Abstract
This study aimed to investigate whether conventional predisposing factors modify the associations of homocysteine with blood pressure levels and hypertension. A total of 2615 adults were recruited from Liaoning province. An elevated homocysteine level was significantly associated with increased hypertension risk and blood pressure (all P<.05). Interaction analyses showed that homocysteine acted synergistically with age, overweight/obesity, dyslipidemia, and family history of hypertension to affect hypertension risk, and the relative excess risk due to interaction was 1.21 (95% confidence interval, 0.07–2.35), 0.72 (95% confidence interval, 0.07–1.36), 0.45 (95% confidence interval, 0.06–0.85), and 1.87 (95% confidence interval, 0.77–2.97), respectively. Increases in blood pressure were higher in patients who were overweight/obese or had a family history of hypertension than in their counterparts (all P interaction <.05). This study provides some strong evidence for interactions of homocysteine with conventional predisposing factors on hypertension.
Keywords: Chinese, homocysteine, hypertension, interaction
1. INTRODUCTION
Hypertension is the leading risk factor for cardiovascular diseases.1 According to the Global Status Report on Non‐Communicable Diseases (2010), hypertension affects 40% of adults worldwide and the prevalence is increasing, specifically in developing countries such as China.2, 3 However, the etiology of hypertension is complicated and not fully understood.
Age, sex, being overweight/obesity, sodium intake, tobacco use, alcohol consumption, and dyslipidemia are well‐established traditional predisposing factors for hypertension.4, 5 Elevated plasma homocysteine levels (hyperhomocysteinemia, defined as plasma homocysteine concentrations ≥10 μmol/L) is an independent risk factor for cardiovascular diseases.6, 7 Our previous meta‐analysis showed that the prevalence of hyperhomocysteinemia in China was 27.5%, and was higher in northerners, the inlanders, men, and the elderly.8 Recently, hyperhomocysteinemia has been considered as a novel potential contributor to hypertension or elevated blood pressures (BPs).9, 10, 11 The underlying biomechanisms by which hyperhomocysteinemia cause hypertension may include increasing arterial stiffness and sodium reabsorption, reducing bioavailability of nitric oxide and vasodilatory capacity, and inducing oxidative stress, arteriolar constriction, insulin resistance, and aberrant genomic DNA methylation status.12, 13, 14 A number of human epidemiological studies have been conducted to evaluate the associations of homocysteine with hypertension and BP in different populations.15, 16, 17, 18, 19, 20 Despite some reported negative and null findings, the overall evidence indicates a positive relationship of homocysteine with hypertension and/or BPs.15, 16, 19 A few of these human studies have also performed further subgroup analyses and found that the association between higher homocysteine levels and increase in BP was stronger in women, smokers, and drinkers,16, 20 which indicates that these factors may modify the association between homocysteine and BPs. In a systematic MEDLINE search, we only found three relevant human epidemiological studies on the interactions of homocysteine with several conventional predisposing factors on BPs and hypertension risk.16, 17, 18 However, all three studies failed to perform formal interaction tests, and it is still unknown to what extent coexposure to homocysteine and these predisposing factors may impact hypertension and arterial BPs.
Therefore, we performed a cross‐sectional study to: (1) confirm whether higher plasma homocysteine levels are associated with increased hypertension susceptibility and BPs after adjusting for traditional predisposing factors, and (2) to quantitatively estimate the interactive effects of the conventional predisposing factors with homocysteine on hypertension and BPs. The study was conducted among 2615 adults living in Liaoning province, northeastern China, where the prevalence rates of both hypertension and hyperhomocysteinemia were previously reported to be high.2, 8
2. METHODS
2.1. Study participants and inclusion criteria
Between April and June 2015, a total of 2761 individuals aged 35 years or older were recruited from Shenhe district. The district consists of 14 blocks and is located in the center of Shenyang city, which is an important industrial center in northeastern China (Figure). Shenhe district has a northerly continental monsoon climate characterized by long, cold, and dry winters, but short, warm, and wet summers. More than 1 million people live in this district, of whom about 73% are registered residents. Most of the residents adopted traditional northern dietary habits, which is characterized by high intake of salt, wheat flour products, and starchy tubers but low consumption of fruits and vegetables.21 Consequently, plasma levels of folate and vitamin B12 were often reported to be lower in these residents.22, 23 Similar to other regions in northern China, the prevalence of cardiovascular diseases such as stroke, coronary heart disease, hypertension, and metabolic syndrome was often reported to be high in the district.24, 25 Our study adopted a multistage sampling method. In the first stage, all 14 blocks in the district were selected and eight residential communities were randomly selected from each of the blocks. In the second stage, systematic sampling was conducted to select 25 households in each residential community. In the third stage, within each household, one person, aged 35 years or older who lived in the district for at least 2 years, was randomly selected without replacement. Of those invited residents, 2615 met our inclusion criteria (without malignant diseases, chronic renal diseases, hypothyroidism, or secondary hypertension; without taking multivitamins; Han nationality) and were finally included in formal analysis. The overall response rate was 94.71%. The study was conducted in accordance with the principles stipulated by the Declaration of Helsinki, and all protocols were approved by the ethics review committee of China Medical University (Shenyang, China). All specimens and survey data were obtained with written informed consent from all participants prior to study entry.
Figure 1.
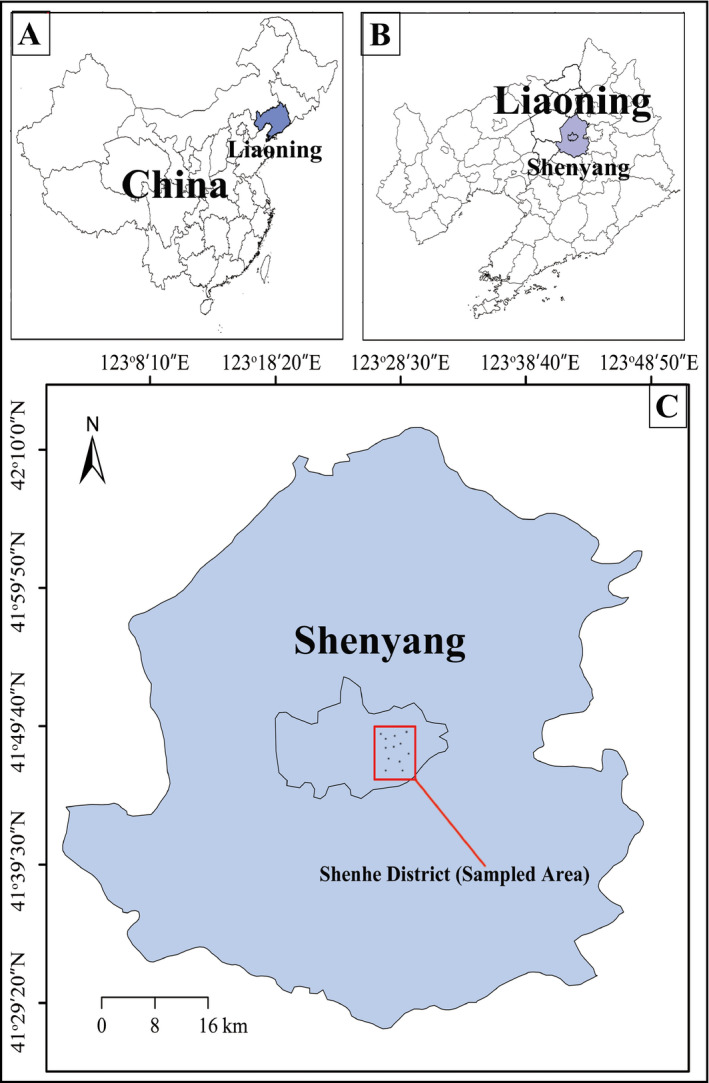
Geographic distribution of the sampled regions in Shenhe district
2.2. Data collection and definitions
All patients underwent a self‐administered questionnaire delivered by a face‐to‐face interview. Participants were asked to provide information on demographic characteristics, tobacco use, alcohol consumption, dietary habits, family history of hypertension, and other health‐related data. Smoking and drinking status were categorized as “current,” “former,” and “nonsmokers or nondrinkers,” which have been detailed in our previous paper.26 We used the combined “current” and “former” as “ever‐smokers or ever‐drinkers” for easy analysis as the number of “former” is too small to deduce valid results. In addition, we used a questionnaire to collect information on the total amount of salt intake and members of a household for meals at home over the past month. Then, individual salt intake was calculated with salt intake per month per household divided by members of the household and 30 (days). Participants were classified into low (≤6 g/d) and high (>6 g/d) salt intake groups based on Chinese Dietary Guidelines and Food Guide Pagoda.27
Systolic BP (SBP) and diastolic BP (DBP) were measured using a standard mercury sphygmomanometer while participants were in the sitting position after 15 minutes of rest.28 The average of three consecutive measurements to the nearest 2 mm Hg was recorded. Hypertension was defined as the mean SBP ≥140 mm Hg and/or DBP ≥90 mm Hg and/or currently receiving treatment for hypertension. Body weight and height were measured using standard techniques and equipment with light clothing and bare feet after an overnight fast. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters (kg/m2). Overweight/obesity was regarded as a BMI ≥24 kg/m2 according to the Guidelines on the Prevention and Management of Overweight and Obese in Adults: China.29
Concentrations of fasting plasma glucose (FPG), triglycerides, total cholesterol, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, and plasma homocysteine were determined by enzymatic method using a Mindray Autoanalyzer (BS 380 type, Mindray Ltd). Dyslipidemia was defined as total cholesterol >5.18 mmol/L and/or triglycerides >1.70 mmol/L and/or high‐density lipoprotein cholesterol <1.04 mmol/L, and/or low‐density lipoprotein cholesterol >3.37 mmol/L according to the Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults.30 Diabetes mellitus was defined as an FPG value ≥7.0 mmol/L and/or currently receiving treatment for diabetes mellitus according to the American Diabetes Association criteria.31 Hyperhomocysteinemia was defined as fasting plasma homocysteine levels ≥10 μmol/L.32
2.3. Statistical analysis
Statistical analyses were performed using SAS software (version 9.2, SAS Institute Inc). Triglyceride and plasma homocysteine levels were natural logarithmically transformed to correct skewed distributions. Differences in age, BMI, total cholesterol, triglycerides, low‐density lipoprotein cholesterol, high‐density lipoprotein cholesterol, FPG, SBP, DBP, and homocysteine levels between the hypertension and normotension groups were analyzed by Student t test. Differences in salt consumption, family history of hypertension, smoking and drinking status, and prevalence of homocysteine, diabetes mellitus, and dyslipidemia between the two groups were analyzed by chi‐square test. Logistic regression analysis was used to explore the relationship between plasma homocysteine levels and hypertension. Subsequently, stratified analyses by age (<60 and ≥60 years [the mean age of the study participants was 59.94 years]), sex, BMI (normal and overweight/obese), smoking status (nonsmokers and ever‐smokers), drinking status (nondrinkers and ever‐drinkers), salt consumption (≤6 and >6 g/d), dyslipidemia (yes and no), type 2 diabetes mellitus (yes and no), and family history of hypertension (yes and no) was performed to explore the potential interaction effects. Furthermore, the relative excess risk due to interaction (RERI) and corresponding 95% confidence interval (CI) were calculated to evaluate the presence of interactions on the additive scale. An RERI of 0 indicates an absent interaction effect, an RERI >0 indicates a positive interaction, and an RERI <0 indicates a negative interaction. The 95% CI excludes 0 indicates P<.05. In addition, generalized linear regression models were used to examine the associations of homocysteine levels with SBP and DBP. A two‐sided P<.05 was taken as statistically significant.
3. RESULTS
3.1. Baseline characteristics
The baseline characteristics of the study participants are presented in Table 1. The average age of the study participants was 59.94±10.62 years (women: 59.70±10.52 years; men: 60.41±10.80 years), and 33.96% were men (888 men and 1727 women). The overall prevalence of hypertension and homocysteine was 43.59% and 70.29%, respectively. Compared with individuals without hypertension, those with hypertension had significantly higher BMI, total cholesterol, triglycerides, low‐density lipoprotein cholesterol, FPG, SBP, DBP, and homocysteine levels, and were more likely to be older, male, and have diabetes mellitus or dyslipidemia, a family history of hypertension, or higher salt consumption (all P<.05).
Table 1.
Baseline demographic and clinical characteristics of the study participants
| Characteristic | Total (n=2615) | Nonhypertension (n=1475) | Hypertension (n=1140) | P Value |
|---|---|---|---|---|
| Age, y | 59.94±10.62 | 57.39±10.82 | 63.24±9.38a | <.001 |
| Men, No. (%) | 888 (33.96) | 456 (30.92) | 432 (37.89)a | <.001 |
| BMI, kg/m2 | 24.54±3.66 | 23.97±3.50 | 25.27±3.74a | <.001 |
| TC, mmol/L | 5.22±1.13 | 5.14±1.14 | 5.32±1.11a | <.001 |
| Triglycerides, mmol/Lb | 1.60 (1.14–2.10) | 1.55 (1.10–2.02) | 1.66 (1.20–2.19)a | <.001 |
| LDL‐C, mmol/L | 2.75±0.87 | 2.67±0.88 | 2.85±0.85a | <.001 |
| HDL‐C, mmol/L | 1.47±0.48 | 1.49±0.51 | 1.44±0.44b | .026 |
| FPG, mmol/L | 5.85±2.76 | 5.70±2.83 | 6.04±2.66b | .002 |
| SBP, mm Hg | 130.05±13.84 | 123.14±9.83 | 139.00±13.14a | <.001 |
| DBP, mm Hg | 79.80±9.10 | 76.38±6.75 | 84.21±1.00a | <.001 |
| Diabetes mellitus, No. (%) | 354 (13.54) | 168 (11.39) | 186 (16.32)a | <.001 |
| Dyslipidemia, No. (%) | 1847 (70.63) | 1000 (67.80) | 847 (74.30)a | <.001 |
| Family history of hypertension, No. (%) | 827 (31.63) | 361 (24.47) | 466 (40.88)a | <.001 |
| Salt, No. (%) | ||||
| ≤6 g/d | 1012 (38.73) | 599 (40.61) | 413 (36.23) | .023 |
| >6 g/d | 1601 (61.27) | 875 (59.32) | 726 (63.68)b | |
| Smoking status, No. (%) | ||||
| Nonsmoker | 2160 (82.60) | 1229 (83.32) | 931 (81.67) | .268 |
| Ever‐smoker | 455 (17.40) | 246 (16.68) | 209 (18.33) | |
| Drinking status, No. (%) | ||||
| Nondrinker | 1888 (72.20) | 1071 (72.61) | 817 (71.67) | .593 |
| Ever‐drinker | 727 (27.80) | 404 (27.39) | 323 (28.33) | |
| Homocysteine, μmol/Lb | 11.70 (9.50–15.10) | 11.00 (9.10–14.00) | 12.70 (10.30–16.20)a | <.001 |
| Hyperhomocysteinemia, % | 1838 (70.29) | 942 (63.86) | 896 (78.60)a | <.001 |
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; FPG, fasting plasma glucose; HDL‐C, high‐density lipoprotein cholesterol; IQR, interquartile range; LDL‐C, low‐density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol.
Differed significantly from nonhypertension group.
Described by the median and interquartile range.
3.2. Relationship of homocysteine with hypertension and BPs
We used logistic regression analysis to evaluate the association of homocysteine with hypertension risk (Table 2). After adjustments for age, sex, BMI, FPG, smoking and drinking status, salt consumption, and family history of hypertension, an increased risk of hypertension was found to be significantly associated with homocysteine (odds ratio [OR], 1.52; 95% CI, 1.24–1.86).
Table 2.
Logistic regression analysis of the association of plasma homocysteine with hypertension risk
| Variable | Crude OR (95% CI) | P 1 | Adjusted ORa (95% CI) | P 2 |
|---|---|---|---|---|
| Homocysteine, μmol/Lb | 2.28 (1.87–2.77) | <.001 | 1.88 (1.50–2.37) | <.001 |
| Homocysteine <10 μmol/L | 1.0 (reference) | 1.0 (reference) | ||
| Homocysteine ≥10 μmol/L | 2.08 (1.74–2.48) | <.001 | 1.52 (1.24–1.86) | <.001 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Adjusted for age, sex, body mass index, smoking and drinking status, salt consumption, family history of hypertension, and fasting plasma glucose.
ln‐transformed homocysteine as a continuous variable.
We also estimated the relationships of homocysteine levels with BPs (Table 3) and found that higher homocysteine levels were significantly associated with elevated SBP and DBP. Specifically, the adjusted increases in SBP and DBP per unit increase of homocysteine (in ln‐transformed values) were 1.67 mm Hg (95% CI, 0.45–2.89) and 1.16 mm Hg (95% CI, 0.30–2.02), respectively.
Table 3.
Estimated absolute increase in blood pressure (mm Hg) with 95% CI per unit of homocysteine (in ln‐transformed values)
| βa | 95% CI | P Value | |
|---|---|---|---|
| Systolic blood pressure | 1.67 | 0.45–2.89 | .007 |
| Diastolic blood pressure | 1.16 | 0.30–2.02 | .009 |
Abbreviation: CI, confidence interval.
Adjusted for age, sex, body mass index, fasting plasma glucose, smoking and drinking status, salt consumption, family history of hypertension, and antihypertensive medication.
3.3. Interaction effects of homocysteine with conventional predisposing factors on hypertension and BPs
Four conventional predisposing factors (older age, overweight/obesity, dyslipidemia, and family history of hypertension) showed significant interactions with homocysteine on hypertension risk (Table S1 and Table 4). More specifically, the joint OR for older age and homocysteine was 5.45 (95% CI, 4.17–7.14), which is much greater than the independent ORs for older age (OR, 3.42; 95% CI, 2.46–4.77) and homocysteine (OR, 1.82, 95% CI, 1.37–2.44), with an RERI of 1.21 (95% CI, 0.07–2.35). Similarly, the RERI for homocysteine with overweight/obese, dyslipidemia, and family history of hypertension was 0.72 (95% CI, 0.07–1.36), 0.45 (95% CI, 0.06–0.85), and 1.87 (95% CI, 0.77–2.97), respectively. No significance was observed for the interactions of homocysteine with the other remaining five factors.
Table 4.
Interaction effects of hyperhomocysteinemia (homocysteinemia ≥10 μmol/L) with conventional predisposing factors on hypertension susceptibility
| Subgroup | Conventional predisposing factors | ORa (95% CI) | P 1 | RERIa (95% CI) | P 2 |
|---|---|---|---|---|---|
| Age, y | |||||
| nHcy | <60 | 1.0 (reference) | 1.21 (0.07–2.35) | .037 | |
| Hyperhomocysteinemia | <60 | 1.82 (1.37–2.44) | .001 | ||
| nHcy | ≥60 | 3.42 (2.46–4.77) | <.001 | ||
| Hyperhomocysteinemia | ≥60 | 5.45 (4.17–7.14) | <.001 | ||
| Sex | |||||
| nHcy | Female | 1.0 (reference) | 0.33 (−0.20 to 0.86) | .222 | |
| Hyperhomocysteinemia | Female | 1.45 (1.16–1.82) | .001 | ||
| nHcy | Male | 0.92 (0.56–1.51) | .740 | ||
| Hyperhomocysteinemia | Male | 1.70 (1.31–2.22) | <.001 | ||
| BMI | |||||
| nHcy | Normal | 1.0 (reference) | 0.72 (0.07–1.36) | .029 | |
| Hyperhomocysteinemia | Normal | 1.41 (1.05–1.89) | .022 | ||
| nHcy | Overweight/obese | 1.90 (1.37–2.63) | <.001 | ||
| Hyperhomocysteinemia | Overweight/obese | 3.03 (2.28–4.01) | <.001 | ||
| Dyslipidemia | |||||
| nHcy | No | 1.0 (reference) | 0.45 (0.06–0.85) | .026 | |
| Hyperhomocysteinemia | No | 1.26 (0.88–1.80) | .204 | ||
| nHcy | Yes | 1.01 (0.71–1.44) | .943 | ||
| Hyperhomocysteinemia | Yes | 1.72 (1.25–2.34) | .001 | ||
| Type 2 diabetes mellitus | |||||
| nHcy | No | 1.0 (reference) | 0.12 (−0.72 to 0.96) | .779 | |
| Hyperhomocysteinemia | No | 1.53 (1.23–1.90) | <.001 | ||
| nHcy | Yes | 1.40 (0.90–2.19) | .138 | ||
| Hyperhomocysteinemia | Yes | 2.05 (1.46–2.87) | <.001 | ||
| Family history of hypertension | |||||
| nHcy | No | 1.0 (reference) | 1.87 (0.77–2.97) | <.001 | |
| Hyperhomocysteinemia | No | 1.32 (1.02–1.70) | .032 | ||
| nHcy | Yes | 2.38 (1.70–3.33) | <.001 | ||
| Hyperhomocysteinemia | Yes | 4.57 (3.42–6.11) | <.001 | ||
| Drinking | |||||
| nHcy | Nondrinkers | 1.0 (reference) | 0.40 (−0.11 to 0.91) | .124 | |
| Hyperhomocysteinemia | Nondrinkers | 1.42 (1.13–1.79) | .003 | ||
| nHcy | Ever‐drinkers | 0.92 (0.62–1.39) | .702 | ||
| Hyperhomocysteinemia | Ever‐drinkers | 1.75 (1.29–2.37) | <.001 | ||
| Smoking | |||||
| nHcy | Nonsmokers | 1.0 (reference) | 0.18 (−0.36 to 0.72) | .514 | |
| Hyperhomocysteinemia | Nonsmokers | 1.47 (1.19–1.83) | <.001 | ||
| nHcy | Ever‐smokers | 0.70 (0.38–1.28) | .241 | ||
| Hyperhomocysteinemia | Ever‐smokers | 1.35 (0.97–1.88) | .074 | ||
| Salt | |||||
| nHcy | ≤6 g/d | 1.0 (reference) | 0.07 (−0.44 to 0.59) | .790 | |
| Hyperhomocysteinemia | ≤6 g/d | 1.58 (1.14–2.18) | .006 | ||
| nHcy | >6 g/d | 1.33 (0.95–1.87) | .100 | ||
| Hyperhomocysteinemia | >6 g/d | 1.98 (1.46–2.69) | <.001 | ||
Abbreviations: BMI, body mass index; CI, confidence interval; nHcy, normal plasma homocysteine levels; OR, odds ratio; RERI, relative excess risk due to interaction.
Adjusted for age, sex, body mass index, smoking and drinking status, salt consumption, family history of hypertension, and fasting plasma glucose.
We also observed that family history of hypertension and BMI modified the associations between homocysteine levels (in ln‐transformed values) and BPs (all P interaction <.05) (Table S2 and Table 5). Specifically, the increases in SBP and DBP per unit increment of homocysteine were 2.59 mm Hg (95% CI, 0.26–4.92) and 2.46 mm Hg (95% CI, 0.78–4.14), respectively, in patients with a family history of hypertension. However, the corresponding increases in SBP and DBP were 1.27 (95% CI, −0.16 to 2.70) and 0.61 (95% CI, −0.38 to 1.60), respectively, in participants without a family history of hypertension. Likewise, the increase in DBP per unit increment of homocysteine in the overweight/obese subgroup was 2.30 mm Hg (95% CI, 1.03–3.58), whereas the estimate was 0.04 mm Hg (95% CI, −0.12 to 1.20) in patients of normal weight.
Table 5.
Estimated absolute increase in blood pressure (mm Hg) with 95% CI per unit of homocysteine (in ln‐transformed values) in subgroups
| Conventional predisposing factors | Category | Systolic blood pressure | Diastolic blood pressure | ||||
|---|---|---|---|---|---|---|---|
| βa | 95% CI | P interaction | βa | 95% CI | P interaction | ||
| Age | <60 y | 1.33 | −0.47 to 3.13 | .412 | 1.23 | −0.05 to 2.50 | .108 |
| ≥60 y | 2.76 | 1.12–4.41 | 1.06 | −0.08 to 2.20 | |||
| Sex | Female | 1.71 | −0.44 to 3.46 | .066 | 0.99 | −0.20 to 2.17 | .576 |
| Male | 1.20 | −0.47 to 2.87 | 1.16 | −0.14 to 2.46 | |||
| BMI | Normal | 1.85 | 0.15–3.56 | .191 | 0.04 | −0.12 to 1.20 | .022 |
| Overweight/obese | 1.38 | −0.36 to 3.13 | 2.30 | 1.03–3.58 | |||
| Dyslipidemia | No | 0.97 | −1.28 to 3.21 | .065 | 0.04 | −1.52 to 1.60 | .101 |
| Yes | 2.06 | 0.58–3.54 | 1.71 | 0.66–2.76 | |||
| Type 2 diabetes mellitus | No | 1.75 | 0.46–3.04 | .297 | 1.20 | 0.29–2.11 | .866 |
| Yes | 1.89 | −1.76 to 5.54 | 1.52 | −1.17 to 4.21 | |||
| Family history of hypertension | No | 1.27 | −0.16 to 2.70 | .045 | 0.61 | −0.38 to 1.60 | .021 |
| Yes | 2.59 | 0.26–4.92 | 2.46 | 0.78–4.14 | |||
| Drinking | Nondrinkers | 2.22 | 0.74–3.70 | .264 | 1.02 | −0.01 to 2.05 | .797 |
| Ever‐drinkers | 0.14 | −1.99 to 2.26 | 1.31 | −0.27 to 2.87 | |||
| Smoking | Nonsmokers | 1.79 | 0.39–3.19 | .396 | 1.09 | 0.12–2.06 | .872 |
| Ever‐smokers | 0.73 | −1.77 to 3.23 | 1.08 | −0.86 to 3.01 | |||
| Salt | ≤6 g/d | 1.81 | −0.09 to 3.72 | .679 | 1.10 | −0.27 to 2.47 | .386 |
| >6 g/d | 1.63 | 0.04–3.23 | 1.30 | 0.18–2.42 | |||
Abbreviations: BMI, body mass index; CI, confidence interval.
Adjusted for age, sex, body mass index, fasting plasma glucose, smoking and drinking status, salt consumption, family history of hypertension, and antihypertensive medication.
4. DISCUSSION
In this study, we found significant and positive associations of homocysteine concentrations with hypertension susceptibility and SBP and DBP levels in a northeastern Chinese population. The associations were stronger among participants who were older, overweight/obese, had dyslipidemia, or had a family history of hypertension, indicating that homocysteine acts synergistically with these factors to exert additive effects on arterial BPs.
The relationships of homocysteine with hypertension and/or BPs have received a great deal of attention during the past 2 decades. A positive correlation has been reported in some but not all prior studies.15, 16, 17, 18 For instance, the Hordaland Homocysteine Study found that homocysteine was positively associated with BPs in Norwegians.15 Similarly, data from the Third National Health and Nutrition Examination Survey (NHANES III) demonstrated that a 5‐μmol/L increment in plasma homocysteine levels was associated with mean increases of 1.3 mm Hg in DBP and of 3.5 mm Hg in SBP.18 In addition, a recent Chinese study observed that homocysteine was independently associated with an increased risk of hypertension and elevated arterial BPs.10, 11 Our findings were consistent with the prior studies mentioned above. Furthermore, our findings were also supported by several previous clinical trials, which indicated that antihomocysteine therapy (eg, folic acid supplementation) was effective in reducing BPs and the risk of cardiovascular diseases.33, 34 For example, a meta‐analysis of 12 randomized controlled clinical trials found that supplementation with 5000 to 10 000 μg/d of folate for at least 6 weeks could lower SBP by 2.03 mm Hg.33 In parallel, a recent meta‐analysis of 30 randomized controlled trials by Li and colleagues34 showed a 10% and 4% reduced risk of stroke and overall cardiovascular disease, respectively, with folic acid supplementation.
However, the Framingham Heart Study showed that the baseline plasma homocysteine levels were not significantly associated with hypertension incidence or longitudinal BPs progression,17 and the results were corroborated by the subsequent study conducted among an American population.35 In addition, a 2‐year follow‐up study in China revealed that there was an approximately U‐shaped distribution of hypertension risk with plasma homocysteine levels quartiles.18 Many factors may contribute to the inconsistencies between our and those previous studies. It is possible that the associations may be confounded by the effects of other factors, such as age, sex, dietary habits, and lifestyle.
In this study, we further performed formal interaction analyses and found that the effects of homocysteine on hypertension were stronger among participants who were older, overweight/obese, and had dyslipidemia or a family history of hypertension. The corresponding RERIs for the interactions of homocysteine with age, BMI, dyslipidemia, and family history of hypertension were 1.21, 0.72, 0.45, and 1.87, respectively. It is difficult to compare our results with other studies because this is the first study to report significant interactions of homocysteine with these factors on hypertension. Also, the precise mechanisms underlying these novel findings are not clear. Older age is not only a risk factor for hypertension but can also increase homocysteine levels via changing renal function, decreasing vitamin levels, and impairing renal metabolism of homocysteine.12, 36, 37, 38 Thus, older age may exacerbate the effect of elevated homocysteine on hypertension risk. Being overweight/obese could increase hypertension risk by inducing insulin resistance, impairing endothelial dysfunction, and increasing sodium retention.39 These pathophysiological mechanisms were also shared by elevated homocysteine levels in causing hypertension.12, 13, 14 Several epidemiological studies observed that overweight/obese patients had higher homocysteine levels than patients of normal weight.40 A body of evidence has also suggested that higher homocysteine levels could contribute to the development of obesity via epigenetic control of gene expression in the regulation of body fat storage.41, 42 Therefore, it is hypothesized that overweight/obese people would be more susceptible to the adverse health effects of elevated homocysteine levels. Evidence from experimental and epidemiological studies has suggested that homocysteine was positively associated with dyslipidemia.40, 41, 42, 43, 44, 45, 46 Thus, elevated homocysteine levels and dyslipidemia may share several common biological pathways (including increased arterial stiffness and induced oxidative stress) in stimulating the development of hypertension.47, 48 In spite of these speculations, there is still a lack of direct evidence on the biological basis for the above interactions. Further, in addition to interactive effects, homocysteine and these conventional predisposing factors can also influence the development of hypertension and BPs independently. For example, the independent ORs for homocysteine and family history of hypertension were 1.32 and 2.38, respectively. This indicates that although the two factors (homocysteine and family history of hypertension) might share several common mechanisms in elevating BPs, each of them may also have independent pathway(s) towards hypertension. Therefore, future well‐designed studies are still needed to uncover the exact mechanisms of these interactions.
We did not observe any interactions of homocysteine with sex, type 2 diabetes mellitus, salt consumption, and smoking and drinking status. In agreement with our findings, the Framingham Heart Study17 and the Kailuan Study18 found that there was no interaction of homocysteine with smoking and diabetes mellitus on incident hypertension or BP progression. However, NHANES III showed that the homocysteine‐sex interaction on SBP was statistically significant, and that alcohol intake slightly strengthened the homocysteine‐SBP association in women.16 In addition, Kennedy and colleagues20 found that plasma homocysteine levels were positively correlated with SBP and DBP in smokers but not in nonsmokers. Homocysteine has been considered an established risk factor for impaired glucose tolerance, altered fasting glucose, or type 2 diabetes mellitus.49, 50 Further, a recent large cross‐sectional study in northeastern China reported that homocysteine increased the prevalence of hypertension in subgroups of individuals with diabetes mellitus.19 These inconsistencies between our and the above published studies may be caused by differences in diagnostic criteria for hyperhomocysteinemia, smoking and drinking habits, study design, genetic backgrounds, and dietary habits.
5. STUDY LIMITATIONS
Although our study provides new insight into the association between homocysteine and hypertension susceptibility, it has several limitations that deserve comment. First, the present study could not establish cause inference because of the cross‐sectional design. Second, our study had a low percentage of men (33.96%). However, we performed additional power calculations and observed that the statistical power in men was 93.3%. Moreover, in all linear and logistic regression analyses of the present study, sex was adjusted as a potential confounding factor. Therefore, the relatively small sample size of men may have little impact on our estimates. Third, we used a questionnaire to collect smoking, drinking, and salt consumption information, which might have caused recall biases. Fourth, information on potential confounders such as renal function, thyroid function, riboflavin vitamin intake (such as folic acid), and polymorphisms of genes involved in the metabolism of homocysteine were not available in our study, which might have impacted the accuracy of our estimation on homocysteine and BPs. Finally, although we observed that homocysteine and several conventional predisposing factors can independently and interactively exert effects on hypertension and BPs, these effects were only modest. For example, the results showed that mean homocysteine levels in the normotension group were >10 μmol/L, although the prevalence of homocysteine in the hypertension group was significantly higher (78.6%) than that in the normotension group (63.9%). Therefore, it should be greatly cautioned in interpreting our findings.
6. STUDY STRENGTHS
Despite the limitations, our study has several advantages. First, to the best of our knowledge, our findings provide the first evidence on the joint effects of homocysteine with age, overweight/obesity, family history of hypertension, and dyslipidemia on hypertension predisposition. Second, the study has a relatively large sample size, which enhances the statistical power. Third, in addition to stratified analyses, we applied formal interaction analysis, which made our statistics more robust.
7. CONCLUSIONS
Our study indicates that an increase in homocysteine level was associated with elevated hypertension risk and BP among a Northern Chinese population. In addition, we found that homocysteine may act synergistically with age, overweight/obesity, dyslipidemia, and family history of hypertension to modify the development of hypertension and elevated BPs. Thus, the intriguing series of interactive effects on hypertension and BPs should incite intervention studies on the effect of homocysteine‐lowering therapy (such as folic acid fortification), motivate individuals to adopt a healthy lifestyle (such as losing weight and consuming a low‐fat diet), and influence design and analysis of future studies on homocysteine levels with hypertension. Replication in Chinese and other populations as well as further mechanistic studies are needed to validate and explain our findings.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Supporting information
ACKNOWLEDGMENTS
The authors gratefully acknowledge the assistance and cooperation of the faculty and staff of Shenhe Center for Disease Control and Prevention and thank all of the participants in our study. The authors also thank Prarthana Nair in China Medical University for her elaborative reviewing of this manuscript and useful suggestions on language use. This study was supported by a grant from the Educational Department of Liaoning Province (No. 20131015900).
Yang B, Fan S, Zhi X, et al. Interactions of homocysteine and conventional predisposing factors on hypertension in Chinese adults. J Clin Hypertens. 2017;19:1162–1170. 10.1111/jch.13075
Yang and Fan contributed equally to this work.
REFERENCES
- 1. Lawes CM, Vander HS, Rodgers A; International Society of Hypertension . Global burden of blood‐pressure‐related disease, 2001. Lancet. 2008;371:1513‐1518. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization. 2010. (NLM classification: WT 500). http://www.who.int/. Accessed June 1, 2016. [Google Scholar]
- 3. World Health Organization . Toward a healthy and harmonious life in china: stemming the rising tide of non‐communicable disease. Geneva, Switzerland: World Health Organization; 2011. http://apps.who.int/. Accessed June 1, 2016. [Google Scholar]
- 4. Biino G, Parati G, Concas MP, et al. Environmental and genetic contribution to hypertension prevalence: data from an epidemiological survey on Sardinian genetic isolates. PLoS ONE. 2013;8:e59612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;386:801‐812. [DOI] [PubMed] [Google Scholar]
- 6. Catena C, Colussi G, Nait F, Capobianco F, Sechi LA. Elevated homocysteine levels are associated with the metabolic syndrome and cardiovascular events in hypertensive patients. Am J Hypertens. 2015;28:943‐950. [DOI] [PubMed] [Google Scholar]
- 7. Catena C, Colussi G, Uri‐Michitsch M, Nait F, Sechi LA. Subclinical carotid artery disease and plasma homocysteine levels in patients with hypertension. J Am Soc Hypertens. 2015;9:167‐175. [DOI] [PubMed] [Google Scholar]
- 8. Yang B, Fan S, Zhi X, et al. Prevalence of hyperhomocysteinemia in China: a systematic review and meta‐analysis. Nutrients. 2014;7:74‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Adachi H, Matsuoka H, Usui M, Imaizumi T. Homocysteine and hypertension. Nihon Rinsho. 2000;58(suppl 2):S415‐S417. [PubMed] [Google Scholar]
- 10. Sengwayo D, Moraba M, Motaung S. Association of homocysteinaemia with hyperglycaemia, dyslipidaemia, hypertension and obesity. Cardiovasc J Afr. 2013;24:265‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li Z, Guo X, Chen S. Hyperhomocysteinemia independently associated with the risk of hypertension: a cross‐sectional study from rural China. J Hum Hypertens. 2016;30:508‐512. [DOI] [PubMed] [Google Scholar]
- 12. Tayama J, Munakata M, Yoshinaga K, Toyota T. Higher plasma homocysteine concentration is associated with more advanced systemic arterial stiffness and greater blood pressure response to stress in hypertensive patients. Hypertens Res. 2006;29:403‐409. [DOI] [PubMed] [Google Scholar]
- 13. Fujimi K, Uehara Y, Abe S, et al. Homocysteine‐induced oxidative stress upregulates chymase in mouse mastocytoma cells. Hypertens Res. 2010;33:149‐154. [DOI] [PubMed] [Google Scholar]
- 14. Kato N, Loh M, Takeuchi F, et al. Trans‐ancestry genome‐wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation. Nat Genet. 2015;47:1282‐1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nygård O, Vollset SE, Refsum H, et al. Total plasma homocysteine and cardiovascular risk profile. The Hordaland Homocysteine Study. JAMA. 1995;274:1526‐1533. [DOI] [PubMed] [Google Scholar]
- 16. Lim U, Cassano PA. Homocysteine and blood pressure in the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2002;156:1105‐1113. [DOI] [PubMed] [Google Scholar]
- 17. Sundström J, Sullivan L, D'Agostino RB, et al. Plasma homocysteine, hypertension incidence, and blood pressure tracking: the Framingham Heart Study. Hypertension. 2003;42:1100‐1105. [DOI] [PubMed] [Google Scholar]
- 18. Wang Y, Chen S, Yao T, et al. Homocysteine as a risk factor for hypertension: a 2‐year follow‐up study. PLoS ONE. 2014;9:e108223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li Z, Guo X, Chen S, et al. Hyperhomocysteinemia independently associated with the risk of hypertension: a cross‐sectional study from rural China. J Hum Hypertens. 2016;30:508‐512. [DOI] [PubMed] [Google Scholar]
- 20. Kennedy BP, Farag NH, Ziegler MG, Mills PJ. Relationship of systolic blood pressure with plasma homocysteine: importance of smoking status. J Hypertens. 2003;21:1307‐1312. [DOI] [PubMed] [Google Scholar]
- 21. Wang D, He Y, Li YP, et al. Dietary patterns and hypertension among Chinese adults: a nationally representative cross‐sectional study. BMC Public Health. 2011;11:925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhu WL, Dao JJ, Cheng J, et al. Relations between serum homocysteine and folic acid levels with congenital heart disease. J Hyg Res. 2005;6:740‐743. [PubMed] [Google Scholar]
- 23. Hao L, Ma J, Stampfer MJ, et al. Geographical, seasonal and gender differences in folate status among Chinese adults. J Nutr. 2003;133:3630‐3635. [DOI] [PubMed] [Google Scholar]
- 24. Gu DF, Reynolds K, Wu XG, et al. Prevalence of metabolic syndrome and overweight among adults in China. Lancet. 2005;365:1398‐1405. [DOI] [PubMed] [Google Scholar]
- 25. Gu DF, Gupta A, Muntner P, et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: Results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia). Circulation. 2005;112:658‐665. [DOI] [PubMed] [Google Scholar]
- 26. Fan S, Yang B, Zhi X, et al. Interactions of methylenetetrahydrofolate reductase C677T polymorphism with environmental factors on hypertension susceptibility. Int J Environ Res Public Health. 2016;13(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang YX, Zhang HM. Introduction to the dietary guidelines (2016) of Chinese. Acta Nutr Sin. 2016;38:209‐217. [Google Scholar]
- 28. Kirkendall WM, Feinleib M, Freis ED, Mark AL. Recommendations for human blood pressure determination by sphygmomanometers. Subcommittee of the AHA Postgraduate Education Committee. Hypertension. 1981;3:510A‐519A. [PubMed] [Google Scholar]
- 29. Working Group on Obesity Problem in China (WGDC) . The guidelines on the prevention and management of overweight and obesity in adults: China. Acta Nutr Sin. 2004;1:1‐4. [Google Scholar]
- 30. Li WX, Lv WW, Dai SX, Pan ML, Huang JF. Joint associations of folate, homocysteine and MTHFR, MTR and MTRR gene polymorphisms with dyslipidemia in a Chinese hypertensive population: a cross‐sectional study. Lipids Health Dis. 2015;14:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486‐2497. [DOI] [PubMed] [Google Scholar]
- 32. Wang Y, Li X, Qin X, et al. Prevalence of hyperhomocysteinaemia and its major determinants in rural Chinese hypertensive patients aged 45–75 years. Br J Nutr. 2013;109:1284‐1293. [DOI] [PubMed] [Google Scholar]
- 33. McRae MP. High‐dose folic acid supplementation effects on endothelial function and blood pressure in hypertensive patients: a meta‐analysis of randomized controlled clinical trials. J Chiropr Med. 2009;8:15‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li Y, Huang T, Zheng Y, Muka T, Troup J, Hu FB. Folic acid supplementation and the risk of cardiovascular diseases: a meta‐analysis of randomized controlled trials. J Am Heart Assoc. 2016;5:e003768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bowman TS, Gaziano JM, Stampfer MJ, Sesso HD. Homocysteine and risk of developing hypertension in men. J Hum Hypertens. 2006;20:631‐634. [DOI] [PubMed] [Google Scholar]
- 36. Guttormsen AB, Ueland PM, Svarstad E, Refsum H. Kinetic basis of hyperhomocysteinemia in patients with chronic renal failure. Kidney Int. 1997;52:495‐502. [DOI] [PubMed] [Google Scholar]
- 37. Selhub J, Jacques PF, Wilson PW, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993;270:2693‐2698. [DOI] [PubMed] [Google Scholar]
- 38. Refsum H, Nurk E, Smith AD, et al. The Hordaland Homocysteine Study: a community‐based study of homocysteine, its determinants, and associations with disease. J Nutr. 2006;136(6 suppl):1731S‐1740S. [DOI] [PubMed] [Google Scholar]
- 39. Kotchen TA. Obesity‐related hypertension: epidemiology, pathophysiology, and clinical management. Am J Hypertens. 2010;23:1170‐1178. [DOI] [PubMed] [Google Scholar]
- 40. Marchesini G, Manini R, Bianchi G, et al. Homocysteine and psychological traits: a study in obesity. Nutrition. 2002;18:403‐407. [DOI] [PubMed] [Google Scholar]
- 41. Terruzzi I, Senesi P, Fermo I, Lattuada G, Luzi L. Are genetic variants of the methyl group metabolism enzymes risk factors predisposing to obesity? J Endocrinol Invest. 2007;30:747‐753. [DOI] [PubMed] [Google Scholar]
- 42. Williams KT, Schalinske KL. New insights into the regulation of methyl group and homocysteine metabolism. J Nutr. 2007;137:311‐314. [DOI] [PubMed] [Google Scholar]
- 43. Woo CW, Siow YL, Pierce GN, et al. Hyperhomocysteinemia induces hepatic cholesterol biosynthesis and lipid accumulation via activation of transcription factors. Am J Physiol Endocrinol Metab. 2005;288:E1002‐E1010. [DOI] [PubMed] [Google Scholar]
- 44. Hirche F, Schroder A, Knoth B, Stangl GI, Eder K. Methionine‐induced elevation of plasma homocysteine concentration is associated with an increase of plasma cholesterol in adult rats. Ann Nutr Metab. 2006;50:139‐146. [DOI] [PubMed] [Google Scholar]
- 45. O K, Lynn EG, Chung YH, Siow YL, Man RY, Choy PC. Homocysteine stimulates the production and secretion of cholesterol in hepatic cells. Biochim Biophys Acta. 1998;1393:317‐324. [DOI] [PubMed] [Google Scholar]
- 46. Liu Y, Li K, Venners SA, et al. Individual and joint associations of methylenetetrahydrofolate reductase C677T genotype and plasma homocysteine with dyslipidemia in a chinese population with hypertension. Clin Appl Thromb Hemost. 2017;23:287‐293. [DOI] [PubMed] [Google Scholar]
- 47. Tsai JC, Kuo HT, Chiu YW, et al. Correlation of plasma homocysteine level with arterial stiffness and pulse pressure in hemodialysis patients. Atherosclerosis. 2005;182:121‐127. [DOI] [PubMed] [Google Scholar]
- 48. Benetos A, Waeber B, Izzo J, et al. Influence of age, risk factors, and cardiovascular and renal disease on arterial stiffness: clinical applications. Am J Hypertens. 2002;15:1101‐1108. [DOI] [PubMed] [Google Scholar]
- 49. Huang T, Ren J, Huang J, Li D. Association of homocysteine with type 2 diabetes: a meta‐analysis implemention Mendelian randomization approach. BMC Genom. 2013;14:867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sudchada P, Saokaew S, Sridetch S, Incampa S, Jaiyen S, Khaithong W. Effect of folic acid supplementation on plasma total homocysteine levels and glycemic control in patients with type 2 diabetes: a systematic review and meta‐analysis. Diabetes Res Clin Pract. 2012;98:151‐158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


