Abstract
Although the definition of white‐coat hypertension (WCH) in children and adolescents is clearly defined, little is known about how this condition is actually approached clinically. To better understand the contemporary approach to the diagnosis and management of WCH in pediatric patients, the authors surveyed the membership of the Midwest Pediatric Nephrology Consortium. Seventy‐four faculty pediatric nephrologists responded to the survey. The survey results demonstrated uniformity in diagnosing WCH, including ambulatory blood pressure monitoring use in 93% of the respondents and a 75% adherence rate according to the 2014 American Heart Association scientific statement on pediatric ambulatory blood pressure monitoring. A total of 85% of respondents would not embark on further diagnostic evaluation once the WCH diagnosis was established, and none would initiate antihypertensive medications. There was a wide variety of practice habits in follow‐up of WCH including frequency of office and out‐of‐office follow‐up blood pressure measurements, the setting and timing of physician follow‐up, and the role of repeat ambulatory blood pressure monitoring. The results of this survey highlight the need for prospective studies aimed at establishing the optimal approach to pediatric patients with WCH.
Keywords: ambulatory blood pressure monitoring, blood pressure measurement, pediatric white‐coat hypertension
1. INTRODUCTION
White‐coat hypertension (WCH) is defined as elevated office blood pressure (BP) measurements with normal BPs outside of the office setting.1 Ambulatory BP monitoring (ABPM) is often utilized for establishing the diagnosis. Various studies have reported a wide range in WCH prevalence ranging from 13% to 52% of children and adolescents with elevated office BP measurements.2, 3, 4, 5 Currently, the clinical significance of WCH in adults and pediatrics are both uncertain, but it may predict development of cardiovascular events in adults and target organ changes in children and adolescents.3, 6 The American Heart Association (AHA) Scientific Statement on pediatric ABPM provides specific criteria for making the diagnosis of WCH.7 However, the availability and utilization of ABPM for elevated BP measurements in pediatric nephrology practices in North America is not known. In addition, there are no data or consensus recommendations addressing management and follow‐up once the diagnosis of WCH is made. The objective of this study was to assess how WCH is currently diagnosed and how WCH patients are currently evaluated and followed by pediatric nephrologists in North America and to generate data for design of future studies of WCH in children and adolescents.
2. METHODS
We designed an Internet‐based 15‐question questionnaire (Table 1) on SurveyMonkey (Palo Alto, CA, USA; http://www.surveymonkey.com). Two email invitations, approximately 2 months apart, were sent using the master email list of the Midwest Pediatric Nephrology Consortium (MWPNC). The MWPNC comprises 57 pediatric nephrology centers in the United States and Canada, many of which have had a long‐standing research interest in childhood hypertension.8, 9, 10, 11 Instructions specified that survey respondents be faculty‐level pediatric nephrologists. We also requested that the recipients forward the survey to other faculty pediatric nephrologists at their respective centers. More than one pediatric nephrologist from each center could answer the survey, as our aim was to collect individual practice habits rather than center‐specific habits. Respondents’ names and their medical centers were not collected due to limitations of the survey instrument. Survey distribution was judged as exempt from institutional review board review according to federal regulations 45 CFR 46.101 (b) category 2.
Table 1.
Survey Questions
Q1: Does your center have a pediatric hypertension clinic?
|
Q2: What is the availability of ambulatory blood pressure (BP) monitoring (ABPM)?
|
| Q3: How may ABPM machines does your program have? (free text) |
Q4: I make a diagnosis of white‐coat hypertension by (check all that apply):
|
Q5: The ABPM studies are analyzed/interpreted by:
|
Q6: Which criteria do you use to read the ABPM?
|
Q7: If you make a diagnosis of WCH based on ABPM, which criteria do you use?
|
Q8: If you make a diagnosis of white‐coat hypertension (WCH) based on readings outside of the office, which criteria do you use?
|
Q9: Prior to making a diagnosis of WCH, which diagnostic evaluations do you perform (check all that apply)?
|
Q10: Is any diagnostic evaluation performed after establishing a diagnosis of WCH?
|
Q11: Is any intervention provided after establishing a diagnosis of WCH?
|
Q12: Once a diagnosis of WCH is made, do you recommend home BP monitoring?
|
Q13: What follow‐up do you recommend for WCH?
|
Q14: If seen back in nephrology for follow‐up of WCH at a later point, what does follow‐up involve? (check all that apply)
|
Q15: If you repeat ABPM after making a diagnosis of WCH, what is the frequency of these follow‐up studies?
|
All of the survey questions were structured as multiple‐choice items (Table 1), and the results of the survey were expressed and compared as fractions and percentages of respondents. There were multiple survey questions that had “other” as a choice allowing respondents to enter free text answers. Each free text answer was reviewed individually by the investigators. When appropriate, free text answers were reclassified to one of the multiple‐choice answers. This reclassification occurred on average about 0.9 responses per question. Calculations and production of figures were performed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA).
3. RESULTS
A total of 74 pediatric nephrologists in the MWPNC responded to the survey. We were unable to calculate the overall response rate as the master MWPNC email list was used, which contained research coordinators and fellows, and we were unable to distinguish which names on the list were faculty pediatric nephrologist. In addition, we do not know to what extent the survey was forwarded to other MWPNC center pediatric nephrologists who were not on the master email list. The respondents had options to skip survey questions and, therefore, the denominator for each question differed as indicated below.
3.1. General description of outpatient pediatric nephrology BP evaluation
Of the pediatric nephrologists who responded to the survey, 47 of 74 providers (64%) had dedicated hypertension specialty clinics or programs at their respective centers. A total of 68 of 72 providers (94%) had ABPM available in their practices. However, only 27 of 72 providers (38%) responded that ABPM was available at all times, while 41 of 72 providers (57%) responded that patients sometimes had to wait to have ABPM performed. Approximately half of respondents had five or fewer monitors available at their centers, 25% had six to 10 monitors, and 25% had >10 monitors. Last, almost all ABPM measurements ordered by the survey respondents (88%) were interpreted by pediatric nephrologists. A small fraction of ABPM studies (12%) were interpreted by nurse practitioners, clinical nurses, and cardiologists either alone or together with pediatric nephrologists.
3.2. Diagnosis of WCH
Survey respondents could select more than one method of WCH diagnosis, and, as indicated in Figure 1, the diagnosis of WCH was primarily made by BP measurements obtained in nonclinical settings. The most frequently used method was ABPM (65 of 70 [93%]), followed by home BP readings (37 of 70 [53%]) and school BP readings (20 of 70 [29%]). There were three responses stating that other office or clinic BP readings were used to diagnose WCH.
Figure 1.
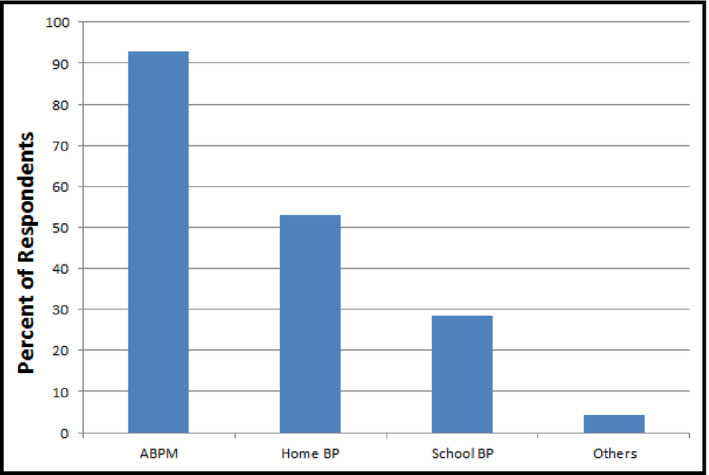
Method of white‐coat hypertension diagnosis (N=70). More than one response was allowed. ABPM, ambulatory blood pressure monitoring; BP, blood pressure
Table 2 shows the criteria by which WCH was diagnosed. First, most respondents cited the use of the 2014 AHA ABPM statement7 followed by the original 2008 AHA ABPM statement12 when interpreting ABPM. Second, consistent with the 2014 AHA guideline, normal day and night mean systolic and diastolic BPs and BP loads <25% were the most common diagnostic criteria for WCH. Last, when providers relied on out‐of‐office BPs to make the diagnosis of WCH, approximately two thirds required out‐of‐clinic BPs to be <95th percentile BP, while approximately one third used out‐of‐clinic BPs <90th percentile (percentiles from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents ).13
Table 2.
Criteria for WCH Diagnosis With and Without ABPM
| ABPM Interpretation Guidelines (n=53) | ABPM WCH Criteria (n=54) | Non‐ABPM WCH Diagnosis Method (n=57) |
|---|---|---|
|
|
|
Abbreviations: ABPM, ambulatory blood pressure monitoring; AHA, American Heart Association; BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure; WCH, white‐coat hypertension.
As demonstrated in Figure 2, there was some practice variety in the approach to the evaluation of elevated BPs. The majority of practitioners did not perform any additional diagnostic studies until the assessment for WCH was complete (35 of 61 [57%]). Diagnostic testing performed prior to or concurrent with assessment for WCH included laboratory studies, imaging studies, and echocardiography.
Figure 2.
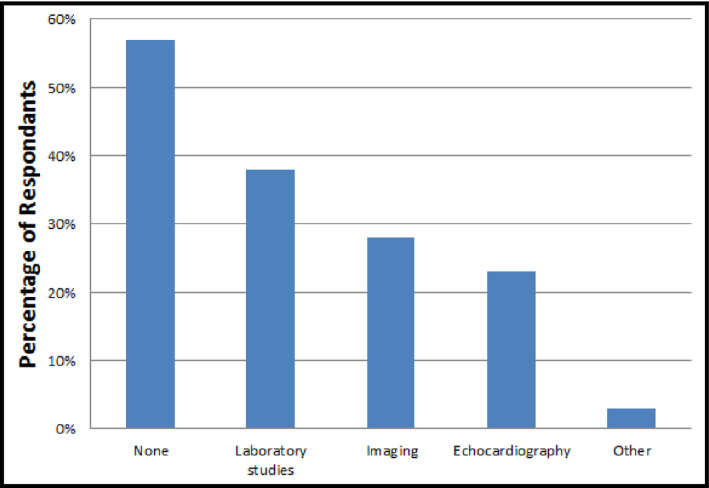
Diagnostic evaluation to perform prior to white‐coat hypertension diagnosis (N=61). More than one response allowed
3.3. Evaluation and management of WCH
After the diagnosis of WCH was made, most pediatric nephrologists did not perform further diagnostic evaluation (53 of 62 [85%]). Of the 15% who responded that they would perform additional evaluation, the most common tests ordered included echocardiography and laboratory studies to investigate for metabolic syndrome (blood tests such as lipid panel and glycated hemoglobin). A total of 79% (53 of 67) of the respondents recommended lifestyle modification for patients with WCH, while 13% (9 of 67) recommended no intervention. Other interventions mentioned by survey respondents included anxiety evaluation and relaxation techniques. Of note, no provider replied that they would prescribe antihypertensive medication.
Table 3 demonstrates the follow‐up approaches of the practitioners once the diagnosis of WCH was established. While the majority of practitioners did not recommend home BP monitoring, a minority suggested monitoring as frequently as once or twice weekly and as infrequently as once a year. About half of the respondents recommended return visits to their own practices, with the most common interval being 6 to 12 months. The remainder recommended primary care provider follow‐up and/or as‐needed follow‐up with pediatric nephrology.
Table 3.
Follow‐Up Plans Once White‐Coat Hypertension is Established
| Recommend Home Blood Pressure Monitoring (N=67) | Recommended MD Follow‐Up (N=67) | |
|---|---|---|
| No: 44 (66%) |
Yes: 23 (34%) How often?
|
|
As demonstrated in Table 4, if WCH patients were seen for follow‐up in pediatric nephrology clinics, many of the providers reviewed various types of interim BP measurements including clinic BP measurements and out‐of‐clinic BP measurements, at home and less often at school. In addition, approximately half of the providers reported repeating ABPM at follow‐up visits in 1 year, 2 years, or on a case‐dependent frequency. Lifestyle modification was reviewed by most providers at follow‐up visits.
Table 4.
Follow‐Up for WCH in Pediatric Nephrology Clinics
| Pediatric nephrology WCH follow‐up includes: (N=62, more than one answer accepted) | Frequency of follow‐up ABPM: (N=45) |
|---|---|
|
|
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; WCH, white‐coat hypertension.
4. DISCUSSION
This survey of pediatric nephrologists in the MWPNC showed a number of similar practice patterns for WCH. First, a large number of MWPNC survey respondents practice at centers with a dedicated hypertension program. Second, ABPM appears to be the predominant diagnostic tool for WCH diagnosis. Third, there has been widespread adoption of the 2014 AHA scientific statement when interpreting ABPM. Fourth, at this point, no pediatric nephrologist in the MWPNC who participated in the survey routinely prescribes antihypertensive medication to WCH patients.
In contrast, there was considerable variation among MWPNC practitioners in the number of ABPM machines available at their respective centers. A majority of surveyed pediatric nephrologists reported that patients sometimes had to wait to have ABPM performed. This suggests that many centers could benefit from having more ABPM machines available to allow for timely evaluation for WCH. Pediatric studies have demonstrated that identification of WCH as the first step in the evaluation of elevated BP measurement is cost‐effective as it reduces unnecessary diagnostic testing and potentially inappropriate antihypertensive therapy.14, 15 Last, and most important, we found variations in practice habits of evaluation and follow‐up of patients with WCH. These variations in practice habits most likely have arisen from a lack of evidence‐based practice guidelines for WCH. This topic would appear to be a fertile area for further research.
Although long‐recognized, the prognostic significance of WCH remains uncertain.16, 17 In adults, the risk of cardiovascular events in WCH individuals may be intermediate between normotensive individuals and hypertensive individuals. In a recent meta‐analysis, individuals diagnosed with WCH by office BP and ABPM or home BP measurements were found to have higher rates of cardiovascular disease morbidity and mortality but not significantly different all‐cause mortality and stroke risk compared with normotensive persons; meanwhile, the risks of cardiovascular disease morbidity and mortality, all‐cause mortality, and stroke rates were significantly increased in sustained hypertensive patients compared with WCH patients.17 Adult WCH in ABPM‐only studies also showed mixed results, as one study demonstrated higher cardiovascular risk18 while another study showed no increase in risk.19 Further, WCH in adults may be a precursor to sustained hypertension, as longitudinal studies have shown that initial WCH patients were more likely to progress to sustained hypertension.20, 21, 22
In children, it is much more difficult to ascertain the cardiovascular implications of WCH because the incidence of cardiovascular events in this population is exceedingly low. In the absence of hard cardiovascular end points, pediatric studies have evaluated the association between WCH and target organ changes such as left ventricular mass and carotid intimal‐medial thickness.23, 24, 25, 26 Recent pediatric studies suggest that WCH in pediatric patients may result in intermediate target organ changes, similar to adult WCH. In a study where age, sex, and body mass index were matched for ABPM‐confirmed WCH patients with confirmed hypertensive and normotensive patients, the mean left ventricular mass index of WCH patients was between that of normotensive and hypertensive patients.2 The difference between the WCH patients and the normotensive patients was statistically significant. Another study found that ABPM‐confirmed WCH patients tended to have higher left ventricular mass index than normotensive patients but lower than hypertensive patients, although no statistically significant differences were found between the groups.4
5. STUDY LIMITATIONS
Limitations of this study include the possibility of recall and selection bias and incomplete capture of current practice habits due to limited survey distribution. We suspect that respondents were more likely to be pediatric nephrologists with a higher level of interest in pediatric hypertension. This survey was limited to physicians at MWPNC centers, and their practices may not reflect the actual practice of pediatric nephrologists as a whole. We were also unable to identify the response rate of the survey, and, by design, we did not collect the practice centers of the survey respondents as we were more interested in finding out the practice patterns of individual practitioners. Thus, it is possible that these survey results may reflect practice patterns of practitioners at a relatively small number of pediatric nephrology centers. Because we did not collect the practice centers, we were unable to identify any center‐specific practice patterns of additional diagnostic studies such as laboratory studies prior to or concurrent with evaluation of WCH (question #9). In addition, results regarding diagnostic testing prior to WCH diagnosis may not be reflective of how MWPNC pediatric nephrologists practice. Many patients referred for elevated BP have already had diagnostic testing performed by their primary care providers prior to their initial pediatric nephrology visit. Although the survey specifically asked whether the respondent performed pretesting, some may have included testing by others when answering question #9. Further, many pediatric nephrology practices conduct routine urinalysis on all clinic patients, which may have been considered by some as laboratory testing when answering the survey.
6. CONCLUSIONS
Despite the above limitations, we feel that this study provides useful initial data in a poorly studied area of childhood hypertension. We noted significant variability in the follow‐up for WCH children and adolescents in terms of timing, clinic type, and method of reevaluation. With future studies of WCH children and adolescents, we hope to establish a standardized practice guideline for the diagnosis, evaluation, management, and follow‐up of these patients. Finally, with larger prospective studies in this population, we may ultimately be able to determine whether target organ changes occur in pediatric WCH and quantify the risk for progression to sustained hypertension.
DISCLOSURE
The authors report no specific funding in relation to this research and no conflicts of interest to disclose.
Miyashita Y, Flynn JT, Hanevold CD. Diagnosis and management of white‐coat hypertension in children and adolescents: A Midwest Pediatric Nephrology Consortium study. J Clin Hypertens. 2017;19:884–889. 10.1111/jch.13006
REFERENCES
- 1. Gelfer M, Dawes M, Kaczorowski J, Padwal R, Cloutier L. Diagnosing hypertension: evidence supporting the 2015 recommendations of the Canadian Hypertension Education Program. Can Fam Physician. 2015;61:957‐961. [PMC free article] [PubMed] [Google Scholar]
- 2. Lande MB, Meagher CC, Fisher SG, Belani P, Wang H, Rashid M. Left ventricular mass index in children with white coat hypertension. J Pediatr. 2008;153:50‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kavey RE, Kveselis DA, Atallah N, Smith FC. White coat hypertension in childhood: evidence for end‐organ effect. J Pediatr. 2007;150:491‐497. [DOI] [PubMed] [Google Scholar]
- 4. Stabouli S, Kotsis V, Toumanidis S, Papamichael C, Constantopoulos A, Zakopoulos N. White‐coat and masked hypertension in children: association with target‐organ damage. Pediatr Nephrol. 2005;20:1151‐1155. [DOI] [PubMed] [Google Scholar]
- 5. Sorof JM, Poffenbarger T, Franco K, Portman R. Evaluation of white coat hypertension in children: importance of the definitions of normal ambulatory blood pressure and the severity of casual hypertension. Am J Hypertens. 2001;14(9 pt 1):855‐860. [DOI] [PubMed] [Google Scholar]
- 6. Cuspidi C, Sala C, Grassi G, Mancia G. White coat hypertension: to treat or not to treat? Curr Hypertens Rep. 2016;18:80. [DOI] [PubMed] [Google Scholar]
- 7. Flynn JT, Daniels SR, Hayman LL, et al. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63:1116‐1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shatat IF, Jakson SM, Blue AE, Johnson MA, Orak JK, Kalpatthi R. Masked hypertension is prevalent in children with sickle cell disease: a Midwest Pediatric Nephrology Consortium study. Pediatr Nephrol. 2013;28:115‐120. [DOI] [PubMed] [Google Scholar]
- 9. Kapur G, Ahmed M, Pan C, Mitsnefes M, Chiang M, Mattoo TK. Secondary hypertension in overweight and stage 1 hypertensive children: a Midwest Pediatric Nephrology Consortium report. J Clin Hypertens (Greenwich). 2010;12:34‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin JJ, Mitsnefes MM, Smoyer WE, Valentini RP. Antihypertensive prescription in pediatric dialysis: a practitioner survey by the Midwest Pediatric Nephrology Consortium study. Hemodial Int. 2009;13:307‐315. [DOI] [PubMed] [Google Scholar]
- 11. VanDeVoorde RG, Barletta GM, Chand DH, et al. Blood pressure control in pediatric hemodialysis: the Midwest Pediatric Nephrology Consortium Study. Pediatr Nephrol. 2007;22:547‐553. [DOI] [PubMed] [Google Scholar]
- 12. Urbina E, Alpert B, Flynn J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association atherosclerosis, hypertension, and obesity in youth committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433‐451. [DOI] [PubMed] [Google Scholar]
- 13. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555‐576. [PubMed] [Google Scholar]
- 14. Swartz SJ, Srivaths PR, Croix B, Feig DI. Cost‐effectiveness of ambulatory blood pressure monitoring in the initial evaluation of hypertension in children. Pediatrics. 2008;122:1177‐1181. [DOI] [PubMed] [Google Scholar]
- 15. Davis ML, Ferguson MA, Zachariah JP. Clinical predictors and impact of ambulatory blood pressure monitoring in pediatric hypertension referrals. J Am Soc Hypertens. 2014;8:660‐667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lurbe E, Torro MI, Alvarez J. Ambulatory blood pressure monitoring in children and adolescents: coming of age? Curr Hypertens Rep. 2013;15:143‐149. [DOI] [PubMed] [Google Scholar]
- 17. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White‐coat hypertension and cardiovascular events: a meta‐analysis. J Hypertens. 2016;34:593‐599. [DOI] [PubMed] [Google Scholar]
- 18. Gustavsen PH, Hoegholm A, Bang LE, Kristensen KS. White coat hypertension is a cardiovascular risk factor: a 10‐year follow‐up study. J Hum Hypertens. 2003;17:811‐817. [DOI] [PubMed] [Google Scholar]
- 19. Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of “masked” hypertension and “white‐coat” hypertension detected by 24‐h ambulatory blood pressure monitoring 10‐year follow‐up from the Ohasama study. J Am Coll Cardiol. 2005;46:508‐515. [DOI] [PubMed] [Google Scholar]
- 20. Bidlingmeyer I, Burnier M, Bidlingmeyer M, Waeber B, Brunner HR. Isolated office hypertension: a prehypertensive state? J Hypertens. 1996;14:327‐332. [DOI] [PubMed] [Google Scholar]
- 21. Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non‐hypertensive participants in the Framingham Heart study: a cohort study. Lancet. 2001;358:1682‐1686. [DOI] [PubMed] [Google Scholar]
- 22. Siven SS, Niiranen TJ, Kantola IM, Jula AM. White‐coat and masked hypertension as risk factors for progression to sustained hypertension: the Finn‐Home study. J Hypertens. 2016;34:54‐60. [DOI] [PubMed] [Google Scholar]
- 23. Kavey RE. Left ventricular hypertrophy in hypertensive children and adolescents: predictors and prevalence. Curr Hypertens Rep. 2013;15:453‐457. [DOI] [PubMed] [Google Scholar]
- 24. Brady TM, Fivush B, Flynn JT, Parekh R. Ability of blood pressure to predict left ventricular hypertrophy in children with primary hypertension. J Pediatr. 2008;152:73‐78. [DOI] [PubMed] [Google Scholar]
- 25. Lande MB, Carson NL, Roy J, Meagher CC. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40‐44. [DOI] [PubMed] [Google Scholar]
- 26. Sorof JM, Alexandrov AV, Garami Z, et al. Carotid ultrasonography for detection of vascular abnormalities in hypertensive children. Pediatr Nephrol. 2003;18:1020‐1024. [DOI] [PubMed] [Google Scholar]


