Abstract
We aimed to compare the ability of the pediatric blood pressure (BP) standards issued by the US Fourth Report, the recently proposed US, Chinese, and international standards to predict adult hypertension and subclinical cardiovascular disease (CVD). 2296 children were randomly selected from Beijing at baseline. The follow‐up survey was conducted among 1177 adults. Subclinical adult CVD was assessed using the carotid‐femoral pulse wave velocity (cfPWV), carotid intima‐media thickness (CIMT), and left ventricular mass index (LVMI). The prevalence of pediatric elevated BP was significantly higher according to the Chinese standards vs the Fourth Report, the updated US standards, and the international standards (18.7% vs 14.2%, 17.5%, and 18.0%, respectively; all Ps < .001). Children identified as elevated BP using any of the 4 standards were more likely to have adult hypertension, high cfPWV, and high LVMI than children without elevated BP. However, only the Chinese and updated US standards can predict the increased risk of adult high CIMT. Our results indicated that the Chinese standards performed equally or better compared with 3 other standards in predicting adult hypertension and subclinical CVD.
Keywords: blood pressure, cardiovascular disease, child
1. INTRODUCTION
Childhood elevated blood pressure (BP) is a public health problem worldwide.1 Subclinical cardiovascular disease (CVD) may already be present in children with elevated BP.2, 3 Children with elevated BP were likely to have hypertension as adults,4 and childhood elevated BP was associated with increased risk of early onset subclinical CVD in adulthood.5, 6 Therefore, accurate early identification of children with elevated BP is the central aspect in the primordial prevention of CVD.
In adults, the definition of hypertension is based mainly on the association of BP levels with adverse cardiovascular outcomes.7 However, there is no evidence relating childhood BP levels to cardiovascular outcomes.8 Given that the upper limits of BP ranges in children were not ideal, the BP percentiles, rather than absolute levels, were used to define childhood elevated BP.9, 10, 11 As a result, the definition of childhood elevated BP was based on the BP distribution and, to some extent arbitrary.
The BP standards for children presented in the US Fourth Report are widely accepted and used in the US, Europe, and elsewhere.11, 12, 13 Recently, the American Academy of Pediatrics updated the Fourth Report BP standards based on new evidence.14 However, the childhood BP standards established in one population may not be applicable to other populations as the distribution of BP values vary across different ethnic groups and geographic areas.15, 16 Several country‐specific childhood BP standards have been established.16, 17, 18, 19 Using nationally representative data, standard BP percentiles by sex, age, and height for Chinese children aged 3‐17 years have also been established.19 For international comparisons of childhood elevated BP prevalence, Xi and colleagues20 combined BP data from 7 countries to establish international childhood BP standards. For reducing the long‐term risk of CVD, it remains unknown whether the Chinese standards are more appropriate to identify Chinese children with elevated BP than other standards.
In this study, we aimed to compare the performance of the Chinese, Fourth Report, updated US and international standards in predicting adult hypertension and subclinical CVD using data from the Beijing BP Cohort Study.
2. METHODS
2.1. Study population
The Beijing BP Cohort Study was a population‐based longitudinal study of CVD risk factors from childhood to adulthood. The details of the study design have been described previously.21, 22 In the baseline survey conducted in 1987, 2442 healthy children aged 6‐18 years were randomly selected from 6 elementary schools and 6 high schools located in urban Beijing using random cluster sampling. After excluding the subjects aged 18 years in the baseline survey (n = 94) and the subjects with incomplete childhood data (n = 52), 2296 subjects were used to compare the prevalence of childhood elevated BP according to 4 different definitions. 1119 subjects were not included mainly because they refused to participate (n = 836), their contact information was unavailable (n = 214), they moved out of the local region (n = 54), or they died (n = 15). The final follow‐up survey was conducted in 2011 among 1177 adults aged 27‐42 years who had participated in the baseline survey as children. Carotid‐femoral pulse wave velocity (cfPWV), carotid intima‐media thickness (CIMT), and left ventricular mass were measured to assess adult subclinical CVD during the final follow‐up. These 1177 subjects were used to compare the ability of 4 different childhood BP standards to predict adult subclinical cardiovascular outcomes.
Written informed consent was obtained from all subjects for each survey, and from the parents/guardians for the baseline survey. The study was approved by the Institutional Review Board and Ethics Committee of the Capital Institute of Pediatrics (Beijing, China).
2.2. General examinations
At both baseline and follow‐up, participants rested for at least 15 minutes before trained observers measured their seated BP in the right arm using a mercury sphygmomanometer. BP was measured 3 times (at least) 1 minute apart and the average values of the last 2 readings were used for further analysis. Systolic BP (SBP) and diastolic BP (DBP) were defined by the first and fifth Korotkoff phases, respectively. According to the Fourth Report, international and Chinese standards,11, 19, 20 childhood elevated BP and hypertension were defined as SBP/DBP ≥ 90th percentile for sex, age, and height (or SBP/DBP ≥ 120/80 mm Hg), and SBP/DBP ≥ 95th percentile for sex, age, and height, respectively. The updated US standards recommended similar definitions for children <13 years of age, but used SBP/DBP ≥ 120/80 and ≥130/80 mm Hg to define childhood elevated BP and hypertension, respectively, for children aged 13 years and older.14 Adult hypertension was defined as SBP/DBP ≥ 140/90 mm Hg and/or self‐reported use of antihypertensive agents. The replicated measurements of weight and height with underwear and no shoes were made using a standard protocol,22 and the mean values were used for calculating body mass index (BMI, weight in kilograms divided by the square of the height in meters).
Demographic data and lifestyle factors (smoking, alcohol consumption, and physical inactivity) were collected from completed questionnaires at follow‐up. Smoking and drinking were defined as smoking or drinking regularly within the last 12 months before the follow‐up survey. Physical inactivity was defined as <1.5 hour/wk regarding moderate to vigorous physical activity.
2.3. Subclinical cardiovascular structure and function
The details of the cfPWV, CIMT, and left ventricular mass measurements have been described elsewhere.21, 22 In brief, the cfPWV was measured by trained observers using a vascular profiler, and calculated as the distance between the 2 arterial recording sites (meters) divided by the pulse wave transit time (seconds). The CIMT was measured on the longitudinal view of the anterior and posterior wall at 1‐1.5 cm proximal to the bifurcation of each common carotid artery using an ultrasound scanner with a 12‐MHz linear transducer. The average of 4 measurements at each of the 2 sites was used for analysis. The left ventricular mass was measured according to the recommendations of the American Society of Echocardiography.23 Left ventricular mass index (LVMI) was assessed according to the De Simone's method (LVMI = left ventricular mass/height2.7).24
2.4. Statistical analysis
The measured values of subclinical cardiovascular structure and function in adulthood were standardized with Z‐transformation (mean = 0, SD = 1) using regression residual analyses stratified by sex, with adjusting for adulthood age. High cfPWV, high LVMI, and high CIMT were defined as Z scores at or above 75th percentile (upper quartile), which were consistent with the previous study.22 Any subclinical CVD was defined as any measures of high cfPWV, high CIMT, or high LVMI.
The differences in the prevalence of pediatric elevated BP among 4 different definitions were tested using χ2 test. Logistic regression models were used to examine the association of childhood elevated BP, as defined by the 4 childhood BP standards (the Chinese, Fourth Report, updated US and international standards) with adult hypertension and subclinical CVD after adjusting for sex, childhood age, and other covariates. The ability of the childhood BP standards to predict hypertension and subclinical CVD in adulthood was also assessed by calculating the area under the receiver operating characteristic curve (AUC).5, 6, 25
Statistical analysis was conducted using SAS version 9.2. Statistical significance was inferred by a 2‐tailed test where P < .05.
3. RESULTS
A total of 2296 participants (mean age, 10.6 years; 54.1% males; mean BMI, 17.0 kg/m2) were eligible for the current analysis at baseline. The prevalence of childhood elevated BP and hypertension among 4 standards is shown in Figure. The prevalence of pediatric elevated BP was significantly higher according to the Chinese standards vs the Fourth Report, the updated US standards, and the international standards (18.7% vs 14.2%, 17.5%, and 18.0%, respectively; for all, P < .001). Of 429 children with elevated BP diagnosed by the Chinese standards, 76.2%, 90.2%, and 93.9% were confirmed by the Fourth Report, updated US and international standards, respectively. The prevalence of childhood hypertension was significantly higher according to the Chinese standards vs the Fourth Report, the updated US standards, and the international standards (9.0% vs 4.9%, 8.1%, and 8.3%, respectively; for all, P < .001).
Figure 1.
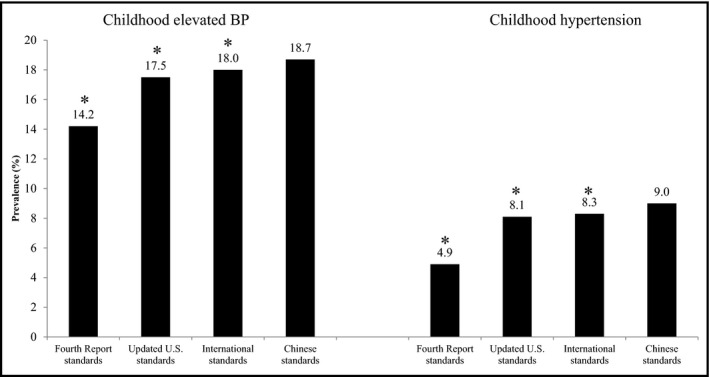
Prevalence of childhood elevated BP and hypertension among 4 different standards at baseline. *P < .001 (Compared with the Chinese standards). BP, blood pressure
The demographic and clinical characteristics of the participants who were successfully followed up are shown in Table 1. The prevalence of hypertension and any subclinical CVD in adulthood were 12.8% and 50.8%, respectively.
Table 1.
Characteristics of the participants who were successfully followed up
| Childhood | Adulthood | |
|---|---|---|
| Males, No. (%) | 642 (54.5) | 642 (54.5) |
| Age, y | 10.7 ± 3.5 | 34.2 ± 3.5 |
| Height, cm | 143.1 ± 18.5 | 167.8 ± 8.5 |
| BMI, kg/m2 | 17.0 ± 3.1 | 24.7 ± 4.3 |
| SBP, mm Hg | 104.5 ± 11.8 | 113.9 ± 15.6 |
| DBP, mm Hg | 53.6 ± 11.0 | 72.3 ± 12.1 |
| Hypertension, No. (%) | 151 (12.8) | |
| Smoking, No. (%) | 556 (47.2) | |
| Drinking, No. (%) | 477 (40.5) | |
| Physical inactivity, No. (%) | 617 (52.4) | |
| cfPWV, cm/s | 692.9 ± 97.5 | |
| CIMT, mm | 0.52 ± 0.05 | |
| LVMI, g/m2.7 | 32.7 ± 8.2 | |
| Any of high cfPWV, high CIMT, or high LVMI, No. (%) | 598 (50.8) |
BMI, body mass index; cfPWV, carotid‐femoral pulse wave velocity; CIMT, carotid intima‐media thickness; DBP, diastolic blood pressure; LVMI, left ventricular mass index; SBP, systolic blood pressure.
Values are mean ± standard deviation for continuous variables or No. (%) for categorical variables.
Table 2 shows the association of childhood elevated BP with hypertension and subclinical CVD in adulthood. After adjusting for sex and childhood age, the children identified as elevated BP using any of 4 standards were more likely to have adult hypertension, high cfPWV, high CIMT, and high LVMI than children without elevated BP. For any of the outcome variables, the strengths of these associations were similar among 4 standards. After additional adjustment for childhood BMI and adult risk factors, the associations did not change substantially, except that the Fourth Report or international standards showed a nonsignificant association with high CIMT in adulthood (odds ratio and 95% confidence interval: 1.37, 0.93‐2.02; 1.41, 0.99‐2.01, respectively). The Chinese or updated US standards still had a significant association with adult high CIMT (odds ratio and 95% confidence interval: 1.49, 1.05‐2.10; 1.46, 1.02‐2.08, respectively).
Table 2.
ORs (95% CIs) of adult hypertension and subclinical CVD according to 4 definitions of childhood elevated BP
| Chinese standards | Fourth Report standards | International standards | Updated US standards | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Hypertension | 2.87 (1.93‐4.27)*** | 2.33 (1.53‐3.57)*** | 2.79 (1.81‐4.30)*** | 2.19 (1.39‐3.46)** | 2.62 (1.75‐3.91)*** | 1.99 (1.30‐3.06)** | 2.73 (1.82‐4.07)*** | 2.05 (1.34‐3.15)** |
| High cfPWV | 1.96 (1.38‐2.77)*** | 1.78 (1.24‐2.55)** | 1.80 (1.22‐2.66)** | 1.62 (1.08‐2.41)* | 1.90 (1.34‐2.71)*** | 1.71 (1.18‐2.46)** | 2.03 (1.42‐2.91)*** | 1.83 (1.27‐2.65)** |
| High CIMT | 1.76 (1.27‐2.45)*** | 1.49 (1.05‐2.10)* | 1.68 (1.16‐2.43)** | 1.37 (0.93‐2.02) | 1.74 (1.25‐2.44)** | 1.41 (0.99‐2.01) | 1.79 (1.28‐2.51)** | 1.46 (1.02‐2.08)* |
| High LVMI | 2.22 (1.61‐3.07)*** | 1.70 (1.20‐2.40)** | 2.31 (1.61‐3.32)*** | 1.75 (1.19‐2.58)** | 2.48 (1.79‐3.45)*** | 1.83 (1.29‐2.60)** | 2.64 (1.90‐3.68)*** | 1.99 (1.39‐2.83)*** |
| Any subclinical CVD | 2.44 (1.77‐3.36)*** | 2.09 (1.51‐2.91)*** | 2.23 (1.56‐3.19)*** | 1.89 (1.31‐2.73)** | 2.46 (1.78‐3.41)*** | 2.06 (1.47‐2.88)*** | 2.46 (1.77‐3.42)*** | 2.08 (1.48‐2.92)*** |
BP, blood pressure; cfPWV, carotid‐femoral pulse wave velocity; CI, confidence interval; CIMT, carotid intima‐media thickness; CVD, cardiovascular disease; LVMI, left ventricular mass index; OR, odds ratio.
Multivariate models were adjusted for model 1: sex and childhood age; model 2: additionally included childhood body mass index and adult risk factors (smoking, drinking and physical inactivity).
*P < .05; **P < .01; ***P < .001.
Table 3 and Figure S1 present the performance of 4 definitions of pediatric elevated BP in predicting adult hypertension and subclinical CVD using receiver operating characteristic curve analysis. For any of the outcome variables, the Chinese, updated US, and international standards had higher sensitivity than the Fourth Report standards, but lower specificity. All standards had high negative predictive value (NPV). The Chinese standards performed equally compared with 3 other standards in predicting adult outcomes, except that the Chinese standards showed a significantly larger AUC for adult any subclinical CVD prediction in comparison with the Fourth Report standards (P = .002 for AUC comparison).
Table 3.
Performance of 4 definitions of childhood elevated BP in predicting adult outcomes based on ROC curve analysis
| Sensitivity, % | Specificity, % | PPV, % | NPV, % | AUC (95% CI) | P value for AUC difference | |
|---|---|---|---|---|---|---|
| Hypertension | ||||||
| Chinese BP standards | 38.4 | 84.4 | 26.6 | 90.3 | 0.614 (0.574‐0.655) | Ref |
| Fourth Report BP standards | 32.5 | 88.1 | 28.7 | 89.9 | 0.603 (0.564‐0.642) | .264 |
| International BP standards | 36.4 | 84.9 | 26.2 | 90.1 | 0.607 (0.567‐0.647) | .209 |
| Updated US standards | 37.1 | 85.6 | 27.5 | 90.2 | 0.613 (0.573‐0.653) | .927 |
| High cfPWV | ||||||
| Chinese BP standards | 25.4 | 84.9 | 35.8 | 77.4 | 0.551 (0.522‐0.580) | Ref |
| Fourth Report BP standards | 19.4 | 87.9 | 34.7 | 76.6 | 0.536 (0.510‐0.563) | .056 |
| International BP standards | 24.3 | 85.3 | 35.3 | 77.2 | 0.548 (0.519‐0.576) | .404 |
| Updated US standards | 24.3 | 86.0 | 36.5 | 77.4 | 0.551 (0.523‐0.580) | .997 |
| High CIMT | ||||||
| Chinese BP standards | 24.9 | 83.6 | 33.5 | 77.1 | 0.543 (0.515‐0.570) | Ref |
| Fourth Report BP standards | 19.1 | 87.0 | 32.7 | 76.4 | 0.531 (0.505‐0.556) | .108 |
| International BP standards | 23.9 | 84.2 | 33.3 | 76.9 | 0.540 (0.513‐0.568) | .667 |
| Updated US standards | 23.5 | 84.7 | 33.8 | 77.0 | 0.541 (0.514‐0.569) | .844 |
| High LVMI | ||||||
| Chinese BP standards | 28.0 | 84.6 | 37.6 | 78.0 | 0.563 (0.535‐0.591) | Ref |
| Fourth Report BP standards | 22.5 | 88.1 | 38.6 | 77.4 | 0.553 (0.527‐0.580) | .183 |
| International BP standards | 28.3 | 85.6 | 39.5 | 78.3 | 0.570 (0.542‐0.598) | .110 |
| Updated US standards | 28.3 | 86.3 | 40.7 | 78.4 | 0.573 (0.545‐0.601) | .076 |
| Any subclinical CVD | ||||||
| Chinese BP standards | 24.6 | 87.7 | 67.4 | 53.0 | 0.562 (0.540‐0.583) | Ref |
| Fourth Report BP standards | 18.9 | 90.0 | 66.1 | 51.8 | 0.544 (0.525‐0.564) | .002 |
| International BP standards | 23.7 | 88.3 | 67.6 | 52.8 | 0.560 (0.539‐0.582) | .636 |
| Updated US standards | 23.1 | 88.6 | 67.6 | 52.7 | 0.558 (0.537‐0.580) | .488 |
AUC, area under curve; BP, blood pressure; cfPWV, carotid‐femoral pulse wave velocity; CI, confidence interval; CIMT, carotid intima‐media thickness; CVD, cardiovascular disease; LVMI, left ventricular mass index; NPV, negative predictive value; PPV, positive predictive value; ROC, receiver operating characteristic.
Sensitivity analysis was conducted to test the robustness of our findings. First, we repeated all the analyses after excluding subjects who used antihypertensive medication in adulthood (n = 41) with similar results (data not shown). Second, we repeated all the analyses in subgroups by sex and age group (6‐11 vs 12‐17 years), and obtained similar results (data not shown). Third, we defined childhood hypertension and repeated all the analyses (Tables S1‐S2). After adjustment for sex, childhood age and BMI, and adult risk factors, any of 4 standards had the nonsignificant association with adult high cfPWV, high CIMT, high LVMI, and any subclinical CVD (Table S1; for all, P > .05).
4. DISCUSSION
In the present study, the prevalence of pediatric elevated BP was significantly higher according to the Chinese standards vs the Fourth Report, the updated US standards, and the international standards. Children with elevated BP diagnosed by any of these 4 standards had increased risks of adult hypertension, high cfPWV, and high LVMI. However, only 2 standards (the Chinese and updated US standards) can predict the increased risk of adult high CIMT. Our findings showed that there were significant differences in the prevalence of pediatric elevated BP among 4 standards, and the Chinese standards performed equally or better compared with 3 other standards in predicting adult hypertension and subclinical CVD.
The Chinese, Fourth Report, and updated US standards were established based on the large and nationally representative samples, BP values obtained using auscultation, and statistical approaches.11, 14, 19 The updated US standards used the same reference population as the Fourth Report standards but excluded overweight and obese children.14 The establishment of international standards was based on the nationally representative datasets from 7 countries.20 To reduce the long‐term risk of CVD, it is still unclear whether the Chinese standards are more appropriate to identify Chinese children with elevated BP than other standards.
Both the Fourth Report and updated US standards were established based on the US pediatric samples. Given the distribution of BP values varied across different ethnic groups and geographic areas,15, 16 these 2 standards should be used with caution in the Chinese population. The Fourth Report or updated US standards may result in unpredictable bias when identifying childhood elevated BP in other countries. In this study, 76.2% and 90.2% of children with elevated BP, diagnosed by the Chinese standards, were confirmed by the Fourth Report and updated US standards, respectively. The differences in the prevalence of pediatric elevated BP were significant between the Chinese and Fourth Report or updated US standards. In addition, the Bogalusa Heart Study demonstrated that the Fourth Report standards had the ability to predict the increased risks of adult hypertension and subclinical CVD in the US population.6 Our findings indicated that the Fourth Report standards cannot predict increased risk of adult high CIMT in the Chinese population. The inconsistent results may mainly be attributed to ethnic difference.
The significant differences in the prevalence of pediatric elevated BP between the Chinese and international standards were observed in our study. Based on logistic regression analysis, the Chinese standards performed equally in predicting adult hypertension, high cfPWV, and high LVMI, and better at predicting adult high CIMT in comparison with international standards. In addition, the international standards had the main limitation that they did not include children aged 3‐5 years.20 The current guidelines recommended that BP should be measured routinely in children age 3 years and older.10, 11, 12 Taken together, caution should be used in using international standards in Chinese children.
The strengths of this study included the design of the prospective cohort study and the high quality of data measurement. However, the study had potential limitations. First, the Beijing BP Cohort Study did not include children younger than 6 years at baseline, and we cannot compare the ability of different standards in predicting subclinical cardiovascular outcomes based on these populations. Further prospective studies are needed to fill this gap. Second, almost half of the participants were not successfully followed up. However, there was no significant difference in baseline characteristics between participants who were successfully followed up and those who were lost to follow‐up (Table S3). Third, the number of hypertensive children was small, which might result in insufficient statistical power in the analyses of childhood hypertension in relation to adult subclinical CVD (Table S1). Fourth, participants who were successfully followed up seemed to be exposed to smoking, drinking, and were overweight far more than the general population in the similar age group in China. Therefore, the association between childhood elevated BP and subclinical CVD in adulthood may be overestimated. Fifth, the setting of the BP measurement may have affected the diagnosis of hypertension in adulthood. Many hypertensive patients may have white‐coat hypertension at follow‐up. Ambulatory BP monitoring is indispensable for identifying white‐coat hypertension. Unfortunately, relevant data were not available in this cohort. Sixth, this cohort study cannot provide cause‐and‐effect association between childhood elevated BP and subclinical CVD in adulthood. Finally, BP in childhood was measured only once at baseline and no other determination of hypertension was performed during the follow‐up, which may affect the association between childhood BP and the development of end‐organ damage during adulthood.
In conclusion, the present study showed that there were the significant differences in the prevalence of pediatric elevated BP among 4 different standards, and the Chinese standards performed equally or better in predicting adult hypertension and subclinical CVD in comparison with the Fourth Report and updated US and international standards. Our results indicated that the Chinese standards seem to be more appropriate to monitor the prevalence of childhood elevated BP and identify Chinese children with elevated BP for reducing the long‐term risk of CVD.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Study concept and design: JM. Acquisition, analysis, or interpretation of data: HF, JM. Drafting of the manuscript: HF. Critical revision of the manuscript for important intellectual content: HF, YY, JM. Statistical analysis: HF. Obtained funding: JM. Administrative, technical, or material support: DH, JL, YY, JM. Study supervision: JM.
Supporting information
ACKNOWLEDGMENTS
This study was supported by the National Key Research and Development Program of China (2016YFC1300101), National Nature Science Foundation of China (81172746), Beijing Key Science and Technology Program (D111100000611002), Beijing Health System Leading Talent Grant (2009‐1‐08), and the Beijing Training Project for the Leading Talents in S&T (2011LJ07).
Fan H, Hou D, Liu J, Yan Y, Mi J. Performance of 4 definitions of childhood elevated blood pressure in predicting subclinical cardiovascular outcomes in adulthood. J Clin Hypertens. 2018;20:508–514. 10.1111/jch.13201
REFERENCES
- 1. Ingelfinger JR. The child or adolescent with elevated blood pressure. N Engl J Med. 2014;370:2316‐2325. [DOI] [PubMed] [Google Scholar]
- 2. Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113:328‐333. [DOI] [PubMed] [Google Scholar]
- 3. Daniels SR, Loggie JM, Khoury P, Kimball TR. Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation. 1998;97:1907‐1911. [DOI] [PubMed] [Google Scholar]
- 4. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta‐regression analysis. Circulation. 2008;117:3171‐3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aatola H, Magnussen CG, Koivistoinen T, et al. Simplified definitions of elevated pediatric blood pressure and high adult arterial stiffness. Pediatrics. 2013;132:e70‐e76. [DOI] [PubMed] [Google Scholar]
- 6. Xi B, Zhang T, Li S, et al. Can pediatric hypertension criteria be simplified? A prediction analysis of subclinical cardiovascular outcomes from the Bogalusa Heart Study. Hypertension. 2017;69:522‐528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Law MR, Wald NJ. Risk factor thresholds: their existence under scrutiny. BMJ. 2002;324:1570‐1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Falkner B. Recent clinical and translational advances in pediatric hypertension. Hypertension. 2015;65:926‐931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blumenthal S, Epps RP, Heavenrich R, et al. Report of the task force on blood pressure control in children. Pediatrics. 1977;59(suppl 52):797‐820. [PubMed] [Google Scholar]
- 10. Daniels SR. How to define hypertension in children and adolescents. Circulation. 2016;133:350‐351. [DOI] [PubMed] [Google Scholar]
- 11. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555‐576. [PubMed] [Google Scholar]
- 12. Lurbe E, Agabiti‐Rosei E, Cruickshank JK, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887‐1920. [DOI] [PubMed] [Google Scholar]
- 13. Kidy F, Rutebarika D, Lule SA, et al. Blood pressure in primary school children in Uganda: a cross‐sectional survey. BMC Public Health. 2014;14:1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flynn JT, Kaelber DC, Baker‐Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904. [DOI] [PubMed] [Google Scholar]
- 15. Cantinotti M, Giordano R, Scalese M, et al. Strengths and limitations of current pediatric blood pressure nomograms: a global overview with a special emphasis on regional differences in neonates and infants. Hypertens Res. 2015;38:577‐587. [DOI] [PubMed] [Google Scholar]
- 16. Ataei N, Hosseini M, Fayaz M, et al. Blood pressure percentiles by age and height for children and adolescents in Tehran, Iran. J Hum Hypertens. 2015;17:142‐151. [DOI] [PubMed] [Google Scholar]
- 17. Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS. Blood pressure percentiles by age and height from non‐overweight children and adolescents in Germany. Pediatrics. 2011;127:e978‐e988. [DOI] [PubMed] [Google Scholar]
- 18. Kułaga Z, Litwin M, Grajda A, et al. Oscillometric blood pressure percentiles for Polish normal‐weight school‐aged children and adolescents. J Hypertens. 2012;30:1942‐1954. [DOI] [PubMed] [Google Scholar]
- 19. Fan H, Yan Y, Mi J. Updating blood pressure references for Chinese children aged 3‐17 years. Chin J Hypertens. 2017;25:428‐435. [Google Scholar]
- 20. Xi B, Zong X, Kelishadi R, et al. Establishing international blood pressure references among non‐overweight children and adolescents aged 6‐17 years. Circulation. 2016;133:398‐408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liang Y, Hou D, Shan X, et al. Cardiovascular remodeling relates to elevated childhood blood pressure: Beijing blood pressure cohort study. Int J Cardiol. 2014;177:836‐839. [DOI] [PubMed] [Google Scholar]
- 22. Yan Y, Hou D, Liu J, et al. Childhood body mass index and blood pressure in prediction of subclinical vascular damage in adulthood: Beijing blood pressure cohort. J Hypertens. 2017;35:47‐54. [DOI] [PubMed] [Google Scholar]
- 23. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M‐mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072‐1083. [DOI] [PubMed] [Google Scholar]
- 24. de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol. 1995;25:1056‐1062. [DOI] [PubMed] [Google Scholar]
- 25. Gonen M. Analyzing Receiver Operating Characteristic Curves with SAS. Cary, NC: SAS Publishing; 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


