called the UCHealth system, including University of Colorado Hospital (UCH), a 690-bed tertiary care academic hospital in Aurora, Colorado. The pathway was integrated into the graphic user interface of the EHR using a software platform (AgileMD, San Francisco, CA) that allows for flowchart visualizations and the placement of orders directly from the pathway workflow. This conforms to the principles of clinical decision support development described previously by Osheroff et al.8
Program Description
A multidisciplinary group was established that comprised physicians, care management, and hospital system leadership to build a standard discharge process for COVID-19 patients. The initiative had 3 key elements: (1) building consensus on discharge readiness criteria, (2) collecting and summarizing discharge criteria for various disposition locations, and (3) establishing standard primary care provider (PCP) follow-up protocols for close monitoring upon discharge. The end result was the discharge pathway (Figure 1) that was implemented across UCHealth, an integrated health system of community and academic health systems. This discharge pathway was used by both academic and community inpatient providers.
Figure 1.
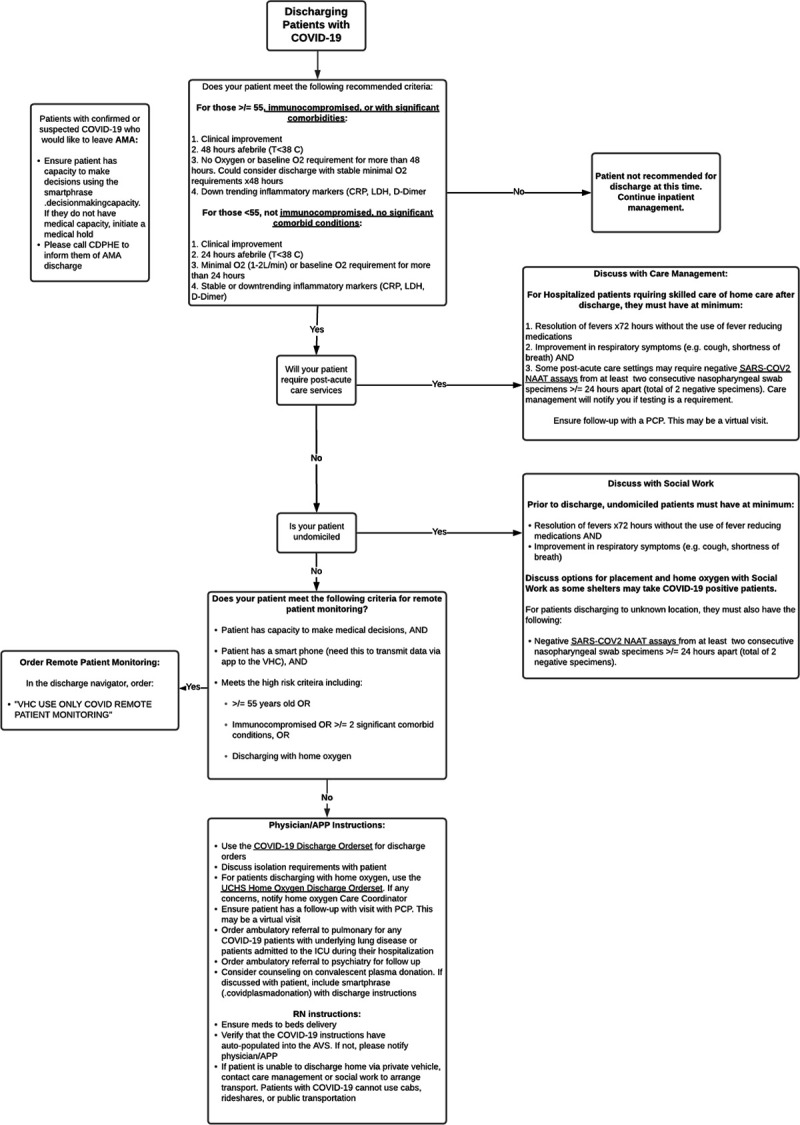
COVID-19 discharge pathway. Underlined text are links to definitions, orders, or other pathways. Abbreviations: AMA, against medical advice; APP, advanced practice provider; AVS, after visit summary; CDPHE, Colorado Department of Public Health and Environment; COVID-19, coronavirus disease 2019; CRP, C-reactive protein; ICU, intensive care unit; LDH, lactate dehydrogenase; NAAT, nucleic acid amplification test; PCP, primary care provider; RN, registered nurse; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; UCHS, UCHealth System; VHC, virtual health center.
The discharge readiness criteria were determined by physician teams using current consensus criteria across academic institutions and known literature. These criteria were further refined by a multidisciplinary physician team including hospital medicine, primary care internal medicine, family medicine, infectious disease, and pulmonary and critical care medicine. Patients were initially divided into 2 categories based on known literature and expert consensus: high risk and low risk for decompensation. High risk was defined as age ≥55 years, immunocompromised because of illness or medications or HIV with CD4 ≤200, pregnant, or those having ≥2 of the following comorbidities: diabetes mellitus, hypertension, coronary artery disease, underlying lung disease, chronic kidney disease, or morbid obesity. Discharge criteria for the high-risk population included (1) clinical improvement, (2) afebrile for 48 hours, (3) stable oxygen requirement for 48 hours, and (4) a downtrend of inflammatory markers including C-reactive protein, lactate dehydrogenase, and d-dimer. Lower risk patients were defined as age <55 years with no significant comorbid conditions and not immunocompromised. Discharge criteria for the lower risk population included (1) clinical improvement, (2) afebrile for 24 hours, (3) stable oxygen requirement for 24 hours, and (4) stable or a downtrend in inflammatory markers including C-reactive protein, lactate dehydrogenase, and d-dimer.
Once the overall discharge readiness criteria were established, the research team partnered with care management to streamline the discharge workflows for various disposition locations including post-acute care facilities, home health care requirements, and undomiciled patients as well as patients discharging home. These recommendations were based on the Centers for Disease Control and Prevention and the Colorado Department of Public Health and Environment guidelines and resulted in the pathway shown in Figure 1. Concurrently, the team partnered with ambulatory physician and administrative leadership to streamline ambulatory processes for follow-up and outpatient monitoring of patients with COVID-19 who are followed by the UCHealth system. This included a nurse care manager follow-up phone call within 2 days of discharge and then follow-up phone calls as needed based on patient improvement. Many patients were either uninsured or did not have PCPs. Given the current pandemic, it was especially difficult to establish new PCP follow-up appointments. Therefore, a new process was built in which patients without an established PCP were monitored by a group of fourth-year medical students and UCHealth nurses with the same protocol as established patients, which included escalation protocols to a physician evaluation via virtual urgent care for worsening symptoms (Figure 2). Lastly, a remote patient monitoring program was built from the virtual health center for high-risk patients discharging from the hospital to their homes. This included discharging high-risk patients with a wearable device for monitoring over an 8-day period post discharge, with vital sign monitoring every 4 hours for signs of early decompensation in conjunction with daily phone calls.
Figure 2.
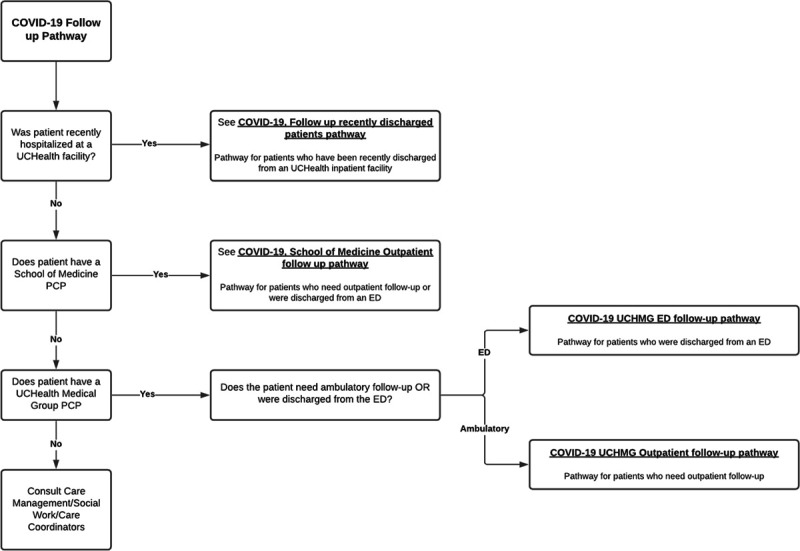
COVID-19 follow-up pathway. Underlined text are links to other pathways. Abbreviations: COVID-19, coronavirus disease 2019; ED, emergency department; PCP, primary care provider; UCHMG, UCHealth medical group.
Results
Data obtained from the EHR and the pathway third-party vendor were used to evaluate overall pathway utilization and 30-day readmission rates with an index admission related to COVID-19. The inpatient discharge pathway was opened 821 times from April 20, 2020, to June 7, 2020, after the pathway was published in the EHR. A total of 422 patients were discharged from the hospital medicine service at UCH from April 20, 2020, to June 7, 2020. Demographic characteristics of the patients are described in the Table. Of these patients, 18 patients were readmitted (4%) and 13 patients (3%) had a 30-day emergency department (ED) visit.
Table.
Characteristics of COVID-19 Patients Discharged From the Hospital Medicine Service.
| Characteristics | N = 422 |
|---|---|
| Age, mean | 55 |
| Sex (%) | |
| Male | 55 |
| Female | 45 |
| Race (%) | |
| Non-Hispanic | 51 |
| Hispanic | 48 |
| Unknown | 1 |
| Race (%) | |
| Other | 44 |
| White or Caucasian | 30 |
| Black or African American | 18 |
| Asian | 5 |
| American Indian and Alaska Native | 1 |
| Native Hawaiian and other Pacific Islander | 1 |
| More than 1 race | 0.5 |
| Unknown | 0.5 |
| Language (%) | |
| English | 59 |
| Spanish | 30 |
| Nepali | 2 |
| Burmese | 1 |
| Other | 8 |
Abbreviations: COVID-19, coronavirus disease 2019.
All 30-day readmissions and all 30-day ED visits with an index admission related to COVID-19 at UCH were reviewed to allow assessment of and real-time changes to the discharge criteria. The main trend observed centered on VTE management. There were 4 patients diagnosed with new or propagating VTE, 2 patients with an ED visit within 30 days, and 2 patients requiring admission. Given this new finding, the research team partnered with hematology specialists to build VTE prevention guidelines and then edited the pathway to include these VTE prevention recommendations tiered for risk based on hospital stay in real time. The main trend from remote patient monitoring data showed new or worsening hypoxia requiring an evaluation from the virtual health center attending physician with subsequent creation of outpatient home oxygen delivery programs.
Discussion
Effective transitions of care processes are essential for providing high-quality patient care. This fundamental aspect of care becomes even more critical given the unpredictable disease course for patients with COVID-19. The initiative described offers an effective and efficient process for coordinating and standardizing care for patients with COVID-19.
Through multidisciplinary collaboration, within weeks of the beginning of the pandemic, an EHR-embedded COVID-19 discharge pathway was deployed across a multihospital system. This pathway allowed integration of clinical guidelines and complex disposition requirements with real-time updates to decrease cognitive burden and implement a strong follow-up protocol for a patient population with an unpredictable course. The hospital system’s previously established PCP clinic processes were capitalized on to optimize and standardize follow-up protocols for patients with COVID-19. Additionally, new processes were built to support uninsured patients who otherwise would have been unable to have timely follow-up. Importantly, the standardized pathway discharge criteria can be adjusted quickly in the circumstance of rapidly rising patient census to prevent further strain on hospital resources. Notably, as seen with the trend for VTE, the pathway allowed rapid integration of newly emerging evidence and growing experience into one location to centralize and standardize care for COVID-19 patients across a health care system. This allowed UCHealth to standardize patient care and attempt to improve patient safety in real time.
Study readmission rates differed from those in the literature: 4% for this initiative in comparison to 9% described in the literature.9 There are likely many variables accounting for this difference. First, although the pathway was implemented across a health system, readmission rates were reviewed only for patients discharged by the hospital medicine service at one hospital. This was because the hospital medicine service at the tertiary academic medical center, UCH, accounted for the bulk of discharges; the data were easily available and the pathway was geared toward hospital medicine services. Second, the 9% readmission rates described by Lavery et al9 accounted for 60-day readmission rates, while the current study only evaluated 30-day readmission rates. Lastly, these data are from early in the pandemic when physicians were unsure of the postdischarge clinical course. It is possible that patients had a longer length of stay to account for this, in turn impacting the 30-day readmission rates.
The rapidity with which this system-wide innovation was able to be instituted was made possible by several factors: high urgency, institutional buy-in, stakeholder engagement, and open feedback channels for improvement. Subsequent changes were made quickly to both the pathway content and its information technology components, allowing the pathway to serve as a trustworthy and timely source of information. Because the solution was fluidly integrated into the EHR, providers could access updated contents easily within their normal workflow. EHR-embedded care pathways can be used for other disease processes to standardize care across health systems, especially because orders are readily incorporated into the pathway for ease of use. Examples of other care pathways at the study institution include Clostridium difficile colitis, pneumonia, and diabetic foot infections.
The main challenge experienced centered on consolidating efforts. Multiple groups were working on similar yet disjointed efforts and quickly organizing these stakeholders under one venture became imperative to offer one standard solution. This was done by cascading inquiries from all leadership groups at the chief medical officer or chief operating officer level to frontline leadership teams, in both ambulatory and inpatient settings. Once all efforts were identified, the work was realigned under specific leaders. For example, one chief medical officer coordinated all efforts concerning transitions of care. Furthermore, all new efforts were coordinated through the institutional command center to centralize all COVID-19–related endeavors. It was also particularly challenging to navigate the rapidly changing face of this novel global pandemic, requiring rapid-cycle improvement based on provider experience, evolving evidence, policy changes, and continued stakeholder input to improve the pathway.
Given the unique characteristics of the study population, who live at an altitude >5000 feet, the discharge criteria may not be applicable to other lower altitude populations. Moreover, the readmission data used to modify the pathway were from a single academic institution and did not capture other safety issues that may have occurred at other UCHealth system hospitals. Additionally, aspects of the pathway were left to provider interpretation, such as what clinical improvement meant and which inflammatory markers to trend, which also may have skewed discharge data. Lastly, the pathway was not used by all providers who discharged COVID-19 patients; therefore, the postdischarge data, including readmissions, may not be truly reflective of the pathway’s efficacy.
Conclusions
This initiative demonstrates the successful adoption of a rapidly deployed, fully integrated electronic care pathway throughout a large health care system during the crisis situation of the COVID-19 pandemic, to aid in transitions of care. Institutions should consider using a similar approach for adoption of other high-impact, high-yield clinical pathways.
Conflicts of Interest
Dr Bookman can potentially receive royalties with AgileMD for emergency medicine content in its pathways product. All the other authors have no conflicts of interest to disclose.
Author Contributions
Dr Patel conceived and designed the pathways, was lead hospitalist representative for follow-up pathways, collected/analyzed/interpreted the data, was primary author with responsibility to write the preliminary article as well primarily responsible for the subsequent second version after the editor/reviewer comments. Dr Virapongse helped conceive, build, and distribute the discharge pathway, helped collect data for the pathway, critically reviewed the primary article, and helped revise the article after the editor/reviewer comments. Dr Baduashvili did the research for the discharge pathway, helped build the pathway, critically reviewed the primary article, and helped revise the article after the editor/reviewer comments. Dr Devitt did the research for the discharge pathway, helped build the pathway, critically reviewed the primary article, and helped revise the article after the editor/reviewer comments. Ms Barr was responsible for dissemination of the discharge pathway across the system, was primary manager and builder for the follow-up pathways that required coordination with multiple specialties, critically reviewed the primary article, and helped revise the article after the editor/reviewer comments. Dr Bookman conceived and designed the follow-up pathways, was responsible for dissemination of the discharge pathway across the system, led the meetings to build all the follow-up pathways that required coordination with multiple specialties, critically reviewed the primary article, and helped revise the article after the editor/reviewer comments.
Disclaimer
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003; 18:646–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: the care transitions measure. Med Care. 2005; 43:246–255 [DOI] [PubMed] [Google Scholar]
- 3.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004; 52:1817–1825 [DOI] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet Lond Engl. 2020; 395:1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191:145–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okonkwo NE, Aguwa UT, Jang M, et al. COVID-19 and the US response: accelerating health inequities. BMJ Evid-Based Med. Published online June 3, 2020. doi: 10.1136/bmjebm-2020-111426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson KM, Fouquet SD, Kerns E, et al. Impact of mobile device-based clinical decision support tool on guideline adherence and mental workload. Acad Pediatr. 2019; 19:828–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osheroff JA, Teich JM, Middleton B, et al. A roadmap for national action on clinical decision support. J Am Med Inform Assoc. 2007; 14:141–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lavery AM, Preston LE, Ko JY, et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1695–1699 [DOI] [PMC free article] [PubMed] [Google Scholar]


