Abstract
Introduction
Intervention in the preschool period is currently recommended for autism spectrum disorder. Therapies delivered by parents are particularly suitable for young children. Preschool Autism Communication Trial (PACT) is a parent-mediated therapy that has shown a significant and sustained impact on autism symptom reduction. However, access to such evidence-based therapies for families is limited due to autism centres located in large urban areas. Using videoconferencing to deliver PACT training to parents may improve accessibility for families living in underserved areas.
Methods and analysis
This single-blind randomised controlled trial, involving six sites in France, will investigate the efficacy of a telehealth, videoconferencing-based, parent-mediated PACT therapy on autism symptoms, over a 12-month period. It will compare PACT plus treatment as usual (TAU) against TAU only in a cohort of 238 toddlers (119 per group) aged 18–36 months at inclusion and living with their families more than 40 min away from the specialist centres for autism. Primary outcome will include change of overall autism score on the Autism Diagnostic Observation Scale (ADOS) at 12 months. Secondary outcomes will measure change in child skills, child functioning, impact on parents (stress, health, priorities) and implementation characteristics. Repeated measures analyses will be used to test the effect of PACT intervention on the overall ADOS module 1 score over the 12-month study period. Linear mixed models will be used with time, treatment allocation and the interaction between treatment and time as fixed effects and individual variation as random effect.
Ethics and dissemination
This protocol (V.5, date: 25 October 2019) is approved by the French National Review Board (reference no 2018-A02516-49). The results will be disseminated via peer-reviewed journals
Trial registration number
Keywords: telemedicine, human resource management, organisation of health services, developmental neurology & neurodisability, child & adolescent psychiatry, medical education & training
Strengths and limitations of this study.
Large multicentre randomised controlled trial in children with autism spectrum disorder under 3 years old, testing remote delivery of an evidenced intervention.
Assessment partially done by videoconferencing and based on video material sent by parents.
Recruitment targeted to children living in underserved areas.
Short-term effect of the intervention will be assessed at 12 months (end of the intervention).
Owing to the nature of the intervention, parents of the children and Preschool Autism Communication Trial therapists will not be blind to the allocation group.
Introduction
Rationale and background
Autism spectrum disorder (ASD) is a common neurodevelopmental disorder with a population prevalence of at least 1.5% in developed countries and can cause significant lifelong disability1–3 and burden for families and caregivers.4 Diagnosis is possible as early as 18 months of age.5 Current evidence suggests that interventions delivered in the early developmental period before the age of 3 years has the potential for maximal impact on autism symptom severity.
Therapies can be delivered by therapists, teachers and parents.6 For preschool children with ASD, parent-mediated therapies can guide parents to face challenging social interaction with their children.7 8 Among the different parent-mediated therapies, Preschool Autism Communication Trial (PACT) has shown significant short and long-term efficacy on objectively assessed autism symptoms in children aged from 2 to 10 years in a large UK cohort (N=152); as showed in a recent systematic review9 and meta-analysis.10 In PACT, parents are guided by a therapist via video feedback to optimise parent–child dyadic interaction, which in turn impacts on child language, communication and autism symptoms.11 In a trial of PACT intervention compared with regular care, PACT showed a statistically significant effect at 13-month endpoint to reduce of autism symptom severity measured on Autism diagnostic Observation Schedule version 2 (ADOS-2) (effect size 0.64; 95% CI 0.07 to 1.20); and an increase in parental communication synchrony with the child and child communication initiations with the parent.12 The follow-up study showed evidence of sustained effect on autism symptom severity 6 years after intervention end, with a significant overall reduction in symptom severity over the course of trial and follow-up period (effect size=0.55, 95% CI 0.14 to 0.91, p=0·004).13 A mechanistic study also confirmed that the distal effect of PACT therapy on autism severity measured by ADOS was mediated by the improvement of child communication initiations, which in turn was mediated by improved parent–child synchrony.14
Availability of PACT therapy is limited; even more so in rural settings or in regions away from specialist centres. Using videoconferencing run by therapists to train parents in PACT may, therefore, be a viable alternative to make such therapies available to families living far from autism centres. Previous studies have shown that it is possible to provide parent-mediated therapies in autism by videoconferencing successfully.15 16 The team who developed the PACT therapy reported positive experiences of parent guidance by videoconferencing (C. Aldred and J. Green, personal communication, June 10, 2020). Indeed, videoconferencing was used to deliver some of the PACT sessions in a recently published randomised controlled trial (RCT).17 However, PACT has never been evaluated when exclusively delivered by videoconferencing. The barriers and facilitators to delivering such therapies via videoconferencing are not sufficiently well understood, and hence it is essential to investigate and address them adequately.18 19
Research question: The proposed protocol is for a large RCT in children under 3 years with ASD to evaluate the effectiveness on autistic symptom severity and other measures of PACT therapy delivered to parents by videoconferencing.
A significant effect would justify and facilitate the routine use of videoconferencing therapy in early intervention and improve the dissemination of this evidence-based practice.
The hypothesis is that PACT intervention delivered by videoconferencing+treatment as usual (TAU) will have a superior efficacy on child autism symptom severity as compared with TAU alone.
Objectives
Our primary objective will be to test the efficacy of a parent-mediated PACT therapy, delivered by trained therapists to parents living in underserved areas via videoconferencing over a 12-month period, on overall autistic symptoms in children with ASD aged from 18 to 36 months at inclusion, measured using the ADOS-2,
Our secondary objectives will include an evaluation of change in child sociocommunicative interactions, language, communication initiation and daily adaptive behaviour. At the parent level, we will evaluate the intervention effects on stress, health and family functioning.
The implementation of the therapy will be evaluated through the adherence of professionals and parents to PACT, and acceptability and feasibility of the PACT sessions to parents and therapists.
Method
Study design
This is a prospective multicentre RCT with two parallel group, 1:1 ratio, single-blind comparing PACT intervention+TAU against TAU alone. Evaluation will be carried out using quantitative and qualitative mixed-method approaches.20 21
Semistructured interviews with parents and therapists will be conducted to understand the barriers and facilitators of using the videoconferencing approaches to delivering the PACT therapy.
Figure 1 shows Consolidated Standards of Reporting Trials (CONSORT) flow chart of the study.
Figure 1.
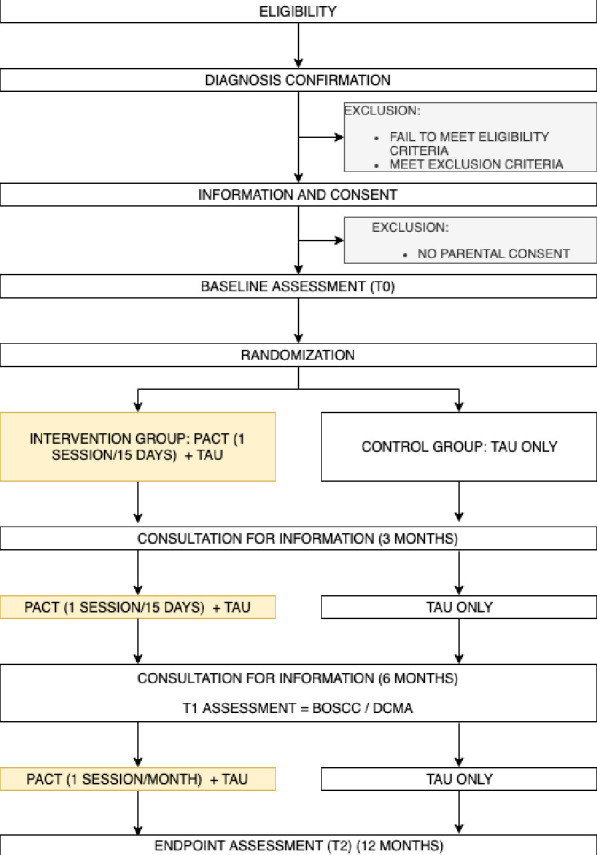
CONSORT flow chart of the study. BOSCC, Brief Observation of Social Communication Change; CONSORT, Consolidated Standards of Reporting Trials; DCMA, Dyadic Communication Measure for Autism; PACT, Preschool Autism Communication Trial; TAU, treatment as usual.
Setting
We will run this trial in six academic centres located in child and adolescent public hospitals in France. All centres have a unit for ASD diagnosis and assessment and a distinct unit for intervention where therapists have been trained in PACT and can provide PACT via videoconferencing. The parents receiving intervention come from a French-speaking population including socioeconomically disadvantaged groups.
Patient and public involvement
Alloisio (Association AAA https://autisme-ambitionavenir.com) and Belkhayat (association https://bleunetwork.fr/pro) are parents of a child with autism and represent two different association. They are part of the steering committee.
Population
Inclusion criteria
Children will be included if they meet the following criteria: (1) aged between 18 and 36 months old at referral, (2) meet criteria for ASD using the two gold-standard instruments ADOS-2 and ADI-R (Autism Diagnostic Interview-Revised). For inclusion into the study, the severity score comparison (CSS) on ADOS-2 will be greater or equal to 4. The score on the ADI-R algorithm for toddlers will be greater or equal to 11.22 The diagnosis will be confirmed by a multidisciplinary team trained in ASD assessment and diagnoses based in the academic departments of the hospitals, (3) have a non-verbal age equal to or above 12 months on the Mullen Scale of Early learning (MSEL) and23 (4) live more than 40 min away from a Centre for Resources in Autism (regional centre)
Referred parents will be included if they meet the following criteria: (1) speak French with their children (2) are able to use videoconferencing methods with therapists who will be based at the centre (assessed through the conduct of the Vineland Assessment Behavioural Scale by videoconferencing) (see online supplemental appendix 1)
bmjopen-2020-044669supp001.pdf (159.5KB, pdf)
Exclusion criteria
Exclusion criteria for the child will include:
A twin brother or sister with ASD or a brother or sister already included in the study.
Diagnosed with epilepsy requiring medication.
Severe hearing or visual impairment.
An identification of a genetic anomaly which may impact on their ability to participate in the intervention or on data validity (determined by the principal investigator on a case-by-case basis).
Exclusion criteria for the referred parents (at least one parent with) will include:
Severe hearing or visual impairment.
Severe psychiatric disorder.
Unstable somatic disorders preventing participation in the intervention.
Lack of internet provision.
Not available for regular intervention and follow-up.
Opposition of one parent to the child’s participation in the study.
Currently undertaking PACT therapy.
Intervention conducted in the experimental group
Eligibility criteria for PACT therapist and adherence
Therapists delivering the intervention will include speech language pathologist (SLP), occupational therapists, clinical nurses, psychologists or child and adolescent psychiatrists, all specialised in ASD. The therapists have already received formal training and supervision in PACT from the team who developed this training.12 24 Fidelity to PACT therapy will be maintained by regular meetings between therapists of all centres, with scoring and feedback of videotaped therapy sessions obtained during the study.
PACT treatment principles
As previously described,17 parents will be trained, via videofeedback, to identify and set key strategies facilitating the sociocommunicative interactions between their child and themselves. Parents will also be encouraged to use PACT every day outside the training session at least half an hour a day. The therapy follows a six-staged approach based on child developmental progression and strategies for establishing fundamental skills for the sociocommunicative development. The first two stages aim to increase parent’s identification of child focus and interest, synchrony, responsiveness and sensitivity to the child interest and communication. The third and fourth stages are targeted towards developing expression and comprehension of the child by commenting and modelling language adapted to the child’s developmental level. Child communication initiation is also improved in the fifth stage through different strategies such as anticipation and routine. The last stage aims to develop conversation and expansion of language for verbal children. Progression from one stage to the next depends on predefined criteria.
Based on the protocol of the first PACT RCT, parents will receive 18 sessions of training in PACT with the therapist over the 12 months12 13: 1-hour session every fortnight for the first 6 months to learn PACT strategies followed by 1-hour session per month over the next 6 months to maintain the capacity of parents to deliver the strategies.
Therapist will train only one parent per family and maintain fidelity to the therapy manual. The ‘referent parent’ will have to be designated before the randomisation of the child. If the referent becomes unavailable, the therapy will stop or will continue with the other parent if possible and this change will be reported.
Parent training session with the professional via videoconferencing
Before each session, the parent will be asked to send a 10 min video of their interaction with their child to the therapist via a secure cloud link. During the videoconferencing session (as in face-to-face intervention), referent parent will begin with a 5 min discussion about their progress since the last session. The therapist will then share his/her screen and watch the home-based 10 min video together with the parent. Together the parent and therapist will identify, review and discuss specific clips that demonstrate accomplishment of therapy goals for the relevant stage of the PACT programme. The therapist’s role will be to guide parents to identify successful strategies and responses (ie, episodes of engagement and/or mutual sharing with their child). Parents will be supported to reflect on their role in enhancing interaction and to identify new intervention goals.
Parent PACT implementation in daily life outside the therapy session
At the end of each session, the therapist will support the parent in setting 2–3 new goals, based on the strategies identified during the session. The therapist will encourage the parent to practice the strategies for the next session and discuss opportunities to achieve these goals in daily routine at home for at least 30 min per day. Parents will be guided to embed PACT strategies in everyday routines across different contexts. As therapy progresses, parents will be asked to send 10 min home videos of daily routines in different contexts.
TAU and two follow-up consultations on ASD and its management
Regardless of group allocation, parents will receive TAU consisting of psychoeducation about ASD, management and educational support for nursery and preschool placement. Parents will be referred to any relevant care available in the community (eg, SLP, occupational therapist, educator, behavioural psychologist, psychiatrist). TAU received during the course of the study will be described in both groups.
Regardless of group allocation, a psychiatrist or a psychologist from each autism centre will provide two supplementary 45 min follow-up consultations conducted by videoconferencing at 3 and 6 months after inclusion. This consultation will be carried out by following an interview guide. Three thematic areas will be systematically discussed with the parents: ASD information, access to treatment in the community, support for school or nursery. These follow-up consultations will ensure that parents of both groups receive homogeneous information on ASD and its management.
Avoidance of contamination
Currently, PACT is not widely implemented in the community in France, particularly in the rural areas. Any families who are currently in receipt of PACT intervention will be excluded from this trial. However, any PACT that might be received in the community as part of TAU will be recorded.25
Research assessors will be separate to the therapists and will be located and supervised separately in each centre.
Professionals conducting the follow-up consultations will not be trained in PACT therapy or be part of the research assessments.
Measures
Primary outcome
To assess autism severity
ADOS-2 is a semistructured, researcher–child interaction based, standardised observational assessment, in communication, play, imaginative skills and repetitive behaviours.26 27 It is a widely used scale in the field of ASD research with good psychometric properties, recommended for the diagnosis of ASD and assessment of core autistic symptoms.28
At baseline and follow-up assessment after 12 months, we will use only ADOS-2 module 1, for children who are 18 months of age and older children who use no or few words.
There is a good inter-rater reliability for module 1.27 Internal consistency Cronbach’s alpha coefficients was high in original study.27 This scale has also shown that it can measure change in autism severity.13 28
ADOS-2 is composed of different items scored 0–3 or 0–2. Item A1 codes the level of language, from the severity for ‘the child is using regular use of statements with two or more words’ (code 0) to ‘the child has no spontaneous use of approximate words or words’ (code 4). For children with no or limited language (A1 the two items measuring language in the algorithm (item A3 speech abnormalities, item A5 stereotyped language) will be scored 3 (worst value) (see reference 12). The minimum overall ADOS-2 module 1 raw score will be 0 and the maximum score 42. A higher score means more autistic symptoms.
Our primary outcome will be the change between baseline and 12 months in the overall raw score in reciprocal sociocommunicative interactions and repetitive and restrictive behaviours in line with the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, fifth version).26 29
Researchers will be trained to achieve recognised standards. Regular reliability meetings of all researchers will address any discrepant ratings to maintain researcher calibration.
Secondary outcomes
To assess social communication and interaction in the natural setting of parent–child interaction at home:
Brief Observation of Social Communication Change (BOSCC).30
To assess dyadic communication in the natural setting of parent-child interaction at home:
Dyadic Communication Measure for Autism (DCMA).24
To assess child cognitive development:
Mullen Scale of Early Learning (MSEL).23
To assess child language development:
Development of Expressive Language, (Développement du Langage de Production en Français, DLPF).31
To assess adaptative behaviour of the child:
Vineland Adaptive Behaviour Scales second version (VABS-2).32
To assess Parent’s Stress, health, priorities and experience of the family:
Autism Family Experience Questionnaire (AFEQ).33
Parental Stress Index (PSI).34
General Health Questionnaire35
To assess implementation of the intervention:
PACT Fidelity Rating Scale.
Number of PACT training sessions undertaken.
Quality of videoconferencing during each session.
Parent’s acceptability of videoconferencing and implementation of PACT at home (self-report on Likert-scale).
Number of hours per day using PACT at home at 12 months.
Parent’s qualitative PACT adherence coded with DCMA on a 12 min home child–parent interaction video.
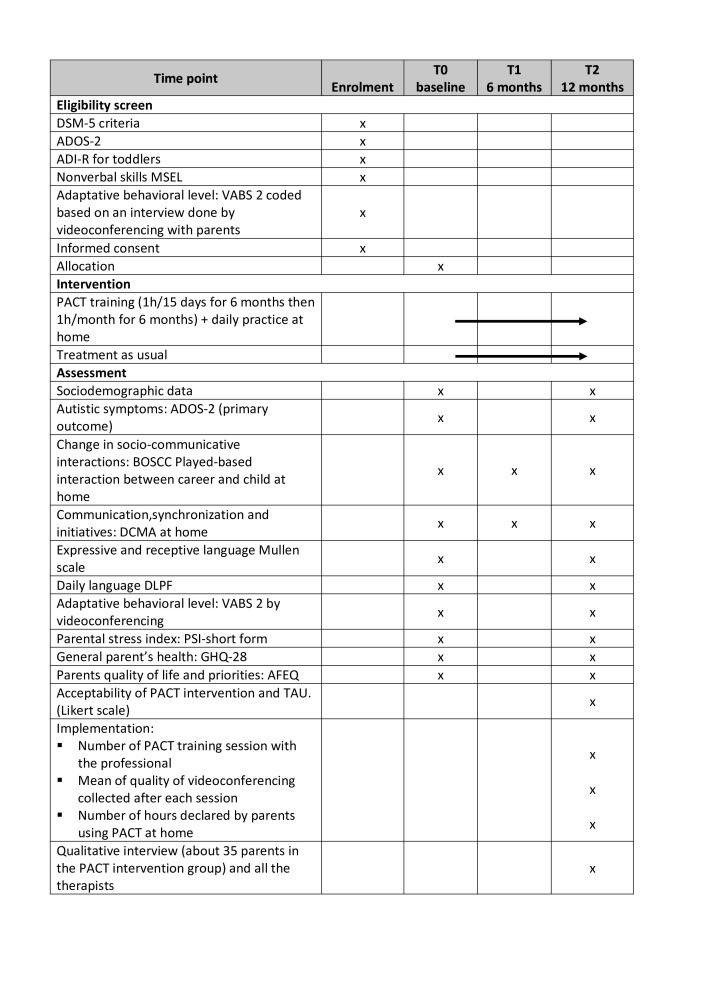
Figure 2 shows schedule of enrolment, interventions and assessments. Online supplemental appendix 1 shows more detailed about assessment.
Figure 2.
Schedule of enrolment, interventions and assessments (SPIRIT). ADI-R, Autism Diagnostic Interview-Revised; ADOS-2, Autism Diagnostic Observation Scale-2; AFEQ, Autism Family Experience Questionnaire; BOSCC, Brief Observation of Social Communication Change; DCMA, Dyadic Communication Measure for Autism; DLPF, Développement du langage de Production en Français; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth version; GHQ, General Health Questionnaire; PACT, Preschool Autism Communication Trial; PSI, Parental Stress Index; SPIRIT, Standard Protocol Items: Recommendations for Interventional Trials; TAU, treatment as usual; VABS, Vineland Adaptive Behaviour Scale.
Participant’s timeline
Toddlers with a suspected ASD will be approached by health professionals with information about this study. The research recruitment team will meet with the family, complete the ADI-R during the first meeting, and confirm eligibility criteria. Complementary assessments, including ADOS, MSEL with the child and Vineland will be conducted by videoconferencing with the parent, to assess the criteria for eligibility. If toddlers and families meet the criteria for participation, parents will be informed about the study and possibility of an intervention using PACT or TAU based on randomisation. A written informed consent will be obtained if the parent/family agrees to participate in the study after 1 week of reflection (see consent form in online supplemental appendix 2).
bmjopen-2020-044669supp002.pdf (133.6KB, pdf)
The ‘referent parent’ used to refer to the parents who will engage with the PACT therapy will be decided before randomisation. Children will be subsequently randomised into the intervention or TAU group. Parents will be informed of the result of the randomisation
Assignment of intervention
Allocation sequence generation and randomisation
All eligible toddlers, with parental consent, will be assigned to the two study groups in a 1:1 ratio using the minimisation method with the following stratification factors: the centre, the children’s age, level of language (according to the ADOS2 scale) and gender. To ensure allocation concealment, a minimisation algorithm with a 0.90 random element will be used and known only to the statistician (AD). The randomisation will be centralised.
Blinding
Owing to the nature of the intervention, parents and PACT therapists cannot be blind to the allocation group. PACT therapists will not be involved in ASD assessment and diagnosis. An assessor blind to the allocation group will administer every assessment. Data manager and biostatistician will be blinded to the allocation groups.
Data collection and management
Data collection
Data will be collected through standardised observations, parental questionnaires and interviews carried out by a researcher blind to the allocation. We will be particularly vigilant about the measurement accuracy of the first criterion of judgement as described in the paragraph on ADOS-2.
Participation retention and follow-up
Children of both groups will benefit from early diagnosis and assessment and will have the same follow-up evaluations over the 1-year study period in the respective study centres Any discontinuation of study participation will be collected and recorded with the reasons.
Data management
The study data will be collected on a secure electronic case report form (eCRF) that will be available at each centre through an internet portal. No personal identifying information will be mentioned on the eCRF. Each subject included in the study will be assigned a unique identification number.
All study data will be stored securely in the Academic Hospital of Lyon. All electronic data will be secured on a password-protected laptop. Paper-based study documents will be stored in a secure filing cabinet at each centre. Access to these files will be limited to research staff involved in the study.
The eCRF will only include the data necessary for the analysis to be reported in a scientific publication.
Statistical analysis
Simple size calculation
On the basis of the findings of the PACT Trial,12 we have powered the study to be able to detect a difference in overall change on the ADOS score of 2 points. The group difference in mean change between baseline and month 12 was −1 point for ADOS social affect score (mean change=2.9, SD=3.9 in TAU group and mean change=−3.9, SD=4.7 in PACT+TAU group) and −0.5 points for ADOS restricted and repetitive behaviours score (mean change=2.9, SD=3.9 in TAU group and mean change=−3.9, SD=4.7 in PACT+TAU group). The premeasure and postmeasure were correlated at 0.67. Therefore, the most conservative values were fixed for ADOS SD and for correlation among the repeated measures from a single participant. A target of 238 subjects (119 subjects per treatment arm) was planned to be randomised in the trial. Assuming a two-point difference in favour of the PACT+TAU compared with TAU, an SD of 5, a correlation between subsequent visits of 0.5, a drop-out rate of 20% and a two-sided significance level of 0.05, the planned sample size would provide about 80% power for the study.
Feasibility of recruitment
A strong partnership with ASD orientation platforms recently implemented in France, a broad communication (meeting, mail, flyers) to healthcare professionals (Speech pathologist, Occupational therapist, therapist, paediatrician, general practitioner) family associations and other stakeholders will allow the trial team to reach the sample size within 2 years.
Statistical analysis
A full statistical analysis plan will be finalised prior to database lock. Statistical analysis and results will be reported at the 12-month endpoint in accordance with the CONSORT 2010 statement. No interim analysis will be scheduled. All the statistical analysis will be carried out according the intention to treat principle using SAS statistical software (SAS Institute).
Baseline characteristics will be presented in each group.
Summary statistics will be presented for process variables (number of PACT sessions, quality of videoconferencing per session, acceptability and satisfaction of PACT intervention, number of hours declared to be realised with the child) to show the feasibility and acceptability of PACT implementation in the intervention group.
The pattern of missing data will be investigated (number and mechanism of missingness). Missing data strategies can be applied, and sensitivity analysis of different strategies (simple or multiple imputation) will be conducted.
A repeated measures analyses will be used to test the effect of PACT intervention on overall ADOS module 1 score over the 12-month study period. A linear mixed model will be run with the overall ADOS score as the dependent variable and including time (baseline, month 12), treatment (TAU or TAU+PACT) and the interaction between treatment and time as fixed effects and patient as random effect. Model will be adjusted for stratification factors (centre, age, level of language (item A1 ADOS-2) and gender) and baseline variables that show evidence of treatment group imbalance. Time will be represented by dummy variable. Model assumption will be verified according to residual analysis. If most of the assumptions are not met, other alternatives such as transformation of ADOS overall raw score will be examined. Sensitivity analyses like complete case and per-protocol analysis will be performed to assess the robustness of the results to protocol deviations. In complete-case analysis, only patient with primary outcome documented will be analysed. In per-protocol participants who violate the protocol will be excluded from the analysis.
All the secondary outcomes, (overall total score of the BOSCC, communication initiation and synchrony measured with the DCMA, overall raw score of the MSEL in receptive and expressive language, overall score in expressive language of the DLFP, overall raw score of communicative and social of the VABS, PSI, Parent General Health score, AFEQ score) will be analysed in a similar way using with appropriate linear or generalised linear mixed models. Tobit models will be used to address potential floor effects.
We will finally explore the parent’s and children’s characteristics, moderating the implementation and efficacy of this therapy. We will also test the previously described mediators implicated in the efficacy of this therapy.14
Qualitative analysis of barriers and facilitators of implementation
Based on parents and of the therapist’s reports, we will describe the facilitators and barriers of the implementation of video-conferencing PACT.
The data will be collected through semistructured interview and will be analysed with the classical technique of Interpretative Phenomenological Analysis.36 Population selection will follow the rules of the purposive sampling and will allow a maximal variation of the sample.37 An estimation of 30–60 parents will be necessary to reach data saturation based on previous studies.38–40 The total number of therapists (around 7–8) will be interviewed. During the 40–60 min interview, we will explore the barriers and facilitators to implementing PACT by videoconferencing. A guide for the interview will be elaborated in the initial phase of the project based on first interviews. Interviews will be recorded and transcribed before analyses.
Data from the quantitative and qualitative sources in the process evaluation will be analysed separately. The results of the qualitative study will be integrated with the quantitative results to optimise the findings.41
Monitoring
M-MG (IP) investigators associated, methodologists, statistician, parent representatives and associate researcher composed the trial steering committee (TSC). The TSC is independent of sponsor and funders and have no competing interests. The TSC has developed the study protocol and is responsible for data collection, management, publications and the final data set.
The coordinating centre is independent from the centres for investigation.
According to the French law, the study requires formal data monitoring undertaken by the sponsor. Annual reporting will be completed and submitted to the funders.
Adverse events
Based on results from previous PACT intervention trials, no specific harm from trial participation is anticipated. However, as required by the French law, adverse events will be collected throughout the study and reported in the eCRF section. Description of the event, date of occurrence, intensity, severity, accountability will be reported. Outcomes of this event and action taken after its report will also be concealed.
We anticipate that the early assessment, follow-up consultation on ASD and its management will help and support both groups during the postdiagnosis period. Hence, no post-trial care is planned.
Trial status
The trial status is currently Recruiting. The study has started the 30 June 30, 2020. The anticipated end date will be 30 June 2023.
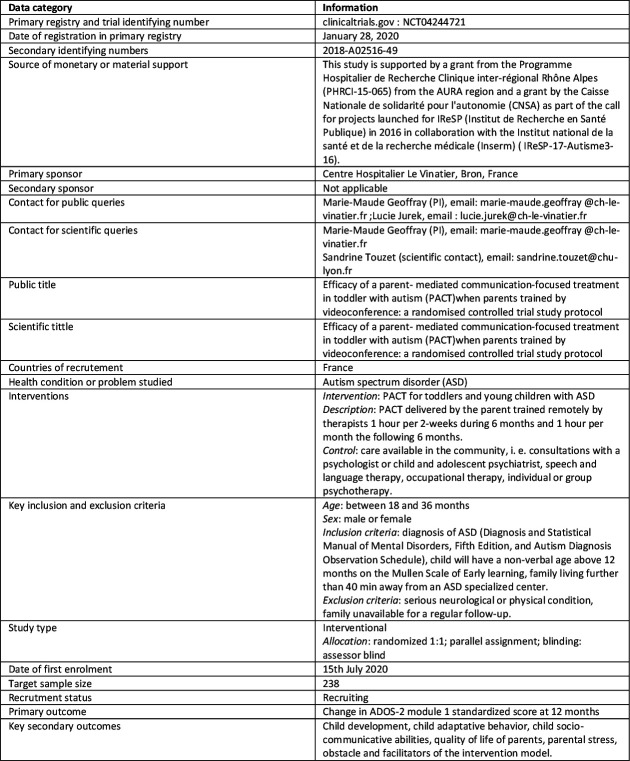
Figure 3 shows WHO trial registration data set. Online supplemental appendix 3 shows Standard Protocol Items: Recommendations for Interventional Trials Checklist.
Figure 3.
Who trial registration data set. ADOS, Autism Diagnostic Observation Scale; PACT, Preschool Autism Communication Trial.
bmjopen-2020-044669supp003.pdf (88.2KB, pdf)
Ethics and dissemination
This study (protocolV.5, date: 25 October 2019) is approved by the French National Review Board (reference No 2018-A02516-49). The results will be disseminated via peer-reviewed journals. It will also disseminate via national and international, general and specialist meeting and through the parent association (https://Bleunetwork.fr; https://autisme-ambitionavenir.com; desailespourgrandir.org). An individual feedback to the participant will be done through a regular newsletter. We will adhere to defined authorship criteria as per the International Committee of Medical Journal Editors.
Supplementary Material
Footnotes
Collaborators: Mrs Pauline Auphan (psychologist), Mrs Laetitia Bouveret (research assistant), Mrs Laurie Herman (research assistant), Dr Anne-Laure Toureille (PACT trainer), Mrs Lucie Jansen (PACT trainer), Dr Sandrine Sonié (CRA Lyon), Pr.Mario Speranza (CHU Versaille), Pr. Bruno Falissard (Paris), Pr Nicolas Georgieff (Lyon), Dr Matias Winter (HCL), Mrs Nadège Alloisio (parent association), Mr Chams-Ddine BELKHAYAT (parent association).
Contributors: M-MG and ST, PO, LJ conceived and design the project, and M-MG is leading the coordination of the trial. M-MG, LJ and PO drafted the protocol and procured the project funding. LJ and M-MG are responsible for study implementation, staff training and supervision. PO, ST, AD and AZ contributed to the sample size calculation, the randomisation procedure and the statistical plan, and are responsible for data management, randomisation and statistical analysis. JG contributed to the protocol and paper writing. AR-L contributed to the protocol of the qualitative study. CA and NG to the PACT training and supervision of the team. M-MG, M-JO, LJ, AA, AJ, AB, CS, TM, TD are responsible for recruitment and evaluation of children. SG contributed to draft the paper. All authors critically reviewed and approved the final version of the manuscript.
Funding: This study is supported by a grant from the Programme Hospitalier de Recherche Clinique inter-régional Rhône Alpes (PHRCI-15-065) from the AURA region and a grant by the Caisse Nationale de solidarité pour l'autonomie (CNSA) as part of the call for projects launched for IReSP (Institut de Recherche en Santé Publique) in 2016 in collaboration with the Institut national de la santé et de la recherche médicale (Inserm) (IReSP-17-Autisme3-16).
Disclaimer: The funders and sponsor (CH le Vinatier, 95, boulevard Pinel, France) have no role in study design, data collection, management, data analysis and interpretation of data, in the writing of the report or in the decision to submit the manuscript for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1. Kogan MD, Vladutiu CJ, Schieve LA, et al. The prevalence of Parent-Reported autism spectrum disorder among US children. Pediatrics 2018;142:e20174161. 10.1542/peds.2017-4161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lyall K, Croen L, Daniels J, et al. The changing epidemiology of autism spectrum disorders. Annu Rev Public Health 2017;38:81–102. 10.1146/annurev-publhealth-031816-044318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baghdadli A, Miot S, Rattaz C, et al. Investigating the natural history and prognostic factors of ASD in children: the multicEntric Longitudinal study of childrEN with ASD - the ELENA study protocol. BMJ Open 2019;9:e026286. 10.1136/bmjopen-2018-026286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Howlin P. Living with impairment: the effects on children of having an autistic sibling. Child Care Health Dev 1988;14:395–408. 10.1111/j.1365-2214.1988.tb00591.x [DOI] [PubMed] [Google Scholar]
- 5. Haute Autorité de Santé . Trouble du spectre de l’autisme Signes d’alerte, repérage, diagnostic et évaluation chez l’enfant et l’adolescent; 2018. https://www.has-sante.fr/upload/docs/application/pdf/2018-02/trouble_du_spectre_de_lautisme_de_lenfant_et_ladolescent__recommandations.pdf
- 6. Geoffray M-M, Thevenet M, Georgieff N. News in early intervention in autism. Psychiatr Danub 2016;28:66–70. [PubMed] [Google Scholar]
- 7. Oono IP, Honey EJ, McConachie H. Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Evidence-Based Child Health: A Cochrane Review Journal 2013;8:2380–479. 10.1002/ebch.1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zwaigenbaum L, Bauman ML, Choueiri R, et al. Early intervention for children with autism spectrum disorder under 3 years of age: recommendations for practice and research. Pediatrics 2015;136 Suppl 1:S60–81. 10.1542/peds.2014-3667E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. French L, Kennedy EMM. Annual research review: early intervention for infants and young children with, or at-risk of, autism spectrum disorder: a systematic review. J Child Psychol Psychiatry 2018;59:444–56. 10.1111/jcpp.12828 [DOI] [PubMed] [Google Scholar]
- 10. Sandbank M, Bottema-Beutel K, Crowley S, et al. Project aim: autism intervention meta-analysis for studies of young children. Psychol Bull 2020;146:1–29. 10.1037/bul0000215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Green J, Garg S. Annual research review: the state of autism intervention science: progress, target psychological and biological mechanisms and future prospects. J Child Psychol Psychiatry 2018;59:424–43. 10.1111/jcpp.12892 [DOI] [PubMed] [Google Scholar]
- 12. Green J, Charman T, McConachie H, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152–60. 10.1016/S0140-6736(10)60587-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pickles A, Le Couteur A, Leadbitter K, et al. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomised controlled trial. Lancet 2016;388:2501–9. 10.1016/S0140-6736(16)31229-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pickles A, Harris V, Green J, et al. Treatment mechanism in the MRC preschool autism communication trial: implications for study design and parent-focussed therapy for children. J Child Psychol Psychiatry 2015;56:162–70. 10.1111/jcpp.12291 [DOI] [PubMed] [Google Scholar]
- 15. Vismara LA, McCormick CEB, Wagner AL, et al. Telehealth parent training in the early start Denver model: results from a randomized controlled study. Focus Autism Other Dev Disabl 2018;33:67–79. 10.1177/1088357616651064 [DOI] [Google Scholar]
- 16. Vismara LA, McCormick C, Young GS, et al. Preliminary findings of a telehealth approach to parent training in autism. J Autism Dev Disord 2013;43:2953–69. 10.1007/s10803-013-1841-8 [DOI] [PubMed] [Google Scholar]
- 17. Green J, Aldred C, Charman T, et al. Paediatric autism communication Therapy-Generalised (PACT-G) against treatment as usual for reducing symptom severity in young children with autism spectrum disorder: study protocol for a randomised controlled trial. Trials 2018;19:514. 10.1186/s13063-018-2881-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khan K, Hall CL, Davies EB, et al. The effectiveness of web-based interventions delivered to children and young people with neurodevelopmental disorders: systematic review and meta-analysis. J Med Internet Res 2019;21:e13478. 10.2196/13478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bearss K, Burrell TL, Challa SA, et al. Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: a demonstration pilot. J Autism Dev Disord 2018;48:1020–30. 10.1007/s10803-017-3363-2 [DOI] [PubMed] [Google Scholar]
- 20. Richards DA, Bazeley P, Borglin G, et al. Integrating quantitative and qualitative data and findings when undertaking randomised controlled trials. BMJ Open 2019;9:e032081. 10.1136/bmjopen-2019-032081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res 2013;48:2134–56. 10.1111/1475-6773.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim SH, Thurm A, Shumway S, et al. Multisite study of new autism diagnostic interview-revised (ADI-R) algorithms for toddlers and young preschoolers. J Autism Dev Disord 2013;43:1527–38. 10.1007/s10803-012-1696-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mullen EM. Mullen scales of early learning. Minnesota: AGS Circle Pines, 1995. [Google Scholar]
- 24. Aldred C, Green J, Emsley R, et al. Brief report: mediation of treatment effect in a communication intervention for pre-school children with autism. J Autism Dev Disord 2012;42:447–54. 10.1007/s10803-011-1248-3 [DOI] [PubMed] [Google Scholar]
- 25. Dunn G, Emsley R, Liu H, et al. Evaluation and validation of social and psychological markers in randomised trials of complex interventions in mental health: a methodological research programme. Health Technol Assess 2015;19:1–116. 10.3310/hta19930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord 2009;39:693–705. 10.1007/s10803-008-0674-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 2000;30:205–23. 10.1023/A:1005592401947 [DOI] [PubMed] [Google Scholar]
- 28. McConachie H, Parr JR, Glod M, et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol Assess 2015;19:1–506. 10.3310/hta19410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: American Psychiatric Association, 2013. [Google Scholar]
- 30. Grzadzinski R, Carr T, Colombi C, et al. Measuring changes in social communication behaviors: preliminary development of the brief observation of social communication change (BOSCC). J Autism Dev Disord 2016;46:2464–79. 10.1007/s10803-016-2782-9 [DOI] [PubMed] [Google Scholar]
- 31. Bassano D, Labrell F, Bonnet P. Le Développement du langage de production en français (DLPF) entre 18 et 42 mois : une synthèse. Enfance 2020;2:151–74. [Google Scholar]
- 32. Sparrow SS, Cicchetti DV, Balla DA. Vineland adaptive behavior scales:(VABS. London: NCS Pearson, 2005. [Google Scholar]
- 33. Leadbitter K, Aldred C, McConachie H, et al. The autism family experience questionnaire (AFEQ): an Ecologically-Valid, Parent-Nominated measure of family experience, quality of life and Prioritised outcomes for early intervention. J Autism Dev Disord 2018;48:1052–62. 10.1007/s10803-017-3350-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lacharité C, Éthier L. « Le stress parental chez les mères d’enfants d’âge préscolaire : validation et normes québécoises pour l’Inventaire de Stress Parental » Carl Lacharité. Louise Éthier et Christiane Piché 2013;17:183–203. [PubMed] [Google Scholar]
- 35. Pariente PD, Challita H, Mesbah M, et al. The GHQ-28 questionnaire in French: a validation survey in a panel of 158 General psychiatric patients. European Psychiatry 1992;7:15–20. 10.1017/S0924933800002455 [DOI] [Google Scholar]
- 36. Smith JA, Shinebourne P. Interpretative phenomenological analysis. : Cooper H, Camic PM, Long DL, et al., . APA Handbook of research methods in psychology, vol 2: research designs: quantitative, qualitative, neuropsychological, and biological. Washington: American Psychological Association, 2012: 73–82. [Google Scholar]
- 37. Guba EG L. Fourth generation evaluation. Thousand Oaks, California: Sage Publications, Inc, 1989. [Google Scholar]
- 38. Lachal J, Speranza M, Taïeb O, et al. Qualitative research using photo-elicitation to explore the role of food in family relationships among obese adolescents. Appetite 2012;58:1099–105. 10.1016/j.appet.2012.02.045 [DOI] [PubMed] [Google Scholar]
- 39. Gorse P, Nordon C, Rouillon F, et al. Subjective motives for requesting in-patient treatment in female with anorexia nervosa: a qualitative study. PLoS One 2013;8:e77757. 10.1371/journal.pone.0077757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Morse JM. The significance of saturation. Qual Health Res 1995;5:147–9. 10.1177/104973239500500201 [DOI] [Google Scholar]
- 41. Richards DA, Bazeley P, Borglin G, et al. Integrating quantitative and qualitative data and findings when undertaking randomised controlled trials. BMJ Open 2019;9:e032081. 10.1136/bmjopen-2019-032081 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044669supp001.pdf (159.5KB, pdf)
bmjopen-2020-044669supp002.pdf (133.6KB, pdf)
bmjopen-2020-044669supp003.pdf (88.2KB, pdf)