Abstract
Introduction
This double-blind, randomised controlled trial (RCT) aims to estimate the effect of a physiotherapist-led intervention with targeted strengthening compared with a physiotherapist-led intervention with standardised stretching, on hip-related quality of life (QOL) or perceived improvement at 6 months in people with femoroacetabular impingement (FAI) syndrome. We hypothesise that at 6 months, targeted strengthening physiotherapist-led treatment will be associated with greater improvements in hip-related QOL or greater patient-perceived global improvement when compared with standardised stretching physiotherapist-led treatment.
Methods and analysis
We will recruit 164 participants with FAI syndrome who will be randomised into one of the two intervention groups, both receiving one-on-one treatment with the physiotherapist over 6 months. The targeted strengthening physiotherapist-led treatment group will receive a personalised exercise therapy and education programme. The standardised stretching physiotherapist-led treatment group will receive standardised stretching and personalised education programme. Primary outcomes are change in hip-related QOL using International Hip Outcome Tool-33 and patient-perceived global improvement. Secondary outcomes include cost-effectiveness, muscle strength, range of motion, functional task performance, biomechanics, hip cartilage structure and physical activity levels. Statistical analyses will make comparisons between both treatment groups by intention to treat, with all randomised participants included in analyses, regardless of protocol adherence. Linear mixed models (with baseline value as a covariate and treatment condition as a fixed factor) will be used to evaluate the treatment effect and 95% CI at primary end-point (6 months).
Ethics and dissemination
The study protocol was approved (La Trobe University Human Ethics Committee (HEC17-080)) and prospectively registered with the Australian New Zealand Clinical Trials Registry. The findings of this RCT will be disseminated through peer reviewed scientific journals and conferences. Patients were involved in study development and will receive a short summary following the completion of the RCT.
Trial registration number
ACTRN12617001350314
Keywords: hip, sports medicine, rehabilitation medicine
Strengths and limitations of this study.
This prospective, double-blind randomised controlled trial (RCT) is the first full-scale study to test a head-to-head comparison of two exercise-based physiotherapist-led interventions for femoroacetabular impingement (FAI) syndrome.
Patient-reported outcomes will be collected at clinically relevant time points and allows analysis of outcomes that are important to patients.
Cost-effectiveness analysis will inform clinical decision making.
This physiotherapist-led RCT has the potential to reduce the burden of FAI syndrome and, if shown to be efficacious, may become the preferred first treatment choice for FAI syndrome.
The blinding of participants and assessors provides the highest level of rigour to test the efficacy of the physiotherapist-led intervention.
Introduction
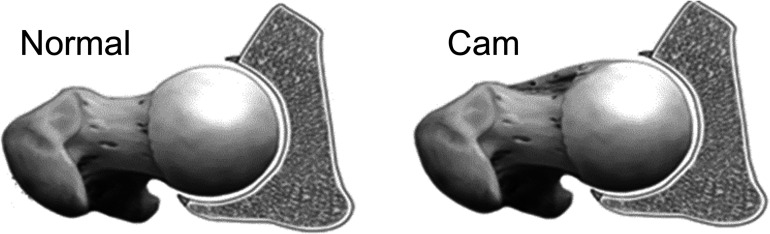
Musculoskeletal conditions, such as hip-related pain,1 are the leading causes of pain and disability in the community, and one of the largest global contributors to years lived with a disability.2 Femoroacetabular impingement (FAI) syndrome is a common cause of hip-related pain in adults,3 and evident in 49% of young and middle-aged adults with hip-related pain.4 It is diagnosed with a triad of imaging findings, patient reported hip-related symptoms, and clinical signs that are associated with excessive bone formation at the femoral head-neck junction (figure 1). The most commonly reported altered bony shape is cam morphology, which describes excessive bone formation at the femoral head–neck junction.5 Cam morphology may lead to aberrant joint forces during functional movements in the position of hip impingement (primarily involving flexion, rotation and abduction or adduction), and subsequent damage to the articular cartilage of the hip joint.6
Figure 1.
Diagrammatic representation of cam morphology at the femoral head–neck junction.54
While most studies focus on musculoskeletal pain affecting the elderly (eg, osteoarthritis), there is compelling and increasing evidence that FAI syndrome in younger adults (eg, aged 18–50 years) creates a substantial burden in society,7 8 associated with persistent hip-related pain and symptoms,9 impaired physical function,10 reduced sports and physical activity participation, and impaired quality of life (QOL). The burden of FAI syndrome is amplified by the high daily physical demands (eg, occupational, familial responsibilities and recreational activities) encountered by younger adults.
Treatment options for FAI syndrome can be surgical or non-surgical.11 Non-surgical approaches are recommended as the first line options for other musculoskeletal pain conditions (evident from clinical guidelines for osteoarthritis,12 low back pain13 and chronic whiplash associated disorders,14) due to the higher costs and risks associated with surgery. Recently published randomised controlled trials (RCTs) comparing hip arthroscopic surgery to physiotherapist-led interventions for FAI syndrome found small15 16 to moderate17 between-group differences favouring hip arthroscopy, with a greater cost and risk of adverse events associated with surgery.15–17 The physiotherapist-led interventions used for comparison to hip arthroscopy involved diverse exercise interventions including stretching, motor control, core stability and strengthening and provided varied detail regarding the individualisation and the content of the exercise interventions. Hence, the specific components of exercise programmes that are effective are not known. A recent consensus meeting recommended individualised, exercise-based interventions as the first-line treatment for young adults with hip-related pain, however, no recommendation was made regarding one type of exercise over another.11 Such a recommendation could not be provided because of the absence of a full-scale RCT comparing the head-to-head effectiveness of different exercise-based, physiotherapist-led interventions for FAI syndrome.18–20 Thus, a physiotherapist-led intervention that compares exercise interventions needs to be developed and tested.
Therefore, the primary aim of this RCT is to estimate the effect of a physiotherapist-led intervention with targeted strengthening compared with a physiotherapist-led intervention with standardised stretching in 164 participants with FAI syndrome on hip-related QOL (International Hip Outcome Tool 33 (iHOT-33)) or patient-perceived global improvement at 6-months.21 We hypothesise that, compared with the standardised stretching physiotherapist-led intervention, the targeted strengthening physiotherapist-led intervention will result in greater improvement in: (1) hip-related QOL or (2) perceived improvement. Secondary aims are to measure: (1) the cost-effectiveness of the targeted strengthening physiotherapist-led intervention compared with the standardised stretching physiotherapist-led intervention; (2) the effects of targeted strengthening physiotherapist-led intervention on physical activity levels; (3) the effects of targeted strengthening physiotherapist-led intervention on hip strength; and explore (4) the effects of targeted strengthening physiotherapist-led intervention on hip biomechanics and (5) the effects of targeted strengthening physiotherapist-led intervention on hip joint structure.
Methods
Participants
This participant and assessor-blinded superiority RCT aligns with the Standard Protocol Items: Recommendations for Interventional Trials guidelines.22 We will recruit 164 participants from the general community in urban (greater Melbourne) and regional Victoria (Ballarat) (Australia) with a history of hip-related pain. The recruited cohort will be randomised into two parallel intervention groups. Block randomisation will be utilised with a 1:1 ratio, with the primary end-points of hip-related QOL and patient-perceived improvement after 6 months. Ethics approval obtained through the La Trobe University Human Ethics Committee (HEC 17–080).
Inclusion and exclusion criteria
Eligibility for this RCT was based on clinical and radiographic features,3 which were used in our previous pilot RCT for FAI syndrome.6
Inclusion criteria: (1) aged 18–50 years; (2) hip-related (anterior hip or groin) pain which is aggravated by prolonged sitting or hip movements into positions of impingement3; (3) hip-related pain ≥3/10 on numerical pain scale for ≥6 weeks; (4) cam morphology (defined as radiographic alpha angle ≥60°),21 as described below and (5) a positive flexion-adduction-internal rotation test.
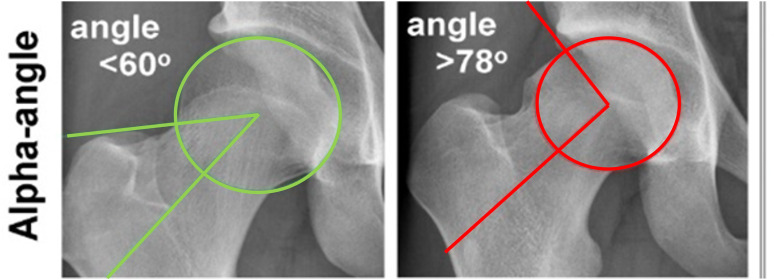
The alpha angle represents the sphericity of the femoral head and is used to identify and then quantify cam morphology if greater than 60° (figure 2). To determine the presence of cam morphology, the potential participants will undergo a standing anteroposterior (AP) and Dunn 45° radiograph, following a standardised protocol.3 21 Following previously described methods,5 the alpha angle will be calculated by one examiner (JLK) using both the AP and the Dunn 45° radiographs, to quantify the asphericity of the femoral head.
Figure 2.
Alpha angle measurement from AP radiograph.21 AP, anteroposterior.
Exclusion criteria: (1) physiotherapy treatment for the hip in the past 3 months; (2) previous hip or back surgery; (3) planned lower limb surgery in the following year; (4) radiographic hip osteoarthritis (Kellgren and Lawrence score ≥2,23 representing moderate to severe hip osteoarthritis); (5) intra-articular hip–joint injection in the previous 3 months; (6) neurological, other MSK or systemic arthritis conditions including other significant musculoskeletal conditions where FAI syndrome was not considered to be the primary cause of hip pain; (7) unable to perform testing procedures; (8) unable to commit to a 6-month physiotherapy-led intervention or associated outcome assessments; (9) contraindications to X-ray (including self-reported pregnancy and pregnancy during the study) or (10) inability to understand English language.
Procedures
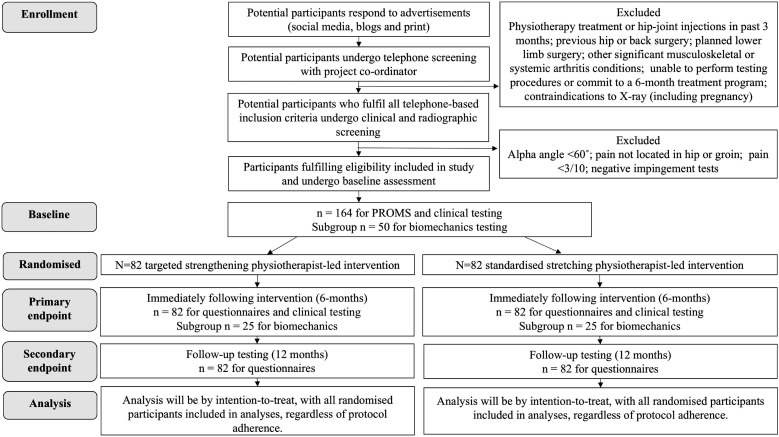
The study procedure flow chart is shown in figure 3. Following clinical and radiographic screening to confirm study eligibility, participants will attend La Trobe University or Lake Health Group, Victoria, Australia to complete written and informed consent. Demographic characteristics will be recorded, and baseline patient-reported outcome measures (PROMs) completed using an electronic data collection system (Promptus, Melbourne, Australia). Participants will undergo clinical and biomechanical assessment (where appropriate) of their hip by a blinded assessor at baseline and on study follow-up (6 months). MRI will be completed at baseline and 12 months follow-up. Participants will be blinded to the randomisation procedure.
Figure 3.
Study procedure flow chart. PROMs, patient-reported outcome measures.
Randomisation
Following baseline assessment, participants will be randomised into one of two intervention groups. To ensure concealed intervention allocation, we will use the telephone-based interactive voice response randomisation services (National Health and Medical Research Council Clinical Trials Centre, University of Sydney, Sydney, Australia). The randomisation schedule (blocks of 8–12) will be revealed to the unblinded assessor (JLK, RTRJ) after the baseline assessment, who will communicate intervention allocation to the participant’s study physiotherapist.
Blinding
As the primary outcomes are self-reported, participants are considered assessors; therefore, participants (and thus assessors) will be blinded to previous scores during the testing time points. Participants will be blinded to the physiotherapist-led interventions and consent will involve limited disclosure. Participants will become unblinded once the data analyses are complete. We do not expect that emergency unblinding will be required due to the very low incidence of adverse events seen in our pilot study of the same trial interventions.
Physiotherapist-led interventions
Study participants will receive one of two physiotherapist-led interventions (targeted strengthening physiotherapist-led treatment or standardised stretching physiotherapist-led treatment) across four clinical sites within Victoria (Australia). Registered physiotherapists will lead the two-phase intervention that will be delivered over a 6-month period and has been described using the Template for Intervention Description and Replication guidelines (table 1).24 Physiotherapists will be trained to deliver the intervention to both groups. Training of the physiotherapists will occur at the commencement of the study and annually thereafter. Treating physiotherapists will also be provided with written treatment manuals and training materials to refer to. In order to limit the likelihood of contamination between treatment groups, treating physiotherapists will be instructed to not have participants from different treatment groups attend the clinic at the same time. We have previously reported treating therapists’ beliefs that both interventions are credible.6 In order to maintain participant blinding, treating physiotherapists will be trained to deliver both interventions with equal enthusiasm. Each of the four clinical sites will have between three and five therapists trained, depending on clinic requirements. The treating physiotherapists were recruited from four large private physiotherapy clinics in Australia, and represent a typical therapist in an Australian private practice where people with FAI syndrome might seek care.
Table 1.
Intervention delivery described using the TIDieR guidelines for both groups
| Phase | What | Targeted strengthening physiotherapist-led treatment | Standardised stretching physiotherapist-led treatment |
| Phase 1. Month 0–3 | Who | Physiotherapists | |
| How | Face-to-face individual sessions | ||
| Where | Physiotherapy clinics (and clinic gyms) in Melbourne/Regional Victoria | ||
| When and how much | Fortnightly: 30 mins physiotherapy; and weekly: 30 mins supervised gym sessions. Exercises progressed based on assessment at each session | ||
| Tailoring | Tailored selection and progression of hip, trunk and functional strength exercises and manual therapy techniques Progressive, tailored physical activity programme |
Standardised non-specific stretching exercises Tailored education and standardised information on increasing physical activity |
|
| How well | Treatment response in files and adherence recorded in mobile phone app | ||
| Phase 2. Month 4–6 | What | Targeted strengthening physiotherapist-led treatment | Standardised stretching physiotherapist-led treatment |
| Who | Physiotherapists and local gymnasium | ||
| How | Face-to-face individual sessions and membership to gymnasium | ||
| Where | Physiotherapy clinics and gymnasiums Melbourne/Regional Victoria | ||
| When and how much | 3×30 min ‘top-up’ physio sessions at month 4, 5 and 6. 3 times weekly unsupervised gym attendance |
||
| Tailoring | Semistandardised with selection of exercise targeted to assessment | Standardised/non-specific stretching exercises | |
| How well | Treatment response in files and adherence recorded in mobile phone app | ||
TIDieR, Template for Intervention Description and Replication.
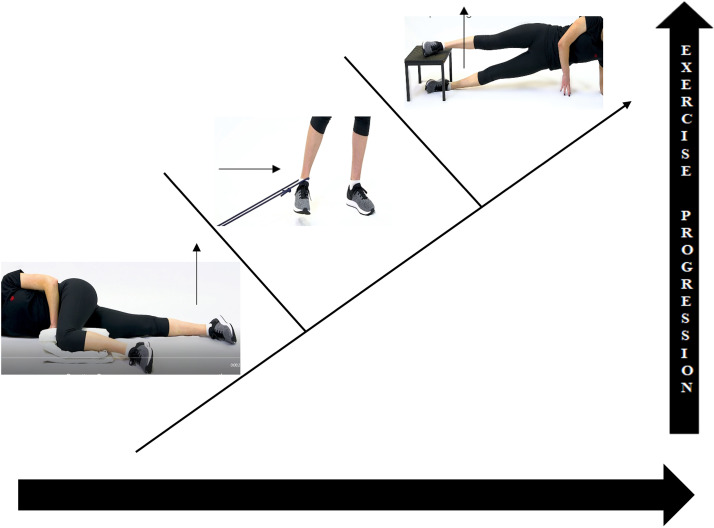
Targeted strengthening Physiotherapist-led treatment
A team of expert physiotherapists with extensive clinical experience in FAI syndrome management (all with >15 years of individual experience) designed both physiotherapist intervention programmes.25–29 The targeted strengthening physiotherapist-led treatment was developed based on knowledge of physical impairments observed in FAI syndrome,18 and a previous pilot study.6 The targeted strengthening physiotherapist-led intervention is personalised to the individual participant’s impairments and goals and has seven key elements: (1) progressive hip muscle strengthening exercises; (2) progressive trunk muscle strengthening exercises; (3) progressive functional exercises; (4) progressive plyometric exercises; (5) a progressive physical activity/return to sport programme; (6) a personalised education programme and (7) tailored manual therapy. Videos of all exercises in the targeted strengthening physiotherapist-led intervention can be found at (https://exercise.trekeducation.org/populations/lower-limb/). The targeted progressive hip and trunk strengthening exercises were designed using strength and conditioning guidelines outlined by the American College of Sports Medicine.30 Adherence to these guidelines aims to facilitate hip joint loading tolerance using exercise dosages, volume and progressions that will increase muscular strength hypertrophy and strength endurance. Full details of the targeted physiotherapist-led intervention programme are contained in online supplemental file 1. An example of how a participant may be provided with progressive targeted hip adductor strengthening exercises are presented in figure 4. The participants will use the Physitrack application (Physitrack, London, UK), a web-based application compatible with smartphones, tablets and computers, which provides photos, videos and instructions of prescribed exercises to be played in real time. Those unable to access the Physitrack application will be provided with paper-based pictures for exercise instruction.
Figure 4.
An example of how an individual participant is given progressive, targeted hip adductor strengthening exercises.
bmjopen-2020-041742supp001.pdf (359.8KB, pdf)
Standardised stretching physiotherapist-led intervention
The standardised stretching physiotherapist-led intervention consists of tailored health education, non-specific, standardised stretching, a standardised physical activity programme and manual therapy individualised to participants’ needs. In order to control for the psychosocial effects of therapist contact inherent with physiotherapy intervention, this programme will provide a credible alternative to physiotherapy exercises to reduce the possibility of resentful demoralisation. Stretching was chosen as our pilot work showed a smaller effect than a targeted strengthening intervention on hip-related QOL and muscle strength.6 (online supplemental file 2).
bmjopen-2020-041742supp002.pdf (159.1KB, pdf)
Delivery of both physiotherapist-led interventions
Phase 1
Zero to three months: (6 physiotherapist-led interventions (1 per fortnight); 12 supervised gym sessions (1 per week), with a further two unsupervised gym sessions encouraged per week).
Phase 2
Four to six months: Both intervention groups will receive a 3-month gym membership to continue with the unsupervised exercises independently. They will receive additional physiotherapy visits at months 4, 5 and 6 (ie, three in total), with the aim of increasing adherence to the unsupervised intervention All clinical-site physiotherapists will receive treatment manuals and undergo three group training sessions (theory and practical) in the delivery of both interventions. Treating physiotherapists will then deliver either intervention. Clinics will be audited annually for treatment fidelity.
Participant adherence to intervention, adverse events and concomitant care
Participants will choose to attend one of four physiotherapy clinics to minimise transport burden within Melbourne and regional Victoria. The lead researcher (JLK) will maintain regular contact with study participants via the online PROM system (via weekly questionnaires on treatment adherence) and the Physitrack app to monitor adverse responses to treatment.6 Any adverse events will be reported to the Human Research Ethics Committee. Participants will be asked to refrain from concomitant physiotherapist-led treatment, other musculoskeletal therapies (chiropractic care, osteopathy, myotherapy or similar) or exercise interventions for their hip pain during the study. Participants will be allowed to continue care for other unrelated pre-existing conditions. There are minimal known risks associated with the physioFIRST study interventions, as such the physioFIRST study will not have a formal data monitoring committee or plans for post-trial care, and does not require an interim analysis.
Measures to be collected
Measures to be collected will include primary and secondary outcomes, descriptive measures of the population, treatment modifiers and treatment mediators. These are listed with time points of collection in table 2.
Table 2.
Trial measures to be collected and their purpose
| PhysioFIRST time line | ||||||||||||||
| Measure | Purpose | Time point (months) collected | ||||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Descriptive measures | ||||||||||||||
| Age (years) | Describe population, treatment modifier | X | ||||||||||||
| Sex | Describe population, treatment modifier | X | ||||||||||||
| Height (m) | Describe population | X | ||||||||||||
| Body mass (kg) | Describe population | X | ||||||||||||
| Leg length (cm) | Describe population | X | ||||||||||||
| Waist and hip circumference (cm) | Describe population | X | ||||||||||||
| Pain provocation tests | ||||||||||||||
| Hip Internal Rotation Test | Describe population | X | X | |||||||||||
| Flexion/Adduction/Internal Rotation Test | Describe population | X | X | |||||||||||
| Bent Knee Fall Out | Describe population | X | X | |||||||||||
| Patient-reported outcome measures | ||||||||||||||
| International Hip Outcome Tool-33 | Primary outcome | X | X | X | X | X | ||||||||
| Patient-perceived global improvement | Primary outcome | X | X | X | X | |||||||||
| The Copenhagen Hip and Groin Outcome Score | Secondary outcome | X | X | X | X | X | ||||||||
| Workplace Activity Limitations Scale | Secondary outcome | X | X | X | X | X | ||||||||
| EuroQol- 5 Dimension 5-Level questionnaire (EQ-5D-5L) | Secondary outcome | X | X | X | X | X | ||||||||
| Pain Detect Questionnaire | Secondary outcome, treatment modifier | X | X | X | X | X | ||||||||
| Keele STarT MSK Tool | Secondary outcome, treatment modifier | X | X | X | X | X | ||||||||
| Tampa Scale for Kinesophobia | Secondary outcome, treatment mediator | X | X | X | X | X | ||||||||
| Hip strength tests | ||||||||||||||
| Hip Abduction (supine) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Hip Adduction (supine) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Hip Extension (prone) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Hip External Rotation (prone) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Hip Internal Rotation (prone) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Hip Flexion (sitting) | Secondary outcome, treatment mediator | X | X | |||||||||||
| Functional tests | ||||||||||||||
| Trunk Muscle Endurance (side lying) | Secondary outcome, treatment mediator | X | X | |||||||||||
| One Leg Rise | Secondary outcome, treatment mediator | X | X | |||||||||||
| Star excursion Balance Test | Secondary outcome | X | X | |||||||||||
| Hop for Distance | Secondary outcome | X | X | |||||||||||
| Single leg squat (video analysis) | Secondary outcome | X | X | |||||||||||
| Range of motion (degrees) | ||||||||||||||
| Hip Flexion | Secondary outcome | X | X | |||||||||||
| Hip External Rotation | Secondary outcome | X | X | |||||||||||
| Hip Internal Rotation | Secondary outcome | X | X | |||||||||||
| Imaging | ||||||||||||||
| Hip MRI cartilage | Secondary outcome, treatment modifier | X | X | |||||||||||
| Hip alpha angle | Describe population, treatment modifier | X | ||||||||||||
| Biomechanics tests | ||||||||||||||
| Walking | Secondary outcome | X | X | |||||||||||
| Y-Balance | Secondary outcome | X | X | |||||||||||
| Single Leg Squat | Secondary outcome | X | X | |||||||||||
| Running | Secondary outcome | X | X | |||||||||||
| Activity monitoring | ||||||||||||||
| Fitbit Activity Monitoring (2-week block) | Secondary outcome | X | X | X | X | |||||||||
| Cost-effectiveness | ||||||||||||||
| Incremental cost per Quality Adjusted Life Year | Secondary outcome | X | ||||||||||||
Descriptive measures of the population
Participant baseline demographic characteristics, such as age, sex, height, body mass leg length and waist and hip circumference, will be recorded. In addition, response to pain provocation tests will be recorded (online supplemental file 3).
bmjopen-2020-041742supp003.pdf (393.3KB, pdf)
Patient-reported outcome measures
Primary outcomes
We will collect multiple (two) primary outcomes.31
Hip-related QOL will be measured using the iHOT-33. The iHOT-33 questionnaire consists of 33 individual questions scored on a visual analogue scale from 0 (worst possible score) to 100 (best possible score). The iHOT-33 has acceptable psychometric properties and is recommended for use in active adults with hip-related pain.32 33 It has a low SE of measurement (six points),34 is responsive,35 with reported minimal clinically important differences ranging from 6 to 10 points35 and minimal detectable change (groups) of 2 points.34
Patient-perceived global improvement will be measured on a 7-point Likert scale (‘much improved’, ‘improved’, ‘a little improved’, ‘no change’, ‘a little worse’, ‘worse’, ‘much worse’). This is a clinically relevant tool for evaluating an individual patient’s perspective on meaningful improvement.36 For the analysis, patient-perceived global improvement will be used as a continuous scale.
Secondary outcomes
The Copenhagen Hip and Groin Outcome Score (HAGOS)37 is a self-reported questionnaire consisting of six subscales that evaluates dimensions of hip and/or groin pain including: pain, symptoms, physical function of daily living, physical function in sport and recreation, participation in physical activities and hip-related QOL. The HAGOS subscales are each scored out of 100 points (100=best possible score) has acceptable reliability and validity in young people with hip and groin pain.38
Workplace Activity Limitations Scale is a 12-item questionnaire that aims to identify arthritis-related activity limitations specific to various employment related tasks. Responses are made using a 4-point Likert scale and a total score is measured out of 33 (higher scores=more impairment).39
EQ-5D-5L (Registration ID 34190_TOU) is a reliable and valid measure of QOL.40 The EQ-5D-QL asks the participant to indicate their health state according to five dimensions that assess: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.40 41
Treatment modifiers
Pain Detect Questionnaire (PD-Q) evaluates the presence and severity of seven qualitative characteristics of pain, including: burning sensation, hyperesthesia, allodynia, shock-like, thermal, numbness and tenderness. Based on the participant’s self-reported scores, the likelihood for pain to be attributable to neuropathic factors is then classified as: (1) likely; (2) unlikely (and thus the pain type is identified as nociceptive) or (3) ambiguous (indicating the pain type is unclear and identified as having a mixed pattern).42 43 The PD-Q is a reliable screening questionnaire for pain types with intra-class correlation co-efficients (ICC’s) for measurement of pain intensities varying between 0.81 (95% CI 0.75 to 0.87) and 0.87 (95% CI 0.82 to 0.91).43
Keele STarT MSK Tool Clinical version contains 10 items that ask the participant about their function and disability, pain and coping, comorbidity and the impact of pain. Once scored, it places the patient into three categories based on their risk of a poor outcome (low, medium, high). This tool has moderate-to-good level predictive ability in the identification of patients who develop persistent disabling pain.44
Tampa scale for Kinesiophobia (TSK) consists of 17 statements which measure pain-related fear of movement in patients with chronic MSK pain.45 Each statement is provided with a 4-point Likert scale, and total scores range from 17 to 51, with a higher score indicating more fear of movement. The TSK demonstrates moderate reliability and validity when tested on patients with acute and chronic MSK pain.46 47
Physical impairment and functional outcome measures
Hip muscle strength will be measured with previously described methods,29 48 as a secondary outcome and as a treatment mediator. A full description of the hip muscle strength tests are contained in online supplemental file 3.
Range of motion tests and functional performance tests are secondary outcomes and will be measured using previously published standardised methods (online supplemental file 3).29 49 These tests of physical impairment will be measured at baseline and 6 months (table 2). The tests have excellent reliability (ICC=0.82–0.95)29 and were selected as they are frequently used in clinical practice and are associated with functional capacity of the hip and lower limb.6 50
Imaging measures
Radiographic hip alpha angle,21 as described above, will be used to describe the population and to determine its effect as a treatment modifier.
Hip joint cartilage structure at baseline will be quantified using the Scoring Hip Osteoarthritis with MRI (SHOMRI) semiquantitative scoring system on a subset of 50 participants (25 per group).51 The SHOMRI classification quantifies cartilage features in 10 subregions.51 The SHOMRI scoring system has excellent previously published intrareader and inter-reader reliability (ICC=0.91–0.97; κ: 0.55–0.79).51 This measure will be a secondary outcome and will also be used as a treatment modifier.
Hip biomechanics
Hip biomechanics will be secondary outcomes. Using three-dimensional motion analysis according to our previously described protocol,48 participants biomechanics during walking, running, the single leg squat and the y-balance test will be examined in a subset of 50 participants (25 per group) at baseline and at 6 months. Changes in hip biomechanics during these tasks will be measured. Details of the biomechanics testing procedures are contained in online supplemental file 4.
bmjopen-2020-041742supp004.pdf (103.5KB, pdf)
Physical activity
Physical activity (average daily step count over 14 days) is a secondary outcome and will be measured using the Fitbit Surge on a subset of 40 participants. The Fitbit Surge is a lightweight wrist worn device that tracks physical activity and has demonstrated reliability in people aged 18–50 years.52
Long-term follow-up
Participants will be invited to complete the PROMs listed in table 2 at annual intervals to 5 years, and then again at 10 years to enable the assessment of long-term predictors of outcome, and progression to hip surgery, including hip arthroscopy and hip arthroplasty.
Data management
Data quality will be ensured via practitioner training, assessing procedural quality and random checks of protocol adherence, data completeness and accuracy. Intervention adherence will be defined as completing ≥80% of the physiotherapist-led treatments and supervised gym sessions and will be tracked by the clinical site booking system and weekly questionnaires or the Physitrack app. All participants will be included in the intention to treat (ITT) analyses, including participants adhering to <80% of treatment and those participants who withdraw from the study.22
Sample size
A power calculation was conducted for this RCT, informed by data from our previous pilot study that used and compared a similar tailored strengthening intervention to a standardised stretching intervention.6 The MCID of the iHOT-33 is still uncertain in non-surgical patients with FAI syndrome and has only been estimated in hip arthroscopy cohorts.34 35 Therefore, the power calculation was based on the observed baseline SD and the between-group differences in the scores of our first primary outcome measure (hip-related QOL (iHOT-33)) from our pilot study (baseline SD=25 points; mean difference 15 points out of 100),6 which exceeded the previously reported MCID of 6–10 points.35 Our pilot trial6 observed a standardised mean difference (SMD) of 0.68 for the iHOT-33. We reduced the proposed SMD to 0.50 for this study to account for the small sample (n=24) in the pilot study, the similarities between the interventions and the difference in the expertise of treating physiotherapists in a full-scale study. This is consistent with previously reported between-group SMD for the second primary outcome (patient-perceived global improvement) of 0.50.53 Estimated sample sizes for a two-sample means t-test assuming 80% power, α=0.025 (accounting for both primary outcomes), results in a sample size estimate of 156 participants. To account for an estimated 5% drop-out due to the study duration, a recommended sample size of 164 participants (82 in each group) will be recruited in this RCT.
Statistical analyses
Data will be analysed using ITT, with all randomised participants included in analyses, regardless of protocol adherence. An experienced biostatistician (AJS) will perform blinded analyses of primary and secondary outcomes. The two primary endpoints chosen will be evaluated separately, such that a significant treatment effect against either of the endpoints will be taken as evidence of efficacy.31 Linear mixed models (with baseline value as a covariate and treatment condition as a fixed factor) will be used to evaluate the treatment effect and 95% CI at 3 and 6 months. Models will be adjusted for age and sex. In addition to the primary ITT analysis, sensitivity analyses for missing outcome data will be performed on multiple imputed datasets, and Complier Average Causal Effects methods will be used to estimate the treatment effect at full and partial levels of participation in addition to the primary ITT analysis.
For the primary analysis, patient-perceived global improvement will be assessed as a 7-point scale, with bootstrapped standard errors to account for non-normality of residuals. A secondary analysis will assess the between-group difference in the proportion of participants reporting being ‘much improved’ or ‘improved’, as an indicator of successful treatment outcome.
Exploratory moderation analysis will be conducted to determine the strength of evidence provided by the study that treatment effects are moderated by the factors outlined as potential moderators in table 2, by incorporating an interaction term between the potential moderator and the treatment group indicator in the linear mixed models for the ITT sample for the primary outcomes. Investigation of the mediation of the treatment effect for the primary outcomes for the ITT sample by the potential mediator variables outlined in table 2 will also be conducted. Standardised estimates of the mediated treatment effect with bootstrapped 95% CIs will be presented.
Cost-effectiveness (incremental cost per quality -adjusted life year)
The economic evaluation will estimate the incremental cost (healthcare system perspective) per quality-adjusted life year from the EQ-5D-QL assessment. Healthcare resource utilisation, including cointerventions for hip-related pain (eg, medicines, complementary treatments and details of hospital presentations), will be collected from several sources to facilitate data analysis, reporting, and corroboration. Data sources will include the Medicare and Pharmaceutical Benefits Scheme databases (includes rebated, private health insurance and out-of-pocket costs). Resources used to deliver the trial interventions for each respective trial arm will also inform the economic evaluation.
Limitations
We acknowledge that our target effect size (SMD=0.50) might represent a larger between group difference than the lower bound of the previously reported between group difference (eg, the lower end of the previously reported MCID for iHOT-33 of 6 points).35 Therefore, we powered the study for an effect size of SMD=0.50, because a moderate effect would be considered clinically meaningful. While our two interventions do contain some similar elements, our pilot trial indicated we could potentially expect larger differences than six points between treatment groups.6
When we developed the two intervention groups, we deliberately sought to compare what we considered ‘best practice’ based on our understanding of impairments (reduced strength) against a standardised comparator that would seem credible to participants, to allow for participant blinding and same level of patient–clinician contact between groups. However, this does not allow us to test whether any between group differences are due to the different exercise components of the programme (strength vs stretch), or to the nature of the interventions (individualised vs standard), and this would need to be explored in future studies.
Trial status
Recruitment commenced in February 2018 and it is anticipated that this will be completed by September 2020. In March 2020, adjustments were made to the study protocol due to COVID-19, these are described in online supplemental file 5.
bmjopen-2020-041742supp005.pdf (46.1KB, pdf)
Conclusion
This RCT aims to compare the effectiveness of a physiotherapist-led intervention with targeted strengthening to a physiotherapist-led intervention with standardised stretching in 164 participants with FAI syndrome on hip-related QOL or patient-perceived global improvement. It may provide an evidence-based framework for physiotherapists to implement the first line of care for the treatment of FAI syndrome.
Ethics and dissemination
This study complies with the Declaration of Helsinki and has been approved by La Trobe University human research ethics committee. All participants will provide written informed consent prior to enrolment in the study. Participant information and consent forms for the study are included as online supplemental files 6 and 7. Participants will undergo a single pelvic radiograph for study inclusion, thus ensuring that the exposure to ionising radiation is no more than that in standard clinical exposure. The ethical and safety considerations associated with this trial are very low. We will disseminate study outcomes via submission to high-impact international peer-reviewed journals and presentation at international scientific conferences. By targeting a general medical journal, we will ensure study findings are disseminated to a variety of health professions.
bmjopen-2020-041742supp006.pdf (86.4KB, pdf)
bmjopen-2020-041742supp007.pdf (243.3KB, pdf)
Patient and public involvement
Patients were involved in the planning stages of this project. Patients provided input via questionnaires and interviews.
Patients’ priorities gathered during the questionnaires and interviews informed the development of the research question.
Patients and clinicians provided input into the development of the interventions, the frequency of treatment and their treatment goals.
Patients were not involved in the recruitment and conduct of the study.
Patients were asked to assess the burden of the intervention and time required to participate in the study during the planning stages of the study.
Patients and clinicians will provide input into the dissemination of study results by assisting with the decision on what information to share and in what format.
Supplementary Material
Acknowledgments
The authors acknowledge the staff of Lake Health Group, Ballarat, Australia; Lake Imaging, Ballarat, Australia; Imaging at Olympic Park, Melbourne, Australia; Clifton Hill Physiotherapy, Melbourne, Australia; Mill Park Physiotherapy, South Morang, Melbourne, Australia; and Complete Sports Care, Hawthorn, Melbourne, Australia.
Footnotes
Twitter: @JoanneLKemp, @MentiplayB, @mattgmking1, @DrDanilo_Silva, @StevenMMcPhail, @kaymcrossley
Contributors: JLK and KC conceived the study design. JLK and RTRJ prepared the manuscript. SLC, DMJ, AGS, BM, MGK, MJS, DDOS, AS, SMM and KC all contributed to the drafting of the manuscript and approved the final version.
Funding: JLK and SMM are funded by the National Health and Medical Research Council of Australia (JLK NHMRC ECF 1119971 and SMM NHMRC fellowship 1161138). Arthritis Australia contributed to the funding of this study.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Reiman MP, Agricola R, Kemp JL, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related pain research network, Zurich 2018. Br J Sports Med 2020;54:631–41. 10.1136/bjsports-2019-101453 [DOI] [PubMed] [Google Scholar]
- 2.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. The Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50:1169–76. 10.1136/bjsports-2016-096743 [DOI] [PubMed] [Google Scholar]
- 4.Mascarenhas VV, Rego P, Dantas P, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. Eur J Radiol 2016;85:73–95. 10.1016/j.ejrad.2015.10.016 [DOI] [PubMed] [Google Scholar]
- 5.Agricola R, Waarsing JH, Thomas GE. Cam impingement: defining the presence of a CaM deformity by the alpha angle: data from the check cohort and Chingford cohort. Osteoarthritis Cartilage 2014;22:218–25. 10.1016/j.joca.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 6.Kemp JL, Coburn SL, Jones DM, et al. The physiotherapy for femoroacetabular impingement rehabilitation study (physioFIRST): a pilot randomized controlled trial. J Orthop Sports Phys Ther 2018;48:307–15. 10.2519/jospt.2018.7941 [DOI] [PubMed] [Google Scholar]
- 7.Byrd JWT. Femoroacetabular impingement in athletes, part 1: cause and assessment. Sports Health 2010;2:321–33. 10.1177/1941738110368392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byrd JWT, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res 2009;467:739–46. 10.1007/s11999-008-0659-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weir A, Brukner P, Delahunt E, et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015;49:768–74. 10.1136/bjsports-2015-094869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kemp JL, Beasley I. 2016 international consensus on femoroacetabular impingement syndrome: the Warwick Agreement-why does it matter? Br J Sports Med 2016;50:1162–3. 10.1136/bjsports-2016-096831 [DOI] [PubMed] [Google Scholar]
- 11.Kemp JL, Risberg MA, Mosler A, et al. Physiotherapist-led treatment for young to middle-aged active adults with hip-related pain: consensus recommendations from the International Hip-related pain research network, Zurich 2018. Br J Sports Med 2020;54:504–11. 10.1136/bjsports-2019-101458 [DOI] [PubMed] [Google Scholar]
- 12.Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2020;72:149–62. 10.1002/acr.24131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018;27:2791–803. 10.1007/s00586-018-5673-2 [DOI] [PubMed] [Google Scholar]
- 14.Bussières AE, Stewart G, Al-Zoubi F, et al. The treatment of neck Pain-Associated disorders and Whiplash-Associated disorders: a clinical practice guideline. J Manipulative Physiol Ther 2016;39:523–64. 10.1016/j.jmpt.2016.08.007 [DOI] [PubMed] [Google Scholar]
- 15.Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK fashion): a multicentre randomised controlled trial. Lancet 2018;391:2225–35. 10.1016/S0140-6736(18)31202-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansell NS, Rhon DI, Meyer J. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med 2018:363546517751912. [DOI] [PubMed] [Google Scholar]
- 17.Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ 2019;364:l185. 10.1136/bmj.l185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freke MD, Kemp J, Svege I, et al. Physical impairments in symptomatic femoroacetabular impingement: a systematic review of the evidence. Br J Sports Med 2016;50:1180. 10.1136/bjsports-2016-096152 [DOI] [PubMed] [Google Scholar]
- 19.Kemp JL, Collins NJ, Makdissi M, et al. Hip arthroscopy for intra-articular pathology: a systematic review of outcomes with and without femoral osteoplasty. Br J Sports Med 2012;46:632–43. 10.1136/bjsports-2011-090428 [DOI] [PubMed] [Google Scholar]
- 20.Reiman MP, Thorborg K, Hölmich P. Femoroacetabular impingement surgery is on the Rise-But what is the next step? J Orthop Sports Phys Ther 2016;46:406–8. 10.2519/jospt.2016.0605 [DOI] [PubMed] [Google Scholar]
- 21.Agricola R, Heijboer MP, Bierma-Zeinstra SMA, et al. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (check). Ann Rheum Dis 2013;72:918–23. 10.1136/annrheumdis-2012-201643 [DOI] [PubMed] [Google Scholar]
- 22.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 25.Charlton PC, Bryant AL, Kemp JL. Single-Leg squat performance is impaired 1 to 2 years after hip arthroscopy. PM&R 2016;8:321–30. [DOI] [PubMed] [Google Scholar]
- 26.Crossley K, Grimaldi A, Kemp J. Grieve’s Modern Musculoskeletal Physiotjerapy : Hip related pain. 4th edn. London, 2015. [Google Scholar]
- 27.JL K, KM C, AG S, et al . Hip-related pain. : PD B, Khan KM, KM C, . Brukner and Khan’s Clinical Sports Medicine. Sydney: McGraw Hill, 2017. [Google Scholar]
- 28.Kemp JL, Moore K, Fransen M, et al. A phase II trial for the efficacy of physiotherapy intervention for early-onset hip osteoarthritis: study protocol for a randomised controlled trial. Trials 2015;16:26. 10.1186/s13063-014-0543-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kemp JL, Schache AG, Makdissi M, et al. Greater understanding of normal hip physical function may guide clinicians in providing targeted rehabilitation programmes. J Sci Med Sport 2013;16:292–6. 10.1016/j.jsams.2012.11.887 [DOI] [PubMed] [Google Scholar]
- 30.Medicine ACoS . .. : ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins, 2017. [Google Scholar]
- 31.McLeod C, Norman R, Litton E, et al. Choosing primary endpoints for clinical trials of health care interventions. Contemp Clin Trials Commun 2019;16:100486–86. 10.1016/j.conctc.2019.100486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mohtadi NGH, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International hip outcome tool (iHOT-33). Arthroscopy 2012;28:595–610. 10.1016/j.arthro.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 33.Impellizzeri FM, Jones DM, Griffin D, et al. Patient-Reported outcome measures for hip-related pain: a review of the available evidence and a consensus statement from the International Hip-related pain research network, Zurich 2018. Br J Sports Med 2020;54:848–57. 10.1136/bjsports-2019-101456 [DOI] [PubMed] [Google Scholar]
- 34.Kemp JL, Collins NJ, Roos EM, et al. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 2013;41:2065–73. 10.1177/0363546513494173 [DOI] [PubMed] [Google Scholar]
- 35.Mohtadi NGH, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International hip outcome tool (iHOT-33). Arthroscopy: The Journal of Arthroscopic & Related Surgery 2012;28:595–610. 10.1016/j.arthro.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 36.ten Klooster PM, Drossaers–Bakker WK, Taal E, et al. Patient-perceived satisfactory improvement (PPSI): Interpreting meaningful change in pain from the patient’s perspective. Pain 2006;121:151–7. 10.1016/j.pain.2005.12.021 [DOI] [PubMed] [Google Scholar]
- 37.Thorborg K, Hölmich P, Christensen R, et al. The Copenhagen hip and groin outcome score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med 2011;45:478–91. 10.1136/bjsm.2010.080937 [DOI] [PubMed] [Google Scholar]
- 38.Thorborg K, Branci S, Stensbirk F, et al. Copenhagen hip and groin outcome score (HAGOS) in male soccer: reference values for hip and groin injury-free players. Br J Sports Med 2014;48:557–9. 10.1136/bjsports-2013-092607 [DOI] [PubMed] [Google Scholar]
- 39.Beaton DE, Tang K, Gignac MAM, et al. Reliability, validity, and responsiveness of five at-work productivity measures in patients with rheumatoid arthritis or osteoarthritis. Arthritis Care Res 2010;62:28–37. 10.1002/acr.20011 [DOI] [PubMed] [Google Scholar]
- 40.Conner-Spady BL, Marshall DA, Bohm E, et al. Reliability and validity of the EQ-5D-5L compared to the EQ-5D-3L in patients with osteoarthritis referred for hip and knee replacement. Qual Life Res 2015;24:1775–84. 10.1007/s11136-014-0910-6 [DOI] [PubMed] [Google Scholar]
- 41.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakawaki M, Fukushima K, Inoue G, et al. Use of the painDETECT questionnaire to differentiate the nature of hip pain associated with a labrum tear. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology 2018;11:1–5. 10.1016/j.asmart.2017.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tampin B, Bohne T, Callan M, et al. Reliability of the English version of the pain DETECT questionnaire. Curr Med Res Opin 2017;33:741–8. 10.1080/03007995.2017.1278682 [DOI] [PubMed] [Google Scholar]
- 44.Campbell P, Hill JC, Protheroe J, et al. Keele aches and pains study protocol: validity, acceptability, and feasibility of the Keele start MSK tool for subgrouping musculoskeletal patients in primary care. J Pain Res 2016;9:807–18. 10.2147/JPR.S116614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller RP KS, Todd D. "The Tampa Scale: A Measure of Kinisophobia.". The Clinical Journal of Pain 1991;7:51–2. [Google Scholar]
- 46.Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000;85:317–32. 10.1016/S0304-3959(99)00242-0 [DOI] [PubMed] [Google Scholar]
- 47.Kvist J, Ek A, Sporrstedt K, et al. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 2005;13:393–7. 10.1007/s00167-004-0591-8 [DOI] [PubMed] [Google Scholar]
- 48.Crossley KM, Pandy MG, Majumdar S, et al. Femoroacetabular impingement and hip osteoarthritis cohort (force): protocol for a prospective study. J Physiother 2018;64:55. 10.1016/j.jphys.2017.10.004 [DOI] [PubMed] [Google Scholar]
- 49.Kemp JL, Risberg MA, Schache AG, et al. Patients with Chondrolabral pathology have bilateral functional impairments 12 to 24 months after unilateral hip arthroscopy: a cross-sectional study. J Orthop Sports Phys Ther 2016;46:947–56. 10.2519/jospt.2016.6577 [DOI] [PubMed] [Google Scholar]
- 50.Culvenor AG, Collins NJ, Vicenzino B, et al. Predictors and effects of patellofemoral pain following hamstring-tendon ACL reconstruction. Journal of Science and Medicine in Sport 2016;19:518–23. 10.1016/j.jsams.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 51.Lee S, Nardo L, Kumar D, et al. Scoring hip osteoarthritis with MRI (SHOMRI): a whole joint osteoarthritis evaluation system. Journal of Magnetic Resonance Imaging 2015;41:1549–57. 10.1002/jmri.24722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jones D, Crossley K, Dascombe B, et al. Validity and reliability of the FITBIT FLEX™ and ACTIGRAPH GT3X+ at jogging and running speeds. Int J Sports Phys Ther 2018;13:860–70. 10.26603/ijspt20180860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 2009;17:163–70. 10.1179/jmt.2009.17.3.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brukner P, Brukner KK. Khan’s Clinical Sports Medicine: Injuries. Fifth Edition. McGraw-Hill Education (Australia), 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-041742supp001.pdf (359.8KB, pdf)
bmjopen-2020-041742supp002.pdf (159.1KB, pdf)
bmjopen-2020-041742supp003.pdf (393.3KB, pdf)
bmjopen-2020-041742supp004.pdf (103.5KB, pdf)
bmjopen-2020-041742supp005.pdf (46.1KB, pdf)
bmjopen-2020-041742supp006.pdf (86.4KB, pdf)
bmjopen-2020-041742supp007.pdf (243.3KB, pdf)