Abstract
Home blood pressure (BP) monitoring is endorsed in multiple guidelines as a valuable adjunct to office BP measurements for the diagnosis and management of hypertension. In many countries throughout Asia, physicians are yet to appreciate the significant contribution of BP variability to cardiovascular events. Furthermore, data from Japanese cohort studies have shown that there is a strong association between morning BP surge and cardiovascular events, suggesting that Asians in general may benefit from more effective control of morning BP. We designed the Asia BP@Home study to investigate the distribution of hypertension subtypes, including white‐coat hypertension, masked morning hypertension, and well‐controlled and uncontrolled hypertension. The study will also investigate the determinants of home BP control status evaluated by the same validated home BP monitoring device and the same standardized method of home BP measurement among 1600 or more medicated patients with hypertension from 12 countries/regions across Asia.
Keywords: Asia, blood pressure control, home blood pressure monitoring, hypertension
1. INTRODUCTION
Hypertension, the leading preventable cause of premature mortality worldwide, affects an estimated 1.4 billion persons, with the majority of these residing in low‐ and middle‐income countries.1, 2, 3 In Asia, the burden of hypertension is particularly high, with some countries continuing to experience increasing rates of mortality from cardiovascular disease (CVD) along with low rates of hypertension control and awareness.4, 5, 6, 7
Dramatic improvements in the rate of CVD mortality are possible, as shown by a 37% reduction in Korea between 2000 and 2012 as a consequence of improved hypertension awareness, treatment, and control rates.6 Effective screening and diagnosis are also critical for the prevention of CVD mortality and management of hypertension. To this end, there is a growing recognition for the role of out‐of‐office blood pressure (BP) monitoring.8
In several parts of Asia, home BP monitoring (HBPM) is recognized in hypertension guidelines as a valuable adjunct to conventional office BP measurements9, 10, 11, 12 and is supported by regional data. For example, the Ohasama study in Japan showed that measurement of BP using HBPM had a stronger predictive power for mortality than office‐based BP screening.13 In Japanese patients with essential hypertension receiving antihypertensive therapy, the HONEST (Home Blood Pressure Measurement With Olmesartan Naive Patients to Establish Standard Target Blood Pressure) study14 demonstrated a relationship between HBPM threshold BP values and risk of a major cardiovascular event. Furthermore, several reports confirmed that HBPM‐guided antihypertensive therapy was effective in preventing target organ damage.15, 16 Importantly, even when office BP is well controlled, uncontrolled masked morning hypertension with residual cardiovascular risk should still be a target for the management of hypertension.17, 18
In addition, BP variability (BPV) is an important risk factor for CVD, independent of average BP. This finding is reinforced by the results of a meta‐analysis showing that in the case of office‐based BP measurements, visit‐to‐visit variability was moderately associated with CVD and all‐cause mortality.19 In the Ohasama study, the day‐to‐day BPV was an independent predictor of cardiovascular mortality.20 In the J‐CORE (Japan‐Combined Treatment With Olmesartan and a Calcium Channel Blocker Versus Olmesartan and Diuretics Randomized Efficacy) study, home BPV was significantly associated with measures of organ damage such as left ventricular mass index, carotid intima‐media thickness, and urinary albumin/creatinine ratio independent of the average home BP measurements.21 However, the indices of BPV differ for home and office settings, which make it difficult to provide a clear message for clinical practice.22
BPV may be greater in Asians than in the Western population. In a recent international collaboration study, morning BP surge was greater in Japanese patients with hypertension than in Spanish and Italian patients.23 Similarly, morning and nocturnal BP surges were greater in Japanese patients with drug‐resistant hypertension when compared with US patients recruited by the same global inclusion and exclusion criteria for a clinical trial of catheter‐based renal denervation.24 Exaggerated morning BP surge was also found to be an independent risk factor for stroke in elderly Japanese patients with hypertension.25 Taken together, these studies suggest that morning BP monitoring may be clinically relevant in the management of hypertension by identifying patients with morning BP surge who may benefit more from long‐acting antihypertensive drugs.18
As dietary intake of salt is typically higher in the Asian population than the Western population, and as higher salt intake decreases renin‐angiotensin system activity, the BP‐lowering effect of renin‐angiotensin system inhibitors may be weaker than that of calcium channel blockers in Asian patients with hypertension. In addition, calcium channel blockers are likely to reduce BPV more extensively than other drugs,26 and this tendency may be more clearly observed in Asian patients with hypertension than those in the Western population.
In Asia, where not only are the hypertension awareness and control rates low, but many physicians are yet to appreciate the influence of BPV on cardiovascular outcomes, there is a plausible benefit in conducting research into HBPM to enhance current recommendations for clinical practice. However, there is no Pan‐Asian study on the control status of home BP using the same validated HBPM device and the same standardized method of home BP measurements across the region.
Therefore, using the same HBPM device, we designed the Asia BP@Home study with the intention of collecting and analyzing data from across 12 territories in Asia, not only to determine relevant indices of BPV in the home setting, but also to undertake an epidemiological evaluation of masked morning hypertension, white‐coat hypertension, uncontrolled hypertension, and well‐controlled hypertension in the region. This study is designed to complement previous recommendations of the World Hypertension League on BP measurement. Herein, we report the study methodology.
2. METHODS
2.1. Study protocol
The study protocol described herein was approved by the institutional review board of Jichi Medical University, Japan, with each participating institution seeking local approval based on its own ethical guidelines. The Asia BP@Home study is a prospective, multicenter, noninterventional study designed to collect home BP data among people with hypertension living in Asia. Patients are to be enrolled from China, Hong Kong, India, Indonesia, Japan, Korea, Malaysia, Pakistan, Philippines, Singapore, Taiwan, and Thailand.
2.2. Objectives
This study is designed to investigate: (1) the proportion of patients who meet predefined criteria for masked morning hypertension, white‐coat hypertension, uncontrolled hypertension, and well‐controlled hypertension based on home BP measurements; and (2) the normal range (90th percentile of standard deviation [SD]) and difference in home BPV among each territory.
2.3. Patient recruitment
Patients living in Asia aged 20 years and older with a diagnosis of hypertension and who are receiving stable doses of antihypertensive medications for ≥3 months are eligible irrespective of whether they have additional risk factors, such as left ventricular hypertrophy, other specified abnormalities on electrocardiogram, type 2 diabetes mellitus, smoking status, hyperlipidemia, chronic kidney disease, coronary artery disease, previous stroke or transient ischemic attack, or peripheral arterial disease (Table). In addition, patients are informed of the purpose and methodology of the study, their right to withdraw at any time, and the measures taken to protect their privacy. After providing written informed consent, patients will be enrolled and their data collected.
Table 1.
Inclusion criteria of the Asia BP@Home study
| Patients living in Asia |
| Age ≥20 years |
| Patients with a diagnosis of hypertension |
| Patients receiving stable doses of antihypertensive medication for ≥3 mo |
| Patients from whom written informed consent was obtained |
2.4. Study procedures
At the initial study visit (visit 1, day 0) during which patients will be screened for eligibility and provide their written informed consent, eligible patients will have their sex, age, birth date, height, weight, and waist and hip circumferences recorded. Medical history includes family history of hypertension, duration of hypertension and antihypertensive therapy, current medication status, and the presence of additional risk factors including diabetes mellitus, hyperlipidemia, carotid artery disease, thoracic aortic aneurysm, chronic kidney disease, atrial fibrillation, history of angina pectoris, myocardial infarction, aortic dissection, peripheral artery disease, stroke (ischemic, hemorrhagic, or other), and congestive heart failure. The following information will also be collected: smoking and drinking habits and whether they are a shift worker. This information, together with the patient's vital signs, including office systolic BP (SBP), diastolic BP, and heart rate (HR), will be recorded on a patient registration form specifically designed for the study. Antihypertensive medications will be categorized by generic name, class, and dosing schedule. Patients will be provided with a validated HBPM device (Omron HEM‐7130‐AP or HEM‐7131‐E) and instructed in its use at the first study visit. At a second study visit (visit 2, day 8–15), the investigator will obtain documentation from each patient regarding recorded home BP data and retrieve the HBPM device.
2.5. Home BP monitoring
Patients will be instructed to measure their BP at home using the provided HBPM device twice in the morning and twice at bedtime for at least 7 days during a 15‐day period. The morning measurements are to be taken within 1 hour after waking, following urination, before taking any medications, before eating breakfast, and after 2 minutes of rest while in a sitting position. Patients will be instructed to lean against a seat back and rest both feet on the floor, with no moving or talking. The bedtime measurements are to be taken immediately before going to bed and after 2 minutes of rest while in a sitting position as before. The interval between the two measurements should be at least 1 minute. BP measurements should be taken from the nondominant arm in the upper arm area. However, if BP readings of the right and left arms differ significantly, patients will be instructed to use the arm with the highest BP––as determined at the first study visit––for use for all subsequent home BP measurements. Patients will be instructed to document the BP values on a sheet provided for all participants and to return this sheet for reporting purposes at the second visit. This sheet includes a set of simple instructions for taking home BP measurements, as well as space for recording up to 15 days of HBPM values, including the time of the first and second measurements on waking and at bedtime, and the SBP, diastolic BP, and pulse values.
2.6. Antihypertensive drugs and concomitant drug use
No restrictions will be placed on antihypertensive drug treatment or concomitant use of other medications. The information of the daily dose and the classes of antihypertensive drugs, and the timing of dosing will be collected.
2.7. Outcomes
The primary outcome measure is the distribution of masked morning, white‐coat, uncontrolled, and well‐controlled hypertension in the overall study sample. SBP measurements of 135 mm Hg and 140 mm Hg obtained by HBPM and office BP measurement, respectively, will be used as cutoff values for defining hypertension. The secondary outcome measure is the mean and SD of home BP values.
2.8. Statistical analysis
Since this study is observational and there is no plan to conduct formal hypothesis testing, sample size calculations are not applicable. A planned sample size of at least 1600 patients across 12 territories was selected to obtain a representative cross‐sectional sample of outpatients with hypertension in Asia. The planned enrollment includes at least 100 patients in each of Hong Kong, India, Japan, Malaysia, Pakistan, Singapore, Taiwan, and Thailand, and at least 200 patients in each of China, Indonesia, Korea, and the Philippines. The mean home SBP (morning SBP, evening SBP, and the average of morning and evening SBPs) vs the mean clinic SBP values of each patient will be plotted to obtain overall and per‐territory estimates of each hypertension subtype (Figure). The Chi‐square test will be used to evaluate the differences in prevalence of each hypertension subtype in each country. The SD of home BP (morning SBP, evening SBP, and the average of morning and evening SBP values) of each patient will be calculated as the measure of home BPV. We will assess the difference in the SD of home BP among each country/region. Finally, we will identify the determinants of four different hypertension subgroups, and of the mean home SBP and SD of home SBP. Possible determinants are age, sex, body mass index, chronic kidney disease, diabetes mellitus, history of CVD, and different classes of antihypertensive drugs. Associations or differences with a P value <.05 (two‐tailed) will be considered statistically significant. All statistical analyses will be conducted by Super Circulation Monitoring With High Technology R&D Center, Jichi Medical University COE Cardiovascular Research and Development Center (JCARD) (Tochigi, Japan).
Figure 1.
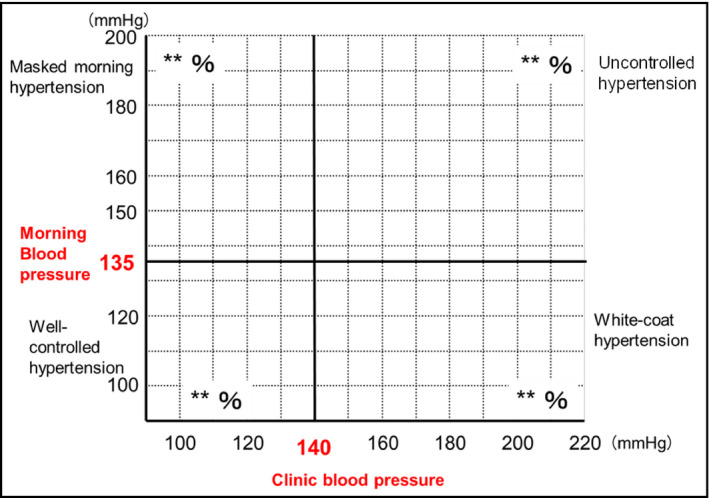
Template distribution plot showing cutoffs for hypertension according to home‐ and office‐based blood pressure measurements. The distribution of masked morning, white‐coat, uncontrolled, and well‐controlled hypertension is based on aggregate data
3. DISCUSSION
The use of HBPM is emphasized in guidelines for its role in diagnosing and managing hypertension.10 The importance of HBPM in patients with hypertension on treatment was demonstrated in the HONEST study, which reported that uncontrolled morning hypertension before taking medication was significantly associated with a high risk of both stroke and coronary artery disease even in patients whose office BP was well controlled.14, 27 Moreover, a higher morning BP surge was shown in a Japanese cohort study than in a Western cohort study.28 Thus, Asians in general may benefit from more effective control of morning BP as an initial step to reducing overall BPV associated with nocturnal BP dipping and morning surge.29 Especially to achieve well‐controlled home morning BP and to reduce home BPV, long‐acting calcium channel blockers may be the most effective antihypertensive drug class, because their BP‐lowering effect is independent of salt intake.
One important area of research that requires further investigation is masked morning hypertension, as its presence may be caused by the loss of BP‐lowering effects of antihypertensive drugs with shorter half‐lives or through patients not taking medication at night. This study will provide data on the distribution of masked morning hypertension in Asia and allow an investigation into its possible cause.
There is some discrepancy among the guidelines in the optimal time of the evening home BP measurement. The ESH 2010 guidelines recommend measuring evening home BP before dinner,30 while the Japanese Society of Hypertension (JSH) 2014 guidelines recommend measurement just before going to bed.10 In a recent study, the at‐bedtime minus the before‐dinner home SBP was −8.7 mm Hg. This reduction is largely affected by consumption of alcohol and taking a bath.31 This depressor effect of bathing significantly persists for 2 hours. Thus, day‐to‐day variability of evening home BP depends largely on daily lifestyle activities. As having dinner outside of the home is common in Asia, it is difficult to measure evening BP before dinner. Thus, considering the Asian lifestyle, morning BP may be a better measure than evening BP to exclude the effects of different evening activities and to more accurately determine the pathophysiology of BPV. The two guidelines also differ on the recommended rest period before measuring home BP, with the ESH guidelines recommending at least 5 minutes and the JSH guidelines recommending 1 to 2 minutes. We chose at least 2 minutes rest for our study as this is more practical and convenient for patients and in line with the JSH recommendations.
In addition to offering prognostic significance for patients receiving treatment, HBPM is ideally suited to the measurement of morning BP since it offers patients convenience. In addition, information and communication technology–based HBPM is beneficial for patients who live in remote Asian geographical locations.32, 33 However, in the wider region, there is uncertainty among practitioners in Asia as to how best to integrate this technology into clinical practice.
CONCLUSIONS
The data on the control status of home BP and its determinants—through which to explore the known benefits of HBPM in a local context—are limited throughout most of Asia. Thus, the Asia BP@Home study plans to investigate the distribution of hypertension subtypes based on the control status of office and home BP measurements and the determinants of home BP control status in patients with hypertension who live in 12 territories in Asia. The Asia BP@Home study will clarify the current control status and determinants of home BP in each Asian territory and facilitate better home BP management, resulting in reduced CVD and renal disease across Asia.
DISCLOSURES
CH Chen has received honoraria for serving as a speaker or member of a speakers’ bureau for AstraZeneca, Bayer AG, Boehringer Ingelheim, Bristol‐Myers Squibb, Daiichi Sankyo, Merck & Co, Novartis, Pfizer, Sanofi, Servier, and Takeda. YC Chia has received honoraria for serving as a speaker or advisor for Abbott, Bayer, Boehringer Ingelheim, Merck, MSD, Novartis, Pfizer, Reckitt Benckiser, Sanofi, Servier, and Takeda; sponsorship to scientific conferences from Pfizer and Takeda; and research grants from Pfizer. K Kario has received research grants from A&D Co., Bayer Yakuhin, Boehringer Ingelheim, Daiichi Sankyo, EA Pharma, Fukuda Denshi, Medtronic, Mitsubishi Tanabe Pharma Corporation, Mochida Pharmaceutical Co., Omron Healthcare, Otsuka, Pfizer, Takeda, and Teijin Pharma; and honoraria from Daiichi Sankyo, Omron Healthcare, and Takeda. S Park has received honoraria from Astellas and Pfizer and consultation fees from Takeda. S Siddique has received honoraria from Bayer, Novartis, Pfizer, Sanofi Aventis, and Servier; and travel, accommodation, and conference registration support from Atco Pharmaceutical, Bayer, Highnoon Laboratories, Novartis, Pfizer, Sanofi Aventis, and Servier. GP Sogunuru has received a research grant related to hypertension monitoring and treatment from Pfizer. L Wong has received nonfinancial support as an advisory board member for Pfizer. All other authors report no potential conflict of interest in relation to this article.
ACKNOWLEDGMENTS
This study is supported by an Investigator‐Initiated Research grant from Pfizer, and Omron Healthcare who provided the use of computer servers to store study‐related data. The protocol for the study was developed by Jichi Medical University School of Medicine. Pfizer was not involved in the development of the protocol nor this article. The authors acknowledge medical writing support from Chris Facey and Howard Christian of MIMS (Hong Kong) Limited, and Ayako Okura, editorial coordinator of Jichi Medical University School of Medicine, Japan.
Kario K, Tomitani N, Buranakitjaroen P,et al. Rationale and design for the Asia BP@Home study on home blood pressure control status in 12 Asian countries and regions. J Clin Hypertens. 2018;20:33–38. 10.1111/jch.13145
This study is designed to complement previous recommendations of the World Hypertension League on blood pressure measurement.
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903‐1913. [DOI] [PubMed] [Google Scholar]
- 2. Park JB, Kario K, Wang JG. Systolic hypertension: an increasing clinical challenge in Asia. Hypertens Res. 2015;38:227‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population‐based studies from 90 countries. Circulation. 2016;134:441‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Castillo R. SSA 03‐1 Prevalence and management of hypertension in Southeast Asia. J Hypertens. 2016;34(suppl 1):e4. [Google Scholar]
- 5. Gupta R. SSA 02‐3 trend in hypertension epidemiology in South Asia. J Hypertens. 2016;34(suppl 1):e2. [Google Scholar]
- 6. Suh I. PL 01‐2 blood pressure and cardiovascular disease mortality in the Asia Pacific region. J Hypertens. 2016;34:e11. [DOI] [PubMed] [Google Scholar]
- 7. Chia YC, Buranakitjaroen P, Chen CH, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia Network. J Clin Hypertens (Greenwich) 2017;19:1192‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sheppard JP, Schwartz CL, Tucker KL, McManus RJ. Modern management and diagnosis of hypertension in the United Kingdom: home care and self‐care. Ann Glob Health. 2016;82:274‐287. [DOI] [PubMed] [Google Scholar]
- 9. Wang JG, for the China HBPM Consensus Expert Panel . Home blood pressure monitoring: a China consensus document. Chin J Hypertens. 2012;20:525‐529. [Google Scholar]
- 10. Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253‐390. [DOI] [PubMed] [Google Scholar]
- 11. Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1‐47. [DOI] [PubMed] [Google Scholar]
- 12. Shin J, Park JB, Kim K, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part I–epidemiology and diagnosis of hypertension. Clin Hypertens. 2015;21:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population‐based observation in Ohasama Japan. J Hypertens. 1998;16:971‐975. [DOI] [PubMed] [Google Scholar]
- 14. Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large‐scale prospective, real‐world observational study. Hypertension. 2014;64:989‐996. [DOI] [PubMed] [Google Scholar]
- 15. Kario K, Matsui Y, Shibasaki S, et al. An alpha‐adrenergic blocker titrated by self‐measured blood pressure recordings lowered blood pressure and microalbuminuria in patients with morning hypertension: the Japan Morning Surge‐1 Study. J Hypertens. 2008;26:1257‐1265. [DOI] [PubMed] [Google Scholar]
- 16. Kario K, Hoshide S, Shimizu M, et al. Effect of dosing time of angiotensin II receptor blockade titrated by self‐measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge‐Target Organ Protection (J‐TOP) study. J Hypertens. 2010;28:1574‐1583. [DOI] [PubMed] [Google Scholar]
- 17. Kario K. Essential Manual of 24‐Hour Blood Pressure Management from Morning to Nocturnal Hypertension. London, UK: Wiley‐Blackwell; 2015:1‐138. [Google Scholar]
- 18. Wang JG, Kario K, Park JB, Chen CH. Morning blood pressure monitoring in the management of hypertension. J Hypertens 2017;35:1554‐1563. [DOI] [PubMed] [Google Scholar]
- 19. Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit‐to‐visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895‐905. [DOI] [PubMed] [Google Scholar]
- 20. Kikuya M, Ohkubo T, Metoki H, et al. Day‐by‐day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52:1045‐1050. [DOI] [PubMed] [Google Scholar]
- 21. Matsui Y, Ishikawa J, Eguchi K, Shibasaki S, Shimada K, Kario K. Maximum value of home blood pressure: a novel indicator of target organ damage in hypertension. Hypertension. 2011;57:1087‐1093. [DOI] [PubMed] [Google Scholar]
- 22. Dolan E, O'Brien E. Is it daily, monthly, or yearly blood pressure variability that enhances cardiovascular risk? Curr Cardiol Rep. 2015;17:93. [DOI] [PubMed] [Google Scholar]
- 23. Hoshide S, Kario K, de la Sierra A, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015;66:750‐756. [DOI] [PubMed] [Google Scholar]
- 24. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic diurnal blood pressure variability between Japanese and American treatment‐resistant hypertensive populations. Circ J. 2017;81:1337‐1345. [DOI] [PubMed] [Google Scholar]
- 25. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401‐1406. [DOI] [PubMed] [Google Scholar]
- 26. Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive‐drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta‐analysis. Lancet. 2010;375:906‐915. [DOI] [PubMed] [Google Scholar]
- 27. Kario K, Saito I, Kushiro T, et al. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST study. J Am Coll Cardiol. 2016;67:1519‐1527. [DOI] [PubMed] [Google Scholar]
- 28. Hoshide S, Yano Y, Haimoto H, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan morning surge‐home blood pressure study. Hypertension. 2016;68:54‐61. [DOI] [PubMed] [Google Scholar]
- 29. Kario K. Perfect 24‐h management of hypertension: clinical relevance and perspectives. J Hum Hypertens. 2016;31:231‐243. [DOI] [PubMed] [Google Scholar]
- 30. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779‐785. [DOI] [PubMed] [Google Scholar]
- 31. Fujiwara T, Hoshide S, Noshizawa M, Matsuo T, Kario K. Difference in evening home blood pressure between before dinner and at bedtime in Japanese elderly hypertensive patients. J Clin Hypertens (Greenwich). 2017;19:731‐739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaihara T, Eguchi K, Kario K. Home BP monitoring using a telemonitoring system is effective for controlling BP in a remote island in Japan. J Clin Hypertens (Greenwich). 2014;16:814‐819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kario K. Evidence and perspectives on the 24‐hour management of hypertension: hemodynamic biomarker‐initiated ‘anticipation medicine’ for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262‐281. [DOI] [PubMed] [Google Scholar]


