Abstract
Hypertension affects about one in three US adults, from recent surveillance, or four in nine based on the 2017 ACC/AHA Hypertension Guideline; about half of them have their blood pressure controlled, and nearly one in six are unaware of their hypertension status. National estimates of hypertension awareness, treatment, and control in the United States are traditionally based on measured BP from National Health and Nutrition Examination Survey (NHANES); however, at the state level, only self‐reported hypertension awareness and treatment are available from BRFSS. We used national‐ and state‐level representative samples of adults (≥20 years) from NHANES 2011‐2014 and BRFSS 2013 and 2015, respectively. The authors generated multivariable logistic regression models using NHANES to predict the probability of hypertension and undiagnosed hypertension and then applied the fitted model parameters to BRFSS to generate state‐level estimates. The predicted prevalence of hypertension was highest in Mississippi among adults (42.4%; 95% CI: 41.8‐43.0) and among women (42.6%; 41.8‐43.4) and highest in West Virginia among men (43.4%; 42.2‐44.6). The predicted prevalence was lowest in Utah 23.7% (22.8‐24.6), 26.4% (25.0‐27.7), and 21.0% (20.0‐22.1) for adults, men, and women, respectively. Hypertension predicted prevalence was higher in most Southern states and higher among men than women in all states except Mississippi and DC. The predicted prevalence of undiagnosed hypertension ranged from 4.1% (3.4‐4.8; Kentucky) to 6.5% (5.5‐7.5; Hawaii) among adults, from 5.0% (4.0‐5.9; Kentucky) to 8.3% (6.9‐9.7; Hawaii) among men, and from 3.3% (2.5‐4.1; Kentucky) to 4.8% (3.4‐6.1; Vermont) among women. Undiagnosed hypertension was more prevalent among men than women in all states and DC.
Keywords: blood pressure, hypertension, prevalence, state‐level, undiagnosed hypertension, variance
1. INTRODUCTION
Hypertension is a leading risk factor for cardiovascular disease and is a significant contributor to morbidity and mortality, affecting nearly one out of three adults, or about 75 million people in the United States according to recent surveillance estimates, or four of nine according to the 2017 ACC/AHA Hypertension Guideline.1, 2, 3 Each year, hypertension contributes to more than 400 000 deaths in the United States and contributes over $50 billion in direct medical costs and indirect costs due to lost productivity from premature death.4 Among those with hypertension, only about half have their blood pressure (BP) under control.2 About one in six, or 11 million US adults with hypertension are not aware that they have it and are not being treated.2 While there have been significant increases in hypertension awareness, treatment, and control over the past decade, the prevalence of hypertension remains largely unchanged.5 Surveillance of hypertension, both diagnosed and undiagnosed, and its treatment and control is important to identify high‐risk populations and refine interventions to improve prevention, management, and control of this prevalent chronic condition.
National surveillance of hypertension, including the objectives and measures reported by the Department of Health and Human Services Healthy People 2020 program and the Million Hearts® initiative, primarily relies upon data from the National Health and Nutrition Examination Survey (NHANES), which assesses participants’ BP through direct measurement using a standardized protocol., , At the subnational level, however, there are currently no comprehensive surveys or data systems that capture measured BP, to provide objective estimates of hypertension. State‐, county‐, or local‐level estimates of hypertension based on measured BP exist only for states or localities that have performed health examination surveys.6, 7, 8 Most often, estimates of hypertension at the state level rely upon information reported by participants in surveys, like the Centers for Disease Control and Prevention's (CDC) Behavioral Risk Factor Surveillance System (BRFSS). However, self‐reported information is subject to recall bias and does not allow for estimates of undiagnosed hypertension or BP control.9 To address this lack of subnational objective data, two previous studies used both NHANES and BRFSS and regression modeling techniques to estimate the prevalence of uncontrolled hypertension by state for 1988‐1992 and 2001‐2003, and by county for 2001 and 2009.10, 11 Our current study expands on this work to (a) provide updated state‐level estimates of hypertension and undiagnosed hypertension in 2013‐2015; and (b) unlike previous studies, we calculated the variance of the prevalence estimates, to provide confidence intervals (CI's) and allow for statistical testing. The variance calculated in this study takes into account the complex sampling designs of both surveys, plus the error inherent to the regression models. We also provided the step‐by‐step methods, to allow for their application to other data sources or outcomes.
2. METHODS
2.1. Data sources
Two sources of data were used for this study. We used NHANES 2011‐2014 to develop the prediction models and estimated the prevalence of hypertension and undiagnosed hypertension at the state‐level based on BRFSS 2013 and 2015.
National Health and Nutrition Examination Survey, conducted by the CDC's National Center for Health Statistics (NCHS), is a nationally representative survey, designed to assess the health and nutritional status of the civilian, noninstitutionalized US population. NHANES includes in‐person interviews and physical examinations conducted in a mobile examination center (MEC). Additional information on the survey design and methods is available online (https://www.cdc.gov/nchs/nhanes). We combined two recent cycles of NHANES (2011‐2012 and 2013‐2014) to generate stratified, multivariable logistic regression models to predict the prevalence of hypertension at the national level. The examination response rate was 69.5% in 2011‐2012 and 68.5% in 2013‐2014.
Selected variables were included from the in‐person interview, including history of hypertension and BP medication use, history of high blood cholesterol and cholesterol‐lowering medication use, smoking, physical activity, alcohol consumption, self‐reported history of diabetes, history of cardiovascular disease, and health insurance coverage. During the physical examination, up to three BP measurements were taken by a physician on all participants aged ≥8 years using a manual sphygmomanometer and a standard protocol.12 Approximately 95% of respondents aged ≥20 years had two or three recorded BP measurements, which were averaged for this analysis. For those participants with only one measurement, the single measure was used. Hypertension was defined as having high BP (an average systolic BP ≥140 mm Hg or an average diastolic BP ≥90 mm Hg) or current BP‐lowering medication use. Undiagnosed hypertension was defined as having high BP and never having been told that they had hypertension or high BP. Participants’ height and weight were also measured and recorded during the examination and used to calculate body mass index (BMI; kg/m2). Because BMI in the adult population has a highly skewed distribution, a natural log transformation was performed for this analysis. Of the 10 907 adults aged ≥20 years who were examined at the MEC during 2011‐2014, we excluded 122 pregnant women, 474 participants who were missing hypertension‐related data, and 112 who were missing data on model covariates, which yielded an analytic sample of 10 199.
BRFSS is conducted in coordination with US states, territories, and the CDC and is a state‐based system of cross‐sectional telephone surveys that collects health‐related risk behaviors and preventive health practices information from more than 400 000 US adult residents each year. The survey was established in 1984, and additional information can be found online (https://www.cdc.gov/brfss/). We combined BRFSS data from 2013 to 2015, because questions regarding hypertension are asked every odd year on the rotating core questionnaire. The median weighted response rate for both landline and cell phones was 45.9% in 2013 and 47.2% in 2015.
Two questions in BRFSS were used to assess the prevalence of self‐reported hypertension. Respondents were asked “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?”. Those who answered “yes” to this question were then asked, “Are you currently taking medicine for your high blood pressure?”. Estimates were calculated for the 50 states and the District of Columbia (DC). Of the 904 967 adults aged ≥20 years who were interviewed in 2013 and 2015, we excluded 5113 pregnant women, 3356 participants who were missing answers to hypertension‐related questions, and 79 072 participants who were missing responses to other covariate questions. The measures and questions incorporated from each survey are shown in Table 1.
Table 1.
Variables used in regression models to predict the probability of Hypertension: NHANES 2011‐2014 and BRFSS 2013/2015
| Survey | NHANES | BRFSS |
|---|---|---|
| Model strata | ||
| Sex | Sex asked if necessary | Sex asked if necessary |
| Hypertension Awareness/Treatment status: | ||
| (1) Unaware | An answer of "No" to the question: "Have you ever been told by a doctor or other health professional that you had hypertension, also called high blood pressure?" | An answer of "No," "Yes, but female told only during pregnancy," or "Told borderline high or pre‐hypertensive" to the question: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?" |
| (2) Aware/Untreated | An answer of "Yes" to the question above and answer of "No" to the question: "Because of your high blood pressure/hypertension have you ever been told to take prescribed medicine?" | An answer of "Yes" to the question: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?" and an answer of "No" to the question: "Are you currently taking medicine for your high blood pressure?" |
| (3) Aware/Treated | An answer of "Yes" to both questions above, and an answer of "Yes" to the question: "Are you now taking a prescribed medicine?" | An answer of "Yes" to both questions: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?" and "Are you currently taking medicine for your high blood pressure?" |
| Outcomes | ||
| (1) Hypertension | High blood pressure (BP) or current use of BP‐lowering medication. | Predicted by models among those Unaware or Aware/Untreated (Strata 1 & 2); participants Aware/Treated are defined as hypertensive (Strata 3). |
| High blood pressure (BP) | Average of up to 3 consecutive measurements. An average systolic BP ≥140 mm Hg or an average diastolic BP ≥90 mm Hg | Not available |
| Current blood pressure lowering medication use | An answer of "yes" to both questions: "Because of your high blood pressure/hypertension have you ever been told to take prescribed medicine?" and "Are you now taking a prescribed medicine?" | An answer of "yes" to both questions: "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" and "Are you currently taking medicine for your high blood pressure?" |
| (2) Undiagnosed Hypertension | High BP and never having been told that they have hypertension or high blood pressure | Predicted by models among those who are unaware of their hypertension/high blood pressure (Strata 1) |
| Model covariates | ||
| Age in yearsa | ||
| 20‐29 | Calculated from date of birth and verified with participant during screener questionnaire | "What is your age?" |
| 30‐39 | ||
| 40‐49 | ||
| 50‐59 | ||
| 60‐69 | ||
| 70‐79 | ||
| 80+ | ||
| Race/ethnicitya | ||
| Non‐Hispanic white | "Do you consider yourself Hispanic/Latino?" and "What race do you consider yourself to be?" | "Are you Hispanic or Latino? (Yes or No)" and "Which one of these groups would you say best represents your race? (White, Black or African‐American, Asian, Native Hawaiian or Other Pacific Islander, American Indian or Alaska Native, or Other)" |
| Non‐Hispanic black | ||
| Non‐Hispanic Asian | ||
| Hispanic | ||
| Other | ||
| Education (≥25 y) | ||
| <High school | "What is the highest grade or level of school you have completed or the highest degree you have received?" | "What is the highest grade or year of school you completed?" |
| High school graduate | ||
| Some college or AA degree | ||
| College graduate | ||
| Household Income | ||
| <$35 000 | "Now I am going to ask about the total combined income in the last 12 mo, including income from all sources we have just talked about such as wages, salaries, Social Security or retirement benefits, help from relatives and so forth. Can you tell me that amount before taxes?" (reported as a range value in dollars) | "Is your annual household income from all sources...?" (reported as a range value in dollars) |
| ≥$35 000 missingb | ||
| Health insurance statusa | ||
| Yes | "Are you covered by health insurance or some other kind of health care plan? [Include health insurance obtained through employment or purchased directly as well as government programs like Medicare and Medicaid that provide medical care or help pay medical bills]" | "Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?" |
| No | ||
| Body mass indexa | (weight [kg]/height [m2]) | (weight [kg]/height [m2]) |
| Height | Measured | "About how tall are you without shoes?" |
| Weight | Measured | "About how much do you weigh without shoes?" |
| Current smoker | ||
| Yes | An answer of "Yes" to the question: "Have you smoked at least 100 cigarettes in your entire life?" and an answer of "Every day" or "Some days" to the question: "Do you now smoke cigarettes...?" | An answer of "Yes" to the question: "Have you smoked at least 100 cigarettes in your entire life?" and an answer of "Every day" or "Some days" to the question: "Do you now smoke cigarettes every day, some days, or not at all?" |
| No | An answer of "No" to the question: "Have you smoked at least 100 cigarettes in your entire life?" or an answer of "Not at all" to the question: "Do you now smoke cigarettes...?" | An answer of "No" to the question: "Have you smoked at least 100 cigarettes in your entire life?" or an answer of "Not at all" to the question: "Do you now smoke cigarettes every day, some days, or not at all?" |
| Alcohol consumption | ||
| <1 drink per day | "In any one year, have you had at least 12 drinks of any type of alcoholic beverage? By a drink, I mean a 12 oz. beer, a 4 oz. glass of wine, or an ounce of liquor." and "In your entire life, have you had at least 12 drinks of any type of alcoholic beverage?" and "In the past 12 mo, how often did you drink any type of alcoholic beverage?" and "In the past 12 mo, on those days that you drank alcoholic beverages, on the average, how many drinks did you have?" | "During the past 30 d, have you had at least one drink of any alcoholic beverage such as beer, wine, a malt beverage or liquor?" and "During the past 30 d, how many days per week or per month did you have at least one drink of any alcoholic beverage?" and "One drink is equivalent to a 12‐ounce beer, a 5‐ounce glass of wine, or a drink with one shot of liquor. During the past 30 d, on the days when you drank, about how many drinks did you drink on the average?" |
| ≥1 drink per day missingb | ||
| Any leisure‐time physical activity | ||
| Yes | An answer of "Yes" to the questions: "Over the past 30 d, did you do any vigorous activities for at least 10 minutes that caused heavy sweating, or large increases in breathing or heart rate?" or "Over the past 30 d, did you do moderate activities for at least 10 minutes that cause only light sweating or a slight to moderate increase in breathing or heart rate?" | An answer of "Yes" to the question: "During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?" |
| No missing | An answer of "No" to both questions above | An answer of "No' to the question above |
| Diabetes | ||
| Yes | An answer of "Yes" to the question: "Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?" | An answer of "Yes" to the question: "Have you ever been told by a doctor that you have diabetes?" |
| No | An answer of "No" or "Borderline" to the above question | An answer of "No," "No, pre‐diabetes or borderline diabetes," or "Yes, but female told only during pregnancy" to the question above |
| High cholesterol | ||
| Yes | An answer of "Yes" to the question: "Have you ever been told by a doctor or other health professional that your blood cholesterol level was high?" | An answer of "Yes" to the question: "Have you EVER been told by a doctor, nurse or other health professional that your blood cholesterol is high?" |
| No | An answer of "No" to the question: "Have you ever had your blood cholesterol checked?" or an answer of "No" to the question above | An answer of "No" to the question: "Have you ever had your blood cholesterol checked?" or an answer of "No" to the question above |
| History of CVD | ||
| Yes | An answer of "yes" to any of the following questions: "Has a doctor or other health professional ever told you that you had…?": "…coronary heart disease?", "angina, also called angina pectoris?", "a heart attack (also called myocardial infarction?", "a stroke?" | An answer of "yes" to any of the following questions: "Has a doctor, nurse, or other health professional ever told you that you had any of the following?": "angina or coronary heart disease", "a heart attack, also called myocardial infarction", "a stroke" |
| No | An answer of "no" to all of the questions. | An answer of "no" to all of the questions. |
BRFSS, Behavioral Risk Factor Surveillance System; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Survey
Variables must be included in the regression models by force.
Due to the high proportion of participants missing data in either survey dataset or analytic sample for these variables (>10%), "missing" categories were created and included in the models.
2.2. Statistical methods and data analysis
Detailed methods, formulas, and model validation results are provided in the supporting document. Briefly, using the NHANES data, we generated stratified, multivariable logistic regression models to estimate the national‐level prevalence of hypertension. We then applied the model coefficients to BRFSS 2013 and 2015 to predict the prevalence of hypertension and undiagnosed hypertension at the state‐level among men, women, and overall. To generate 95% CIs and test for significant differences from the median state‐level predicted prevalence (t test), we used the jackknife repeated sampling technique to estimate the variance.
We stratified the analysis by self‐reported hypertension status; participants were classified into three hypertension status groups: (a) Those who were never told they had hypertension (“Unaware”); (b) those who had been told they had hypertension but were not currently taking prescribed medication (“Aware/Untreated”); and (c) those who had been told they had hypertension and were currently taking prescribed medication (“Aware/Treated”). We further stratified the groups by sex, creating a total of six analytic strata (Table 1).
Age was included in the models as a categorical variable (20‐29; 30‐39; 40‐49; 50‐59; 60‐69; ≥70). Race/ethnicity was classified into four groups: non‐Hispanic white, non‐Hispanic black, Hispanic, and other races including multiracial. Educational level was defined for those aged ≥25 years: <high school graduate, high school graduate, some college or associate degree, and college graduate. Household income was categorized into two groups: <$35 000 per year and ≥$35 000 per year; two categories were defined to preserve model degrees of freedom. Because of a high proportion of missing values (>10% in BRFSS), participants missing household income were categorized as such and included in the models. Health insurance coverage was dichotomized as yes or no. Smoking status was categorized as current smoker, yes or no. Self‐reported consumption of alcohol was averaged and categorized as none, <1 alcoholic beverage per day, or ≥1 alcoholic beverage per day. Participants missing information on alcohol consumption were included in the analysis, due to the high proportion missing (about 10% of participants). Leisure‐time aerobic physical activity was classified as any physical activity or none. BMI was log‐transformed as a continuous variable. Participants’ self‐reported history of cardiovascular disease, diagnosed diabetes, and high blood cholesterol (yes or no) was also considered in the models.
We included four variables (a) age groups; (b) race/ethnicity; (c) health insurance status; and (d) log‐transformed BMI by force in regression models, which were known to be associated with blood pressure (BP) and/or uncontrolled hypertension. Additionally, eight variables were considered as potential covariates and some of them were selected by backward model selection method to get a best‐fitted model for each analytic stratum.
The BRFSS samples were also stratified into the 6 groups by sex and by self‐reported hypertension status, which were used for the regressions described above. The groups were then pooled using appropriate sample weights to predict estimates of probabilities by state. We thus predicted state‐level estimates of the prevalence of hypertension and the prevalence with uncontrolled hypertension among all adults, men, and women, respectively. Detailed formulas are described in the Section “Estimating the State‐level Prevalence using regression models” in the Supporting information.
A concatenated dataset using analytic sample datasets from both NHANES and BRFSS was first built. For the BRFSS samples, we combined strata which had only one or relatively few primary sample units (PSU), with their adjacent strata to form somewhat larger “pseudostrata” or “sampling error calculation strata.” Then, we divided the combined PSUs within each pseudostratum into random groups to form pseudoPSUs or “sampling error computation units” in order to simplify variance estimation and reduce computation time. We applied a jackknife resampling technique for each state by deleting one pseudostratum at a time to estimate its variance of the estimated prevalence. More details are described in the Section “Variance estimation using a Jackknife resampling technique” in the Supporting information.
All statistical analyses were performed using SAS (Release 9.4; Cary, NC, USA) with procedures to incorporate the sampling weights and complex sampling designs.
3. RESULTS
The sample sizes and characteristic distributions for each stratum in NHANES and BRFSS are provided in Table 2. In NHANES 2011‐2014, there were a total of 10 199 adults in the sample; 6458 had never been told they had hypertension (“Unaware”), 948 reported having been told they had hypertension but were not currently taking BP‐lowering medication (“Aware/Untreated”), and 2793 reported being told they had hypertension and taking BP‐lowering medication (“Aware/Treated”). In BRFSS 2013 and 2015, a total of 817 426 adults were interviewed and had complete data on all model covariates; 480 503 reported never being told that they had hypertension (“Unaware”), 53 437 reported having been told they had hypertension but were not taking BP‐lowering medication (“Aware/Untreated”), and 283 486 reported being told that they had hypertension and were taking BP‐lowering medication (“Aware/Treated”).
Table 2.
Characteristic distributiona of analytic samples for NHANES 2011‐2014 and BRFSS 2013/2015, by hypertension awareness and treatment statusb, c, d
| NHANES 2011‐2014 | BRFSS 2013/2015 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Unawareb | Aware/Untreatedc | Aware/Treatedd | Total | Unawareb | Aware/Untreatedc | Aware/Treatedd | |||||||||
| (n = 10 199) | (n = 6458) | (n = 948) | (n = 2793) | (n = 817 426) | (n = 480 503) | (n = 53 437) | (n = 283 486) | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Sex | ||||||||||||||||
| Men | 5045 | 49 | 3247 | 49.6 | 511 | 54.1 | 1287 | 45.3 | 339 289 | 48.7 | 195 417 | 47.7 | 28 318 | 61.4 | 115 554 | 47.9 |
| Women | 5154 | 51 | 3211 | 50.4 | 437 | 45.9 | 1506 | 54.7 | 478 137 | 51.3 | 285 086 | 52.3 | 25 119 | 38.6 | 167 932 | 52.1 |
| Age in years | ||||||||||||||||
| 20‐29 | 1713 | 18.3 | 1 576 | 25.2 | 118 | 14.1 | 19 | 0.7 | 65 852 | 16.7 | 59 756 | 22.9 | 4839 | 16.9 | 1257 | 1.1 |
| 30‐39 | 1756 | 17.4 | 1432 | 21.4 | 208 | 20.9 | 116 | 4.9 | 88 878 | 17.2 | 75 080 | 22 | 7532 | 21.3 | 6266 | 4.3 |
| 40‐49 | 1787 | 19 | 1269 | 20.6 | 214 | 24.6 | 304 | 12.4 | 113 386 | 17.5 | 84 324 | 19.6 | 9312 | 21 | 19 750 | 11.5 |
| 50‐59 | 1696 | 19 | 970 | 16.8 | 184 | 22.2 | 542 | 23.8 | 171 337 | 19.6 | 103 827 | 17.7 | 13 138 | 21.2 | 54 372 | 24.1 |
| 60‐69 | 1698 | 14.3 | 714 | 10 | 132 | 10.8 | 852 | 27.7 | 188 921 | 15.4 | 88 761 | 10.6 | 10 829 | 12.4 | 89 331 | 28.3 |
| ≥70 | 1549 | 12.1 | 497 | 6 | 92 | 7.5 | 960 | 30.5 | 189 052 | 13.5 | 68 755 | 7.3 | 7787 | 7.2 | 112 510 | 30.8 |
| Race‐ethnicity | ||||||||||||||||
| Non‐Hispanic white | 4104 | 66.6 | 2 525 | 65 | 389 | 65.1 | 1190 | 71.7 | 658 893 | 66.8 | 387 571 | 65.7 | 41 898 | 63.9 | 229 424 | 70.2 |
| Non‐Hispanic black | 2372 | 11.3 | 1264 | 9.8 | 228 | 12.9 | 880 | 14.6 | 66 460 | 11.8 | 30 165 | 10.1 | 4370 | 12.7 | 31925 | 15.7 |
| Hispanic | 2141 | 14.3 | 1476 | 16.3 | 206 | 14.8 | 459 | 8.6 | 52 600 | 14.9 | 36 917 | 16.8 | 4216 | 17.3 | 11 467 | 9.4 |
| Other | 1582 | 7.8 | 1193 | 8.9 | 125 | 7.3 | 264 | 5.1 | 39 473 | 6.6 | 25 850 | 7.3 | 2953 | 6 | 10 670 | 4.7 |
| Education (≥25 y) | ||||||||||||||||
| <High school | 2125 | 14.4 | 1147 | 12.4 | 202 | 15.9 | 776 | 19.2 | 59 979 | 14.3 | 27 819 | 11.3 | 4637 | 16.1 | 27 523 | 16.7 |
| High school graduate | 1992 | 18.6 | 1113 | 16.7 | 223 | 21.8 | 656 | 22.7 | 219 700 | 18.5 | 112 232 | 22 | 14 541 | 25.7 | 92 927 | 31.3 |
| Some college or AA degree | 2653 | 27.5 | 1553 | 25.1 | 273 | 32.2 | 827 | 32.5 | 212 513 | 27.5 | 120 017 | 26.1 | 14 944 | 28.8 | 77 552 | 30.1 |
| College graduate | 2496 | 29.7 | 1784 | 32.2 | 183 | 22.5 | 529 | 25.4 | 294 669 | 29.8 | 192 146 | 28.5 | 17 373 | 21.9 | 85 150 | 21.5 |
| <25 y of age | 933 | 9.8 | 861 | 13.6 | 67 | 7.5 | 5 | 0.2 | 30 565 | 9.9 | 28 289 | 12.1 | 1942 | 7.4 | 334 | 0.3 |
| Household incomee | ||||||||||||||||
| <$35 K | 3939 | 29.6 | 2298 | 27.3 | 414 | 34.8 | 1227 | 33.9 | 271 102 | 29.5 | 139 381 | 31.8 | 20 420 | 39.5 | 111 301 | 38.8 |
| ≥$35 K | 5792 | 67 | 3856 | 69.2 | 497 | 62.1 | 1439 | 62.7 | 432 555 | 67.1 | 278 388 | 55.6 | 26 647 | 49.2 | 127 520 | 46.8 |
| Missing income | 468 | 3.4 | 304 | 3.5 | 37 | 3.1 | 127 | 3.4 | 113 769 | 3.4 | 62 734 | 12.5 | 6370 | 11.3 | 44 665 | 14.4 |
| Health insurancef | ||||||||||||||||
| Yes | 7916 | 81.1 | 4710 | 77.3 | 673 | 76.4 | 2533 | 92.9 | 743 440 | 85.7 | 427 802 | 83.4 | 45 221 | 78.5 | 270 417 | 93.3 |
| No | 2283 | 18.9 | 1748 | 22.6 | 275 | 23.6 | 260 | 7.1 | 73 986 | 14.3 | 52 701 | 16.6 | 8216 | 21.5 | 13 069 | 6.7 |
| Current smokerg | ||||||||||||||||
| Yes | 2080 | 19.9 | 1369 | 20.3 | 262 | 28.4 | 449 | 15.4 | 125 649 | 17.6 | 77 160 | 17.9 | 11 863 | 25.7 | 36 626 | 14.9 |
| No | 8119 | 80.1 | 5089 | 79.7 | 686 | 71.6 | 2344 | 84.6 | 691 777 | 82.4 | 403 343 | 82.1 | 41 574 | 74.3 | 246 860 | 85.1 |
| Alcohol consumptionh | ||||||||||||||||
| None | 5244 | 45.2 | 3258 | 44 | 468 | 44.3 | 1518 | 48.7 | 492 647 | 57.7 | 268 440 | 54.3 | 30 605 | 54.6 | 193 602 | 66.8 |
| <1 drink/day | 2605 | 30 | 1879 | 33.6 | 241 | 27.2 | 485 | 21 | 222 839 | 29.2 | 150 496 | 32.3 | 14 241 | 27.9 | 58 102 | 21.7 |
| ≥1 drink/day | 1279 | 15.7 | 820 | 15.3 | 149 | 18.9 | 310 | 15.6 | 101 940 | 13.2 | 61 567 | 13.3 | 8591 | 17.5 | 31 782 | 11.5 |
| Missing alcohol | 1071 | 9.2 | 501 | 7.1 | 90 | 9.6 | 480 | 14.7 | ||||||||
| Any physical activityi | ||||||||||||||||
| Yes | 5098 | 54.4 | 3549 | 59.3 | 447 | 48.6 | 1102 | 42.9 | 572 367 | 69.5 | 355 608 | 72.4 | 36 697 | 67.8 | 180 062 | 62.7 |
| No | 5101 | 45.6 | 2909 | 40.7 | 501 | 51.4 | 1691 | 57.1 | 206 748 | 24.7 | 101 467 | 21.5 | 14 304 | 26.4 | 90 977 | 32.2 |
| Missing PA | 0 | 0 | 0 | 0 | 38 311 | 5.8 | 23 428 | 6.1 | 2436 | 5.7 | 12 447 | 5.1 | ||||
| Diabetesj , k | ||||||||||||||||
| Yes | 1366 | 10.3 | 416 | 4.7 | 90 | 7.4 | 860 | 26.8 | 106 318 | 10.9 | 26 029 | 4.5 | 5617 | 9.1 | 74 672 | 27.4 |
| No | 8833 | 89.7 | 6042 | 95.3 | 858 | 92.6 | 1933 | 73.2 | 711 108 | 89.1 | 454 474 | 95.5 | 47 820 | 90.9 | 208 814 | 72.6 |
| High cholesterolj,l | ||||||||||||||||
| Yes | 3536 | 34.9 | 1482 | 23.9 | 353 | 38.8 | 1701 | 63.3 | 316 137 | 31.8 | 122 788 | 20.4 | 23 224 | 38.8 | 170 125 | 58.5 |
| No | 6663 | 65.1 | 4976 | 76.1 | 595 | 61.2 | 1092 | 36.7 | 501 289 | 68.2 | 357 715 | 79.6 | 30 213 | 61.2 | 113 361 | 41.5 |
| History of CVDj , m | ||||||||||||||||
| Yes | 927 | 7.6 | 221 | 3.1 | 68 | 5.8 | 638 | 20.6 | 97106 | 9 | 25 449 | 3.8 | 5606 | 8.3 | 66 051 | 22.1 |
| No | 9272 | 92.4 | 6237 | 96.9 | 880 | 94.2 | 2155 | 79.4 | 720 320 | 91 | 455 054 | 96.2 | 47 831 | 91.7 | 217 435 | 77.9 |
BRFSS, Behavioral Risk Factor Surveillance System; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Survey
Unweighted sample size (n) and weighted percent (%).
Unaware is defined as: NHANES: an answer of "no" to the question "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?"; BRFSS: an answer of "No," "Yes, but female told only during pregnancy," or "Told borderline high or pre‐hypertensive" to the question: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?"
Aware/Untreated is defined as: NHANES: an answer of "yes" to the question "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?" and an answer of no to the questions "Because of your high blood pressure/hypertension have you ever been told to take prescribed medicine?" or "Are you now taking a prescribed medicine?"; BRFSS: an answer of "Yes" to the question: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?" and an answer of "No" to the question: "Are you currently taking medicine for your high blood pressure?"
Aware/Treated is defined as: NHANES: an answer of "yes" to the questions "Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?", "Because of your high blood pressure/hypertension have you ever been told to take prescribed medicine?", and "Are you now taking a prescribed medicine?"; BRFSS: An answer of "Yes" to the questions: "Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure?" and "Are you currently taking medicine for your high blood pressure?"
Household Income is defined by answers to the questions (unknowns and refusals defined as "missing"): NHANES: "Now I am going to ask about the total combined income in the last 12 mo, including income from all sources we have just talked about such as wages, salaries, Social Security or retirement benefits, help from relatives and so forth. Can you tell me that amount before taxes?" (reported as a range value in dollars); BRFSS: "Is your annual household income from all sources...?" (reported as a range value in dollars)
Health insurance is defined by an answer of "yes"/"no" to the questions (unknowns and refusals excluded): NHANES: "Are you covered by health insurance or some other kind of health care plan?"; BRFSS: "Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?"
Current smoking status is defined by answers to the questions: "Have you smoked at least 100 cigarettes in your entire life?" and "Do you now smoke cigarettes every day, some days, or not at all?" Unknowns and refusals excluded.
Average alcohol consumption (drinks per day) is defined by answers to the questions (unknowns and refusals defined as "missing"): NHANES: "In any one year, have you had at least 12 drinks of any type of alcoholic beverage? By a drink, I mean a 12 oz. beer, a 4 oz. glass of wine, or an ounce of liquor." and "In your entire life, have you had at least 12 drinks of any type of alcoholic beverage?" and "In the past 12 mo, how often did you drink any type of alcoholic beverage?" and "In the past 12 mo, on those days that you drank alcoholic beverages, on the average, how many drinks did you have?"; BRFSS: "During the past 30 d, have you had at least one drink of any alcoholic beverage such as beer, wine, a malt beverage or liquor?" and "During the past 30 d, how many days per week or per month did you have at least one drink of any alcoholic beverage?" and "One drink is equivalent to a 12‐ounce beer, a 5‐ounce glass of wine, or a drink with one shot of liquor. During the past 30 d, on the days when you drank, about how many drinks did you drink on the average?"
Leisure‐time physical activity is defined by answers to the questions (unknowns and refusals excluded): NHANES: "Over the past 30 d, did you do any vigorous activities for at least 10 minutes that caused heavy sweating, or large increases in breathing or heart rate?" and "Over the past 30 d, did you do moderate activities for at least 10 minutes that cause only light sweating or a slight to moderate increase in breathing or heart rate?"; BRFSS: "During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?"
Based on self‐report in NHANES to align with BRFSS.
Diabetes is defined by answers to the questions (unknowns and refusals excluded): NHANES: "Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?" Answers of "Borderline" are defined as no diabetes. BRFSS: "Have you ever been told by a doctor that you have diabetes?" Answers of "No, pre‐diabetes or borderline diabetes," or "Yes, but female told only during pregnancy" are defined as no diabetes.
High cholesterol is defined by answers to the questions (unknowns and refusals excluded): NHANES: "Have you ever been told by a doctor or other health professional that your blood cholesterol level was high?"; BRFSS: "Have you EVER been told by a doctor, nurse or other health professional that your blood cholesterol is high?"
History of CVD is defined by answers to the questions (unknowns and refusals excluded): NHANES: "Has a doctor or other health professional ever told you that you had…?": "…coronary heart disease?", "angina, also called angina pectoris?", "a heart attack (also called myocardial infarction?", "a stroke?"; BRFSS: "Has a doctor, nurse, or other health professional ever told you that you had any of the following?": "angina or coronary heart disease", "a heart attack, also called myocardial infarction", "a stroke"
Model parameters selected varied by sex and hypertension awareness and treatment status. Fitted models contain six or seven covariates including four forced ones. Household income and smoking status were not included in any stratum. Three covariates (alcohol consumption, history of high blood cholesterol, and cardiovascular disease), in addition, to the forced four covariates, were selected for the hypertension unaware group among men, while only history of high blood cholesterol was selected for the aware/untreated men and alcohol consumption and history of cardiovascular disease were selected for the aware/treated men. Alcohol consumption, any physical activity status, and history of high blood cholesterol were selected for the unaware women, but educational level was selected for the other hypertension awareness and treatment status groups. Two covariates, educational level and history of high blood cholesterol, were selected for the aware/untreated women, while educational level and history of diagnosed diabetes were selected for the aware/treated women.
The estimated coefficients of the fitted logistic regression models for all six strata are shown in Table S4. For models for all six strata, the predicted probability of hypertension tended to increase with age. Non‐Hispanic whites had a lower predicted probability of hypertension than other race‐ethnic groups, except for the unaware men group. Those who had health insurance tended to have lower predicted probability of hypertension except for the unaware or aware/treated men groups.
3.1. Hypertension
Among all adults aged ≥20 years, the predicted prevalence of hypertension ranged from 23.7% (95% CI: 22.8%‐24.6%) in Utah to 42.4% (95% CI: 41.8%‐43.0%) in Mississippi (Figure 1A and Table S1). The median predicted prevalence was 32.7% (95% CI: 31.9%‐33.4%) in Illinois, and the interquartile range (IQR) was 30.8% (Montana; 95% CI: 29.7%‐32.0%) to 36.2% (Missouri; 95% CI: 35.3%‐37.0%). The predicted prevalence of hypertension was significantly higher than the median in most Southern and Eastern states (Maine, Rhode Island, Pennsylvania, Ohio, Indiana, Mississippi, Virginia, Maryland, Louisiana, Alabama, West Virginia, Tennessee, Kentucky, South Carolina, Arkansas, Oklahoma, North Carolina, Georgia, Delaware, Mississippi, Florida, and Missouri; Figure 1A and Table S1; P < 0.05). The predicted prevalence of hypertension was significantly lower than the median in most of the western states (Utah, Colorado, Alaska, California, Idaho, Wyoming, Washington, Nevada, Arizona, New Mexico, Montana, and Oregon) (Figure 1A and Table S1, P < 0.05). The predicted prevalence was also significantly lower than the median in Massachusetts, New Hampshire, Vermont, Minnesota, Nebraska, New York, Texas, and DC.
Figure 1.
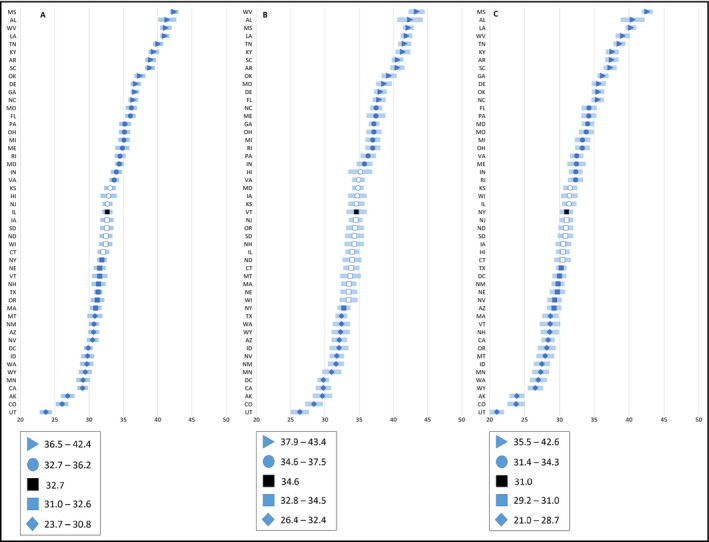
Model‐predicted prevalence of hypertension among adults (≥20 y) by state and sex—BRFSS 2013/2015. Diamonds represent the first quartile (Q1). Squares indicate the second quartile (Q2). Circles indicate the 3rd quartile (Q3). Triangles indicate the 4th quartile (Q4). Black square indicates the median prevalence of all states. Solid (blue)‐filled shapes are significantly different from the median of all states, while white shapes are not significantly (P‐value <0.05). Panel A, All adults (≥20; Q1 range: 23.7‐30.8; Q2 range: 31.0‐32.6; Q3 range: 32.7‐36.2; Q4 range: 36.5‐42.4). Panel B, Men (Q1 range: 26.4‐32.4; Q2 range: 32.8‐34.5; Q3 range: 34.6‐37.5; Q4 range: 37.9‐43.4). Panel C, Women (Q1 range: 21.0‐28.7; Q2 range: 29.2‐31.0; Q3 range: 31.4‐34.3; Q4 range: 35.5‐42.6). BRFSS, Behavioral Risk Factor Surveillance System
The predicted prevalence of hypertension among men ranged from 26.4% (95% CI: 25.0%‐27.7%) in Utah to 43.4% (95% CI: 42.2%‐44.6%) in West Virginia, while among women, it ranged from 21.0% (95% CI: 20.0%‐22.1%) in Utah to 42.6% (95% CI: 41.8%‐43.4%) in Mississippi. The predicted prevalence of hypertension was higher among men than women in all states except Mississippi and DC. The median predicted prevalence among men and women was 34.6% (Vermont; 95% CI: 33.1%‐36.1%) and 31.0% (New York; 95% CI: 30.1%‐32.0%), respectively. The IQR of predicted prevalence among men was 32.4% (Texas; 95% CI: 31.6%‐33.3%) to 37.5% (Maine; 36.1%‐38.9%), and the IQR among women was 28.7% (Massachusetts; 95% CI: 27.5%‐29.9%) to 34.3% (Florida; 95% CI: 33.2%‐35.4%). The predicted prevalence of hypertension showed strong geographic patterns, with highest burden localized to southern states and lowest burden localized to western states for each sex as well as for all adults (Figure 2).
Figure 2.
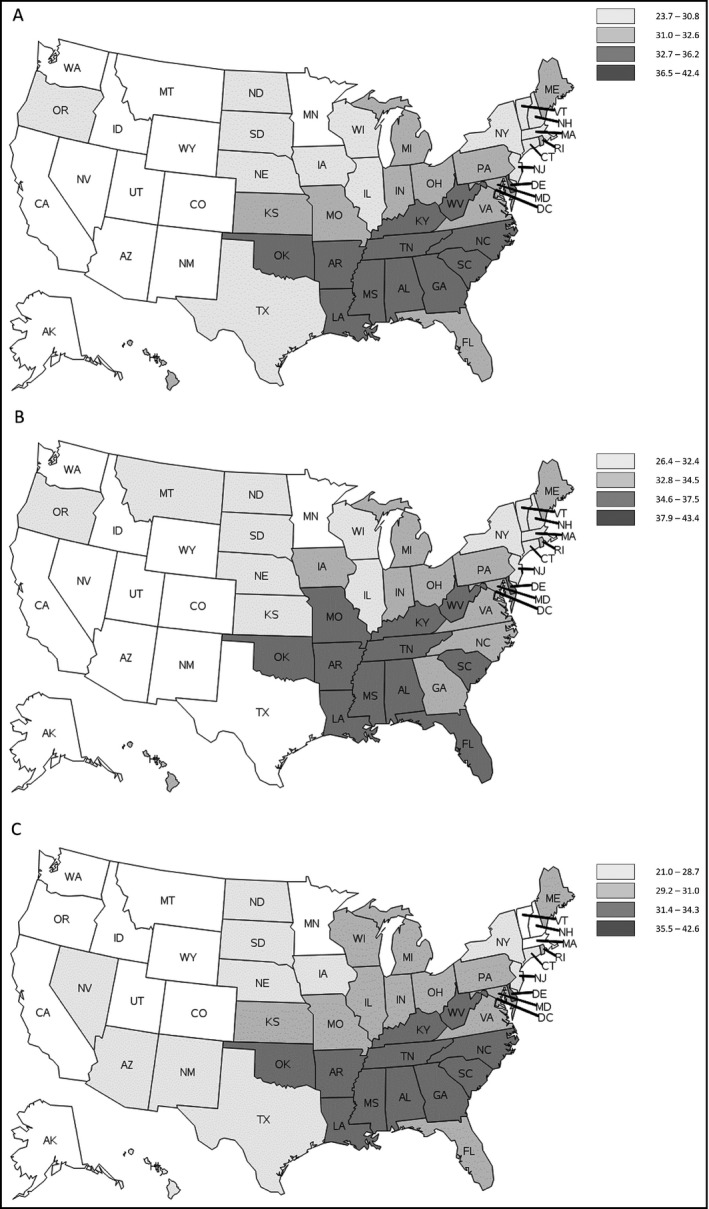
Map of model‐predicted prevalence of hypertension among adults (≥20 y) by sex —BRFSS 2013/2015. BRFSS, Behavioral Risk Factor Surveillance System. AK, Alaska; AL, Alabama; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT,,Connecticut; DC, District of Columbia; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming. Panel A, All adults (≥20). Panel B, Men. Panel C, Women
3.2. Undiagnosed hypertension
The predicted prevalence of undiagnosed hypertension ranged from 4.1% (95% CI: 3.4%‐4.8%) in Kentucky to 6.5% (95% CI: 5.5%‐7.5%) in Hawaii (Figure 3A and Table S2). The median predicted prevalence of undiagnosed hypertension was 5.0% (Arizona; 95% CI: 4.4%‐5.7%), and the IQR was 4.7% (Georgia; 95% CI: 4.1%‐5.3%) to 5.2% (Missouri; 95% CI: 4.4%‐6.0%). The median predicted prevalence was 6.0% (Arizona; 95% CI: 5.2%‐6.9%) among men and 4.1% (Michigan; 95% CI: 3.1%‐5.0%) among women. The predicted prevalence of undiagnosed hypertension ranged from 5.0% in Kentucky (95% CI: 4.0%‐5.9%) to 8.3% in Hawaii (95% CI: 6.9%‐9.7%) among men and from 3.3% in Kentucky (95% CI: 2.5% to 4.1%) to 4.8% in Vermont (95% CI: 3.4% to 6.1%) among women. The IQR of predicted prevalence was 5.8% (South Carolina; 95% CI: 5.0%‐6.6%) to 6.2% (Virginia; 95% CI: 5.4%‐7.1%) among men and 3.7% (DC; 95% CI: 2.8%‐4.6%) to 4.2% (Washington; 95% CI: 3.2%‐5.2%) among women (Figure 3B,C and Table S2).
Figure 3.
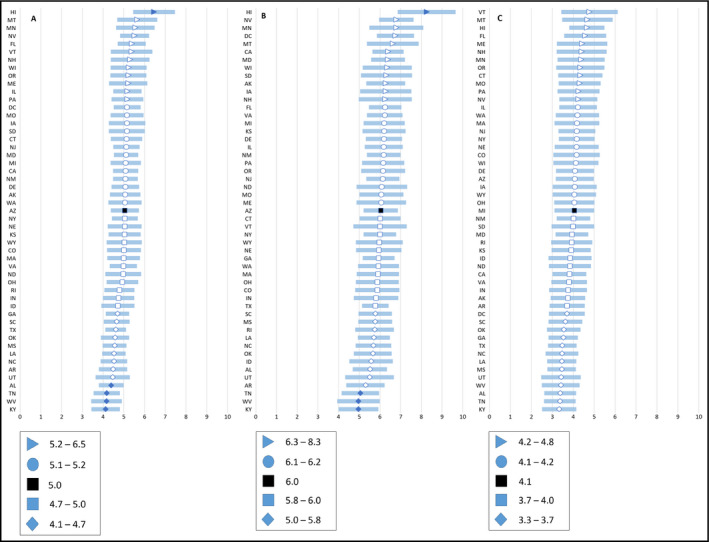
Model‐predicted prevalence of undiagnosed hypertension among adults (≥20 y) by state and sex—BRFSS 2013/2015. Diamonds represent the first quartile (Q1). Squares indicate the second quartile (Q2). Circles indicate the 3rd quartile (Q3). Triangles indicate the 4th quartile (Q4). Black square indicates the median prevalence of all states. Solid (blue)‐filled shapes are significantly different from the median of all states, while white shapes are not significantly (P‐value <0.05). Panel A, All adults (≥20; Q1 range: 4.1‐4.7; Q2 range: 4.7‐5.0; Q3 range: 5.1‐5.2; Q4 range: 5.2‐6.5). Panel B, Men (Q1 range: 5.0‐5.8; Q2 range: 5.8‐6.0;Q3 range: 6.1‐6.2; Q4 range: 6.3‐8.3). Panel C, Women (Q1 range: 3.3‐3.7; Q2 range: 3.7‐4.0; Q3 range: 4.1‐4.2; Q4 range: 4.2‐4.8). BRFSS, Behavioral Risk Factor Surveillance System
The predicted prevalence of undiagnosed hypertension was higher among men than women in all states and DC. Geographic patterns in the predicted prevalence of undiagnosed hypertension were evident, but less pronounced than with the predicted prevalence of hypertension. The predicted prevalence in northern states tended to be higher and the predicted prevalence in southern states tended to be lower than the median among all adults, men, and women (Figure 4). States having higher hypertension predicted prevalence tended to have lower undiagnosed hypertension predicted prevalence, while states having lower hypertension predicted prevalence tended to have higher undiagnosed hypertension predicted prevalence. Among all adults, only in Hawaii was the predicted prevalence significantly higher than the median (5.0% in Arizona). In Alabama, Tennessee, Kentucky, and West Virginia, the predicted prevalence was significantly lower than the median (Arizona; Figure 3A and Table S2). Among men, only one state (Hawaii) had significantly higher predicted prevalence than the median (Arizona) and three states (Tennessee, West Virginia, and Kentucky) had significantly lower predicted prevalence. Among women, none of the states had significantly higher predicted prevalence than the median 4.1% in Michigan and none of the states had significantly lower predicted prevalence than the median (Figure 3B,C and Table S2).
Figure 4.
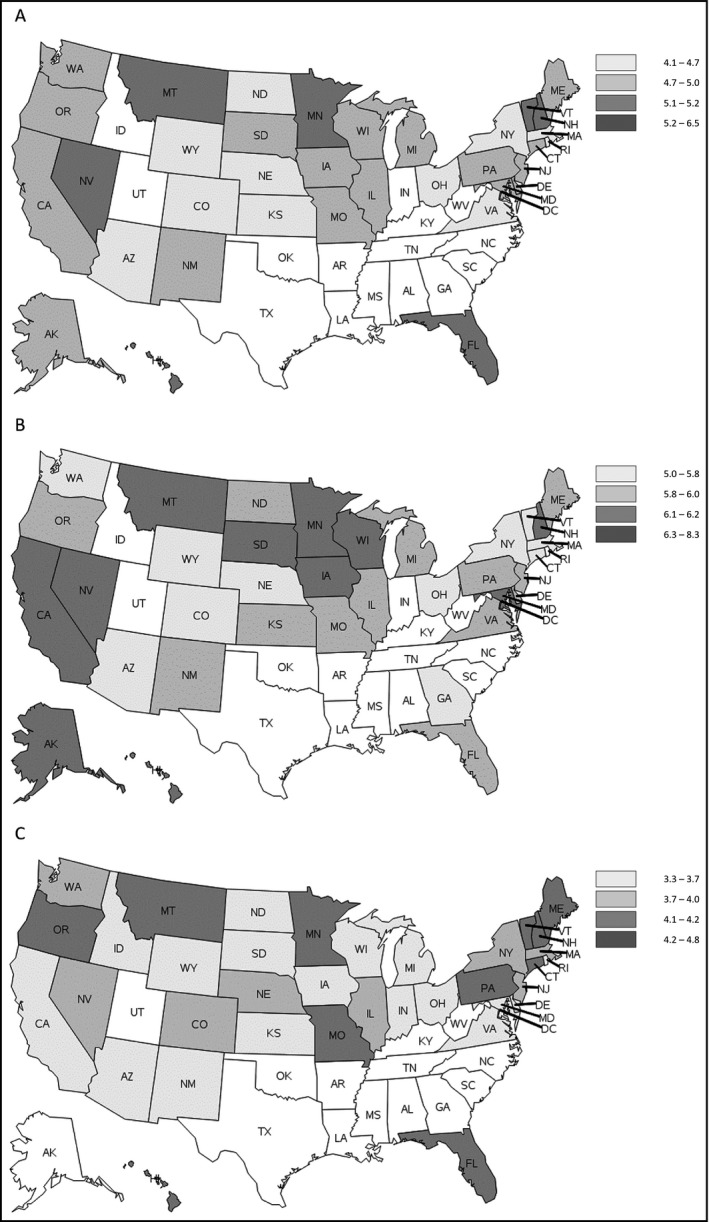
Map of model‐predicted prevalence of undiagnosed hypertension among adults (≥20 y) by sex—BRFSS 2013/2015. BRFSS, Behavioral Risk Factor Surveillance System. AK, Alaska; AL, Alabama; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT,,Connecticut; DC, District of Columbia; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming. Panel A, All adults (≥20). Panel B, Men. Panel C, Women
4. DISCUSSION
This study examined state‐level prevalence estimates of hypertension and undiagnosed hypertension, building, and expanding on previous studies by estimating the variance of the computed prevalence, which allowed for the calculation of 95% CI's and statistical testing. Geographic patterns and trends in hypertension predicted prevalence were apparent in this study, as reported previously.10, 13 Greater hypertension predicted prevalence was observed in the southern states, which was also noted in a comparable study assessing hypertension at the county‐level.14 While the predicted prevalence of undiagnosed hypertension was lower in the southern states, its geographic patterns were less pronounced. Sex differences were evident, with the predicted prevalence of hypertension and undiagnosed hypertension both generally higher among men than women.
Our methodology differs from previous analyses; in addition to predicting prevalence estimates using a modeling strategy, we also estimated the variance of these estimates, which took into account the sample design of both NHANES and BRFSS surveys, plus the error inherent in the regression models. This additional statistical inference provides CI's as well as point estimates for state‐level prevalence of hypertension and undiagnosed hypertension and allows for statistical comparisons. Variance estimates were calculated using the delete‐one‐jackknife method, which is useful in settings where standard variance estimation techniques are not applicable or difficult to implement. Modeled estimates such as these can guide programs and help identify disparate groups and/or geographic regions, to better focus prevention programs and interventions. This methodology can be used for other diseases or conditions, when performing regression on one complex survey and applying those models to the population from a different complex survey, and subsequently obtaining variance estimates for statistics of interest.
This study has several limitations to be considered. Limitations pertaining to NHANES and BP measurement have been published elsewhere.15 Hypertension and undiagnosed hypertension may be underestimated in NHANES due to the ineligibility of military personnel and those living in institutions, including nursing and assisted living facilities. This study was unable to take into account those who were using lifestyle or dietary approaches to reduce their BP, specially affecting the ability to determine the need for treatment among those with a previous diagnosis of hypertension (ie, aware/untreated).
In addition, the results of this analysis should be interpreted by taking into account the limitations of the statistical methodology and the assumptions made prior to analysis. The wording of some of survey questions and response options differs between NHANES and BRFSS and for survey years. This difference could affect the prevalence estimates. The NHANES questionnaires were administered in‐person, while those for the BRFSS were administered over the telephone and all of the information collected during the BRFSS survey is based on self‐report which is subject to recall bias and nonresponse rates. For example, while height and weight which were used to calculate BMI are measured in the NHANES survey, that information is based on self‐report in BRFSS and could be underestimated. Misreporting of self‐reported height and weight has been reported in previous research, but BMI based on self‐report is highly correlated with BMI based on physical measurements with r = 0.90 to 0.95.16
Moreover, the 2017 ACC/AHA guideline is not applied to this study, because the study used awareness of hypertension to model the prevalence of hypertension and undiagnosed hypertension, which relies on self‐report of health care provider diagnosis which was based on JNC7 guideline.3, 13 The impact of the 2017 ACC/AHA hypertension guideline on this type of analysis can be applied to data collected from 2018 onward.
Further, there are factors associated with the risk and prevalence of hypertension and undiagnosed hypertension which could not be accounted for in the current methodology, specifically heterogeneous probabilities of those conditions across regions within identical socioeconomic and demographic population groups. The methods used in this analysis assume that the probability of having hypertension or undiagnosed hypertension is constant across all states, given the factors used in the regression models. By applying the same models to each state, it is possible to underestimate or overestimate the prevalence, which might exhibit atypical characteristics that are not captured.
Some states with higher hypertension prevalence had lower prevalence of undiagnosed hypertension. From the definitions of predicted prevalence of hypertension and undiagnosed hypertension in the supporting document, the ratio of predicted prevalence of hypertension to predicted prevalence of undiagnosed hypertension becomes number of hypertension over the number of unaware people with hypertension. Therefore, when two states have same predicted prevalence of hypertension but one state has much large unaware population, that state would have higher predicted prevalence of undiagnosed hypertension.
A combination of community and clinical approaches to hypertension will be necessary to improve hypertension control. Public health approaches can be undertaken to reduce the burden of hypertension and uncontrolled hypertension. These approaches should focus on the leading modifiable risk factors for hypertension, including poor diet, high sodium intake, overweight or obesity, and limited physical activity.17 Public health approaches include policy initiatives that focus on environmental and systems changes related to these risk factors. At the clinical level, health information technology (HIT) can be useful for identifying persons with elevated BP who are either undiagnosed or uncontrolled and monitoring them so that their risk factors, including lifestyle risk factors, can be reduced, and beginning medication treatment when necessary.18 Other HIT approaches used strategically, such as registries, clinical decision support, patient reminders, and patient portals, can be effective in improving BP measurement and hypertension control. Team‐based care, recommended by the Community Preventive Services Task Force, is also an effective strategy for improving hypertension control, by promoting improved communication with patients and other health care providers and adherence to evidence‐based guidelines.19, 20, 21 In addition to these approaches, improved self‐management strategies and other innovations in technology, such as BP self‐monitoring and telemonitoring, can play an important role in achieving greater hypertension control.22
Improving hypertension control will assist with meeting the national Healthy People 2020 objectives of reducing the proportion of adults with hypertension by 10% (HDS‐5.1) and increasing the proportion of adults with hypertension whose BP is under control to 61.2% (HDS‐12).23 The improvement in hypertension control has been identified as a priority within Healthy People and has been selected as the only Healthy People 2020 Heart Disease and Stroke Leading Health Indicator (LHI). The distinction of hypertension control as a LHI highlights the importance of the factor in the overall prevention, treatment, and control of cardiovascular disease. Healthy People 2020 also provides evidence‐based resources to address and improve hypertension control (https://www.healthypeople.gov/topicsobjectives2020/ebr.aspx?topicId=2121).
Other national efforts are also targeting improvements in hypertension prevention, treatment, and control. The Million Hearts® initiative, co‐led by CDC and the Centers for Medicare and Medicaid Services, is focusing efforts on preventing 1 million or more heart attacks and strokes in the United States by 2022.24 Million Hearts® seeks to improve the cardiovascular health of the nation by focusing on priority areas in the community (reducing sodium intake, decreasing tobacco use, increasing physical activity) and in the clinical environments (improving the ABCS [appropriate aspirin use for those at risk, BP control, cholesterol management, and smoking cessation], increasing cardiac rehabilitation use, engaging patients in heart‐healthy behaviors). Diverse, yet targeted, activities in the community and clinical environments, supported and implemented using evidenced‐based interventions and engaged partners, will be needed to improve the management of hypertension and reduced long‐term risk of cardiovascular disease.
5. DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
CONFLICT OF INTEREST
The authors report no conflict of interests.
Supporting information
Park S, Gillespie C, Baumgardner J, et al. Modeled state‐level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013‐2015. J Clin Hypertens. 2018;20:1395–1410. 10.1111/jch.13388
Notes
For more information about Healthy People 2020, see: https://www.healthypeople.gov/.
For more information about Million Hearts, see: https://millionhearts.hhs.gov/index.html.
For more information about NHANES, see: https://www.cdc.gov/nchs/nhanes/index.htm.
For more information about BRFSS, see: https://www.cdc.gov/brfss/.
REFERENCE
- 1. Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS data brief, no 220. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 2. Merai R, Siegel C, Rakotz M, et al. CDC grand rounds: a public health approach to detect and control hypertension. MMWR Morb Mortal Wkly Rep. 2016;65:1261‐1264. [DOI] [PubMed] [Google Scholar]
- 3. Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71(2):109‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics‐2017 update: A REPORT FROM the American Heart Association. Circulation. 2017;135(10):e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. JACC. 2012;60(7):599‐606. [DOI] [PubMed] [Google Scholar]
- 6. Zohoori N, Pulley L, Jones C, Senner J, Shoob H, Merritt RK. Conducting a statewide health examination survey: the Arkansas cardiovascular health examination survey (ARCHES). Prev Chronic Dis. 2011;8(3):A67. [PMC free article] [PubMed] [Google Scholar]
- 7. Thorpe LE, Gwynn RC, Mandel‐Ricci J, et al. Study design and participation rates of the New York City health and nutrition examination survey, 2004. Prev Chronic Dis. 2006;3(3):A94. [PMC free article] [PubMed] [Google Scholar]
- 8. Van Eenwyk J, Bensley L, Ossiander EM, Krueger K. Comparison of examination‐based and self‐reported risk factors for cardiovascular disease, Washington state, 2006–2007. Prev Chronic Dis. 2012;9:E117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43(1):87‐91. [DOI] [PubMed] [Google Scholar]
- 10. Ezzati M, Oza S, Danaei G, Murray CJ. Trends and cardiovascular mortality effects of state‐level blood pressure and uncontrolled hypertension in the united states. Circulation. 2008;117(7):905‐914. [DOI] [PubMed] [Google Scholar]
- 11. Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in united states counties, 2001–2009. PloS one. 2013;8(4):e60308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all‐cause and cvd mortality among us adults. JAMA. 2012;307(12):1273‐1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Howard G, Prineas R, Moy C, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: The reasons for geographic and racial differences in stroke study. Stroke. 2006;37(5):1171‐1178. [DOI] [PubMed] [Google Scholar]
- 14. Loop M, Howard G, Campos G, et al. Heat maps of hypertension, diabetes, and smoking in the continental US. Circ Cardiovasc Qual Outcomes. 2017;10(1):e003350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention . Vital signs: Awareness and treatment of uncontrolled hypertension among adults–united states, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61(35):703‐709. [PubMed] [Google Scholar]
- 16. McAdams MA, Dam R, Hu FB. Comparison of self‐reported and measured BMI as correlates of disease markers in U.S. adults. Obesity. 2007;15(1):188‐196. [DOI] [PubMed] [Google Scholar]
- 17. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Hypertension. 2003;289(19):2560‐2572. [DOI] [PubMed] [Google Scholar]
- 18. Suarez C, Galgo A, Mantilla T, Leal M, Escobar C. Variables associated with change in blood pressure control status after 1‐year follow up in primary care: A retrospective analysis: the TAPAS study. Eur J Prev Cardiol. 2014;21(1):12‐20. [DOI] [PubMed] [Google Scholar]
- 19. Guide to community preventive services. Cardiovascular disease prevention and control: Team‐based care to improve blood pressure; 2012.
- 20. Community Preventive Services Task Force . Team‐based care to improve blood pressure control: Recommendation of the community preventive services task force. Am J Prev Med. 2014;47(1):100‐102. [DOI] [PubMed] [Google Scholar]
- 21. Proia KK, Thota AB, Njie GJ, et al. Team‐based care and improved blood pressure control: A community guide systematic review. Am J Prev Med. 2014;47(1):86‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Logan AG. Transforming hypertension management using mobile health technology for telemonitoring and self‐care support. Can J Cardiol. 2013;29(5):579‐585. [DOI] [PubMed] [Google Scholar]
- 23. US Department of Health and Human Services . Healthy people 2020: heart disease and stroke; 2013.
- 24. Frieden TR, Berwick DM. The "million hearts" initiative–preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


