Abstract
This review aims to identify, summarize, and appraise studies reporting on the implementation of salt reduction interventions that were published between March and August 2016. Overall, 40 studies were included: four studies evaluated the impact of salt reduction interventions, while 36 studies were identified as relevant to the design, assessment, and implementation of salt reduction strategies. Detailed appraisal and commentary were undertaken on the four studies that measured the impact of the interventions. Among them, different evaluation approaches were adopted; however, all demonstrated positive health outcomes relating to dietary salt reduction. Three of the four studies measured sodium in breads and provided consistent evidence that sodium reduction in breads is feasible and different intervention options are available. None of the studies were conducted in low‐ or lower middle–income countries, which stresses the need for more resources and research support for the implementation of salt reduction interventions in these countries.
Keywords: salt, salt reduction, sodium
1. Introduction
High salt intake is one of the main contributors to premature death from cardiovascular diseases globally.1 In view of this, all World Health Organization (WHO) Member States have committed to reduce salt consumption by 30% by 2025 as part of a number of targets to reduce noncommunicable diseases.2 WHO recently published the SHAKE Package for Salt Reduction, a set of evidence‐based practices, policies, and interventions from different settings around the world, envisioned to guide Member States to achieve a reduction in population salt consumption.3 Globally, countries are encouraged to implement the strategies through five key action areas: Surveillance, Harnessing industry, Adopting standards for labeling, Knowledge, and Environment—with a view to translating them into effective public policies. A recent Cochrane systematic review on national population‐level sodium reduction initiatives showed that a number of countries (China, Finland, France, England, and Ireland) had already achieved significant reductions in population salt intake.4 Although encouraging, two other countries showed an increase in salt intake while others demonstrated no change in sodium intake over the period.4 For other countries it was not possible to assess the impact of the interventions because of lack of evaluation (eg, no pre‐ or post‐data point with which to examine the impact of the intervention/s). This demonstrates the need for ongoing evaluation of national sodium reduction strategies and improving the monitoring of impact of programs internationally.
With the goal of keeping clinicians and policy stakeholders informed of the growing body of research related to dietary salt, alternating narrative summaries on the effects of salt on health and the impact of population‐wide salt reduction interventions are being published in the Journal of Clinical Hypertension. Building on previous reviews since June 2015, this series aims to evaluate the studies based on a set of established quality criteria to provide a more objective interpretation of study conclusions.5 The current review aims to critically appraise the studies related to implementation of salt reduction interventions published from March to August 2016.
2. Methodology
A detailed description of the search strategy used to identify and screen studies in this review has been previously reported.5 Briefly, articles related to dietary salt reduction in populations were identified weekly through a standardized MEDLINE literature search and their summaries were published in the Science of Salt Weekly newsletter. Studies published from March 2016 to August 2016 were screened for eligibility using the previously established inclusion and exclusion criteria.6
In the current review, studies evaluating the impact of salt reduction interventions were appraised for risk of bias by two independent reviewers using a modified Cochrane risk of bias tool for nonrandomized trials of intervention studies.4, 7 Detailed appraisal and commentary were also performed on these studies. Other types of studies that provided information pertinent to the design, implementation, and assessment of salt reduction interventions were summarized in a table. These include (1) studies on monitoring and surveillance of salt intake; (2) salt content in foods; (3) consumers’ knowledge, attitudes, and behaviors toward salt; (4) economic evaluation or modeling studies of salt reduction strategies; and (5) other studies related to implementation of salt reduction initiatives.
3. Results
The MEDLINE search identified 3675 citations, of which 85 were considered potentially eligible for full review on the basis of their findings relevant to salt reduction interventions. Ultimately, a total of 40 studies met the inclusion criteria: four studies evaluated the impact of salt reduction interventions, 21 were surveillance or monitoring studies, five were modeling studies relating to salt reduction, and 10 other studies related to the implementation of salt reduction interventions (Figure 1).
Figure 1.
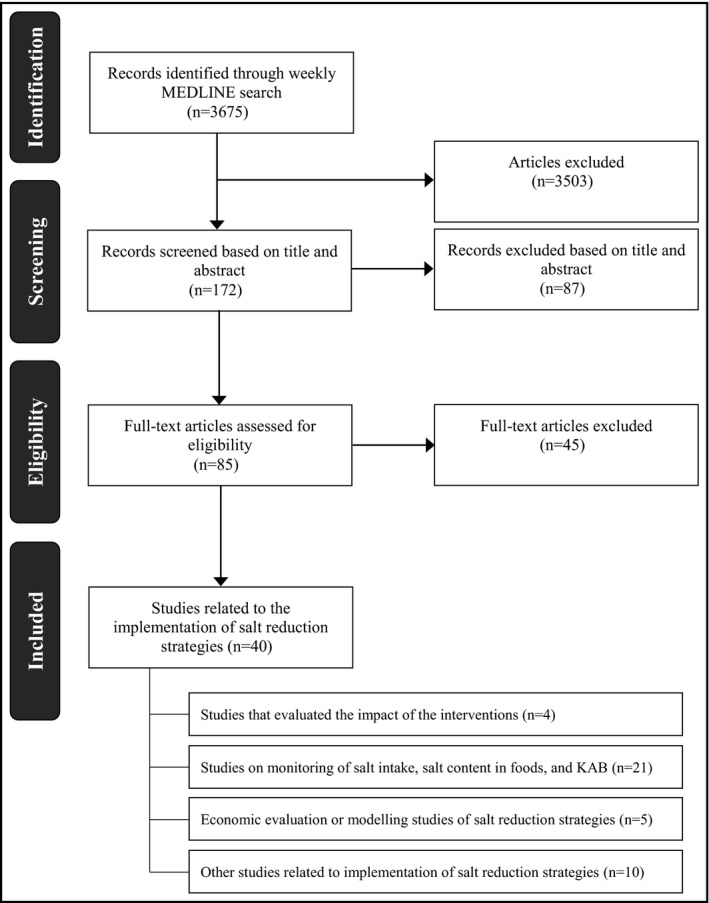
Studies included in the current review: March to August 2016. KAB indicates knowledge, attitudes, and behaviors
The studies that evaluated the impact of salt reduction interventions were selected for detailed appraisal and commentary. Risk of bias assessments for the four studies are included in Appendix S1. The studies were conducted in Australia,8 Canada,9 Spain10 (high‐income countries), and Iran11 (an upper middle–income country); none were conducted in low‐ or lower middle–income countries. Two studies measured the effects of a multicomponent intervention (ie, advocacy, community mobilization, awareness campaigns, and salt substitution in Australia, and awareness campaigns and food reformulation in Iran) conducted at a community level,8, 11 one assessed the impact of salt substitution in breads employed at a community level,10 and one evaluated the changes in sodium levels in foods achieved through voluntary sodium reduction targets implemented at a national level.9
The method for evaluating the impact of the interventions varied across the four studies. The Australian study was based on change in mean salt intake measured using 24‐hour urine samples; the Iranian study was also based on change in mean salt intake but used spot urine samples; the Spanish study compared the sales data of breads before and after the intervention; and the Canadian study determined the change in sodium content of packaged food using a Nutrition Facts table. Despite the use of different evaluation methods, all studies scored low risk for detection bias, a domain that scores the validity of outcome assessment, as all of the approaches for assessing the impact of the interventions were deemed suitable for the purpose of the different studies (Figure 2). However, all studies scored unclear or high risk in one or more bias domains. All except one study scored low risk for selection bias (sampling), while three studies scored high risk for performance bias (adjustment for confounders or exposure to other factors).
Figure 2.
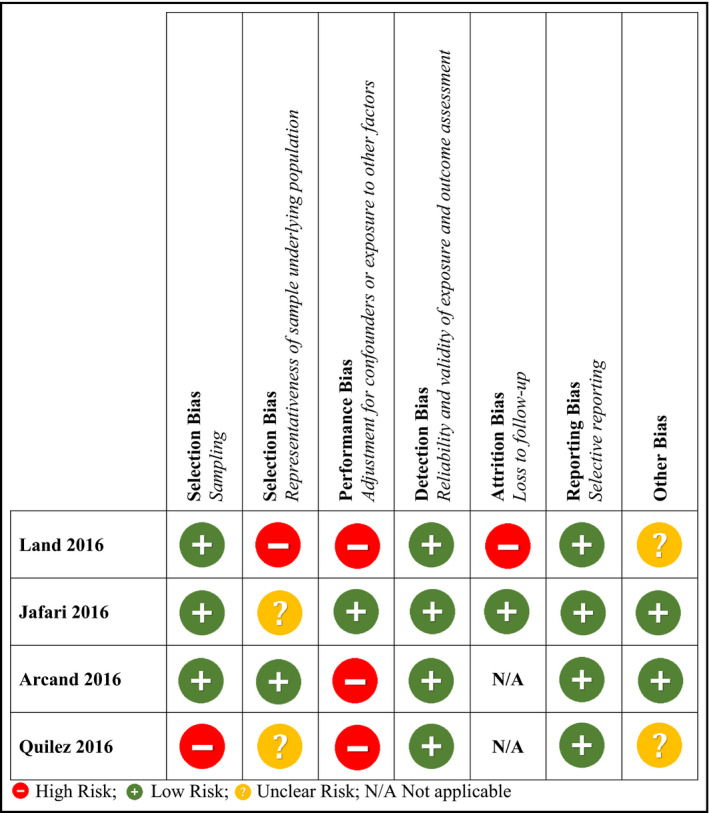
Risk of bias assessment of included intervention studies
All studies found some positive outcomes related to dietary salt reduction. The two studies that implemented multicomponent interventions showed a statistically significant reduction in salt intake. The study that substituted salt in breads demonstrated that the sales of normal‐salt and reduced‐salt breads were comparable, and the study on voluntary sodium reduction targets showed that a number of food categories had significant decreases in sodium, although most food categories did not show change.
Further details of the other 36 studies are outlined in the Table. Two thirds (24) of these studies were conducted in high‐income countries, a quarter (nine) in middle‐income countries (seven in upper middle–income and two in lower middle–income countries), and one in a low‐income country. Two further studies were systematic reviews conducted on a regional (sub‐Saharan Africa)12 or global scale.13 Of the 21 surveillance studies, 11 measured population salt intake, three measured salt levels in foods, and seven measured consumers’ knowledge, attitudes, and behavior regarding salt. For studies that measured population salt intake, the most common method of assessment was 24‐hour urine collection (five) and 24‐hour dietary recall (five). Of the 10 other studies related to the implementation of salt reduction interventions, three were on acceptability of low‐sodium foods, five were on validity of tools or methods for measuring salt intake, and two were systematic reviews related to salt consumption.
Table 1.
Summary for other implementation studies
| A. Monitoring or surveillance studies: population salt intake (n=11) | |||||
|---|---|---|---|---|---|
| Study | Country | Study Design | Study Population | Method of Assessment | Results |
| Goncalves15 | Portugal | Cross‐sectional study | Adolescents aged 13–18 y (n=200) | One 24‐h urine collection | Mean urinary sodium excretion was 3725 mg/d and 3062 mg/d in boys and girls, respectively, with only 9.8% of boys and 22% of girls meeting the WHO recommendations for sodium intake. |
| An16 | United States | Secondary analysis of NHANES cross‐sectional data | Adults aged 18 y and older (n=11 646) | Two 24‐h dietary recalls | Weekend diet was associated with an increase in daily intake of sodium by 205.59 mg and increase in the prevalence of fast‐food (10.21%) and full‐service restaurant consumption (17.79%). |
| Jackson17 | United States | Secondary analysis of NHANES cross‐sectional data | Individuals aged 2 y and older (n=14 728) | Two 24‐h dietary recalls | Eighty‐nine percent of adults (≥19 y) and >90% of children (2–18 y) exceeded age‐specific recommendations for sodium intake. |
| Land8 | Samoa | Cross‐sectional study | Women aged 18–45 y (n=152) | One 24‐h urine collection | Mean 24‐h salt excretion among women was 6.6 g/d (SD: 3.2 g/d), with more than two thirds of the women exceeding the WHO‐recommended daily maximum level. |
| Okuda18 | Japan | Cross‐sectional study | Secondary school adolescents aged 12–15 y (n=68) | Two 24‐h urine collections and three overnight urine collections | Estimated salt intake was 10.6 g/d (SD: 1.2 g/d) for boys and 10.0 g/d (SD: 2.4 g/d) for girls. Sodium excretion was associated with physical activity but not body weight. |
| Service19 | Australia | Cross‐sectional study | Primary school children (n=168) and their parents (n=148) | One 24‐h urine collection and dietary habits questionnaire | A 1 g/d increase in mother's salt intake was associated with a 0.2 g/d increase in child's salt intake, after adjusting for parental age, child age, and sex. There was no association between father's salt intake and child's salt intake. Sixty‐seven percent of parents added salt during cooking while 37% of children added salt at the table. |
| Sobiecki20 | United Kingdom | Secondary analysis of cross‐sectional data from EPIC‐Oxford cohort study | Adults aged 30–90 y (n=30 251) | One semi‐quantitative food frequency questionnaire, which had no measure of table salt use | There was no statistically significant (P>.05) difference in mean sodium intake between the four dietary groups (meat eaters, fish eaters, vegetarians, and vegans). The means from all groups exceeded the recommended daily sodium intake of 2400 mg/d and ranged from 2624 to 2701 mg/d. |
| Rehm21 | United States | Secondary analysis of repeated cross‐sectional data from NHANES | Adults aged 20 y and older (n=33 932) | One or two 24‐h dietary recalls | No significant change was demonstrated for sodium intake over the period 1999–2012, with estimated mean sodium intakes ranging from 3355 mg/d in 2001–2002 to 3557 mg/d in 2006–2006. |
| O'Halloran22 | Australia | Secondary analysis of data from the Melbourne InFANT program | Preschool children aged ≈3.5 y (n=251) | Three 24‐h dietary recalls | Mean daily sodium intake was 1565 mg/d in boys and 1452 mg/d in girls, and was significantly higher among those with adequate intake of potassium. The major sources of sodium were milk products, cereal products, and meat products. |
| Wang23 | China | Secondary analysis of cross‐sectional data from CRHI‐SRS | Adults aged 20 y and older (n=1903) | Survey and one 24‐h urine collection | The effect of the salt reduction intervention (in terms of salt intake, potassium intake, sodium to potassium ratio, and KAB) did not vary across different levels of education. Among all educational groups, salt intake was lower in the intervention than in the control group. |
| Kang24 | Korea | Secondary analysis of cross‐sectional data from KNHANES IV and V | Adults older than 30 y with (n=12 477) and without diabetes (n=1480) | One 24‐h dietary recall | Healthy individuals had higher mean sodium intake than diabetics (5188.2 mg/d vs 4910.2 mg/d, P>.1). Among diabetics, those who were newly diagnosed had higher sodium intake than those who were formerly diagnosed (P>.1). All groups consumed more than the recommended sodium intake per day. |
| B. Monitoring or surveillance studies: salt content in foods and meals (n=3) | |||||
|---|---|---|---|---|---|
| Study | Country | Study Design | Type of Foods Assessed | Source of Sodium Information | Results |
| Kraemer25 | Brazil | Cross‐sectional study | Processed snack foods consumed by children and adolescents (n=2945) | Nutrition information panel | Twenty‐one percent of processed foods had high levels of sodium (>600 mg/100 g) while 35% had medium sodium levels (>120 and ≤600 mg/100 g). |
| Prentice26 | New Zealand | Cross‐sectional study | Savoury fast foods from chain restaurants (n=471) and independent outlets (n=52) | Nutrition information from company Web sites and food analysis for foods sourced from independent outlets | The majority of fast foods exceeded the UK Food Standards Agency 2012 sodium targets. Sauces, salad dressings, and fried chicken had the highest sodium content from chain restaurants, while from independent outlets, sausage rolls, battered hotdogs, and mince and cheese pies had the highest. |
| John27 | United States | Cross‐sectional study | Regular foods (savoury snacks, cheese, salad dressings, soups) and their lower‐calorie or lower‐fat food counterparts (n=283 matches) | Nutrient information from manufacturers’ Web sites | Changes in sodium content from calorie and fat modification varied by food category. Mean sodium content of modified soups was significantly lower compared with regular soups. Modified salad dressings and cheeses had slightly higher mean sodium content, while modified savoury snacks had similar mean sodium content as regular versions. |
| C. Monitoring or surveillance studies: consumer's KABs related to salt (n=7) | |||||
|---|---|---|---|---|---|
| Study | Country | Study Design | Study Population | Method of KAB Assessment | Results |
| Rasheed28 | Bangladesh | Cross‐sectional mixed method study | Adults aged 18 y and older (n=400 for the quantitative survey) | Focus group discussion, key informant interview, and survey | Participants had low awareness of the risks associated with excess salt consumption, and many reported that salt was beneficial to health. Salt reduction strategies were not a priority for participants. |
|
John29 |
United States | Secondary analysis of cross‐sectional data from Porter Novelli's ConsumerStyles online database | Adults aged 18 y and older (n=6378) | Online survey | Sixty‐eight percent of the respondents agreed that it is important for baby or toddler foods to be low in sodium. Adjusted analysis showed that agreement was most strongly associated with being a parent of a child <2 y, thinking sodium was harmful, and watching or reducing own sodium intake. |
| Regan30 | Ireland | Cross‐sectional study | Adults aged 18 and older (n=501) | Online survey | The majority of respondents supported 11 of 13 government‐led salt reduction policies (both voluntary and regulated, including education, labeling, and salt restriction in foods). Fewer participants supported subsidizing low‐salt foods and taxing high‐salt foods. |
| Lee31 | South Korea | Cross‐sectional study | Food service personnel at worksite cafeterias (n=104) | Survey | Most of the participants regarded sodium reduction as very or moderately important. The biggest barriers to providing sodium‐reduced meals were use of processed foods and limited methods of sodium‐reduced cooking in worksite cafeterias. |
| Sugimoto32 | Japan | Cross‐sectional study | Female dietitians (n=99) and nondietitians (n=117) aged 20–69 y at welfare facilities | Survey, two 24‐h urine collections, and 4‐d semi‐weighted diet records | Nutritional knowledge and dietary behavior were moderately associated with sodium to potassium ratio, but not with either sodium or potassium excretion. |
| Quader33 | United States | Secondary analysis of repeated cross‐sectional data from NHANES | Individuals aged 2 y and older (n=38 896) | Dietary habits questionnaire for participants and/or proxy (for children) | Use of salt “very often” at the table and during home cooking both declined from 18% to 12% and from 42% to 37%, respectively, between 2003 and 2012. There was no change in the proportion of the population who never used discretionary salt. Discretionary salt use differed by age, race or ethnicity, body mass index, self‐reported diabetes status, and income. |
| Asakura34 | Japan | Cross‐sectional study | Adults aged 20–69 y (n=392) | Four semi‐weighted diet records and two 24‐h urine collections | The proportion of sodium from discretionary sources was more than 50% in both sexes and was found to be lower in younger patients. The major contributors to sodium intake differed by age, but the top contributors were similar for both sexes (seasonings such as salt, and fish and shellfish). |
| D. Economic evaluations or modeling studies: effects of salt reduction (n=5) | ||||
|---|---|---|---|---|
| Study | Country | Intervention | Outcome Measure | Results |
| Wilson35 | New Zealand | Achievement of full and component food category sodium reduction targets (total of 10 targets) | Health gains measured by QALY and cost‐savings | Achieving the full target (overall 35% reduction in dietary salt intake through the mandatory approach) would have the largest health gain (235 000 QALYs) and the greatest cost‐savings (NZD 1260 million). For specific target components, the range of health gain was from 122 000 to 6100 QALYs. All 10 target interventions were cost‐saving. |
| Souza36 | Brazil | Reduction of sodium content in processed foods based on voluntary agreements between the government and food industry | Average salt intake | Sodium reduction targets in processed foods based on voluntary agreements would have a small impact on mean salt intake of the Brazilian population. The estimated mean sodium intake reduction 5 y after the agreement was 1.5%. |
| van Buren37 | Netherlands | Reformulation: replacing sodium chloride with potassium chloride (total of three reformulation scenarios) | Dietary impact and potassium intake | 20%, 50%, and 100% replacement scenarios would lead to an increase in the median intake of potassium by 453 mg/d, 674 mg/d, and 733 mg/d, respectively, which would result in better compliance to potassium intake guidelines. Reformulation would have the largest impact on bread, processed fruits and vegetables, snacks, and processed meat. |
| Watkins38 | South Africa | Salt reduction policy: reducing salt consumption to the target of 5 g/d | Health impacts measured by reductions in cardiovascular disease, and economic impacts | Reducing salt consumption to the target of 5 g/d could reduce the burden of cardiovascular disease by 11%, could save households $4.06 million in out‐of‐pocket expenditures, and save the government $51.25 million in healthcare subsidies yearly. |
| Nghiem39 | New Zealand | Salt substitution and setting maximum levels of sodium in breads (total of four interventions) | Health gains measured by QALYs and cost‐savings | The intervention where most (59%) of the sodium in processed foods was replaced by potassium and magnesium salts had the largest health gain (294 000 QALYs) and the highest net cost‐savings (NZD 1.5 billion). All interventions resulted in relatively larger per capita QALYs for men than women and for the indigenous Maori population than non‐Maori. |
| E. Other studies related to salt reduction interventions (n=10) | ||||
|---|---|---|---|---|
| Study | Country | Type of Study | Subject | Results |
| Jezewska‐Zychowicz40 | Poland | Acceptability of low‐sodium foods–survey of adult consumers | Bread | Self‐reported willingness to consume breads produced without preservatives or raising agents was higher than reduced‐salt breads. Women, people older than 55 y, and people who often consume white breads were more willing to consume reduced‐salt breads, while those with a higher education, who were older than 45 y, and who rarely consume wholemeal bread were more willing to eat bread without preservatives or raising agents. |
| McMahon41 | Australia | Acceptability of low‐sodium foods–consumer taste test | Bread | The difference between standard and reduced‐salt breads was not detected by the participants. Further, there was no significant difference in overall liking between the two breads. |
| De Kock42 | South Africa | Acceptability of low‐sodium foods–consumer taste test | Chicken stew | The standard chicken stews and chicken stews prepared with reduced‐salt stock powders were equally well liked by the consumers; however, 19% of consumers added salt back at the table, with more salt being added with increased salt reduction in the meals, to the point of full compensation in some cases. |
| Peng43 | China | Validity of tools or assessment methods | Spot urine to estimate 24‐h urinary sodium excretion vs 24‐h urine collection | The Kawasaki, INTERSALT, and Tanaka methods underestimated the measured 24‐h urinary sodium excretion in the sample of Chinese adults. The Kawasaki method was least biased (mean bias –740 mg/d), followed by the Tanaka method (mean bias –2305 mg/d), and the INTERSALT method (mean bias –2797 mg/d). |
| Yasutake44 | Japan | Validity of tools or assessment methods | Overnight (8‐h) urine samples obtained using a self‐monitoring device vs 24‐h urine collection | There was a significant positive correlation between 24‐h urine salt and overnight urine salt; however, the coefficients of variation for the overnight urine were lower than those for the 24‐h urine, suggesting a narrow measurement range for the self‐monitoring device. |
| Mizehoun‐Adissoda45 | Benin | Validity of tools or assessment methods | Spot urine to estimate 24‐h urinary sodium excretion vs 24‐h urine collection | Mean sodium chloride and potassium chloride excretion from 24‐h urine were 10.2 g/d and 2.9 g/d, respectively, while the estimated values from spot urine were 10.7 g/d and 3.9 g/d, respectively. Spot urine is an acceptable method to assess sodium and potassium intake in black populations, but its high variation limits its application in clinical settings. |
| Ma46 | China | Validity of tools or assessment methods | Salt sales survey to estimate 24‐h urinary sodium excretion vs 24‐h urine collection | The results from the salt sales survey were consistent with the results from 24‐h urine and potassium data. The salt sales survey cost only 14% of the cost of the 24‐h urine method and had greater statistical power. |
| Sugimoto32 | Japan | Validity of tools or assessment methods | 24‐h urine collection vs 4‐d semi‐weighted diet record vs two validated diet history questionnaires | All dietary assessment methods underestimated salt intake measured from 24‐h urinary collection. Correlation coefficients between 24‐h urine collection and diet record were higher than the two validated diet history questionnaires for sodium, potassium, and protein. Compared with nondietitians, dietitians were more likely to underreport sodium and protein intake and overreport potassium intake. |
| Muthuri12 | Sub‐Saharan Africa | Systematic review related to salt intake | Effectiveness of salt reduction interventions | All interventions had at least one significantly improved outcome measure, including reduction in 24‐h urinary sodium excretion, systolic blood pressure, or mean arterial blood pressure. |
| Huang13 | Global | Systematic review related to salt intake | Spot urine to estimate 24‐h urinary sodium excretion vs 24‐h urine collection | The average population salt intake estimated from 24‐h urine samples and spot urine samples were 9.3 g/d and 9.0 g/d, respectively. Spot urine samples overestimated salt intake at lower levels of consumption and underestimated intake at higher levels of consumption. |
Abbreviations: CRHI‐SRS, China Rural Health Initiative–Sodium Reduction Study; EPIC, European Prospective Investigation into Cancer and Nutrition; InFANT, Infant Feeding Activity and Nutrition Trial; KAB, knowledge, attitudes, and behaviour; KNHANES, Korean National Health and Nutrition Examination Survey; NHANES, National Health and Nutrition Examination Survey; NZD, New Zealand dollar; QALY, quality‐adjusted life year; SD, standard deviation; WHO, World Health Organization.
Studies evaluating the impact of salt reduction interventions
Land MA, Wu JH, Selwyn A, et al. Effects of a community‐based salt reduction program in a regional Australian population. BMC Public Health. 2016;16:388.
Objective: To evaluate the effect of a multicomponent community‐based salt reduction intervention on mean salt intake and consumer knowledge, attitudes, and behaviors related to salt.
Design: Community intervention. The evaluation employed an uncontrolled pre‐post survey of residents.
Setting: The intervention was conducted in the regional town of Lithgow (population around 20 000) in New South Wales, Australia.
Participants: Residents of Lithgow aged 20 years or older: 419 participants were surveyed at baseline (306 were randomly selected from the electoral roll, and 113 volunteers were recruited from shopping centres) and 572 participants were surveyed at follow‐up (101 participants from the random baseline survey, 106 new participants randomly selected from the telephone directory, 36 volunteers from the baseline survey, and 329 new volunteers).
Intervention: The intervention, based on the Communication for Behavioural Impact framework, included public advocacy and communication with key stakeholders, community mobilization and advertising, interpersonal communication, and point‐of‐service contact using tools such as a salt substitute and a smartphone application (FoodSwitch) that enabled consumers to interpret food labels and identify low salt products.
Outcomes: Change in mean salt intake from baseline to follow‐up measured through 24‐hour urine collection; change in consumers’ knowledge, attitudes, and behaviors regarding salt.
Summary of results: Mean salt intake decreased from 8.8 g/d at baseline to 8.0 g/d at follow‐up. This difference was statistically significant (P<.001) in adjusted and unadjusted models. Significant changes were also demonstrated in participant knowledge and salt‐related behaviors over the study period.
Sources of funding: The study was funded by a National Health and Medical Research Council (NHMRC) of Australia partnership project.
Comments: This study demonstrated that the Salt Swap Lithgow intervention was associated with a significant reduction in mean population salt intake of around 10%, as well as increased awareness of the recommended upper limit of salt intake and the importance of salt reduction. It also reported positive changes in some behaviors related to reducing salt intake. The uncontrolled pre‐post study design meant that the authors were not able to account for the effect of other salt reduction initiatives that were implemented nationally (such as the former government's Food and Health Dialogue, a voluntary partnership between government, the food industry, and nongovernment organizations to improve the nutritional composition of the food supply14). Low response rates in the randomly selected population samples (16% and 5% at baseline and follow up, respectively) may limit the generalizability of the results; however, findings from the randomly selected participants and volunteers did not differ substantially. Sources of bias inherent to the study and study design were discussed appropriately by the authors. The authors followed the Transparent Reporting of Evaluations with Nonrandomized Design (TREND) reporting guidelines.
Jafari M, Mohammadi M, Ghazizadeh H, et al. 11
Objective: To study the feasibility of reducing salt in bread and its effect on salt intake and blood pressure.
Design: Community intervention. The evaluation involved a controlled pre‐post survey of residents.
Setting: Two cities in Kerman province (Zarand as the intervention city and Ravar as the control city), Southern Iran.
Participants: A total of 346 and 310 individuals older than 18 years residing in Zarand and Ravar, respectively.
Intervention: Gradual reduction of salt in bread by 40% (from 1.5% to 0.9%) during a 4‐week period, in conjunction with the installation of educational banners and door‐to‐door distribution of brochures about the harmful effects of salt. The control city received door‐to‐door distribution of brochures.
Outcomes: Change in mean salt intake estimated from spot urine samples using the Kawasaki equation; change in systolic blood pressure (SBP) and diastolic blood pressure (DBP).
Summary of results: There was a significantly greater reduction in mean salt intake in the intervention group compared with the control group (P<.001), after adjusting for baseline salt intake in the two groups. A reduction in the intervention group was also observed for SBP (P=.012) but was not significant for DBP (P=.500).
Sources of funding: The study was funded by the Iran Health Insurance Organization.
Comments: The study shows that gradual reduction of salt in bread by 40% is feasible and could lower salt intake and SBP. However, the results should be interpreted with caution as salt intake was estimated through spot urine samples rather than 24‐hour urine collection. The random selection of participants, comparable characteristics between the intervention and control groups, and good follow‐up rates (more than 95% for both groups) were the strengths of the study. It should be noted that the baseline salt intake, SBP, and DBP were different between the intervention and control groups. However, the authors addressed this by adjusting for baseline measurements in the analysis.
Arcand J, Jefferson K, Schermel A, et al. Examination of food industry progress in reducing the sodium content of packaged foods in Canada: 2010 to 2013. Appl Physiol Nutr Metab. 2016;41:684–690.
Objective: To examine the changes in sodium levels in packaged foods sold in Canada from 2010 to 2013, with a focus on changes in food categories, and to examine the products that meet Health Canada's sodium reduction benchmark targets.
Design: Repeated cross‐sectional.
Setting: Canada. Data were collected from February 2010 to April 2011 and from May 2103 to September 2013.
Data: A total of 6918 and 9199 packaged foods and beverages from four largest Canadian grocery chains in 2010 and 2013, respectively.
Intervention: Health Canada's voluntary sodium reduction targets.
Outcomes: Change in sodium levels in foods. Sodium contents were obtained from the Nutrition Facts table. Foods were classified based on Health Canada's Guidance for the Food Industry on Reducing Sodium in Processed Foods.
Summary of results: Between 2010 and 2013, 81.9% of food categories had no change in sodium, 16.2% had a significant reduction in sodium, and 1.9% had a significant increase in sodium. There was a slight increase in the proportion of foods that met Health Canada's sodium benchmark targets from 51.4% of products in 2010 to 58.2% in 2013. The greatest improvements in food categories that met the targets include canned vegetables and legumes, meat and meat substitutes and ready‐to‐eat breakfast cereals.
Source of funding: The study was funded by grants from Canadian Institutes for Health Research and the Canadian Stroke Network. Additional funds were obtained from collaboration of seven food manufacturers and five retailers in Canada to pay for staff to undertake data processing. Author JA had funding from Heart and Stroke Foundation of Canada and MRL from the Earle W. McHenry endowed Chair at the University of Toronto.
Comments: This study showed that overall 16.2% of food categories had significant reductions in sodium content between 2010 and 2013. The large number of products (n=25 881) collected in the database from four major grocery chains, which represents about 75% of the food retail sales, indicates the study is likely to be representative of all products available in Canada. Sodium values were obtained from Nutrition Facts labels, which are shown to accurately report sodium content in Canada. However, there was no use of sales weighted data, which would have provided more information on the likely effects of the reductions or increases on population salt consumption. Overall, this study provides a useful examination of the sodium content in foods in 2010–2011 and 2013 in relation to the voluntary program of sodium reduction in foods in Canada.
Quilez J, Salas‐Salvado J.10 The feasibility and acceptability of reducing salt in partially baked bread: a Spanish case study. Public Health Nutr. 2016;19:983–987.
Objective: To assess the feasibility and acceptability of salt reduction in partially baked breads, by partly replacing salt with a potassium salt.
Design: Before and after survey of sales of reduced salt breads and comparison of complaints between reduced salt bread vs standard salt bread.
Setting: Spain.
Participants: Bread wholesalers.
Intervention: Nine breads reduced sodium by 27.7% by replacing salt with potassium citrate were introduced into the market.
Outcomes: Changes in sales of reduced salt compared with standard bread products.
Summary of results: There were no changes in sales of reduced salt or standard salt breads and no complaints. The wholesalers showed little awareness of the salt reduction.
Source of funding: The work was supported by Europastry S.A. Spain and one of the authors is also a director of that company.
Comments: This study showed that it was possible to reduce salt in bread by around 28% without affecting sales or consumer acceptance. The study was uncontrolled, therefore it is not possible to rule out the fact that other factors may have affected the sales of bread. It was also unclear what percentage of total bread consumption the nine baguette‐like products contributed or whether there were differences between this bread and other breads on the market that might have influenced the results. Sales of neither of the three groups (wholemeal bread, bread containing seeds, or bread containing rye) were affected by the reduction. However, all breads were partially baked and frozen and then defrosted and cooked prior to sale so it is not clear whether it would be possible to make the same reduction in freshly baked bread products. The authors noted that based on these reductions, consumers of reduced‐salt bread would be eating 0.5 g of salt per day less than standard bread consumers. While the work is funded by one of the companies that makes the bread and one of the authors is a company director, we found no evidence of biased results in this case.
4. Discussion
This periodic review identified 40 studies relevant to salt reduction in populations from March to August 2016. While all of the studies provided information related to the implementation of salt reduction strategies, this paper focused on the four studies that evaluated the impact of the interventions. These studies adopted different approaches to measure impact: two through change in salt intake in the population, one through change in sales data and acceptability of low‐sodium foods, and one through changes in sodium levels in packaged foods. Overall, the four studies demonstrated successful interventions that achieved positive results related to dietary salt reduction.
Although the four studies showed positive outcomes, the findings should be interpreted within the context of potential risks of bias. First, in terms of design, only one study employed a control group to compare the effects of the intervention.11 Yet, it was not a “true” control group since the respondents received one of two components of the intervention. Nevertheless, this study allowed for comparison of a multicomponent (structural plus behavior change) vs a single‐component intervention (behavior change alone). The results showed that although the behavior change intervention led to a reduction in salt intake, the multicomponent intervention achieved a significantly greater reduction. This supports the findings from previous studies which demonstrated that salt reduction initiatives are likely to be more effective if they are multicomponent and incorporate intervention activities at a structural level.4, 6
Second, in terms of method of outcome assessment, as described above, the studies used different approaches. Of the two studies that measured change in population salt intake, one used the gold‐standard 24‐hour urine collection while the other used spot urine. The use of spot urine to estimate sodium intake is becoming more widespread, which is likely because of the ease and feasibility of collecting samples. The application of 24‐hour urine collection is often limited in population surveys, which usually require hundreds or thousands of participants, because of its burdensome nature. This is apparent in this review showing that the Australian study8 which collected 24‐hour urine samples, had very low baseline participation and follow‐up rates, while the Iranian study11 which collected spot urine samples, had very good baseline participation and follow‐up rates. While spot urine collections are not considered acceptable to assess individual intake, studies have shown that they can provide an acceptable estimate of mean population salt consumption levels.13 However, most of these studies were conducted in high‐income countries and there is little evidence about the usefulness of spot urine in low‐ or middle‐income countries.45, 47, 48 In the recently published SHAKE Package for Salt Reduction, WHO recommends that if resources and capacity permit, countries should collect 24‐hour urine samples, but in cases where this is not possible, countries may obtain spot urine samples to measure population salt consumption.3 The usefulness of spot urine in estimating mean change in population salt intake over time has also been recently explored.48, 49 Future robust research studies on spot urine are still required to strengthen the evidence regarding its application and to better understand which equations to use in different population groups.
Finally, it is important to note that the interventions were implemented and evaluated in real‐world settings, and thus the results might be confounded by factors not measured by the studies. The findings should be interpreted with this in mind. Although randomized controlled trials or studies conducted in controlled clinical settings are generally considered to give stronger levels of evidence, the four studies nonetheless offer valuable information about real‐world population‐wide interventions with the potential to impact millions of people.
Furthermore, it is noteworthy that bread was the focus of three out of four included studies. This is not surprising since in most high‐income countries, bread is the major source of sodium in the diet.22, 50, 51, 52 Salt in breads, as in other processed foods, provides important functions such as texture, preservation, and taste. However, many industrial bread companies allow salt levels in their products to reach unnecessarily high levels. The growing concern regarding high salt levels in breads led to discussions, calls for action, and negotiations with the bread industry in different countries to reduce sodium in breads. In this review, the Iranian and Spanish study both showed that it is possible to reduce sodium in breads through either gradual reduction or salt substitution, without compromising consumer acceptability and sales. This is in line with the results of a systematic review which showed that salt in breads can be reduced by 40% without significantly affecting consumer acceptability.53 The Canadian study also showed that it is possible to reduce sodium in breads through voluntary sodium reduction targets. These findings show that different intervention options are available to encourage the bread industry to reformulate their products to make them heathier. The WHO SHAKE Package highlights the different strategies to promote food reformulation for a wide range of food products.3
This review also showed that while there is an increasing amount of implementation research related to salt in the upper middle–income and high‐income countries, very few studies are being conducted in low‐ and lower middle–income countries. This stresses the need for more resources and support to conduct research and evaluate interventions in low‐ and lower middle–income countries, given the increasing levels of noncommunicable diseases and deaths.
Conclusions
The four studies varied in approach and quality but showed consistent evidence for the effectiveness of salt reduction interventions, particularly on reducing salt in bread. This review also provided useful information relating to the implementation and evaluation of real‐world population‐wide interventions and demonstrated the need for greater research and support for the implementation of programs to reduce salt in low‐ and lower middle–income countries.
Disclosures
JAS, KT, TSR, CJ, and RM have no conflicts of interest to declare. JW is the Director of the World Health Organization Collaborating Centre on Population Salt Reduction and is supported by a National Health and Medical Research Council/National Heart Foundation Career Development Fellowship on International strategies to reduce salt. JW receives funding from WHO, VicHealth, and the Australian National Health and Medical Research Council of Australia for research on salt reduction. JW was an author on the Land et al. (2016) study and JA was an author on the Arcand et al. (2016) study included in this review.
Supporting information
Acknowledgments
The process to provide regular updates on the science of sodium is supported by the World Hypertension League, the WHO Collaborating Centre on Population Salt Reduction (The George Institute for Global Health), Pan American Health Organization/World Health Organization Technical Advisory Group on Cardiovascular Disease Prevention through Dietary Sodium, and World Action on Salt and Health.
Santos JA, Trieu K, Raj TS, et al. The Science of Salt: A regularly updated systematic review of the implementation of salt reduction interventions (March–August 2016). J Clin Hypertens. 2017;19:439–451. doi: 10.1111/jch.12971.
References
- 1. Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; 2013.
- 3. World Health Organization . SHAKE The Salt Habit: The SHAKE technical package for salt reduction; 2016.
- 4. McLaren L, Sumar N, Barberio AM, et al. Population‐level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst Rev. 2016;9:CD010166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arcand J, Webster J, Johnson C, et al. Announcing “up to date in the science of sodium.” J Clin Hypertens (Greenwich). 2016;18:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trieu K, McLean R, Johnson C, et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (November 2015 to February 2016). J Clin Hypertens (Greenwich). 2016;18:1194–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [Google Scholar]
- 8. Land M‐A, Wu JHY, Selwyn A, et al. Effects of a community‐based salt reduction program in a regional Australian population. BMC public health. 2016;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arcand J, Jefferson K, Schermel A, et al. Examination of food industry progress in reducing the sodium content of packaged foods in Canada: 2010 to 2013. Appl Physiol Nutr Metab. 2016;41:684–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Quilez J, Salas‐Salvado J. The feasibility and acceptability of reducing salt in partially baked bread: a Spanish case study. Public Health Nutr. 2016;19:983–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jafari M, Mohammadi M, Ghazizadeh H, Nakhaee N. Feasibility and outcome of reducing salt in bread: a community trial in Southern Iran. Glob J Health Sci. 2016;8:57138. [Google Scholar]
- 12. Muthuri SK, Oti SO, Lilford RJ, Oyebode O. Salt reduction interventions in sub‐saharan africa: a systematic review. PLoS One. 2016;11:e0149680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huang L, Crino M, Wu JH, et al. Mean population salt intake estimated from 24‐h urine samples and spot urine samples: a systematic review and meta‐analysis. Int J Epidemiol. 2016;45:239–250. [DOI] [PubMed] [Google Scholar]
- 14. Elliott T, Trevena H, Sacks G, et al. A systematic interim assessment of the Australian Government's Food and Health Dialogue. Med J Aust. 2014;200:92–95. [DOI] [PubMed] [Google Scholar]
- 15. Goncalves C, Abreu S, Padrao P, et al. Sodium and potassium urinary excretion and dietary intake: a cross‐sectional analysis in adolescents. Food Nutr Res. 2016;60:29442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. An R. Weekend‐weekday differences in diet among U.S. adults, 2003–2012. Ann Epidemiol. 2016;26:57‐65. [DOI] [PubMed] [Google Scholar]
- 17. Jackson SL, King SM, Zhao L, Cogswell ME. Prevalence of excess sodium intake in the United States ‐ NHANES, 2009–2012. MMWR Morb Mortal Wkly Rep. 2016;64:1393‐1397. [DOI] [PubMed] [Google Scholar]
- 18. Okuda M, Asakura K, Sasaki S, Shinozaki K. Twenty‐four‐hour urinary sodium and potassium excretion and associated factors in Japanese secondary school students. Hypertens Res. 2016;39:524‐529. [DOI] [PubMed] [Google Scholar]
- 19. Service C, Grimes C, Riddell L, He F, Campbell K, Nowson C. Association between parent and child dietary sodium and potassium intakes as assessed by 24‐h urinary excretion. Nutrients. 2016;8:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sobiecki JG, Appleby PN, Bradbury KE, Key TJ. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: results from the European Prospective Investigation into Cancer and Nutrition‐Oxford study. Nutr Res. 2016;36:464‐477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. 2016;315:2542‐2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O'Halloran SA, Grimes CA, Lacy KE, Nowson CA, Campbell KJ. Dietary sources and sodium intake in a sample of Australian preschool children. BMJ Open. 2016;6:e008698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang X, Li X, Vaartjes I, et al. Does education level affect the efficacy of a community based salt reduction program? ‐ A post‐hoc analysis of the China Rural Health Initiative Sodium Reduction Study (CRHI‐SRS). BMC Public Health. 2016;16:759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kang MS, Kim CH, Jeong SJ, Park TS. Dietary sodium intake in people with diabetes in Korea: The Korean National Health and Nutrition Examination Survey for 2008 to 2010. Diabetes Metab J. 2016;40:290‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kraemer MV, Oliveira RC, Gonzalez‐Chica DA, Proenca RP. Sodium content on processed foods for snacks. Public Health Nutr. 2016;19:967‐975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Prentice CA, Smith C, McLean RM. Sodium in commonly consumed fast foods in New Zealand: a public health opportunity. Public Health Nutr. 2016;19:958‐966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. John KA, Maalouf JB, Barsness C, Yuan K, Cogswell ME, Gunn JP. Do lower calorie or lower fat foods have more sodium than their regular counterparts? Nutrients. 2016;8:511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rasheed S, Siddique AK, Sharmin T, et al. Salt intake and health risk in climate change vulnerable coastal Bangladesh: what role do beliefs and practices play? PloS One. 2016;11:e0152783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. John KA, Cogswell ME, Zhao L, Maalouf J, Gunn JP, Merritt RK. US consumer attitudes toward sodium in baby and toddler foods. Appetite. 2016;103:171‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Regan A, Shan CL, Wall P, McConnon A. Perspectives of the public on reducing population salt intake in Ireland. Public Health Nutr. 2016;19:1327‐1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lee J, Park S. Management of sodium‐reduced meals at worksite cafeterias: perceptions, practices, barriers, and needs among food service personnel. Osong Public Health Res Perspect. 2016;7:119‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sugimoto M, Asakura K, Masayasu S, Sasaki S. Relationship of nutrition knowledge and self‐reported dietary behaviors with urinary excretion of sodium and potassium: comparison between dietitians and nondietitians. Nutr Res. 2016;36:440‐451. [DOI] [PubMed] [Google Scholar]
- 33. Quader ZS, Patel S, Gillespie C, et al. Trends and determinants of discretionary salt use: National Health and Nutrition Examination Survey 2003–2012. Public Health Nutr. 2016;19:2195‐2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Asakura K, Uechi K, Masayasu S, Sasaki S. Sodium sources in the Japanese diet: difference between generations and sexes. Public Health Nutr. 2016;19:2011‐2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wilson N, Nghiem N, Eyles H, et al. Modeling health gains and cost savings for ten dietary salt reduction targets. Nutr J. 2015;15:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Souza Ade M, de Souza Bda S, Bezerra IN, Sichieri R. The impact of the reduction of sodium content in processed foods in salt intake in Brazil. Cad Saude Publica. 2016;32:e00064615. [DOI] [PubMed] [Google Scholar]
- 37. van Buren L, Dotsch‐Klerk M, Seewi G, Newson RS. Dietary impact of adding potassium chloride to foods as a sodium reduction technique. Nutrients. 2016;8:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Watkins DA, Olson ZD, Verguet S, Nugent RA, Jamison DT. Cardiovascular disease and impoverishment averted due to a salt reduction policy in South Africa: an extended cost‐effectiveness analysis. Health Policy Plan. 2016;31:75‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nghiem N, Blakely T, Cobiac LJ, Cleghorn CL, Wilson N. The health gains and cost savings of dietary salt reduction interventions, with equity and age distributional aspects. BMC Public Health. 2016;16:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jezewska‐Zychowicz M. Impact of health and nutrition risks perception on the interest in pro‐healthy food on the example of bread. Rocz Panstw Zakl Hig. 2016;67:81‐87. [PubMed] [Google Scholar]
- 41. McMahon E, Clarke R, Jaenke R, Brimblecombe J. Detection of 12.5% and 25% salt reduction in bread in a remote indigenous Australian community. Nutrients. 2016;8:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. De Kock HL, Zandstra EH, Sayed N, Wentzel‐Viljoen E. Liking, salt taste perception and use of table salt when consuming reduced‐salt chicken stews in light of South Africa's new salt regulations. Appetite. 2016;96:383‐390. [DOI] [PubMed] [Google Scholar]
- 43. Peng Y, Li W, Wang Y, et al. Validation and assessment of three methods to estimate 24‐h urinary sodium excretion from spot urine samples in Chinese adults. PloS One. 2016;11:e0149655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yasutake K, Horita N, Umeki Y, et al. Self‐management of salt intake: clinical significance of urinary salt excretion estimated using a self‐monitoring device. Hypertens Res. 2016;39:127‐132. [DOI] [PubMed] [Google Scholar]
- 45. Mizehoun‐Adissoda C, Houehanou C, Chianea T, et al. Estimation of daily sodium and potassium excretion using spot urine and 24‐hour urine samples in a black population (Benin). J Clin Hypertens (Greenwich). 2016;18:634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ma Y, He FJ, Li N, et al. Salt sales survey: a simplified, cost‐effective method to evaluate population salt reduction programs–a cluster‐randomized trial. Hypertens Res. 2016;39:254‐259. [DOI] [PubMed] [Google Scholar]
- 47. Webster J, Su'a SA, Ieremia M, et al. Salt intakes, knowledge, and behavior in Samoa: monitoring salt‐consumption patterns through the World Health Organization's Surveillance of Noncommunicable Disease Risk Factors (STEPS). J Clin Hypertens (Greenwich). 2016;18:884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Do HT, Santos JA, Trieu K, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a vietnamese province based on estimations from spot urine samples. J Clin Hypertens (Greenwich). 2016;18:1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Petersen KS, Wu JHY, Webster J, et al. Estimating mean change in population salt intake using spot urine samples. Int J Epidemiol. 2016;0:1–9. [DOI] [PubMed] [Google Scholar]
- 50. Centers for Disease Control and Prevention . Vital signs: food categories contributing the most to sodium consumption––United States, 2007–2008. MMWR Morb Mortal Wkly Rep. 2012;61:92–98. [PubMed] [Google Scholar]
- 51. Kloss L, Meyer JD, Graeve L, Vetter W. Sodium intake and its reduction by food reformulation in the European Union—a review. NFS J. 2015;1:9–19. [Google Scholar]
- 52. Charlton K, Yeatman H, Houweling F, Guenon S. Urinary sodium excretion, dietary sources of sodium intake and knowledge and practices around salt use in a group of healthy Australian women. Aust N Z J Public Health. 2010;34:356–363. [DOI] [PubMed] [Google Scholar]
- 53. Jaenke R, Barzi F, McMahon E, Webster J, Brimblecombe J. Consumer acceptance of reformulated food products: a systematic review and meta‐analysis of salt‐reduced foods. Crit Rev Food Sci Nutr. 2016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


