Abstract
Results of the SPRINT study have been disputed, based on the assumption that unattended BP measurements do not correlate with usual BP measurements. In this study, the authors investigated the correlation of unattended SPRINT‐like measurements with other conventional measurements. All BP measurements were taken with the patient seated in a comfortable chair with the legs uncrossed and not speaking during the procedure. For the purpose of this study, sixty‐five patients, mostly male (93%), were recruited from our hypertension clinic and all were on antihypertensive medication (av 3.0 ± 1.1). Patients were at high cardiovascular risk with high rates of comorbidities, av age 68 ± 12 years, 49% with diabetes, 34% with mild CKD (CKD 1‐3, average eGFR 55.0 ± 13 mL/min/1.73 m2), and 20% with history of stable coronary artery disease. All BP measurements were similar with no statistically significant difference (one‐way ANOVA, P = 0.621). Compared to unattended SPRINT BP values (139.77 ± 19.22/75.42 ± 11.72 mm Hg), the clinic BP measurements were numerically slightly higher but with a NS P value (P = 0.163). Similarly, unattended BP measurements were similar to values taken by the clinic physician. In a smaller cohort of 11 patients, the authors compared unobserved vs observed SPRINT‐like BP measurements, and in 13 patients, the authors compared unobserved SPRINT‐like BP measurements to average home BP measurements (Table 3). There were no significant differences between any of the subgroups (one‐way ANOVA, P = 0.816 for systolic and P = 0.803 for diastolic). The authors conclude that unattended BP measurements taken (the SPRINT way) are similar to other conventional office blood pressure measurements.
Keywords: auscultatory BP, automated office blood pressure, conventional BP, unattended SPRINT BP
1. INTRODUCTION
Hypertension is a powerful cardiovascular risk factor, and treatment and control of hypertension obviate most of that risk.1, 2 Blood pressure is, however, a dynamic measure and varies in many different ways. It can vary from beat to beat, minute to minute, and certainly from visit to visit. Furthermore, blood pressure can vary depending on patient's physical status, position, emotional status, and the presence of external influences, such as the presence a threat, fear, or a white coat. Although blood pressure is closely related to the degree of target organ involvement3 and degree of cardiovascular risk,4, 5 the optimal method of BP measurement that closely relates to cardiovascular risk has not been clearly determined. Since 1944, Smirk6 pointed out the need to measure basal BP devoid of external influences: “The lability of the blood pressure in a case of essential hypertension may be judged by the degree of difference between the casual and basal pressures. Measurements of the basal pressure, whatever technique be adopted to obtain it, aim at removing these known causes of variation and at measuring a pressure that has been obtained under standard conditions of mental and physical rest.” The difference between basal and casual blood pressure was called supplemental BP. It was thought then, and it is still believed today that some kind of “basal” BP correlates best with hypertension‐related events, whereas supplemental BP or BP elevations due to white coat effect or other external factors correlate poorly. The basal BP of Smirk was measured “after the patients were fasted overnight for 10‐12 hours and, next morning, were transferred in their beds to a quiet, warm examination room where they rested for a period of half an hour. At the end of this time, the observer entered and measured the blood pressure.” Measurements were taken with a mercury manometer in the supine position. Since then, things evolved and methods have changed. Seated position is widely acceptable nowadays, and mercury manometers have been replaced by oscillometric or automated devices (primarily due to toxicity from mercury). Nonetheless obtaining the patient's true or “basal” BP, devoid of external influences remained important. Guidelines have recommended that BP needs to be measured accurately and emphasized the need to avoid systematic errors. Optimally, patients should be seated in a quiet examination room for >5 min with legs uncrossed, feed on the floor, back supported, and neither the patient nor the health care professional talking during the resting period or the BP measurement. Furthermore, avoidance of caffeine, exercise, and smoking for at least 30 minutes before BP measurement has always been considered essential. Recommendations on how to prepare the patient, how to use the proper technique, and how to take proper measurements to diagnose and treat hypertension have explicitly been stated in the newly published ACC/AHA guidelines.7
Following the publication of SPRINT (Systolic Blood Pressure Intervention Trial)8 that demonstrated substantial benefits from intensive BP control, an intense debate erupted in the literature9, 10 contesting the validity of the SPRINT results. The main argument was that the method used to measure blood pressure in SPRINT was “unattended” automated office BP (AOBP) and thus different from measurements used in any daily practice or other studies. Furthermore, it has been speculated that the “unattended” BP measurement utilized in SPRINT had grossly underestimated the true value of achieved BP by up to 20 mm Hg. Thus targeting low BP levels as measured in SPRINT, it was considered inappropriate and perhaps dangerous.11 This hypothesis has been endorsed by a recent (but potentially flawed) publication12 that reported a difference of 16 mm Hg between unattended automated and manual office BP. Recently, the debate has intensified13, 14, 15 and expected to continue with the publication of the new ACC/AHA guidelines.7 Although some studies have attempted to compare AOBP to other office BP measurements, home or ambulatory measurement, carefully done studies comparing AOBP to all possible conventional office BP methods during the same visit in the usual clinic environment have not been done.
In this study, therefore, we compared the unattended AOBP to office BP taken by the clinic nurse, AOBP taken by the clinic physician, and auscultatory BP also taken by the clinic physician. In a smaller sample, we also compared unattended AOBP to BP taken with the SPRINT device but with the SPRINT nurse present. The study was approved by the institutional ethics committee.
2. METHODS
Patients were recruited from the hypertension and vascular medicine clinic of the Veterans Administration Medical Center in Washington DC. The clinic is held on the second floor of the hospital, in a large, but quite wing. There is a waiting area with TV to help patients relax. Patients are first seen in the nursing station where an experienced nurse checks BPs with the methods described below. Patients are given time to relax and ask questions. The clinic is supervised by an experienced hypertension expert and patients are seen by second‐year nephrology fellows (male or female). All patients signed informed consent prior to enrollment in the study. Sixty‐five patients referred for resistant or difficult to control hypertension were included in the study. Patients with known secondary causes of hypertension or end‐stage diseases (such as COPD, terminal cancer, or end‐stage renal disease) that would affect blood pressure (BP) measurements were excluded from the study. We elected to enroll patients attending the regular resistant or difficult to control hypertension clinic so to have patients in their usual clinic environment and actually use the same equipment and methods used in daily practice and/or research (in the case of SPRINT measurements). In all instances, BP was measured with the patients seated in a comfortable chair, with the back supported, feet on the floor, uncrossed, and neither the patient nor the health care professional talking. Patients were advised to avoid caffeine or smoking for at least 3 hours prior to clinic visit. For the clinic BP measurements, we used a commercially available automated BP monitor (Dinamap ProCare DPC 400 Vital Signs Monitor), which has been validated and calibrated at yearly intervals. For auscultatory measurements by the clinic physician, we used a validated aneroid sphygmomanometer and a stethoscope, and for the SPRINT measurements, the automated Omron 907 model (Omron Healthcare, Lake Forest, IL, USA). All measurements were taken during the same clinic visit in the same clinic area, but using separate examination rooms for the clinic nurse, the SPRINT nurse (the nurse was actually the coordinator for the SPRINT study), and the clinic physician. To avoid sequence bias, the sequence of BP measurements was randomly assigned: Thus, some patients had clinic nurse measurements first, some SPRINT measurements first, and some clinic physician measurements first. For power calculations, using a t test, it was estimated that a sample size of 63 patients was needed in order to have a 90% power to detect a difference of 10 mm Hg in mean systolic BP values assessed by paired t test assuming that the common SD was 20 mm Hg with an α‐significance level of 0.01.
The following blood pressure measurements were taken in all patients:
Clinic nurse BP: Patient was seated in a quiet examination room as above, and the clinic nurse applied the correct size BP cuff. Patient rested for 1‐3 minutes before BP measurements and could talk to the nurse during the waiting period. The nurse remained in the examination room with the patient, but did not speak during BP measurements. One to three BP measurements were taken. If the first BP was <140/90 mm Hg, it was recorded as the clinic nurse BP, if it was elevated, three BPs were taken and averaged as clinic BP value.
Physician automated and auscultatory BP: Patients entered the examination room and were seated for 1‐3 minutes. The clinic physician interviewed the patients during the waiting period and measured auscultatory BPs first and automated BP (Dinamap) later, in triplicate. The clinic physician was not aware of BP measurements taken by the clinic nurse or the SPRINT nurse.
-
Automated office BP measurements: SPRINT measurements:
Unattended: The patient was seated in a comfortable chair in a separate examination room, and the SPRINT nurse applied the appropriate size cuff, pressed the button, and left the examination room. The Omron device was programmed to wait for 5 minutes before starting to measure BPs, then measured three BPs one minute apart, and calculated the average.
Attended: This procedure was added in a subgroup of patients in addition to unattended SPRINT measurement. In this case, the nurse remained in the examination room, but did not speak to the patient during BP measurements although could speak to the patient during the waiting period. Attended and unattended measurements alternated in sequence.
Home BP measurement: This was taken in a subgroup of study patients enrolled in telehealth. These patients have been instructed to monitor daily BPs at home using a provided, validated, and calibrated monitoring device. BPs were transmitted electronically to patient's charts. We averaged BPs from the last two weeks prior to patients’ clinic visit.
Demographic data were collected at the beginning of the visit and from chart review after the patient signed the informed consent.
2.1. Statistical analysis
The baseline characteristics of participants were summarized using descriptive statistics. Data are presented as mean ± SD. All BP measurements were compared to unattended SPRINT BP using a paired 2‐sided Student t test. Blood pressure values of the four measurement techniques were compared by 1‐way ANOVA with Tukey's post hoc analysis and by the paired 2‐sided Student t test. Pearson's correlation analyses were performed to assess the strength and direction of the linear relationship between values obtained by various methods of BP measurement, and the goodness of fit of regression lines was assessed by the R 2 coefficient. P < 0.05 was regarded as statistically significant.
3. RESULTS
Sixty‐five patients, mostly male (93%), 57% black, were recruited for the purpose of this study. All patients were followed in the resistant or difficult to control hypertension clinic, and all of them were on antihypertensive medication (av 3.0 ± 1.1). Patients were at high cardiovascular risk with high rates of the usual comorbidities (Table 1). The average age of the group was 68 ± 12 years, 49% were with diabetes, 34% with mild CKD (CKD 1‐3, average eGFR 55.0 ± 13 mL/min/1.73 m2), and 20% with history of stable coronary artery disease. Most of the patients were overweight (43%) or obese (35%) with an average BMI of 30.4 ± 6.0 kg/m2. Table 2 shows the heart rate and BP values. Heart rate averaged 68.05 ± 12.4 BPM during the clinic nurse BP measurement and remained pretty much at the same range during the other BP measurements. All BP measurements were similar with no statistically significant difference (one‐way ANOVA, P = 0.621). Compared to unattended SPRINT BP values (139.77 ± 19.22/75.42 ± 11.72 mm Hg), the clinic BP measurements were numerically slightly higher but with a NS P value (P = 0.163). Similarly, BP values taken by the clinic physician, either by an automated device or manually (by auscultation), were similar to unattended SPRINT BP measurements (Table 2). Figure presents systolic and diastolic BPs of all four groups. In a smaller cohort of 11 patients, we compared unobserved vs observed SPRINT‐like BP measurements, and in 13 patients, we compared unobserved SPRINT‐like BP measurements to average home BP measurements. There were no significant differences between any of these subgroups (one‐way ANOVA, P = 0.816 for systolic and P = 0.803 for diastolic; Table 3).
Table 1.
Patient demographics
| N | 65 |
| Age | 68 ± 12 |
| Male sex | 93% |
| Black | 57% |
| Current smokers | 4.6% |
| Body mass index | 30.4% |
| Body mass index 25−29 | 43% |
| Body mass index ≥30 | 35% |
| Coronary artery disease | 20% |
| Diabetes mellitus | 49% |
| Obstructive sleep apnea | 17% |
| Chronic kidney disease | 34% |
| Peripheral vascular disease | 12% |
| Heart failure | 9% |
| Sodium | 139 ± 3.4 |
| Potassium | 4.15 ± 0.56 |
| Fasting blood glucose | 146 ± 81 |
| HgA1c | 8.09 ± 2.15 |
| LDL‐cholesterol | 108 ± 39 |
| HDL‐cholesterol | 48 ± 14 |
| Serum creatinine | 1.29 ± 0.74 |
| Estimated glomerular filtration rate | 55 ± 13 |
| Number of antihypertensive medication | 3.0 ± 1.11 |
Table 2.
Mean and SD of various BP measurements
| Heart rate (clinic nurse) | 68.05 ± 12.4 | |
| Systolic BP | P value | |
| Unobserved SPRINT | 139.77 ± 19.22 | — |
| Clinic nurse BP | 144.23 ± 16.97 | 0.163 |
| Clinic physician automated | 143.05 ± 19.53 | 0.336 |
| Clinic physician auscultatory | 140.49 ± 78.14 | 0.816 |
| Diastolic BP | ||
| Unobserved SPRINT | 75.42 ± 11.72 | — |
| Clinic nurse BP | 77.94 ± 10.73 | 0.248 |
| Clinic physician automated | 76.97 ± 11.70 | 0.492 |
| Clinic physician auscultatory | 78.14 ± 11.17 | 0.221 |
Compared to unobserved SPRINT measurements, all other values were similar. None of the P values was statistically significant.
Table 3.
Comparison of SPRINT nurse absent BP measurements with nurse present (N = 11) and average 2 week home BP measurements
| Heart rate | 70.69 ± 15.02 | |
| Systolic BP | P value | |
| SPRINT nurse absent | 140.73 ± 29.65 | — |
| SPRINT nurse present | 143.64 ± 28.31 | 0.816 |
| Diastolic BP | ||
| SPRINT nurse absent | 78.00 ± 15.78 | — |
| SPRINT nurse present | 79.36 | 0.803 |
| systolic BP | ||
| SPRINT nurse absent | 142.15 ± 17.48 | |
| Av home BP | 138 ± 12.82 | 0.553 |
| Diastolic BP | ||
| SPRINT nurse absent | 75.77 ± 16.21 | — |
| Av home BP | 73.69 ± 8.08 | 0.683 |
None of the comparisons resulted in significant differences (N = 13).
Figure 1.
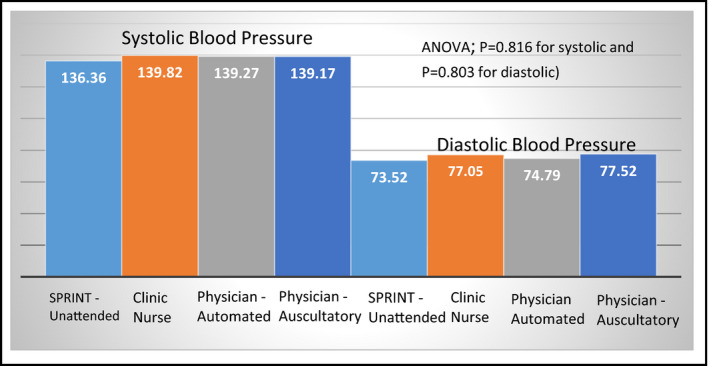
The figure presents systolic and diastolic BPs for all methods used. There was no statistically significant difference between any of the groups
Figure 3 presents correlations and correlation coefficients of unattended SPRINT measurements with all other 3 methods. There was considerable variability, but correlation was close.
Figure 2.
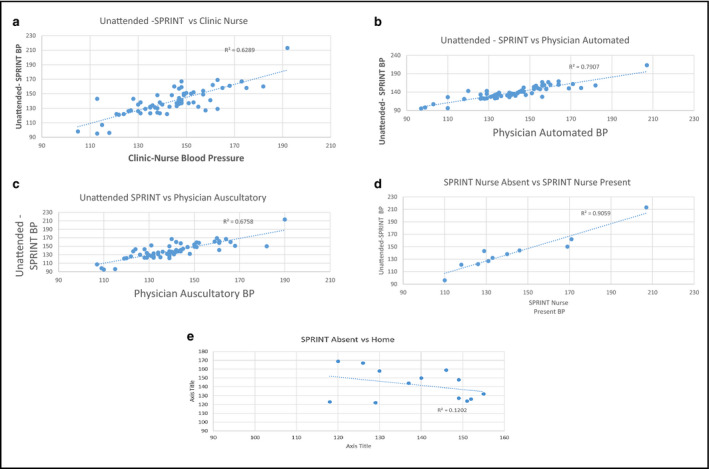
A‐E, The figure shows correlations between the unattended SPRINT‐like BP measurements and BPs taken by 4 other methods. There was a close correlation between all BP measurement methods
4. DISCUSSION
This was a small but carefully done study aiming primarily to compare the unattended automated BP measurement—as done in the SPRINT study—to the usual or conventional clinic BP measurement and other commonly used methods. In order to avoid environmental biases, we chose to conduct the study in the usual clinic environment, using the same personnel and devices used for clinical purposes. Thus, we used the clinic nurse and physician and the same manometers used in clinical practice. We also used the OMRON (SPRINT) device and the SPRINT nurse‐coordinator to take the SPRINT measurements (attended or unattended), in the same clinic environment using a separate dedicated examination room. In order to avoid timing bias, the sequence of BP measurements was randomly assigned and all BP measurements were taken during the same visit in close proximity. For all BP measurements, we followed the standard guidance for resting period and patient positioning. All BP measurements were taken with automated, validated devices, except for the manual/auscultatory measurement taken by the clinic physician. Our data indicate that unattended SPRINT‐like BP measurements are similar to all other BP measurements measured in clinic or even out of office. The BP measurement taken by the clinic nurse used an automated oscillometric device (Dinamap), which has been used in our institution and nationwide for over 15 years. All devices are regularly serviced and calibrated by trained engineers. All BP measurements taken by clinic nurses are entered into the electronic medical records (CPRS) and eventually into the national database (VINCI). Using these pressures, we have shown BP control rates over 75% and explored the importance of consistently lower BPs16, 17 in more than 600 000 patients from 15 VA hospitals. We also presented (but not yet published, manuscript in preparation) mortality results from over 7 million people.18
Similar results, to unattended SPRINT measurements, were obtained by the clinic physician, using the same automated device (Dinamap) or by the auscultatory method. It has been hypothesized that the white coat effect may be different when the patient is phasing a nurse versus a physician. In our study, it does not seem that was the case. Similar BPs were obtained with the nurse present, with the nurse absent, with the physician using an automated device, and with the physician taking BP manually. Automated devices have been used for BP measurements for a long time and have been adopted in many clinical, outcome trials.19, 20, 21, 22 In fact, most trials also adopted techniques that mandated a waiting period of 3‐5 minutes and BP measurements in triplicate.19, 20, 21, 22, 23, 24 It is not known how closely these requirements were followed in various studies, through the years (physicians do not like to wait). For this reason and for consistency and homogeneity, the SPRINT study incorporated a 5‐minute waiting period and encouraged the nurses to refrain from talking to the patients after the device was activated and even be outside the examination room. The unattended BP measurement following a 5‐minute waiting period was thought to have eliminated the white coat effect. In our study population, the white coat effect does not appear to have been a problem. In fact in a smaller sample, we found no difference between attended and unattended BP measurements (SPRINT way) or between clinic and average home BP measurement.
Following the publication of SPRINT results, a flurry of publications appeared in the literature disputing the results and questioning the accuracy or relevance of BP measurements implemented in SPRINT.9, 25, 26
The main argument was that unattended BP measurements were much lower than the usual—conventional—BP measurements and thus inconsistent with clinical practice or outcome trials. In fact, known authorities in hypertension made the argument that the final BP values of the SPRINT study should have been approximately 135 vs 155 mm Hg (instead of 121 vs 136 mm Hg).14 This argument, however, is based on assumptions and not actual data. The (ugly) results of our study disprove their (beautiful) hypothesis.
One other study that appeared recently in the literature found similar results to ours. Bauer et al27 compared unattended automated office BP to office auscultatory, home, and ambulatory BP. Unattended office BP, office auscultatory, and ambulatory BP were similar, but home BP measurements were slightly lower. The authors concluded that unattended and attended office BP measurements are comparable when measurements take place at a familiar general practitioner's office. In another recently published study,28 in 146 patients, we also found that there was no difference between attended and unattended AOBPs and both were similar to daytime ambulatory BP measurements.
Admittedly, all patients included in the current study were established and were seen in a familiar clinic environment. Furthermore, patients were at high cardiovascular risk, with resistant hypertension, treated with multiple drugs. Thus, results may be different for younger or lower risk patients or newcomers who are more likely to express white coat effect.
In summary, we conclude that automated office blood pressure measurements taken after a 5‐minute waiting period, with the patient correctly seated and with the nurse out of the examination room, are similar to other carefully taken, conventional clinic measurements such as those taken by the clinic nurse, or measured by the clinic physician, using an automated device or an auscultatory method. These findings suggest that automated BP measurements in SPRINT, attended or unattended, are similar to carefully taken routine clinic BP measurements.
CONFLICT OF INTEREST
None of the authors has conflict of interest related to this Review Paper.
Papademetriou V, Tsioufis C, Chung A, Geladari C, Andreadis EA. Unobserved automated office BP is similar to other clinic BP measurements: A prospective randomized study. J Clin Hypertens. 2018;20:1411–1416. 10.1111/jch.13371
REFERENCES
- 1. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903‐1913. [DOI] [PubMed] [Google Scholar]
- 2. Rapsomaniki E, Timmis A, George J, et al. pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life‐years lost, and age‐specific associations in 1.25 million people. Lancet. 2014;383:1899‐1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nadar SK, Tayebjee MH, Messerli F, Lip GY. Target organ damage in hypertension: pathophysiology and implications for drug therapy. Curr Pharm Des. 2006;12(13):1581. [DOI] [PubMed] [Google Scholar]
- 4. Rutan GH, Kuller LH, Neaton JD, Wentworth DN, McDonald RH, Smith WM. Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the Multiple Risk Factor Intervention Trial. Circulation. 1988;77:504‐514. [DOI] [PubMed] [Google Scholar]
- 5. Moser M, Roccella EJ. The treatment of hypertension: a remarkable success story. J Clin Hypertens (Greenwich). 2013;15:88‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smirk FH. Casual and basal blood pressures, IV. Their relationship to the supplemental pressure with a note on statistical implications. Br Heart J. 1944;6:176‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension. 2017;2018(71):1‐283. [Google Scholar]
- 8. Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kjeldsen SE, Lund‐Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67:808‐812. [DOI] [PubMed] [Google Scholar]
- 10. Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension. 2010;55:195‐200. [DOI] [PubMed] [Google Scholar]
- 11. Kjeldsen SE, Mancia G. Unobserved automated office blood pressure measurement in the Systolic Blood Pressure Intervention Trial (SPRINT): systolic blood pressure treatment target remains below 140 mmHg. Eur Heart J Cardiovas Pharmacother. 2016;2:79‐80. [DOI] [PubMed] [Google Scholar]
- 12. Filipovský J, Seidlerová J, Kratochvíl Z, Karnosová P, Hronová M, Mayer O. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 2016;25(4):228‐234. [DOI] [PubMed] [Google Scholar]
- 13. Lu¨scher T. From,. ‘essential’ hypertension to intensive blood pressure lowering: the pros and cons of lower target values. Eur Heart J. 2017;38(44):3258‐3271. [DOI] [PubMed] [Google Scholar]
- 14. Kjeldsen SE, Mancia G. A critical review of the systolic blood pressure intervention trial (SPRINT). Eur Heart J. 2017;00:3‐8. [Google Scholar]
- 15. Papademetriou V. SPRINT is a landmark trial: results should be adopted in clinical practice. Eur Heart J. 2017;00:8‐14. [Google Scholar]
- 16. Fletcher RD, Amdur RL, Kolodner R, et al. Blood pressure control among US veterans: a large multiyear analysis of blood pressure data from the veterans administration health data repository. Circulation. 2012;125(20):2462‐2468. [DOI] [PubMed] [Google Scholar]
- 17. Doumas M, Tsioufis C, Fletcher R, Amdur R, Faselis C, Papademetriou V. Time in therapeutic range, as a determinant of all‐cause mortality in patients with hypertension. J Am Heart Assoc. 2017;3;6(11):e007131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fletcher R, Kheirbek R, Amdur R, Jones R, Faselis C, Papademetriou V. Effect of blood pressure control on mortality in patients with hypertension using a national data base. AHA meeting Nov 15–20th Dallas Tx Circulation. 2013, Ab# 19229.
- 19. Mancia G, Parati G, Bilo G, et al. Ambulatory blood pressure values in the ongoing telmisartan alone and in combination with ramipril global endpoint trial (ONTARGET). Hypertension. 2012;60:1400‐1406. [DOI] [PubMed] [Google Scholar]
- 20. Dolan E, Stanton AV, Thom S, et al. Ambulatory blood pressure monitoring predicts cardiovascular events in treated hypertensive patients–an Anglo‐Scandinavian cardiac outcomes trial substudy. J Hypertens. 2009;27:876‐885. [DOI] [PubMed] [Google Scholar]
- 21. Mancia G, Omboni S, Parati G, et al. Twenty‐four hour ambulatory blood pressure in the hypertension optimal treatment (HOT) study. J Hypertens. 2001;19:1755‐1763. [DOI] [PubMed] [Google Scholar]
- 22. ThijsL AA, Clement D, Cox J, et al. Ambulatory blood pressure monitoring in elderly patients with isolated systolic hypertension. J Hypertens. 1992;10:693‐699. [PubMed] [Google Scholar]
- 23. Siragy HM. Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). Curr Hypertens Rep. 2003;5(4):293‐294. [DOI] [PubMed] [Google Scholar]
- 24. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288(23):2981–2997. [DOI] [PubMed] [Google Scholar]
- 25. Mancia G, Kjeldsen SE. Adopting systolic pressure intervention trial (SPRINT)‐like office blood pressure measurements in clinical practice. J Hypertens. 2017;35(3):471–472. [DOI] [PubMed] [Google Scholar]
- 26. Kjeldsen SE, Mancia G. Unobserved automated office blood pressure measurement in the systolic blood pressure intervention trial (SPRINT): systolic blood pressure treatment target remains below 140 mmHg. Eur Heart J Cardiovasc Pharmacother. 2016;2:79–80. [DOI] [PubMed] [Google Scholar]
- 27. Bauer F, Seibert FS, Rohn B, et al. Attended versus unattended blood pressure measurement in a real life setting. Hypertension. 2018;71:243–249. [DOI] [PubMed] [Google Scholar]
- 28. Andreadis EA, Geladari CV, Angelopoulos ET, Savva FS, Georgantoni AI. Papademetriou V. Attended and unattended automated office blood pressure measurements have better agreement with ambulatory monitoring than conventional office readings. J Am Heart Assoc. 2018;7(8);e008994. [DOI] [PMC free article] [PubMed] [Google Scholar]


